Abstract
Background
The functional lumen imaging probe (FLIP), measures esophagogastric junction (EGJ) distensibility (cross sectional area/luminal pressure) during volume-controlled distension. The aim of this study was to apply this tool to the assessment of the EGJ in untreated and treated achalasia patients and to compare EGJ distensibility with other diagnostic tools utilized in managing achalasia.
Methods
Findings from FLIP, high-resolution manometry (HRM), timed barium esophagram, and symptom assessment by Eckardt Score (ES) were compared in 54 achalasia patients (23 untreated, 31 treated). Twenty healthy volunteers underwent FLIP as a comparator group. The EGJ distensibility index (EGJ-DI) was defined at the ‘waist’ of the FLIP bag during volumetric distension, expressed in mm2/mmHg. The ES was used to gauge treatment outcome: good response < 3 or poor response ≥ 3.
Key Results
Of the 31 treated patients, 17 had good and 14 poor treatment response. The EGJ-DI was significantly different among groups, greatest in the control subjects and least in the untreated patients; patients with good treatment response had significantly greater EGJ-DI than untreated or patients with poor response. The correlations between EGJ-DI and ES and integrated relaxation pressure on HRM were significant.
Conclusion
The FLIP provided a useful measure of EGJ distensibility in achalasia patients that correlated with symptom severity. The measurement of EGJ distensibility was complementary to existing tests suggesting a potentially important role in the clinical management of achalasia.
INTRODUCTION
Although the pathophysiology of achalasia is associated with impairment of both lower esophageal sphincter (LES) relaxation and peristalsis, treatments are focused on improving esophagogastric junction (EGJ) opening after swallowing. Thus, substantial effort in the patient evaluation is focused on assessing surrogates of EGJ opening, such as deglutitive EGJ relaxation pressure on high-resolution manometry (HRM) and bolus retention on timed barium esophagram. These tools are helpful in the diagnosis and management of achalasia 1–3, but they do not actually measure EGJ opening or distensibility after swallowing.
Our research group has recently validated a new technique based on high-resolution impedance planimetry to investigate the distensibility of the EGJ in both reflux disease 4 and post-fundoplication patients 5. This device measures cross-sectional area (CSA) at recording sites extending over an 8 cm axial length while concurrently measuring intraluminal pressure during volume controlled distensions. Our major findings were that the EGJ was more distensible in reflux patients than in control subjects, and that the fundoplication reduced distensibility to normal levels. Hence, we hypothesized that this tool could also be applied to study the mechanical properties of the EGJ in achalasia and that it might serve as a complementary tool to guide management. A recent paper by Rohof, et al. 6 suggests that EGJ distensibility may be a better predictor of esophageal emptying and clinical response than LES pressure using conventional manometry. However, these findings require further corroboration before being adopted clinically and a comparison with high resolution manometry would also be helpful as this has largely replaced conventional manometry in clinical practice. Thus, the aim of this study was to determine whether EGJ distensibility measured using the FLIP correlated with symptom severity in achalasia patients before and after treatment. Additionally, we sought to assess the relationship between EGJ distensibility and HRM metrics of EGJ function and radiographic measurements utilized in the management of achalasia.
MATERIALS AND METHODS
Subjects
54 patients (age [19–80] years, 29 male) were studied. Patients were prospectively recruited from the Esophageal Center at Northwestern based on esophageal symptoms suggestive of achalasia and previous evaluation confirming achalasia on HRM. Two cohorts were recruited: Group A) no achalasia treatment and Group B) patients after treatment with pneumatic dilation (n=17), Heller myotomy with partial fundoplication (n=10) or per-oral esophageal myotomy (n=4). All subjects were consented to undergo a questionnaire symptom assessment and FLIP evaluation. Every patient also underwent HRM, timed barium esophagram, and endoscopy as part of their clinical evaluation within one month of the FLIP study. Data from previously studied asymptomatic controls 4 were utilized as a healthy control group for EGJ distensibility. The study protocol was approved by the Northwestern University Institutional Review Board.
Symptom Score
Prior to the FLIP procedure, patients completed questionnaires to obtain basic demographic information and the components of the Eckardt Score (ES): weight, dysphagia severity, chest pain, and regurgitation. Each component was graded from 0 to 3 making the possible range of the ES from zero to twelve, with higher scores indicative of more severe symptoms 3. The group B patients were classified as having a good treatment response if the ES <3 or poor treatment response if the ES ≥ 3.
High-resolution Manometry
Manometric studies were done with the patients in the supine posture after at least a 6-h fast. The HRM catheter was a 4.2 mm outer diameter solid-state assembly with 36 circumferential sensors at 1-cm intervals (Given Imaging, Duluth, GA). Transducers were calibrated at 0 and 300 mmHg using externally applied pressure. The manometric assemblies were placed transnasally and positioned to record from the hypopharynx to the stomach with at least three intragastric sensors. The manometric protocol included a 5-min baseline recording and ten 5-ml swallows.
High resolution manometry studies were analyzed using ManoView analysis software (Given Imaging, Duluth, GA) to measure key esophageal pressure topography (EPT) metrics for analysis of clinical HRM studies: integrated relaxation pressure (IRP) 7, peristaltic integrity using the 20 mmHg isobaric contour (IBC), distal contractile integral, contractile front velocity, and the distal latency 8. The IRP quantifies EGJ relaxation both in completeness and persistence and reports the lowest mean EGJ pressure for 4 contiguous or non-contiguous seconds in the 10-second period following deglutitive upper sphincter relaxation. The upper limit of normal utilized for the IRP was <15 mmHg 7. Pressure topography metrics for describing esophageal peristalsis and pressurization patterns were utilized to diagnose achalasia and also to define achalasia subtypes 9: type 1, absent peristalsis with 100% failed peristalsis; type 2, achalasia with panesophageal pressurization in ≥ 20% of swallows; type 3 no normal peristalsis and premature (spastic) contractions in ≥ 20% of swallows.
Endoscopy
Subjects underwent esophagogastroduodenoscopy (EGD) in the left lateral decubitus position to rule out the exclusion criteria of esophagitis and stricture and also to help place the FLIP across the EGJ for distensibility measurements. A diagnostic gastroscope of 8.8 mm outer diameter was used (Olympus® GIF type Q180J, Olympus Corporation, Tokyo, Japan). Moderate sedation with 3 – 10 mg midazolam and 25 – 200 μg fentanyl was administered before and during the procedure.
Functional Luminal Imaging Probe (FLIP) System
EGJ distensibility was measured using a commercially developed FLIP (Crospon Medical Devices, Galway, Ireland), based on the concepts described previously 10. The FLIP utilizes impedance planimetry to determine multiple adjacent CSAs within a cylindrical bag placed in a tubular organ during volume-controlled distensions. The additional measure of the corresponding intrabag pressure during distension allows assessment of the CSA-pressure relationship (distensibility) of the area under study.
The FLIP assembly was 240 cm long with a 3-mm outer diameter. The infinitively compliant bag (up to a fill-in volume of 40 ml) mounted on the distal 14 cm of the probe was designed to assume a cylindrical shape 10 cm long between the tapering cone-shaped ends sealed at the assembly and designed to measure a minimal-to-maximal CSA range of 10 to 491 mm2. Within the bag was an 8-cm segment comprised of seventeen ring electrodes spaced 5-mm apart for impedance planimetry measurement. Excitation electrodes at either end emitted a constant low current making the voltage measured across each of the sixteen adjacent pairs of ring electrodes proportional to the impedance between them. Thus, as the bag was filled with a specially formulated conductive solution, the impedance across each segment was inversely proportional to the CSA of the bag at that locus. The probe also contained a solid-state pressure transducer that provided measurements of intra-bag pressure.
Measurements from the sixteen electrode pairs and pressure transducers were sampled at 10 Hz with the data acquisition system and transmitted to the recording unit that displayed them in real time as an 80-mm cylinder of varying diameter along its length, reflective of the 16 measured intraluminal diameters. Both the probe and the pressure transducers were precalibrated during the manufacturing process and required no additional calibration prior to use (CSA resolution 0.8 mm2, accuracy ±0.8 mm2; intra-bag pressure resolution 0.1 mmHg, accuracy ±0.8 mmHg). The only required preparation was to remove all air from the probe assembly using an automated purge sequence controlled by the recording unit. Subsequent establishment of pressure baseline and infusion of the conductive solution into the balloon were controlled using the touch-screen on the recording unit.
FLIP Protocol
At the end of the endoscopy, the FLIP was placed trans-orally until the center of the bag was positioned at the level of the SCJ measurement made during endoscopy. We have shown previously, that the FLIP bag assumes an hourglass shape when distended straddling the EGJ with a central constriction localized at the diaphragmatic hiatus. If the EGJ could not be confidently localized, the endoscope was reintroduced to confirm its position. The FLIP measures of EGJ CSAs and the corresponding distension pressure were made with the bag filled from 10 to 50 ml. In instances that measurements were interrupted by esophageal peristalsis, they were repeated. FLIP measurements were monitored in real-time to assure proper bag placement using the display of CSAs on the recording unit. If bag migration was suspected, the bag was repositioned and the measurement repeated. After completing the EGJ measures, the FLIP bag was deflated and withdrawn from the esophagus. The assessment of EGJ distensibility was usually completed in less than 5 minutes.
Esophagogastric junction CSAs and intra-bag pressures were assessed at each FLIP bag volume by quantifying the 50th percentile of each measure during each test 30-s recording. EGJ distensibility (CSA/pressure) was based on the narrowest CSA and the corresponding intrabag pressure. The EGJ distensibility index (EGJ-DI) at each distension volume was calculated as the narrowest CSA/intra-bag pressure, expressed in mm2/mmHg.
Timed Barium Esophagram
Timed barium esophagrams were done with the patient in the upright position to obtain frontal spot images of the esophagus at time zero, 1, 2, and 5 min after ingestion of 200 ml of low-density (45% weight in volume) barium sulphate (volume of barium sometimes limited by patient tolerance). The vertical height of the barium column relative to the axial position of the EGJ was measured on each timed image using a lead grid placed directly on the patient. A blinded radiologist made the measurement (SK). Additionally, the maximal esophageal width was measured perpendicular to the axial plane of the esophagus. A 5 cm cutoff for abnormal bolus retention was utilized based on previous data 11.
Statistical Analysis
Data for all continuous variables were expressed as median (IQR or 5th to 95th percentile). Statistical comparisons among groups used Kruskal-Wallis tests with significance set at p<0.05. Correlations between the various metrics (HRM variables, timed barium esophagram variables, EGJ-DI values) were calculated using Pearson correlation. Categorical variables were assessed using the Chi Square test.
RESULTS
Demographic Data
Patients were divided into three groups based on treatment status and ES score. Among the 54 achalasia patients, 23 were classified as no treatment, 17 as good treatment response, and 14 as poor treatment response. Demographic and symptom data among groups are presented in Table 1. The poor response patients and the no treatment patients had significantly greater ES compared to good treatment response patients. There was no significant difference in ES between the no treatment patients and the poor treatment response patients.
Table 1.
Comparison of achalasia patients based on treatment status: Esophageal function assessed by HRM and timed barium esophagram.
| Median (IQR) | No-treatment N=23 |
Good treatment response N=17 |
Poor treatment response N=14 |
|---|---|---|---|
| Age | 23 – 76 | 19 – 80 | 21 – 77 |
| M/F | 17/6 | 10/7 | 4/10 |
| Weight | 195 [170 – 209] | 170 [143 – 204] | 150 [131 – 164] |
| Eckardt Score | 6 [5 – 7.25] | 1 [0.75 – 2] § | 6 [5 – 11]* |
| Treatment | - | PD-8, LHM-6, POEM-3 | PD-9, LHM-4, POEM-1 |
| GERDQ | 9 [7 – 11] | 3.5 [1 – 7] | 5 [4 – 9] |
| Pre-treatment Achalasia Body Pattern | I-6, II-16, III-1 | I-6, II-9, III-2 | I-7, II-5, III-2 |
| Post-treatment Body Pattern | - | I-2, II-2, III-0, A-6, B-7, C-0 | I-5, II-1, III-2, A-3, B-2, C-1 |
| Basal EGJ pressure (mmHg) | 20 [3 – 46] | 8 [5.5 – 11.3] § | 10 [7 –16] § |
| Nadir EGJ relaxation pressure (mmHg) | 15.4 [4 – 38] | 8 [3 – 11] § | 11.6 [10 – 12.5] § |
| IRP (mmHg) | 19 [4.7 – 45.3] | 8.3 [6.1 – 13.3] § | 15.7 [12.3 – 20.1] *§ |
| Barium Column at 5 minutes (cm) | 10 [0 – 30] | 2.9 [0 – 7.2] § | 5.5 [2.2 – 8.2] § |
| Esophageal Diameter (cm) | 3.4 [0 – 7] | 2.5 [0.8 – 3.2] | 2.3 [1.4 – 3.3] |
PD- pneumatic dilation, LHM- Laparoscopic Heller myotomy, POEM- per-oral esophageal myotomy
Post treatment contractility pattern: A-absent peristalsis, B-weak peristalsis, C-spasm
p<0.05 poor responder versus good responder
p<0.05 treated versus untreated
Feasibility
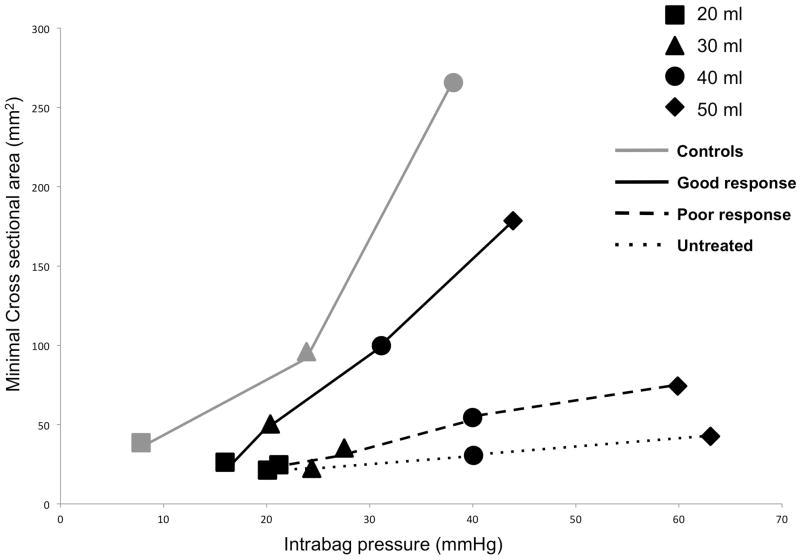
The FLIP bag assumed an hourglass shape in all patients (Figure 1). Real-time monitoring of FLIP measurements on the recording unit display facilitated the identification of occasional esophageal contractions and these were easily excluded from the analysis of the EGJ distensibility.
Figure 1.
Examples of the FLIP displayed EGJ geometry during a 40 ml distention in the three patient groups. EGJ distension is illustrated as a cylinder of varying diameter corresponding to the 16 cross-sectional areas (CSAs) measured by impedance planimetry within the FLIP bag. The corresponding intra-bag pressure is measured with a solid-state transducer also within the bag. Typically, the EGJ narrowed at the hiatus forming an hourglass shape with the locus of maximal constriction being the measurement of interest. The ‘waist’ at the EGJ in these examples is larger in the treated patient with a good response. Additionally, the pressure associated with the larger opening diameter is also lower, consistent with increased distensibility in this patient compared to the no-treatment and poor responder patients.
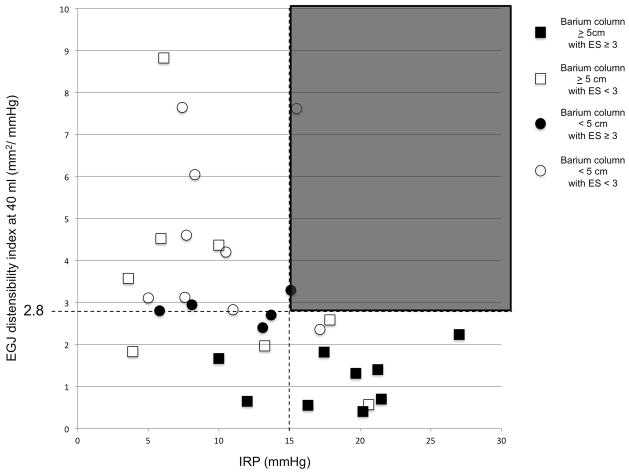
EGJ distensibility as a measure of treatment outcome in achalasia
Esophagogastric junction distensibility among the three achalasia groups and control subjects are illustrated in Figure 2 and the corresponding EGJ-DI values are presented in Table 2. The EGJ distensibility indices at 20, 30 ml and 40 ml were significantly different among the 4 groups. Specifically, the EGJ-DI was greatest in the control subjects and least in the untreated patients; patients with a good treatment response had significantly greater EGJ-DI than untreated patients or patients with a poor treatment response. The correlation between ES and EGJ-DI at 40 ml was significant (r=−0.49; p<0.05) (Figure 3A).
Figure 2.
Comparison of the EGJ-DI during volume controlled distention in the four study groups. The overall EGJ-DI, defined as the CSA (mm2) divided by the intrabag pressure (mmHg), was greater in control subjects compared to untreated patients and poor responders. The good responders also had greater distensibility compared to poor responders and untreated patients, comparable to control subjects.
Table 2.
EGJ-DI during volume distentions – Median [5th–95th]
| FLIP™ bag volume (ml) | EGJ-DI (mm2/mm Hg) | ||||
|---|---|---|---|---|---|
| Control subjects | Untreated achalasia | Achalasia, good treatment response | Achalasia, poor treatment response | P value | |
| 20 | 4.2 [0.3 – 7.1] | 1.1 [0.9 – 1.6] | 1.8 [1.2 – 2.2] | 1.4 [1 – 2.2] | <0.05 |
| 30 | 5.1 [0.8 – 21.7)] | 1 [0.8 – 1.2] | 2.5 [1.3 – 3.4] | 1.1 [0.8 – 2.6] | <0.001 |
| 40 | 8.2 [1.7 – 18.7] | 0.7 [0.5 – 1.1] | 3.4 [2.2 – 4.9] | 1.5 [0.6 – 2.8] | <0.001 |
Figure 3.
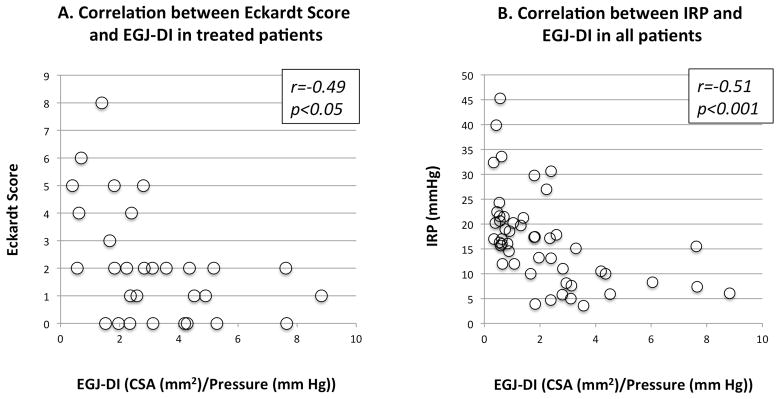
The correlation between EGJ distensibility index at 40 mL (EGJ-DI) and Eckardt score in treated patients (A). There was a moderate to weak inverse correlation between the two variables with ES rising as EGJ-DI decreased. The correlation between EGJ-DI and IRP in all patients (B). There was an inverse correlation between EGJ-DI and IRP.
Relationship between EGJ Distensibility and measures of esophageal function
The HRM metrics and timed barium esophagram measurements for the three subject groups are presented in Table 1. Among the untreated group, 6 patients were type 1, 16 were type 2 and one was type 3 achalasia. The resting EGJ pressure, nadir EGJ relaxation pressure, and IRP all were significantly greater in the untreated group compared to achalasia patients with a good and poor treatment response. The correlation between EGJ-DI at 40 ml and HRM metrics of EGJ function were significant for resting EGJ pressure, r=−0.4 (p<0.05), IRP, r=−0.51 (p<0.001) [figure 3B], and nadir EGJ relaxation pressure r=−0.4 (p>0.05).
The 5-minute barium column height and the esophageal diameter from the timed barium esophagrams are also presented in Table 1. Untreated patients had a higher median 5-minute barium column height and greater esophageal diameter compared to the treated patients. The correlation between the EGJ-DI at 40 ml and the barium column height was significant: r=−0.42 (p<0.05), however, there was no correlation with esophageal diameter: r=−0.27 (p>0.05).
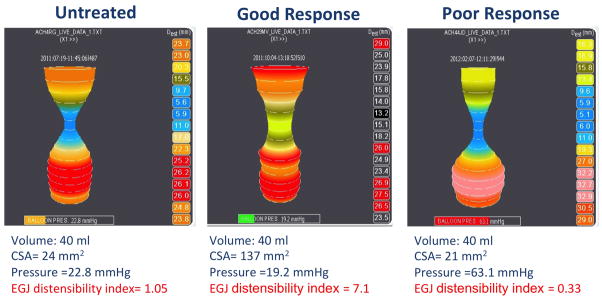
Concordance of the three functional assessments with Eckardt Score
Figure 4 depicts the relationship between the EGJ-DI at 40 ml, IRP, barium column height at 5 minutes, and ES. The correlations between EGJ-DI at 40 ml and IRP, ES and TBE are evident in Figure 4. There were only 2 instances in which the IRP was greater than 15 mmHg and the EGJ-DI was higher than 2.8. In these cases, IRP was marginally higher than 15 mmHg, suggesting that an abnormal IRP was almost never associated with normal distensibility (Figure 4, dark gray quadrant). Additionally, most of subjects with an abnormal IRP and an EGJ-DI at 40 ml of less than 2.8 had abnormal bolus retention on timed barium esophagram. However, there were instances of discordance between functional measures. There were 6 instances in which the IRP was normal and the EGJ-DI was less than 2.8 indicative of reduced opening. Four of these patients had an ES ≥ 3 and the two others had a barium column higher than 5 cm at 5 minutes on TBE, suggesting poor emptying. Additionally, the EGJ-DI of 2.8 had good correlation with ES despite the timed barium esophagram results. There were only 3 patients with an ES > 3 despite an EGJ-DI at 40 ml greater than 2.8; these patients had acid regurgitation with minimal to no dysphagia. This cut-off value of EGJ-DI of 2.8 was confirmed by the ROC curve, showing an area under the curve of 0.864.
Figure 4.
The relationship between IRP, EGJ-DI, and bolus retention on timed barium esophagram, and ES in the group of treated patients. The EGJ-DI at 40 ml, and IRP are plotted on the axes and the data point for each individual is further characterized based on the ES and barium column height at 5 minutes (BC). There was a logical concordance between IRP and EGJ-DI at 40 ml in that there was no instance where the two were contradictory; there were no instances in which the IRP was abnormal and the EGJ-DI at 40 ml was normal (dark gray box). However, there were instances in which the IRP was normal and patients continued to have either bolus retention and/or an ES ≥ 3. The cut-off value based on the 95th percentile for EGJ-DI at 40 ml (2.8 mm2/mmHg) had good discrimination for symptoms. Patients with an EGJ-DI at 40 ml > 2.8 mm2/mmHg and abnormal bolus retention had poor bolus clearance that was not directly related to an obstruction at the EGJ. Reduced emptying in this scenario was associated with low esophageal pressure that may be related to some esophageal dilatation and poor longitudinal muscle function. These defects would prevent the esophagus from pressurizing to a degree that facilitated bolus transit across the EGJ.
DISCUSSION
The cardinal abnormality of achalasia is a tightly closed LES that restricts flow to the stomach. The aim of this investigation was to test a novel instrument designed to characterize the severity of that restriction during clinical endoscopy. Our findings suggest that measuring EGJ distensibility with the FLIP was a feasible way to demonstrate reduced EGJ distensibility in untreated achalasia patients and to quantify the adequacy of treatments that had been rendered to mechanically disrupt the LES. EGJ distensibility, summarized by the EGJ-DI, was significantly less than normal in untreated achalasia patients and in patients with a poor treatment response while patients with a good treatment response had significantly greater EGJ distensibility than those with a poor response. The EGJ-DI also correlated with HRM measures of disease severity. These findings suggest that the FLIP may be a useful tool in achalasia management.
The EGJ is a complex anatomic zone that exists in a state of paradoxical function, both maintaining a tightly closed antireflux barrier and a compliant outlet to allow passage of food into the stomach after swallowing. This delicate balance depends on the harmonious functions of the LES, crural diaphragm, luminal geometry, and the inherent mechanical characteristics of the EGJ. Understanding the physiology of this small anatomic zone is essential because aberrations of EGJ opening during swallowing and/or at rest are the root cause of major esophageal diseases. The FLIP is a device uniquely suited to study the pathogenesis of these disorders as it provides a direct measurement of the flow limiting diameter of the EGJ under conditions in which it is challenged with volume distention. The measurement of the CSA and corresponding intraluminal pressure during these distensions provides a surrogate for the overall compliance of the EGJ reflective of the dominant pathology; in the case of achalasia a LES with impaired inhibitory innervation and even paradoxical contraction in the post-swallow interval. Findings from this study confirm that the FLIP can quantify these abnormalities and our results are in line with a recent paper by Rohof, et al. using a similar protocol 6. Together, these findings support that the FLIP is useful in the management of achalasia and other diseases manifest by EGJ dysfunction.
Other clinical tests have been utilized in the diagnosis and management of achalasia, specifically manometry and timed barium esophagram. However, these provide only surrogate measures of EGJ opening. Manometry detects force in the vector perpendicular to the luminal axis of the EGJ and measures sphincter contraction only when the esophageal wall is in contact with the sensor. Although, most patients with achalasia have a pinpoint LES, there are examples in which LES pressure may be normal or hypotensive and yet patients continue to have bolus retention on fluoroscopy. Similarly, although a timed barium esophagram images bolus retention and anatomical constriction at the EGJ, it provides minimal information on the distensibility of the EGJ challenged by volume distension. Even so, the EGJ-DI was significantly correlated with both HRM and timed barium esophagram measures in achalasia patients. However, we also found several instances of discrepancies among these measures in the treated patients. For example, there were eight instances in which the barium column at 5 minutes showed significant bolus retention and the IRP was normal; FLIP analysis suggested that four of these patients had bolus retention due to poor EGJ distensibility while the other four patients had adequate EGJ relaxation and distensibility, but bolus retention associated with low esophageal pressures related to anatomical deformity (sigmoid esophagus in two cases) or potentially impaired esophageal longitudinal muscle function.
Although FLIP provides a more direct measurement of EGJ function than HRM or timed barium esophagram; its likely use would be complementary to these tests. HRM is uniquely suited to characterize the pattern of esophageal contractility and to quantify impaired EGJ relaxation, thereby providing useful physiologic endpoints for defining the disease and assessing treatment efficacy. Similarly, a timed barium esophagram uniquely provides information on esophageal anatomy and bolus retention that has been demonstrated to be helpful in predicting long-term outcome. On the other hand, the FLIP could serve as an intraoperative tool during Heller myotomy or per oral endoscopic myotomy to determine the appropriate length and adequacy of the myotomy in real time. FLIP may also serve as an arbitrator of EGJ function in patients with symptoms after pneumatic dilation or myotomy and may help in difficult cases in which esophagectomy is contemplated as an alternative to further treatments targeting the EGJ.
In conclusion, this study showed that the FLIP provided a useful measurement of EGJ distensibility in achalasia patients that correlated with symptom severity. The measurement of EGJ distensibility is complementary to existing tests suggesting a potentially important role in the clinical management of achalasia. Outcome studies utilizing rigorous evaluation before and after treatment in a large series will be required to define the relative merits of FLIP, HRM and timed barium esophagram in achalasia management.
Acknowledgments
This work was supported by R01 DK56033 (PJK) and R01 DK079902 (JEP) from the Public Health Service
Abbreviations
- CSA
cross sectional area
- EPT
esophageal pressure topography
- EGJ
esophagogastric junction
- EGJ-DI
esophagogastric junction distensibility index
- HRM
high resolution manometry
- IRP
integrated relaxation pressure
- ES
Eckardt Score
Footnotes
AUTHORS CONTRIBUTION
John E. Pandolfino contributed to the conception and study design, obtained funding, data interpretation, manuscript editing, critical revision and final approval.
Annemijn de Ruigh contributed to data analysis and interpretation, and manuscript final approval.
Frédéric Nicodème contributed to the conception and study design, study supervision, data collection, analysis and interpretation, statistical analysis, manuscript drafting, editing, critical revision and final approval.
Yinglian Xiao contributed to analysis and interpretation, critical revision and final approval.
Lubomyr Boris contributed to data collection and analysis, and final approval.
Peter J. Kahrilas contributed to the conception and study design, obtained funding, data interpretation, editing, critical revision and final approval.
Conflicts of Interest: none
References
- 1.Vaezi MF, Baker ME, Richter JE. Assessment of esophageal emptying post-pneumatic dilation: use of the timed barium esophagram. Am J Gastroenterol. 1999;94:1802–1807. doi: 10.1111/j.1572-0241.1999.01209.x. [DOI] [PubMed] [Google Scholar]
- 2.Vaezi MF, Baker ME, Achkar E, et al. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50:765–770. doi: 10.1136/gut.50.6.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–1738. doi: 10.1016/0016-5085(92)91428-7. [DOI] [PubMed] [Google Scholar]
- 4.Kwiatek MA, Pandolfino JE, Hirano I, et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP) Gastrointest Endosc. 2010;72:272–278. doi: 10.1016/j.gie.2010.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwiatek MA, Kahrilas K, Soper NJ, et al. Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg. 2010;14:268–276. doi: 10.1007/s11605-009-1086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohof WO, Hirsch DP, Kessing BF, et al. Efficacy of Treatment for Patients with Achalasia Depends on the Distensibility of the Esophagogastric Junction. Gastroenterology. 2012:1–35. doi: 10.1053/j.gastro.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–85. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 8.Pandolfino JE, Ghosh SK, Rice J, et al. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103:27–37. doi: 10.1111/j.1572-0241.2007.01532.x. [DOI] [PubMed] [Google Scholar]
- 9.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 (Suppl 1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMahon BP, Frøkjaer JB, Liao D, et al. A new technique for evaluating sphincter function in visceral organs: application of the functional lumen imaging probe (FLIP) for the evaluation of the oesophago–gastric junction. Physiol Meas. 2005;26:823–836. doi: 10.1088/0967-3334/26/5/019. [DOI] [PubMed] [Google Scholar]
- 11.Nicodème F, de Ruigh A, Xiao Y, et al. A Comparison of Symptom Severity and Bolus Retention to Chicago Classification Esophageal Pressure Topography Metrics in Patients with Achalasia. Clin Gastroenterol Hepatol. 2012 doi: 10.1016/j.cgh.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]