Summary
Background
Although heart rate and respiratory rate are routinely measured in children in acute settings, current reference ranges are not evidence-based. The aim of this study is to derive new centile charts for heart rate and respiratory rate using systematic review data from existing studies, and to compare these with existing international ranges.
Methods
We searched MEDLINE, EMBASE, and CINAHL to April 2009, and reference lists to identify studies which had measured heart rate and/or respiratory rate in normal children between birth and 18 years of age. We used a non-parametric kernel regression method to create centile charts for heart rate and respiratory rate with respect to age. We compared existing reference ranges with those derived from the centile charts.
Findings
We included 69 studies, 59 of which provided data on the heart rate of 143,346 children, and 20 on the respiratory rate of 3,881 children. Our new centile charts demonstrate the decline in respiratory rate from birth to early adolescence, with the steepest decline apparent in infants under two years; decreasing from a median of 44 breaths/minutes at birth to 26 breaths/minute at the age of two. The heart rate centile chart demonstrates a small peak at one month of age. The median heart rate increases from 127 beats/minute at birth to a maximum of 145 beats/minute at approximately one month of age, before decreasing to 113 beats/minute by the age of two. Comparison of the centile charts with existing published reference ranges for heart rate and respiratory rate show marked disagreement with the centile charts, with limits from published ranges frequently exceeding the 99th and 1st centiles, or crossing the median.
Interpretation
Our review shows that existing international guidelines for heart rate and respiratory rate in children are not based on evidence. We have created new centile charts based on a systematic review of studies which have measured these vital signs in normal children. Clinical and resuscitation guidelines should be updated in the light of these evidence-based reference ranges.
Funding
Research funded by the National Institute for Health Research programme grant for applied research ‘Development and implementation of new diagnostic processes and technologies in primary care’. SF was funded by the Engineering and Physical Sciences Research Council and the National Institute for Health Research Biomedical Research Centre Programme.
Keywords: children, heart rate, respiratory rate, normal, centiles, ranges
Introduction
Heart rate and respiratory rate are key vital signs used to assess the physiological status of children in many clinical settings. They are used as initial measurements in acutely unwell children, as well as in those undergoing more intensive monitoring in high dependency or intensive care settings. During cardiopulmonary resuscitation, heart rate and respiratory rate are critical values used to determine responses to lifesaving interventions. Heart rate and respiratory rate remain an integral part of the standard clinical assessment of children presenting with acute illnesses,1 and are used in paediatric early warning scores2,3 and triage screening.4,5 Early warning scores are widely used in routine clinical care, and there is good evidence that they can provide early warning of clinical deterioration in hospitalised children and in emergency situations.6–9
Reference ranges for heart rate and respiratory rate in children are published by a variety of international bodies (Web Box 1). Of these, only two guidelines quote sources for their reference ranges: the Pediatric Advanced Life Support (PALS) guidelines10 cite two textbooks,11,12 neither of which cite sources for their ranges, and the WHO limits for respiratory rate, which are based on measurements made in developing countries.13 The evidence underpinning the guidelines is therefore limited, and it is likely that many of the ranges are based on clinical consensus.
Scoring systems underpinning triage and resuscitation protocols for children invariably require measurement of heart rate and respiratory rate. Measured rates are converted to a numerical score by applying age-specific thresholds. Accurate reference ranges are key to assessing whether a vital sign is abnormal. Thresholds that are incorrectly set too low risk overdiagnosing tachycardia or tachypnoea, whereas ones set too high risk missing children who do have tachycardia or tachypnoea. In addition, a reference range that is applied to an age range that is too broad is likely to lead to incorrect assessment of children within some parts of these age groups.
The aim of the present study is to develop new age-specific centiles for heart rate and respiratory rate in children, derived from a systematic review of all studies which measured these vital signs in normal children. We use these centiles to define new evidence-based reference ranges for normal children, which we compare with the existing reference ranges.
Methods
Search strategy and selection criteria
We included published studies based on the inclusion and exclusion criteria in Box 1. There were no language restrictions. We searched MEDLINE (1950 to April 2009), EMBASE (1980 to April 2009), and CINAHL (1982 to April 2009). Search terms included MeSH terms and free text (Web Table 1). We also searched reference lists of retrieved papers. Two authors (SF, MT) assessed eligibility of studies for inclusion, and disagreements were resolved by a third reviewer (AP).
Box 1. Inclusion and Exclusion Criteria.
Inclusion Criteria
– Cross-sectional, case-control, or longitudinal study
– Minimum of 20 subjects
– Age range between birth and 18 years
– Objective measurement of heart rate and/or respiratory rate
– Raw data or average measure of heart rate and/or respiratory rate reported for each age group
Exclusion Criteria
– Pre-term infants
– Children with illnesses likely to affect the cardiac or respiratory system
– Children with pacemakers or requiring ventilatory support
– Anaesthetised children
– Children known to be taking medications that would affect the cardiac or respiratory system
– Data from exercising children, without baseline (pre-intervention) measurements
– Measurements taken at elevations greater than 1,000m above sea level
– Age groups including adults (without subgroups)
– Age groups spanning more than 10 years (without subgroups)
Sources of existing reference ranges were identified by clinicians (MT, IM). To reflect the likely exposure of clinicians to reference ranges, we concentrated on ranges published in resuscitation guidelines, manuals for standardised clinical training courses, and international guidelines from the WHO (Web Box 1). These sources are not intended to be exhaustive, as a variety of reference ranges may be found in textbooks and as part of triage scores or early warning scores. These reference ranges were not considered in this review because of their heterogeneity.
Data extraction
The following data were extracted by one author (SF), and checked by a second reviewer (AP): year of study, participants (age range, number, reason for measurements being performed), study setting, method of measurement, and whether awake or asleep. The minimum and maximum ages of the group and the sample size were extracted, with the reported summary statistics (i.e. mean, median, centiles, standard deviation, confidence intervals, and/or standard error) for heart rate and/or respiratory rate. Where data were reported separately (i.e. for male and female subjects, or for subjects in different ethnic groupings) within the same age group, we treated them as independent groups.
Where multiple results were reported for a single group of children at a particular age (e.g. in different phases of sleep, or using different measurement methods) we selected a single data point to avoid introducing bias, based on the following guidelines agreed prior to data extraction: i) if different measurement methods were used, data from the least invasive or stressful method were selected; ii) where data were presented as combined age groups, we selected data from separate age groups unless the age ranges spanned by the individual groups were very small (e.g. infants between one and two days of age); iii) we used the awake measures when both awake and asleep measurements were available; iv) we averaged readings over all sleep states where multiple states of sleep were reported; v) we used the first baseline result where multiple baseline measurements were recorded in intervention studies. The guidelines were chosen to ensure that the data used was relevant to the clinical setting, where children are typically awake and at rest, to improve the accuracy of the calculated centile charts, and to avoid potential confounding factors such as the definition of sleep states, or distress due to invasive measurements or interventions. Combined age groups were separated to ensure that the most accurate age range was associated with each data point, but very small age ranges were left combined, as it was felt that the benefit of accurate ages would be small, compared to the loss of accuracy for raw centiles calculated from small sample sizes.
Data analysis
We calculated the median and representative centiles (1st, 10th, 25th, 75th, 90th, 99th) for the data from each included study. Where the relevant summary statistics were not reported by a study, we estimated them from the mean and standard deviation. We used Pearson’s 2nd skewedness coefficient and Bowley skewness to test for skewness. We observed no skewness in either the heart rate or respiratory rate data, and so assumed a normal distribution at each age. We excluded two outlier values of data spread (one standard error, and one set of confidence intervals) as they resulted in negative respiratory rates for a number of centiles, which is not physiologically plausible.14,15 We did not identify any outliers in the heart rate data.
We created centile charts using kernel regression, a form of non-parametric curve fitting16 which avoids imposing an excessive degree of constraint on the resulting curves. We adjusted the classical kernel regression to take account of both the age range and sample size associated with each data point. More details on this method may be found in Web Annex 1. For both heart rate and respiratory rate, kernel regression was used to fit seven curves showing the variation with respect to age, using the calculated values for the median and six representative centiles from the included studies. These centiles were compared visually to the reference ranges in Web Box 1.
Subgroup analyses assessed whether the setting, economic development of the country, method of measurement, or awake/asleep state of the child had an effect on the vital signs after correction for age using the centile charts. While ideally separate centile charts could be created to compare subgroups, many subgroups did not contain sufficient data across the full age range to allow this. Therefore, the mean and standard deviation of the measured vital signs from each study were normalised using the centile charts, so that variations due to age were removed. The normalised data was analysed using one-way ANOVA, taking into account the size and variation in each study. In addition, regression analysis of the normalised means, weighted by the sample size of each study, was carried out to identify trends related to the date of publication.
We determined cut-off values for heart rate and respiratory rate using the data from the centile charts by calculating the mean value in each of 13 age groups covering the full range of ages (0-18 years). The age groups were selected to correspond to changes of approximately five beats/minute in heart rate and two breaths/minutes in respiratory rate. Cut-off values were selected based on this mean value by choosing an appropriate integer value.
Role of the funding source
The sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, writing of the report or the decision to submit the paper for publication. SF had full access to all the data in the study, and had final responsibility for the decision to submit for publication.
Results
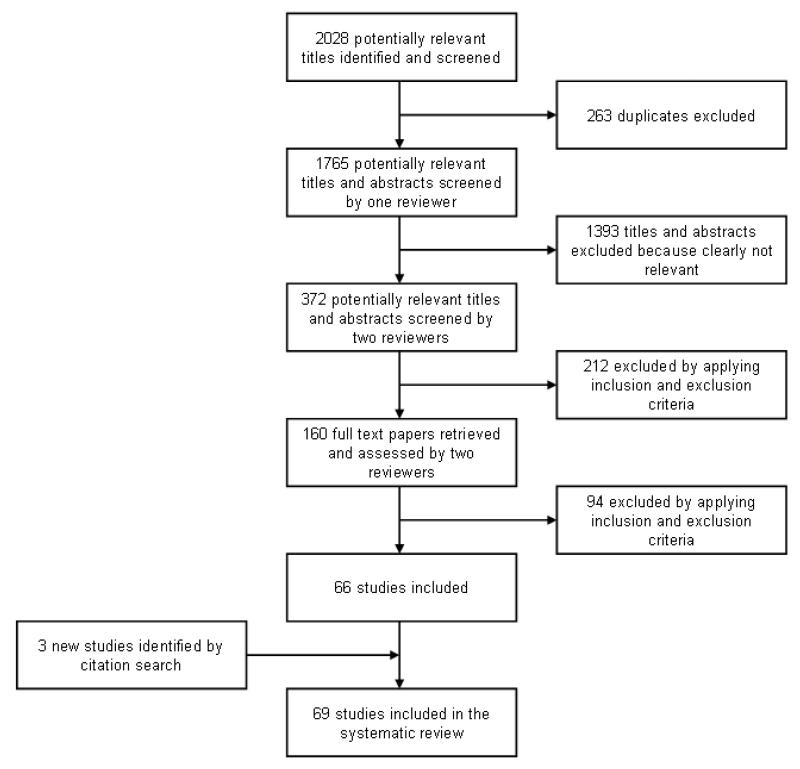
We identified 69 studies from an initial 2,028 publications (Figure 1). Of the 69 studies, 59 provided data on heart rate from 150,080 measurements on 143,346 children, and 20 provided data on respiratory rate from 7,565 measurements on 3,881 children, with ten studies providing data on both. Scatter plots of the data extracted from the studies are shown in Web Figure 1. Study types were cross-sectional (46), longitudinal (12), or case-control (11). Studies were performed in 20 different countries from four continents (Web Tables 2 & 3): 55 (80%) in developed countries (as defined by the United Nations Statistics Division), 7 (10%) in developing countries, and 7 (10%) in countries considered to be neither developing nor developed.
Figure 1.
Flowchart of the systematic search process
The number of subjects per study ranged from 20 to 101,259. Studies were carried out in the community e.g. home, school or kindergarten (27 studies, 26,024 measurements), in clinical settings e.g. hospitals, clinics or medical centres (19 studies, 105,982 measurements), in unspecified or multiple settings (17 studies, 15,957 measurements), and in research laboratories (6 studies, 3,976 measurements). Most measurements (32 studies, 132,891 measurements) were on awake children, while 8 studies (505 measurements) were on asleep children, and 29 studies (18,545 measurements) did not report the state of wakefulness, or did not distinguish between data from awake or asleep children.
Most studies measured heart rate with an electrocardiograph (ECG) (31 studies, 114,802 measurements), while others used automated blood pressure monitors (12 studies, 21,362 measurements), manual measurement (6 studies, 10,228 measurements), echocardiography (4 studies, 890 measurements), and pulse oximeters or proprietary heart rate monitors (6 studies, 2,798 measurements). The majority of respiratory rate measurements were made manually (7 studies, 6,531 measurements), with automated measurements using strain gauges, thermistors, thoracic impedance and helium dilution in 13 studies (1,034 measurements).
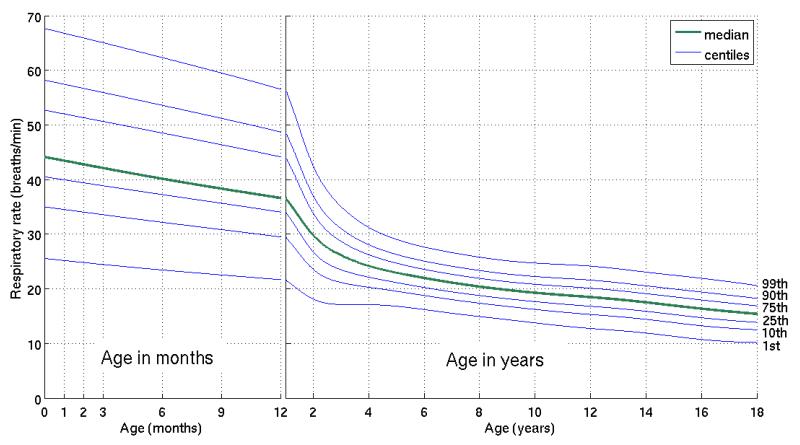
Centiles of normal respiratory rate
The 1st to 99th centiles of respiratory rate in normal children from birth to 18 years of age are displayed in Figure 2. These demonstrate the decline in respiratory rate from birth to early adolescence, with the steepest decline apparent in infants during the first two years of life. The median respiratory rate decreases by 40% in these two years (44 breaths/minute at birth to 26 breaths/minute at two years). Web Table 4 presents the proposed cut-offs for respiratory rate at each of 13 age groups from birth to 18 years of age.
Figure 2.
Centiles of respiratory rate for normal children from birth to 18 years of age
The subgroup analysis of the respiratory rate data showed no significant differences based on the type of study setting (P=0·09), level of economic development of the country in which it was carried out (P=0·83), wakefulness of the child (P=0·36), or whether manual or automated methods of measurement were used (P=1·00). Regression analysis on the dates of publication did not show any significant difference in measured respiratory rate (P=0·19).
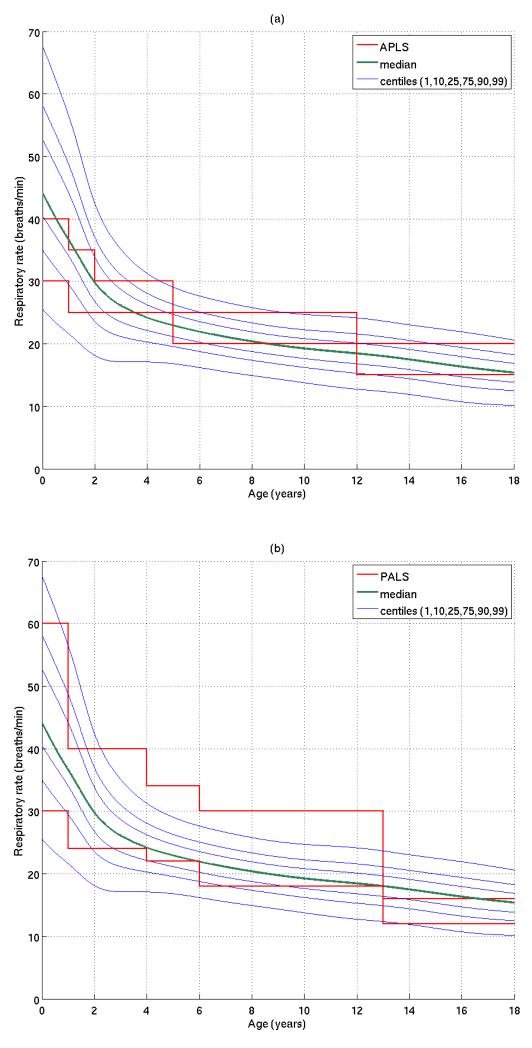
Figure 3 shows how the centiles derived from our systematic review compare to two existing reference ranges (APLS and PALS). None of the existing reference ranges detailed in Web Box 1 showed good agreement with our centile charts across the whole age range from birth to 18 years of age, but the best agreement was seen with the ranges quoted by APLS and EPLS (European Paediatric Life Support Course).17,18 Examples of this disparity can be seen in the graphs in Figure 3. For example, in children under one year of age, the APLS upper limit for respiratory rate is 40 breaths/minute, which approximates to the median value on our centile chart for children in this age range. In children over 12 years of age, the PALS upper limit of 16 breaths/minute is below the median value on our centile chart for much of this age range.
Figure 3.
Comparison of respiratory rate centiles with paediatric reference ranges from the Advanced Paediatric Life Support (APLS) and Pediatric Advanced Life Support (PALS) guidelines.
We noted that one median value of respiratory rate for children between 0 and 6 months of age,19 was considerably higher than the median values at this age from many other studies. However, as can be seen from Web Figure 1(a), the spread of measured respiratory rates at these ages is very large. Since the kernel regression method used to create the centile charts takes account of both age range and sample size, it was not felt that this data point would bias the estimation, and so we did not consider this to be an outlier.
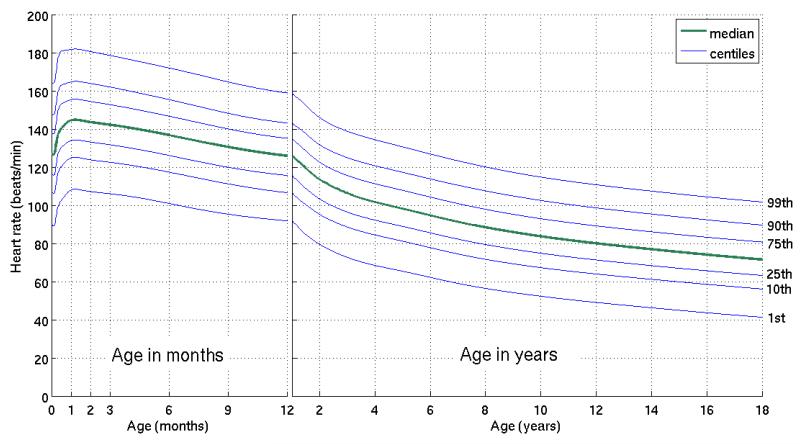
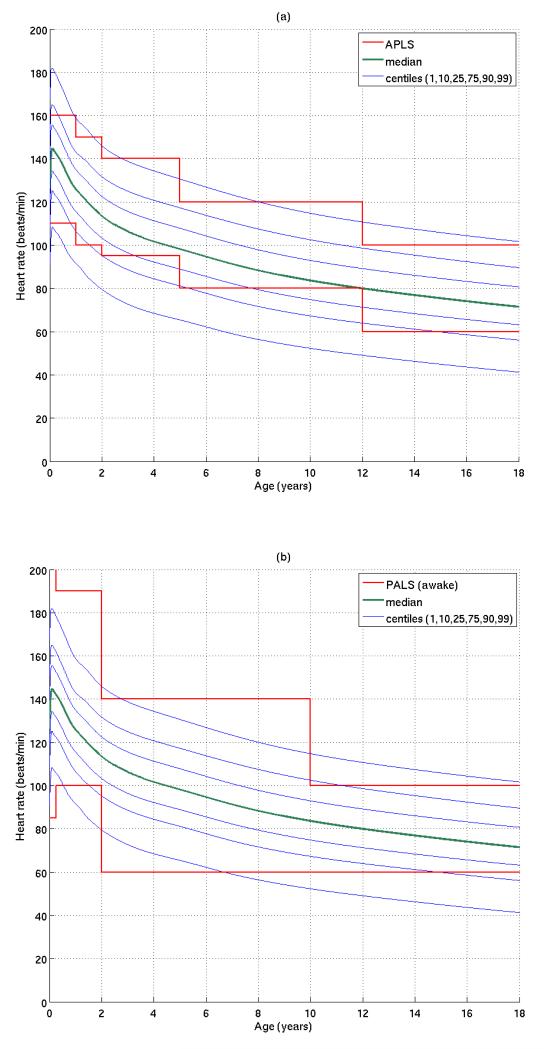
Centiles of normal heart rate
The 1st to 99th centiles of heart rate against age are displayed in Figure 4, with the proposed cut-offs for heart rate in Web Table 5. These show a decline in heart rate with age. The first section of Figure 4, showing the heart rate centile chart for infants under one year of age, demonstrates a small peak in heart rate at one month of age. This peak is not an artefact of the modelling method, but can be observed in the primary data from a number of studies that report multiple measurements on infants under one year of age.20-25 The median heart rate in this age range increases from 127 beats/minute at birth, reaching a maximum of 145 beats/minute at approximately one month of age, before decreasing to 113 beats/minute by two years of age.
Figure 4.
Centiles of heart rate for normal children from birth to 18 years of age
Subgroup analysis revealed that heart rates measured in community settings were higher (P<0·0001) than those measured in clinical or laboratory settings, and rates measured using automated techniques (e.g. ECG) were higher (P=0·0011) than those measured manually. Heart rates of children in developing countries were also found to be higher than those measured in developed countries (P<0·0001). Although heart rates measured in awake children tended to be higher than those measured in asleep children, this did not reach statistical significance (P = 0·06). Regression analysis on the dates of publication showed that there was a small but significant trend in heart rate (P<0·0001), with older studies tending to measure lower heart rates than more recent studies.
Figure 5 compares the reference ranges from the APLS and PALS guidelines with our centiles of heart rate. Comparisons were also made between our centile chart and the other reference ranges cited in Web Box 1. As with respiratory rate, none of these ranges showed good agreement with our centile chart across the whole age range from birth to 18 years of age. The best agreement between the reference ranges for heart rate and our centile chart was observed with the APLS and ATLS reference ranges,17,26 although both of these also showed considerable disagreement with our centile charts. For example, in children from 2 to 5 years of age, the APLS lower limit for heart rate is 95 beats/minute, which approximates to the 25th centile from our chart, and reaches the median heart rate at the upper end of the age range. In children 2 to 10 years of age, the upper limit for PALS is 140 beats/minute, which lies above the 99th centile from our chart for most of the age range.
Figure 5.
Comparison of heart rate centiles with paediatric reference ranges from the Advanced Paediatric Life Support (APLS) and Pediatric Advanced Life Support (PALS) guidelines.
Discussion
The reference ranges for heart rate and respiratory rate cited in international paediatric guidelines, such as those presented in Web Box 1, are widely used as the basis for clinical decisions when interpreting vital signs in children. For example, the widely used PAWS and Brighton PEWS2,3 assessment tools refer to APLS reference ranges. We have shown that: 1) there is considerable disagreement between these reference ranges; 2) they appear to be inconsistent with existing evidence on heart and respiratory rates in healthy children.
For clinicians involved in the assessment of children, our findings suggest that current consensus-based reference ranges for heart rate and respiratory rate should be updated with new thresholds based on our proposed centile charts, particularly for age groups where our findings show that many children are likely to be misclassified. Normal ranges, such as those published in textbooks and clinical handbooks, should also be updated in the light of our results. To assist the development of cut-offs for use in clinical settings, we present values corresponding to the median and six different centiles for both heart rate and respiratory rate for 13 age groups between birth and 18 years of age.
By providing several different centiles for children of all ages, we have given clinicians and those responsible for developing clinical guidelines and early warning scores sufficient information to select cut-offs that are most appropriate to the type of clinical setting in which they are likely to be used. Selection of an appropriate cut-off should take into account the likely derangement in vital signs associated with the level of illness that is to be detected, and the penalty associated with misclassifying both healthy and unwell children. Further research may be required in some areas to ascertain this. Where multiple measurements are made over time, the centile charts may also be used to assess the magnitude of changes in heart rate or respiratory rate.
Clinicians who wish to carry out accurate measurements of heart rate in children should be aware that manual measurement of heart rates, which is common practice in many settings, may underestimate the true rates. In these children, measurement of heart rate by automated methods provides more accurate results. Professional bodies responsible for publishing guidelines and scoring systems should consider revising current thresholds, by selecting heart rate and respiratory rate values that represent an upper centile for each age group. To facilitate this, the authors propose to make the data used to create Figures 2 and 4 freely available upon request.
A key strength of our approach is that the centile charts were created using kernel regression, a non-parametric modelling technique which avoids imposing any particular form onto the shape of the centile charts. This is particularly important for this type of data, as there is no reason to expect that it will follow an analytical function such as a straight line or exponential. However, a number of limitations to the method are worth noting. Our systematic review involved an extensive search of the available literature using three large databases, with no restriction on language or country of publication. However, it is possible that our search strategy and inclusion criteria may have missed relevant studies, particularly studies published before 1960. We excluded 13 studies as we were not able to extract the required data or could not obtain full copies, and we did not attempt to contact original authors to obtain individual patient data, as this would not have been feasible given the number of included studies, some of which were published over 25 years ago. We observed marked heterogeneity in the settings in which the children were measured, their state of wakefulness, and the method of measurement, all of which may have an effect on the measured variables. As reported, subgroup analysis showed that the setting, method of measurement, and economic development had a significant effect on heart rate in children, but not on respiratory rate (for more detail see Web Annex 2). We excluded children with illnesses that might affect the heart rate or respiratory rate, and measurements known to be made during exertion, but many studies did not report whether children were quiet or agitated during measurement, which may have introduced additional heterogeneity that could not be assessed. However, by using the subgroup analysis on wakefulness as a proxy for agitation, it is unlikely that this would have a significant effect on the results. The heterogeneity of the data can also be interpreted as a strength, making the centiles more relevant to a wide spectrum of clinical settings.
Our centile charts have been developed using data from normal children. As with all clinical measurements, they should be used as part of an overall assessment of a child’s condition, and interpretation of measured values should also take into account any factors which might be expected to affect the measured value. For example, measurements of heart rate may be increased in the presence of fever,27 anxiety, or if measured with automated methods or in developing countries. These should therefore inform the selection of appropriate centiles for use as cut-offs in such situations.
Further research should consider assessing the benefit of integrating our centiles into early warning scores. Improvement in sensitivity and specificity will be age-dependent and will depend on the accuracy of the previous reference ranges. For the existing APLS reference ranges, which were observed to have the greatest agreement with our centiles, Figures 3 and 5 suggest that a large number of children are currently misclassified. For example, at the age of ten years, the APLS cut-off for heart rate classifies approximately 40% of normal children as abnormal, and the APLS cut-off for respiratory rate misclassifies approximately 63% of normal children. Furthermore, based on the age distribution of children presenting to primary care in a previously reported study,27 we estimate that the specificity of APLS could be improved by as much as 20% for heart rate, and 51% for respiratory rate if revised centile charts are used. Further research, in both healthy children, and those presenting with a spectrum of conditions, should test the validity of our centiles and any cut-offs derived from them.
In conclusion, we have shown that existing reference ranges for heart rate and respiratory rate in children are inconsistent, and do not agree with centile charts derived from a systematic review of observational studies. This has potentially wide-ranging implications for clinicians involved in the assessment of children, and for the design of resuscitation guidelines, triage scores, and early warning systems.
Supplementary Material
Box 2. Summary.
Systematic Review
– We searched CINAHL, MEDLINE and EMBASE to April 2009, and reference lists, for studies measuring heart rate and/or respiratory rate in normal children between birth and 18 years of age.
– Measurements during exercise, at altitude, or on children whose condition was likely to affect their heart rate or respiratory rate were excluded.
– Non-parametric kernel regression taking into account age range and sample size was used to construct centile charts based on the extracted data.
Interpretation
– There is considerable disagreement between existing consensus-based reference ranges for heart rate and respiratory rate in children.
– Existing reference ranges for heart rate and respiratory rate in children do not correspond to centile charts derived from a meta-analysis of observational studies across the full range of ages.
Acknowledgements
The authors wish to acknowledge the assistance and advice of Nia Roberts, Ruth Davis, Dr Robert Oakey, Dr Lee Wallis, and Dr Jill Mant, and the support of the NIHR School for Primary Care Research, the Engineering and Physical Sciences Research Council and the NIHR Biomedical Research Centre Programme. The Department of Primary Health Care is part of the NIHR School of Primary Care Research. This study was funded by the NIHR Programme Grant ‘Development and implementation of new diagnostic processes and technologies in primary care’.
Footnotes
Conflicts of interest IM is the UK chair for the European Paediatric Life Support Course, and a member of the European Guidelines writing team.
References
- 1.National Collaborating Centre for Women’s and Children’s Health . Feverish illness in children: assessment and initial management in children younger than 5 years. National Institute for Health and Clinical Excellence; 2007. Report number: CG47. [Google Scholar]
- 2.Monaghan A. Detecting and managing deterioration in children. Paediatric nursing. 2005;17(1):32–5. doi: 10.7748/paed2005.02.17.1.32.c964. [DOI] [PubMed] [Google Scholar]
- 3.Egdell P, Finlay L, Pedley DK. The PAWS score: validation of an early warning scoring system for the initial assessment of children in the emergency department. Emergency medicine journal : EMJ. 2008;25(11):745–9. doi: 10.1136/emj.2007.054965. [DOI] [PubMed] [Google Scholar]
- 4.Gilboy N, Tanabe P, Travers D, Rosenau A, Eitel D. Emergency Severity Index, Version 4: Implementation Handbook. Agency for Healthcare Research and Quality; 2005. [Google Scholar]
- 5.Warren DW, Jarvis A, LeBlanc L, Gravel J. Revisions to the Canadian Triage and Acuity Scale paediatric guidelines (PaedCTAS) Canadian Journal of Emergency Medicine. 2008;10(3):224–43. [PubMed] [Google Scholar]
- 6.Duncan H, Hutchinson J, Parshuram CS. The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children. J Crit Care. 2006;21(3):271–8. doi: 10.1016/j.jcrc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Parshuram CS, Hutchinson J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Critical Care. 2009;13:R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akre M, Finkelstein M, Erickson M, Liu M, Vanderbilt L, Billman G. Sensitivity of the Pediatric Early Warning Score to identify patient deterioration. Pediatrics. 2010;125(4):e763–9. doi: 10.1542/peds.2009-0338. [DOI] [PubMed] [Google Scholar]
- 9.Bradman K, Maconochie I. Can paediatric early warning score be used as a triage tool in paediatric accident and emergency? Eur J Emerg Med. 2008;15(6):359–60. doi: 10.1097/MEJ.0b013e3283026208. [DOI] [PubMed] [Google Scholar]
- 10.American Heart Association . Pediatric Advanced Life Support Provider Manual. American Heart Association; 2006. [Google Scholar]
- 11.Adams FH, Emmanouilides GC, Riemenscheider TA, editors. Moss’ Heart Disease in Infants, Children and Adolescents. 4th ed Williams and Wilkins; 1989. [Google Scholar]
- 12.Hazinski MF. Manual of Pediatric Critical Care. Mosby; 1999. [Google Scholar]
- 13.World Health Organization . Technical bases for the WHO recommendations on the management of pneumonia in children at first-level health facilities. World Health Organization; 1991. Report number: WHO/ARI/91.20. [Google Scholar]
- 14.Balasubramanian S, Suresh N, Ravichandran C, Dinesh CG. Reference values for oxygen saturation by pulse oximetry in healthy children at sea level in Chennai. Annals of Tropical Paediatrics: International Child Health. 2006;26(2):95–9. doi: 10.1179/146532806X107421. [DOI] [PubMed] [Google Scholar]
- 15.Ward SL, Jacobs RA, Gates EP, Hart LD, Keens TG. Abnormal ventilatory patterns during sleep in infants with myelomeningocele. J Pediatr. 1986;109(4):631–4. doi: 10.1016/s0022-3476(86)80226-8. [DOI] [PubMed] [Google Scholar]
- 16.Wand MP, Jones MC. Kernel Smoothing. Chapman and Hill; 1995. [Google Scholar]
- 17.Advanced Life Support Group . Advanced Paediatric Life Support: The Practical Approach. 4th ed WileyBlackwell; 2004. [Google Scholar]
- 18.Biarent D, Resuscitation Council (UK) European Resuscitation Council . European paediatric life support course. 2nd ed Resuscitation Council (UK); 2006. [Google Scholar]
- 19.Morley CJ, Thornton AJ, Fowler MA, Cole TJ, Hewson PH. Respiratory rate and severity of illness in babies under 6 months old. Arch Dis Child. 1990;65(8):834–7. doi: 10.1136/adc.65.8.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Betau H, Tzee-Chung W, Meng L. An electrocardiographic study of chinese infants. Chung Hua Min Kuo Hsiao Erh Ko I Hsueh Hui Tsa Chih. 1980;21(4):247–55. [Google Scholar]
- 21.Davignon A, Rautaharju P, Boisselle E, Soumis F, Mégélas M, Choquette A. Normal ECG standards for infants and children. Pediatr Cardiol. 1980;1(2):123–31. [Google Scholar]
- 22.Lindner W, Döhlemann C, Schneider K, Versmold H. Heart rate and systolic time intervals in healthy newborn infants: longitudinal study. Pediatr Cardiol. 1985;6(3):117–21. doi: 10.1007/BF02336549. [DOI] [PubMed] [Google Scholar]
- 23.Gemelli M, Manganaro R, Mamí C, De Luca F. Longitudinal study of blood pressure during the 1st year of life. European Journal of Pediatrics. 1990;149(5):318–20. doi: 10.1007/BF02171556. [DOI] [PubMed] [Google Scholar]
- 24.Macfarlane PW, McLaughlin SC, Devine B, Yang TF. Effects of age, sex, and race on ECG interval measurements. J Electrocardiol. 1994;27(Suppl):14–9. doi: 10.1016/s0022-0736(94)80039-1. [DOI] [PubMed] [Google Scholar]
- 25.Semizel E, Öztürk B, Bostan OM, Cil E, Ediz B. The effect of age and gender on the electrocardiogram in children. Cardiology in the Young. 2008;18(1):26–40. doi: 10.1017/S1047951107001722. [DOI] [PubMed] [Google Scholar]
- 26.American College of Surgeons . ATLS: Advanced Trauma Life Support for Doctors. 7th ed American College of Surgeons; 2004. [Google Scholar]
- 27.Thompson MJ, Harnden A, Perera R, et al. Deriving temperature and age appropriate heart rate centiles for children with acute infections. Arch Dis Child. 2009;94(5):361–5. doi: 10.1136/adc.2008.145011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.