Abstract
This report outlines the case of a 3-year-old boy whose initial presentation was that of asymptomatic hypertension (lowest recording 148/90), found at preoperative check prior to stage 2-correction surgery for distal hypospadias. Upon diagnosis of true hypertension, an ultrasound of the child's renal tract showed evidence of marked hydronephrosis and calyceal dilatation. On the background of deteriorating renal function (Urea 25.5 and Creatinine 188), a Micturating Cystourethrogram was performed, demonstrating posterior urethral dilatation. With difficulties controlling blood pressure, the child was transferred to Urology care, where resection of a posterior urethral valve (PUV) was undertaken. Despite this, renal function deteriorated further and re-cystoscopy identified an anterior urethral valve (AUV), which was also resected. Renal function, although improved, remains poor and blood pressure is controlled with two anti-hypertensives. To the publisher's knowledge, the association between hypospadias, PUVs and AUVs is as yet undocumented.
INTRODUCTION
This is a case-report of a 3-year-old boy who was born by lower segment caesarean section following a normal antenatal scan at 42 weeks. He was found to have distal hypospadias at neonatal examination. He underwent stage-1 correction surgery of distal hypospadias at the age of 17 months uneventfully. Aged 18 months, the child was admitted to Hospital due to a viral-induced wheeze. He was found to have asymptomatic high blood pressures ranging between 128/67 and 144/68 and when checked at home over the following days, his blood pressure settled to a maximum of 105/53 and so no further intervention was planned. After a further asymptomatic period, stage-2 correction surgery of distal hypospadias was planned at 3 years of age. Pre-operatively, his blood pressure was found to be 145/97; as such his surgery was cancelled and he was referred to Paediatric clinic for hypertension investigations.
CASE REPORT
Repeated measurements of his blood pressure showed a lowest blood pressure of 148/90. As per the fourth report; any blood pressure above 109/65 for this 3-year-old child meets the criteria for hypertension [1]. On more direct questioning, the mother reported that the child always had a poor urinary stream. An urgent ultrasound of the child's urinary tract showed gross hydronephrosis bilaterally with calyceal dilatation (see Fig. 1).
Figure 1:
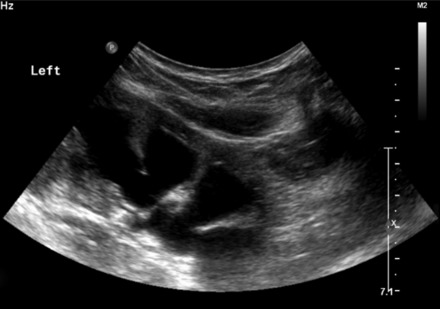
Left renal ultrasound.
Subsequently, a Micturating Cystourethrogram (MCUG) was reported to show a markedly trabeculated bladder and posterior urethral valves (PUVs) (see Fig. 2). The child was also found to have deranged renal function (urea 21.7, cretainine 148). His blood pressure remained high despite the commencement of oral Nifedipine twice daily.
Figure 2:

An urgent MCUG showing a markedly trabeculated bladder with dilatation of the posterior urethra.
With problems controlling blood pressure and worsening renal function (urea 25.5 and creatinine 188), the child was transferred to Urologists, who performed an urgent cystoscopy for posterior urethral valve (PUV) and/or stricture formation as the result of catheterization during stage-1 correction surgery of Hypospadias. Cystoscopy identified a PUV, which was resected. On removal of the catheter, the patient's renal function deteriorated rather than showing the anticipated improvement. Re-cystoscopy was undertaken upon which the identification of an anterior urethral valve (AUV) was made, which was resected. Even on retrospective review of the MCUG, AUV could not be identified; this could possibly be due to the poor urinary flow as a result of the PUV, as well as the catheter in situ obscuring visualization.
After resection of the AUV, the child's renal function improved; however, he still remains in chronic renal failure.
DISCUSSION
The association between Hypospadias and PUVs has been described in literature only twice previously. The association with both an AUV and a PUV is an extremely rare congenital abnormality. To have all in conjunction with hypertension is, as far as the publishers are aware, not previously documented.
PUVs are found exclusively in males and the aetiology is as yet unknown. The belief is that during embryogenesis, at 4 weeks, the Mesonephric duct is usually absorbed into the primitive Cloaca; however, in the development of a PUV, both fuse at 4 weeks, leading to the formation of a membrane rather than a valve.
Anterior urethral valves can occur anywhere along the anterior urethra, distal to the external urinary sphincter. They are 7 times less common than PUVs [2]. The accepted hypothesis is of incomplete fusion of a segment of the urethral plate leading to a prominent semi-lunar fold in the mucous membrane of the urethra.
Progression to end-stage renal failure after resection of valves is not uncommon. PUVs remain the most common cause of renal transplantation in children, representing 1% of those awaiting renal transplantation, with up to 28% of children progressing to end-stage renal failure [3]. The cause of this relates to hypertrophy and hyperplasia of detrusor muscle, which reduces bladder compliance. Bladder emptying then occurs at intra-vesical pressures higher than normal, which is transmitted to the renal collecting system.
This interesting case raises the question of whether to perform renal ultrasound for any child presenting with hypospadias. Certainly conducting an ultrasound for this child would have identified valves earlier and early resection may have prevented deteriorating renal function. Current guidelines state that the incidence of upper urinary tract anomalies does not differ from the general population in those with hypospadias. Only in very severe forms of hypospadias with associated abnormalities (impalpable testis, ambiguous genitalia), is further investigation warranted [4]. There are associations with hypospadias (enlarged prostatic utricle and low grade vesico-ureteric reflux) but these do not normally affect the patient clinically.
Hypertension in the paediatric population is an ever-growing area of paediatrics due to obesity and secondary pathologies. Hypertension is defined as average systolic blood pressure or diastolic blood pressure that is greater than or equal to the 95th percentile for sex, age and height on at least three separate occasions [2]. There is the question as to whether Ambulatory blood pressure monitoring (ABPM), at the age of 18 months, (when high blood pressure was first detected) could have diagnosed true hypertension and lead to early diagnosis of PUV. ABPM is a non-invasive method of measuring blood pressure at frequent intervals over a set period of time; usually 24 h. This apparatus is not readily available in Distirict General Hospitals for Paediatric practice.
Currently, NICE guidelines in the UK for adults recommend that ABPM be used to confirm hypertension in anyone found to have a BP >140/90; there are not, however, paediatric equivalents. ABPM is useful in evaluation of blood pressure levels in children; however, there are limited large data sets and limited information on standardized protocols for validation of monitors used in paediatric patients [5]. By eliminating white coat hypertension and analysing the natural circadian rhythm of the patient in question, it may have been possible to diagnose hypertension in this child as well as monitor response to anti-hypertensives commenced. With the continual rise in paediatric hypertension, it is suggested that further large trial data be collected into the effectiveness of ABPM in paeditric patients in order to diagnose more readily true hypertension.
AUTHORS’ CONTRIBUTION
J.C.: Idea for the article, literature search, draft of initial manuscript, revisions to further versions, preparation of final manuscript and the guarantor. R.M.: Initial guidance for the paper and editing of further manuscripts. Both authors have agreed on the final submitted version.
Conflict of interest statement: None declared.
REFERENCES
- 1.U.S. Department of Health and Human Services. National Institutes of Health, National Heart, Lung, and Blood Institute; 2005. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents; pp. 96–3790. [Google Scholar]
- 2.Lassaad S, Rachida L, Manel B, Randa S, Mongi M, Kais M., et al. Anterior and posterior urethral valves: a rare association. O J Ped. 2011;1:34–6. [Google Scholar]
- 3.Indudhara R, Joseph DB, Pérez LM, Diethelm AG. Renal transplantation in children with posterior urethral valves revisited: a 10-year followup. J Urol. 1998;160(3 Pt 2):1201–3. [PubMed] [Google Scholar]
- 4.Riedmiller H, Androulakakis P, Beurton D, Kocvara R, Gerharz E European Association of Urology. EAU guidelines on paediatric urology. Eur Urol. 2001;40:589–99. doi: 10.1159/000049841. [DOI] [PubMed] [Google Scholar]
- 5.Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–51. doi: 10.1161/HYPERTENSIONAHA.108.190329. [DOI] [PubMed] [Google Scholar]


