Abstract
Amyloidosis is typically a systemic depositional disease, diagnosed on clinical symptoms and signs in conjunction with histopathology. When occurring on a localized basis in the head and neck, the lesion is most commonly observed in the larynx. Primary localized nasal amyloidosis however is an uncommon finding, with 25 reported cases in the literature to date. We present the case of a young woman presenting with primary localized nasal amyloidosis secondary to the curious symptoms of unilateral hearing loss.
INTRODUCTION
Amyloidosis is usually a systemic disease, only rarely observed on a localized basis. Primary localized nasal amyloidosis therefore is a particularly uncommon finding, with 25 reported cases in literature to date [1, 2]. When diagnosed in the head and neck, it has predilection for the larynx, occurring in 61% of cases [1], with no gender or age predominance [3]. It is pathologically benign.
We present the case of a young woman presenting with primary localized nasal amyloidosis.
CASE REPORT
A 31-year-old teacher was referred by her General Practitioner (GP) for investigation of an 18-month history of left-sided fluctuating hearing loss. No other otological symptoms were reported. The patient had a history of focal migraines and polycystic ovary disease and took no regular medication. Initial physical examination revealed rhinitic-like mucosa bilaterally. Otoscopy and audiometry suggested a unilateral otitis media with effusion and unilateral conductive deafness, respectively, with subsequent flexible endoscopy revealing a cystic lesion (Fig. 1) obstructing the Eustachian tube opening.
Figure 1:

Images from left-sided rigid endoscopy demonstrating an abnormal cystic mass.
A left grommet was inserted and the lesion was biopsied, revealing an amyloid plaque confirmed on Congo Red staining. Computed tomography and magnetic resonance imaging scans were subsequently performed (see Figs 2 and 3) which showed a ‘1.5 × 2.3 cm mass arising from the torus tubaris and pterygoid fossa, protruding into the post nasal space’. Further radiological investigations of the entire body were conducted for investigation primary amyloidosis which all proved negative, confirming the diagnosis of primary isolated sinonasal amyloidosis. Management options were discussed and, due to the resolution of symptoms, a period of watchful waiting was commenced. Two years after initial presentation, the patient was discharged back to her GP without need for further intervention.
Figure 2:
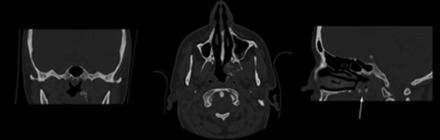
Initial CT images of sinonasal lesion.
Figure 3:
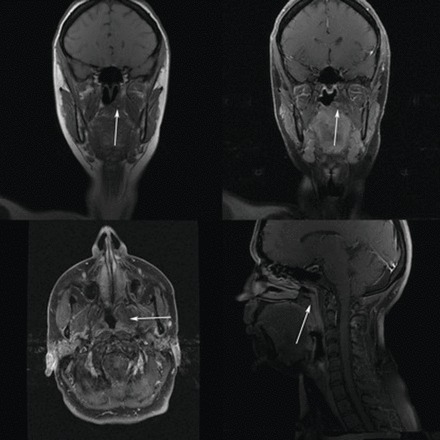
MRI images of sinonasal lesion.
Eight years after discharge, the patient presented once again with ipsilateral hearing loss secondary to re-accumulation of a middle ear effusion. At this point, the growth had extended beyond resectable limits and the patient was treated palliatively for symptom control and placed on annual outpatient follow-up.
DISCUSSION
Amyloidosis is a depositional disease characterized by the accumulation of amyloid, a fibrillar protein substance [3, 4], in cells throughout the body. Its architecture is classically described as a meshwork of straight fibrils arranged in a β-pleated sheet [4]—a figuration which consequently forms amyloid and not a particular DNA sequence.
The diagnosis is a complement of clinical and histo-pathological signs [5]. Alongside the classical systemic nature of its presence, a tissue biopsy is required which often demonstrates a pink hyaline material [4] and can be noted to take up certain stains, one of which is Congo Red. A positive Congo Red stain is confirmed by a green birefringence seen via a polarizing microscope [4, 6].
Rarely however, amyloidosis present in a localized form. When found in the head and neck, it can involve the orbit, sinuses [5], nasopharynx, oral cavity, salivary gland and larynx [6], the latter of which is most common. There is no clearly defined affected age group or gender predominance [7].
With only 25 cases of sinonasal amyloidosis reported to date [1], little is known of the condition, its aetiology or natural history. Often the lesion occurs as a nodular mass, much like a neoplasm and symptoms occur secondary to its presence or pressure effect. These are commonly related to its location for example, in the upper aero-digestive tract, causing episodic epistaxis, nasal congestion and glue ear [8]—as in the case illustrated above, which can lead to eustachian tube dysfunction.
The management of localized amyloidosis provides considerable difficulty and no definitive treatment has been established [5]. Surgical management can often be futile in that, despite treatment and its slow progressing nature, the condition can persist or recur, with rates of recurrence as high as 50% [1]. This said, there are isolated reports of surgical success [9]. The removal of symptomatic lesions can also be justified.
No evidence to date confirms that surgical removal correlates to improved morbidity and mortality or prevents transformation to systemic amyloidosis. Furthermore, there are no reports to suggest that localized amyloidosis progresses inevitably to its systemic form [5].
The long-term follow-up of this condition however suggests that although the condition is benign, amyloid lesions will progressively grow. If options are to be considered, they are best done early rather than adopting a watch-and-wait strategy.
In summary, we present the rare case of nasal amyloidosis in a 30-year-old woman with fluctuating hearing loss secondary to otitis media with effusion. With respect to the literature, this is the 26th report of a particularly rare condition. As an infrequent entity, it should form part of the differential diagnosis of a nasal mass.
REFERENCES
- 1.Sadeqhipour A, Mirzaie AZ, Mohammadi Sh, Nilipour Y. Primary localized amyloidosis in a child, a rare case report. Int J Pediatr Otorhinolaryngol. 2011;6:310–2. [Google Scholar]
- 2.Panda NK, Saravanan K, Purushotaman GP, Gurunathan RK, Mahesha V. Localised amyloidosis masquerading as nasopharyngeal tumor: a review. Am J Otolaryngol. 2007;28:208–11. doi: 10.1016/j.amjoto.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Tsikoudas A, Martin-Hirsch DP, Woodhead CJ. Primary sinonasal amyloidosis. J Laryngol Otol. 2001;115:55–6. doi: 10.1258/0022215011906803. [DOI] [PubMed] [Google Scholar]
- 4.Stevens A, Lowe J. Pathology. 2nd edn. London: Mosby; 2000. pp. 543–6. [Google Scholar]
- 5.Nakayama T, Otori N, Komori M, Takayanagi H, Moriyama H. Primary localised amyloidosis of the nose. Auris Nasus Larynx. 2012;30:107–9. doi: 10.1016/j.anl.2011.01.022. doi:10.1016/j.anl.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Patel A, Pambuccian S, Maisel R. Nasopharyngeal amyloidosis. Am J Otolaryngol. 2002;23:308–11. doi: 10.1053/ajot.2002.124195. doi:10.1053/ajot.2002.124195. [DOI] [PubMed] [Google Scholar]
- 7.Mufarrij AA, Busaba NY, Zaytoun GM, Gallo GR, Feiner HD. Primary localised amyloidosis of the nose and paranasal sinuses. A case report with immunohistochemical observations and a review of the literature. Am J Surg Pathol. 1990;14:379–83. doi: 10.1097/00000478-199004000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Prasad D, Somayaji GK, Aroor R, Abdulla MN. Primary nasal amyloidosis. Internet J Otorhinolaryngol. 2009;9:2. [Google Scholar]
- 9.Kakani RS, Goldstein AE, Meisher I, Hoffman C. Nodular amyloidosis: case report and literature review. J Cutan Med Surg. 2001;5:101–4. doi: 10.1007/BF02737862. doi:10.1007/BF02737862. [DOI] [PubMed] [Google Scholar]


