Abstract
OBJECTIVES:
Our purpose was to compare the efficacy, complications, success rate, recurrence rate at 1 year, and crossovers of rubber band ligation (RBL) with those of bipolar electrocoagulation (BPEC) treatment for chronically bleeding internal hemorrhoids.
METHODS:
A total of 45 patients of mean age 51.5 years, who had rectal bleeding from grade II or III hemorrhoids and in whom intensive medical therapy failed, were randomized in a prospective study comparing RBL with BPEC. Treatment failure was predefined as continued bleeding, occurrence of a major complication, or failure to reduce the size of all internal hemorrhoidal segments to grade I in ≤ 3 treatments. Patients were followed up for 1 year.
RESULTS:
With similar patients, rectal bleeding and other symptoms were controlled with significantly fewer treatments of RBL than of BPEC (2.3±0.2 vs. 3.8±0.4, P < 0.05), and RBL had a significantly higher success rate (92% vs. 62%, P< 0.05). RBL had more cases of severe pain during treatment (8% vs. 0%, P> 0.05), but significantly fewer failures and crossovers (8% vs. 38%). Symptomatic recurrence at 1 year was 10% RBL and 15% BPEC.
CONCLUSIONS:
For patients with chronically bleeding grade II or III internal hemorrhoids that are unresponsive to medical therapy, safety and complication rates of banding and BPEC were similar. The success rate was significantly higher with RBL than with BPEC. Symptom recurrence rates at 1 year were similar.
INTRODUCTION
Internal hemorrhoids are a common health problem that results in significant morbidity and high economic cost for health care of patients. In 1994, the National Institutes of Health estimated that 10.4 million Americans suffer from hemorrhoids annually, prompting at least 3.5 million physician visits per year at an estimated cost of $500 million (1). Internal hemorrhoids are the most common cause of recurrent hematochezia in ambulatory adults (1 - 4). They are dilated venous plexuses located above the dentate line. As internal hemorrhoids enlarge, the increasing amount of redundant tissue leads to progressive hemorrhoid protrusion below the dentate line. Chronic venous engorgement may eventually lead to bleeding, pain, and other symptoms. The most common symptoms of internal hemorrhoids include rectal bleeding, protrusion, pain, itching, and soiling (5).
For the majority of patients with grade I hemorrhoids and intermittent hemorrhoidal symptoms, medical therapy is appropriate and adequate (5). Surgical hemorrhoidectomy is the most effective and rapid treatment for chronic, symptomatic grades III and IV internal hemorrhoids. However, it is associated with significantly more pain and complications than non-operative techniques (6). Accordingly, surgery is usually recommended in selected patients who fail medical and non-operative therapy; have grade IV hemorrhoids, mixed internal and external hemorrhoids, or concomitant anorectal conditions most amenable to surgery; as well as for those who choose surgery as their preferred treatment (7). Approximately 10–20 percent of patients with symptomatic internal hemorrhoids are currently being treated surgically (5,6,8).
The development of anoscopic and endoscopic devices for the non-operative treatment of internal hemorrhoids allowed physicians, surgeons, and endoscopists to have a wider range of therapeutic options for their patients who failed medical management. Non-operative techniques for ablating hemorrhoids include sclerotherapy, rubber band ligation (RBL), infrared photocoagulation, direct current coagulation, bipolar electrocoagulation (BPEC), and heater probe thermocoagulation. Each of these non-operative therapies can be safely carried out on an outpatient basis. None of the therapies require conscious sedation, and complications are infrequent and usually minor. Endoscopic treatment is most appropriate for grades II and III internal hemorrhoids, but is also indicated when medical treatment of grade I hemorrhoids has failed (5). Sclerotherapy is the oldest form of non-operative treatment. It is recommended as a treatment option for patients with grades I and II hemorrhoidal disease. This technique causes thrombosis of vessels, sclerosis of connective tissue, and shrinkage of the overlying mucosa. Pain is variably reported in 12–70% of patients (9-11). Severe complications, including erectile dysfunction and abscess formation, are rare but may occur (12-15).
Rubber band ligation is now more commonly used than sclerotherapy. Ligation causes focal ischemic necrosis, ulceration, and scarring, which results in fixation of the connective tissue to the rectal wall. Earlier studies have shown that RBL is the most effective non-operative treatment with the fastest obliteration rate and the lowest recurrence rate (16-20). However, more discomfort was reported than with other techniques (21-23).
Bipolar electrocoagulation is one of the most effective coagulation techniques for internal hemorrhoid treatment (4,24,25). It causes coagulation, occlusion, sclerosis, and fibrosis of the internal hemorrhoidal tissue. The procedure is fast and has relatively few complications, which are usually minor (4,24,25). Several studies have compared BPEC with other types of coagulation. In randomized prospective trials comparing BPEC with direct current coagulation, the BPEC treatments were significantly more comfortable, took less time, and resulted in fewer recurrences, but had more complications (4,24). In another randomized prospective comparative study of bipolar coagulation vs. heater probe, the techniques and complications of the two treatments were reported to be similar (25). However, although bipolar coagulation caused less pain during the treatment than the heater probe, it also resulted in a greater number of treatment failures and required more treatment sessions for symptomatic relief (25). In another randomized comparison of infrared coagulation with bipolar coagulation, there was no significant difference in complications or number of treatments required to relieve internal hemorrhoidal symptoms, including bleeding (26).
To our knowledge, there have been no earlier randomized studies reported that compare the relative risks and benefits of RBL vs. bipolar coagulation for the treatment of bleeding from internal hemorrhoids. Our purposes in this randomized prospective study were to assess whether RBL obliterated internal hemorrhoids more rapidly than bipolar coagulation, and whether RBL was as safe and well tolerated as bipolar coagulation for patients with chronic bleeding from internal hemorrhoids. Durability of treatments and recurrence of hemorrhoidal bleeding or other symptoms were also evaluated at 1 year.
METHODS
Specific aims, inclusion, and exclusion criteria
This randomized study of endoscopic RBL vs. anoscopic BPEC for internal hemorrhoids was carried out at the UCLA Medical Center and at the Greater Los Angeles VA Health Care System. This study was approved by IRB committees at each medical center. The specific aims of this study were: (i) to compare the efficacy of endoscopic band ligation vs. BPEC for the treatment of patients with chronic bleeding from grades II and III internal hemorrhoids, (ii) to evaluate the safety and tolerability of the two different treatments, and (iii) to evaluate the durability of treatment effect and recurrence of symptoms at 1 year. All patients enrolled into this study met all of the following inclusion criteria: (i) grade II or III internal hemorrhoids with chronic rectal bleeding, which failed at least 8 weeks of intensive medical therapy, (ii) age over 18 years, (iii) a life expectancy of at least 24 months, and (iv) a signed written informed consent.
The spectrum of internal hemorrhoid bleeding includes severe overt bleeding (bright red blood, with or without bowel movements or with exercise) with anemia, to moderate overt rectal bleeding, to only spotting red blood on toilet tissue or underclothes or passage of blood-tinged mucus. However, all patients randomized in this study had to have severe episodic rectal hemorrhage. The primary goal of the treatments was to eliminate all types of internal hemorrhoid bleeding.
Patients were excluded from the study if any one of the following were present: (i) the patient was uncooperative, unable to sign a written informed consent, or could not return for routine outpatient follow-up, (ii) severe or end-stage comorbid illness, including cirrhosis, portal hypertension, severe renal or respiratory failure, sepsis, active rectal inflammatory bowel disease, and acquired immune deficiency syndrome, (iii) earlier endoscopic (e.g., sclerotherapy, ligation, etc.) or surgical (e.g., hemorrhoidectomy) treatment of hemorrhoids within the past 6 months, (iv) ongoing need for anticoagulation therapy (with warfarin or heparin) or high doses of aspirin and/or non-steroidal anti-inflammatory agents, (v) presence of severe rectal pain, (vi) only grade I or presence of grade IV internal hemorrhoids, (vii) recently thrombosed internal or external hemorrhoids, (viii) anal stricture, fissure, fistula, or abscess, (ix) rectal carcinoma or bleeding distal colonic polyp, (x) rectal varices, (xi) acute or chronic colitis, (xii) rectal prolapse, (xiii) radiation telangiectasia of the rectum, (xiv) coagulopathy defined as a prothrombin time >3 s over control (INR (international normalized ratio) >1.3), or (xv) thrombocytopenia defined as a platelet count < 75,000.
All patients in this study had chronic rectal bleeding from grade II or III internal hemorrhoids documented by diagnostic sigmoidoscopy, or colonoscopy and anoscopy, and they had failed at least 8 weeks of intensive medical therapy with bulk agents (psyllium, Metamucil, or Citrucel), stool softeners (Colace or Surfak), warm water sitz baths, topical creams and/or suppositories with low-dose corticosteroids. Internal hemorrhoid grade was assessed using a slotted anoscope before study enrollment and before all treatments in every patient.
Sample size estimate
A sample size estimate was made on the basis of our earlier experience with RBL and BPEC for the number of treatment sessions to completely control rectal bleeding. This was expected to be a mean of two treatment sessions for RBL vs. four sessions with BPEC. For 80% power, an alpha of 0.05, and two-sided comparison, 14 patients per group were the estimated sample size. To obviate any problems with potential dropouts, inaccuracy of this estimate, and to insure adequate numbers of patients for the analyses of secondary outcomes, we sought to randomize approximately 45 patients, or 21–24 patients per treatment group.
Data collection and analysis
The Data were collected by the investigators and a study coordinator on standard Center for Ulcer Research and Education: Digestive Diseases Research Center (CURE: DDRC) hemostasis study forms. Data were entered into computer files and SAS was used for data management and analyses.
The primary outcome compared between the two treatment groups was the number of treatment sessions required to: (i) relieve the bleeding and (ii) reduce all internal hemorrhoids to grade 0 or I. Secondary outcomes that were analyzed for the two treatments were: (i) treatment complications, and (ii) rate of recurrent bleeding or other internal hemorrhoidal symptoms within 12 months.
The mean and median numbers of sessions were compared between the two groups using t-tests and the non-parametric analog (Wilcoxon rank sum test). Secondary outcomes were compared using these same methods. Time to symptomatic internal hemorrhoid recurrence was examined over a 12-month post-obliteration follow-up period using survival (time-to-event) analysis methods and log-rank tests for comparing the two groups. Background variables, such as sex, age, hemorrhoid grade, and other demographics, were also compared to verify that the randomization was carried out successfully.
Assessment, randomization, and hemorrhoids treatment devices and techniques
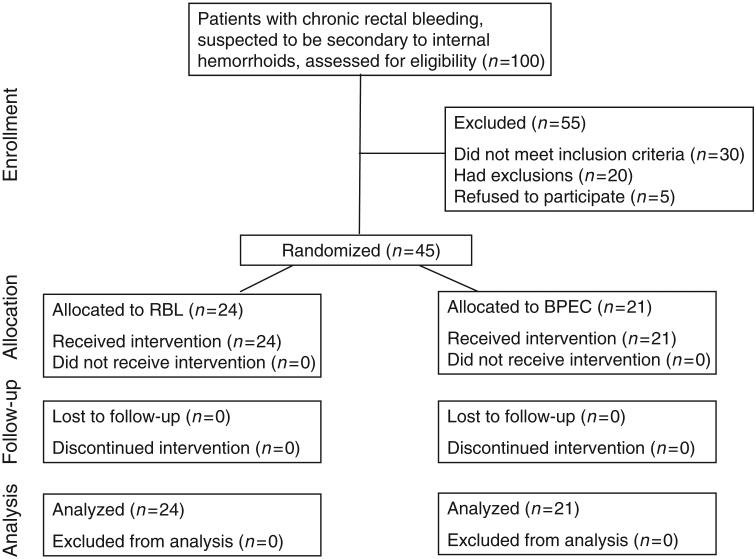
All patients who were referred to investigators for evaluation of rectal bleeding (suspected to be from hemorrhoids by the referral physicians) underwent an initial sigmoidoscopy, or colonoscopy and anoscopy for evaluation of rectal bleeding (refer to Figure 1). Aft er patients met the inclusion and exclusion criteria and signed a written informed consent, the treatment was determined by opening a sealed envelope at the time of the slotted anoscopy, which randomized patients to one of two treatment groups: (i) endoscopic RBL, or (ii) BPEC. Before initiation of the study, a study notebook with sealed opaque envelopes containing cards designating the treatment were prepared for both centers. A computer-generated randomization schedule was used to make up these cards. Two very experienced hemostasis-attending physicians (Jensen DM and Jutabha R) assessed the grade of the hemorrhoids and carried out all the therapeutic endoscopies.
Figure 1.
CONSORT diagram. BPEC, bipolar electrocoagulation probe; RBL, rubber band ligation.
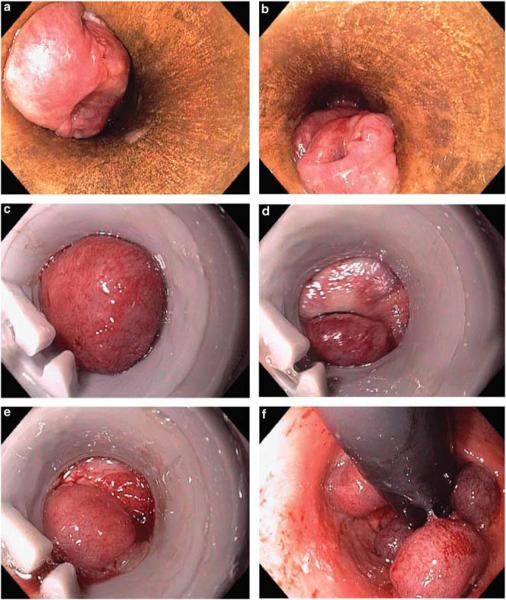
Patients randomized to endoscopic RBL were treated with a diagnostic video endoscope (Pentax 2900, Pentax Medical Co., Montvale, NJ) fitted with a single-shot ligating device (Stiegmann-Goff Ligator, C.R. Bard, Tewksbury, MA) or multi-shot device (Four-shooter, Cook Endoscopy, Winston-Salem, NC). Rubber band ligation was carried out with the endoscope in an end-on and/or retroflexed position similar in technique to esophageal variceal ligation and junctional gastric variceal ligation. The majority of treatments were carried out using the single-shot device. A maximum of four internal hemorrhoids were banded ≥ 1 cm above the dentate line during each session (see Figure 2). Treatments were repeated every 4–6 weeks until relief of bleeding and reduction of all internal hemorrhoids to grade 0 or I.
Figure 2.
Grade II internal hemorrhoids: RBL treatment. (a and b) Slotted-anoscope images of grade II internal hemorrhoids. (c) Endoscopic suction of internal hemorrhoid segment through single-shot ligator on an endoscope. (d) Banding placed end-on, above the dentate line. (e) Internal hemorrhoid segment banded above the dentate line. (f) Four internal hemorrhoids banded—retroflexion after removal of RBL cap.
Patients randomized to bipolar coagulation therapy (previous Circon ACMI, Stamford, CT; new manufacturer now CONMED, Utica, NY) had a maximum of four hemorrhoid segments treate ≥ 1 cm above the dentate line using a rigid probe with 1 s pulses at a 16 watt setting (average of 6–8 pulses per internal hemorrhoid segment) through a slotted anoscope (see Figure 3). Treatments were repeated at 4- to 6 -week intervals until relief of bleeding and reduction of all internal hemorrhoids to grade 0 or I.
Figure 3.
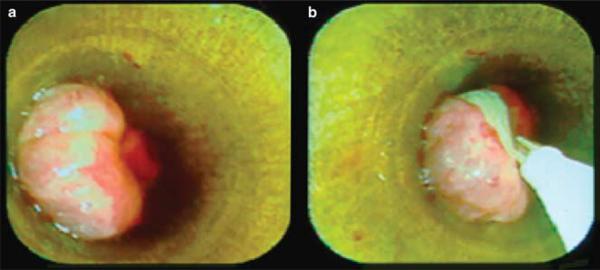
Grade II internal hemorrhoids: BICAP treatment. (a) Grade II internal hemorrhoid segment as shown through a slotted anoscope. (b) Bipolar coagulation probe treatment above the dentate line of a grade II segment.
Pain ratings, follow-up, and success/failure ratings
After each session, patients filled out a questionnaire form using a 10-cm visual analog scale to assess the level of pain associated with the treatment. Patients were instructed to continue intensive medical management with daily warm water sitz baths, stool softeners, fiber supplementation, and hydrocortisone-based creams (RBL) or hydrocortisone suppositories (bipolar group) as needed (for swelling, pressure, mild pain, or bleeding) during the first week aft er these treatments. In our experience, for a week after RBL, pushing a suppository into the anus against the banded internal hemorrhoids may lead to worse pain. Hence, we recommended the cream in RBL patients, instead of suppositories. Patients were also advised to notify the research coordinator if they developed severe rectal pain, bleeding, fevers, or chills.
Study end points were control of all (both severe and on toilet tissue) rectal bleeding, a severe complication or refusal to continue the treatment, and reduction of all internal hemorrhoid segments to grade 0 or I in three or less treatment sessions. These end points were monitored and independently recorded on study forms by a research study coordinator. She first clarified any questions with the patient, primary care physician, or endoscopist.
After achieving the treatment end points, all patients were followed up by the gastroenterologist and/or study coordinator once every 3 months for a total of at least 12 months to assess the recurrence of internal hemorrhoidal symptoms and change in size of internal hemorrhoids. Symptomatic recurrences were treated medically, and if this failed, anoscopic re-treatment was carried out.
Treatment failures for this study were predefined as: (i) a major complication of treatment (e.g., severe rectal pain requiring analgesics or severe bleeding, i.e., fall in baseline hematocrit ≥ 5%; anal stricture; or rectal abscess), or (ii) unresponsiveness to therapy, defined as failure to reduce all internal hemorrhoid segments to grade I or less after three treatment sessions. Patients who failed treatment were taken off the study and given the choice of either crossover and treatment with the other therapy (e.g., bipolar probe or RBL), or treatment with any current medical, endoscopic, or surgical therapies.
RESULTS
Baseline and initial results
From 1997 to May 2000, 100 patients with chronic rectal bleeding suspected to be from internal hemorrhoids by referral physicians were assessed for this study (refer to Figure 1). A total of 55 patients were excluded because they did not meet inclusion criteria (n = 30), had exclusions (n = 20), or refused to participate (n = 5). A total of 45 patients of mean age 51.5 years, with bleeding grade II or III internal hemorrhoids, were enrolled into this prospective randomized trial comparing RBL (24 patients) vs. bipolar coagulation (21 patients). Background variables are shown in Table 1. The two treatment groups were comparable with respect to age (53±3 vs. 50±3 years), gender (54% vs. 71% men), and duration of chronic, recurrent rectal bleeding before randomization (9±2 vs. 8±2 years) for RBL and bipolar coagulation, respectively. Hemorrhoid grade was somewhat more advanced in patients treated with bipolar coagulation (29% grade II, 71% grade III) than with RBL (42% grade II, 56% grade III), although these differences were not statistically significant.
Table 1.
Background variables
| Treatment | RBL | Bipolar coagualation |
|---|---|---|
| Number of patients | 24 | 21 |
| Males | 54% | 71% |
| Mean age (years) | 53±3 | 50±3 |
| Duration of bleeding symptoms before randomization (years) |
9±2 | 8±2 |
| Hemorrhoid grade | ||
| II | 42% | 29% |
| III | 56% | 71% |
RBL, rubber band ligation.
None of the differences were signifi cant.
The patients in the RBL treatment group and bipolar coagulation treatment group had similar symptoms at the time they were randomized, as shown in Table 2. All patients had recurrent rectal bleeding. Concomitant hemorrhoidal prolapse and rectal discomfort occurred in 41–62% of all patients. Perirectal itching and soiling were reported in 13–33% of patients.
Table 2.
Internal hemorrhoidal signs and symptoms before anoscopic treatment
| Treatment | RBL | Bipolar coagualation |
|---|---|---|
| Bleeding | 100% | 100% |
| Prolapse | 50% | 62% |
| Pain or pressure | 41% | 62% |
| Itching | 25% | 33% |
| Soiling | 13% | 14% |
RBL, rubber band ligation.
There were no signifi cant differences in baseline symptom rates.
Treatment results and follow-up
Rubber band ligation was more effective than bipolar coagulation in controlling bleeding and reducing the hemorrhoid size (92% vs. 62%, respectively, P < 0.05) within three treatment sessions (see Table 3). Furthermore, RBL required significantly fewer treatment sessions (2.3±0.2 sessions) than bipolar coagulation therapy (3.8±0.4 sessions) to control the bleeding ( P < 0.05).
Table 3.
Outcomes of both treatments
| RBL | Bipolar coagualation | |
|---|---|---|
| Successful treatment | 92% | 62%a |
| Failures and crossovers | 8% | 38%* |
| Complication of treatment | 4% | 5% |
| Mean treatment sessions to achieve hemostasisa |
2.3±0.2 | 3.8±0.4a |
RBL, rubber band ligation.
Results are as intention to treat and include the additional anoscopic treatments after crossover.
P<0.05.
Eight patients (38%) treated with bipolar coagulation failed to achieve the treatment end points within three sessions because of ongoing rectal bleeding or persistent hemorrhoidal prolapse (grade ≥ II). All of these patients were crossed over to RBL, which controlled bleeding or prolapse after 1–2 treatments. No patients were crossed over from RBL to bipolar coagulation. No patients required surgical hemorrhoidectomy in this study.
The complication rate was low for both treatments. Two patients (8%) treated with RBL and no patients treated with bipolar coagulation had moderately severe rectal pain, requiring oral narcotic analgesics, but not hospitalization (P > 0.05). No one in either group had other severe complications such as perirectal abscess, anal fissure, or rectal stenosis. Mild complications were in similar frequency in both groups (4% in RBL group, 5% in bipolar group). Median pain scores collected from our questionnaire using a 10-cm visual analog scale were not different between the two groups (see Table 4). Only during the second treatment session was the pain score higher in the RBL group than in the bipolar coagulation group.
Table 4.
Median pain score from a 10-cm visual analog scale questionnaire
| RBL | Bipolar coagualation | |
|---|---|---|
| Pain in session 1 | 2 | 2 |
| Pain in session 2 | 3 | 2 |
| Pain in session 3 | 2 | 2 |
RBL, rubber band ligation.
Pain scores as recorded just after treatment on a visual analog scale. Pain was rated from median scores are shown for sessions 1–3:0 (none) to 10 (severe). None of the differences were significant.
Once the bleeding was controlled and the internal hemorrhoids were reduced to grade I or less in size, other symptoms (e.g., shown in Table 2) were also controlled. However, with internal hemorrhoid enlargement, bleeding, prolapse, and pain recurred more oft en than itching or soiling. The rate of recurrent internal hemorrhoid symptoms (rectal bleeding and/or hemorrhoidal prolapse) was low in both treatment groups. At a mean follow-up period of 50 weeks, the respective rates for RBL and bipolar probe pretreatment for recurrent internal hemorrhoidal symptoms or bleeding were 10 and 15%. These symptoms were easily controlled with 1–2 repeat anoscopic treatments in all patients with recurrence.
DISCUSSION
Internal hemorrhoids are very common in adults and are the most frequent cause of self-limited hematochezia in ambulatory adults (1-4). Hemorrhoid bleeding may occur from any grade of internal hemorrhoids, but severe bleeding usually occurs from grade II, III, or IV hemorrhoids. When bleeding is chronic over several years, as in our study, most patients fail medical therapy and require either endoscopic or surgical therapy to control the bleeding. The patients in this study were representative of a subgroup with severe internal hemorrhoidal bleeding who did not respond to a minimum 8 weeks of intensive medical treatment. They had grade II or III hemorrhoids and had suffered from these internal hemorrhoids with recurrent symptoms for 6 to 11 years. By history, patients had received many courses of medical therapy without control of rectal bleeding and pain.
This is the first randomized prospective study comparing RBL treatment with bipolar coagulation. We tested the hypothesis that RBL treatment would be superior to bipolar coagulation treatment for chronically bleeding, large internal hemorrhoids. The rationale for this hypothesis and study was that endoscopic RBL is reported to be easy, fast, and efficient, particularly for control of severe bleeding (27-29). However, we expected higher rates of rectal pain and other complications with RBL, as these have been reported in the past (30-32). In earlier randomized trials, bipolar coagulation was also an effective technique, superior to direct current coagulation (4). In addition, in another randomized study by our group, bipolar probe was less effective than heater probe for hemostasis of chronically bleeding internal hemorrhoids (25). However, no earlier study has compared RBL with bipolar coagulation head to head.
Successful treatment was defined as treatment resulting in control of hematochezia, decrease of all internal hemorrhoid segments to grade I or less, and the absence of severe complications within three treatment sessions. RBL was found to be more efficacious than bipolar coagulation as supported by the fact that 92% of patients who underwent RBL had successful treatment vs. 62% of patients who had bipolar coagulation. The complete resolution of bleeding with RBL after crossover when bipolar coagulation failed helped confirm the superiority of the RBL treatment efficacy.
The significantly fewer number of treatment sessions needed to control hemorrhoidal bleeding with RBL vs. bipolar coagulation (3.8 vs. 2.3, P < 0.05) supports our hypothesis that RBL treats symptomatic grades II and III internal hemorrhoids more rapidly and effectively than bipolar coagulation.
After RBL, a few more patients had moderately severe post-treatment pain (8%-2 patients) than bipolar pain (0%), but the difference was not statistically significant. In addition, somewhat higher pain scores were reported with the second RBL treatment than with second bipolar treatment, but this was not significant. There was no statistically significant difference in complication rates between the RBL group and the bipolar coagulation group. Thus, RBL was as safe and well tolerated as bipolar coagulation for treating patients with chronically bleeding internal hemorrhoids. This was contrary to what has been reported when RBL was compared with other treatments (30-32).
On the basis of these results, the overall efficacy of RBL was significantly higher than bipolar coagulation in patients with grades II and III chronically bleeding internal hemorrhoids. Given that both treatments were equally safe and well tolerated, RBL should be considered as the first-line treatment of patients with grades II and III hemorrhoids that have failed medical management. Bipolar coagulation may be recommended for patients who have had pain or other complications of earlier RBL treatment and who are reluctant to have a repeat RBL treatment because of moderate or severe pain from earlier RBL. It should be emphasized that all patients in this study had relief of their symptoms as a result of medical therapy combined with RBL and/or bipolar coagulation.
Our conclusions from this study are: (i) RBL had a significantly higher success rate and took fewer sessions than bipolar coagulation to relieve symptoms, (ii) The safety and complication rates were similar for RBL and bipolar coagulation, (iii) The recurrence rate of internal hemorrhoidal symptoms after 1 year was low in both the treatment groups, (iv) a few more patients had severe pain with RBL, but the difference was not significant.
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
 Bleeding from internal hemorrhoids is very common.
Bleeding from internal hemorrhoids is very common. Most gastroenterologists do not treat such bleeding.
Most gastroenterologists do not treat such bleeding. However, they use coagulation and other treatments for other gastrointestinal treatments.
However, they use coagulation and other treatments for other gastrointestinal treatments. There are very few randomized controlled studies comparing rubber band ligation (RBL) vs. bipolar electrocoagulation probe (BPEC).
There are very few randomized controlled studies comparing rubber band ligation (RBL) vs. bipolar electrocoagulation probe (BPEC).
WHAT IS NEW HERE
 Patients with chronically bleeding grade II or III hemorrhoids in whom medical therapy failed were studied.
Patients with chronically bleeding grade II or III hemorrhoids in whom medical therapy failed were studied. The success rate was higher with RBL than with BPEC.
The success rate was higher with RBL than with BPEC. Safety and complication rates were similar for RBL and BPEC.
Safety and complication rates were similar for RBL and BPEC. The recurrent hemorrhoidal bleeding rate was 10% with RBL and 15% with BPEC.
The recurrent hemorrhoidal bleeding rate was 10% with RBL and 15% with BPEC.
ACKNOWLEDGMENTS
We thank Mary E. Jensen and Nan Sun for data management, and Oren Goltzer for assisting in the initial preparation of this manuscript.
Financial support: This research study was funded in part by NIH DK41301 (CURE DDRC Human Studies Core), the American Digestive Health Foundation Endoscopy Research Award (Dr Jutabha), NIH-GCRC M01-RR00865, and NIH-IK24DK02650 (Dr Jensen).
Footnotes
CONFLICT OF INTEREST
Guarantor of the article: Dennis M. Jensen, MD.
Specific author contributions: Each author participated in the writing and revisions of the manuscripts.
Potential competing interests: None.
REFERENCES
- 1.Johanson JF. Hemorrhoids In Digestive Diseases in the United States: Epidemiology and Impact. 94-1447. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases US Government Printing Office, NIH Publication; Washington, DC: 1994. pp. 273–98. [Google Scholar]
- 2.Jensen DM, Machicado GA. Colonoscopy for diagnosis and treatment of severe lower gastrointestinal bleeding: routine outcomes and cost analysis. Gastrointest Endosc Clin N Am. 1997;7:477–98. [PubMed] [Google Scholar]
- 3.Savides TJ, Jensen DM. Evaluation and endoscopic treatment of severe lower gastrointestinal bleeding. Tech Gastrointest Endosc. 2003;5:148–54. [Google Scholar]
- 4.Randall GM, Jensen DM, Machicado GA, et al. Prospective randomized comparative study of bipolar vs. direct current electrocoagulation for treatment of bleeding internal hemorrhoids. Gastrointest Endosc. 1994;40:403–10. doi: 10.1016/s0016-5107(94)70201-2. [DOI] [PubMed] [Google Scholar]
- 5.Pfenninger JL. Modern treatments for internal haemorrhoids. BMJ. 1997;314:1211–2. doi: 10.1136/bmj.314.7089.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holzheimer RG. Hemorrhoidectomy: indications and risks. Eur J Med Res. 2004;9:18–36. [PubMed] [Google Scholar]
- 7.Kaidar-Person O, Person B, Wexner SD. Hemorrhoidal disease: A comprehensive review. J Am Coll Surg. 2007;204:102–17. doi: 10.1016/j.jamcollsurg.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 8.Bleday R, Pena JP, Rothenberger DA, et al. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477–81. doi: 10.1007/BF02049406. [DOI] [PubMed] [Google Scholar]
- 9.Walker AJ, Leicester RJ, Nicholls RJ, et al. A prospective study of infrared coagulation, injection and rubber band ligation in the treatment of haemor-rhoids. Int J Colorectal Dis. 1990;5:113–6. doi: 10.1007/BF00298482. [DOI] [PubMed] [Google Scholar]
- 10.Sim AJ, Murie JA, Mackenzie I. Comparison of rubber band ligation and sclerosant injection for first and second degree haemorrhoids-- a prospective clinical trial. Acta Chir Scand. 1981;147:717–20. [PubMed] [Google Scholar]
- 11.Sim AJ, Murie JA, Mackenzie I. Three year follow-up study on the treatment of first and second degree hemorrhoids by sclerosant injection or rubber band ligation. Surg Gynecol Obstet. 1983;157:534–6. [PubMed] [Google Scholar]
- 12.Pilkington SA, Bateman AC, Wombwell S, et al. Anatomical basis for impotence following haemorrhoid sclerotherapy. Ann R Coll Surg Engl. 2000;82:303–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Bullock N. Impotence after sclerotherapy of haemorrhoids: case reports. BMJ. 1997;314:419. doi: 10.1136/bmj.314.7078.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray-Lyon IM, Kirkham JS. Hepatic abscesses complicating injection sclerotherapy of haemorrhoids. Eur J Gastroenterol Hepatol. 2001;13:971–2. doi: 10.1097/00042737-200108000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Ribbans WJ, Radcliffe AG. Retroperitoneal abscess following sclerotherapy for hemorrhoids. Dis Colon Rectum. 1985;28:188–9. doi: 10.1007/BF02554242. [DOI] [PubMed] [Google Scholar]
- 16.Cazemier M, Felt-Bersma RJ, Cuesta MA, et al. Elastic band ligation of hemorrhoids: flexible gastroscope or rigid proctoscope? World J Gastroenterol. 2007;13:585–7. doi: 10.3748/wjg.v13.i4.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg. 1997;40:14–7. [PMC free article] [PubMed] [Google Scholar]
- 18.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum. 1995;38:687–94. doi: 10.1007/BF02048023. [DOI] [PubMed] [Google Scholar]
- 19.Alemdaroglu K, Ulualp KM. Single session ligation treatment of bleeding hemorrhoids. Surg Gynecol Obstet. 1993;177:62–4. [PubMed] [Google Scholar]
- 20.Lee HH, Spencer RJ, Beart RW., Jr Multiple hemorrhoidal bandings in a single session. Dis Colon Rectum. 1994;37:37–41. doi: 10.1007/BF02047212. [DOI] [PubMed] [Google Scholar]
- 21.Marques CF, Nahas SC, Nahas CS, et al. Early results of the treatment of internal hemorrhoid disease by infrared coagulation and elastic banding: a prospective randomized cross-over trial. Tech Coloproctol. 2006;10:312–7. doi: 10.1007/s10151-006-0299-5. [DOI] [PubMed] [Google Scholar]
- 22.Gupta PJ. Infrared coagulation vs. rubber band ligation in early stage hemorrhoids. Braz J Med Biol Res. 2003;36:1433–9. doi: 10.1590/s0100-879x2003001000022. [DOI] [PubMed] [Google Scholar]
- 23.Gupta PJ. Radiofrequency coagulation vs. rubber band ligation in early hemorrhoids: pain vs. gain. Medicina (Kaunas) 2004;40:232–7. [PubMed] [Google Scholar]
- 24.Hinton CP, Morris DL. A randomized trial comparing direct current therapy and bipolar diathermy in the outpatient treatment of third-degree hemorrhoids. Dis Colon Rectum. 1990;33:931–2. doi: 10.1007/BF02139101. [DOI] [PubMed] [Google Scholar]
- 25.Jensen DM, Jutabha R, Machicado GA, et al. Prospective randomized comparative study of bipolar electrocoagulation vs. heater probe for treatment of chronically bleeding internal hemorrhoids. Gastrointest Endosc. 1997;46:435–43. doi: 10.1016/s0016-5107(97)70037-3. [DOI] [PubMed] [Google Scholar]
- 26.Dennison A, Whiston RJ, Rooney S, et al. A randomized comparison of infrared photocoagulation with bipolar diathermy for the outpatient treatment of hemorrhoids. Dis Colon Rectum. 1990;33:32–4. doi: 10.1007/BF02053198. [DOI] [PubMed] [Google Scholar]
- 27.Trowers EA, Ganga U, Rizk R, et al. Endoscopic hemorrhoidal ligation: preliminary clinical experience. Gastrointest Endosc. 1998;48:49–52. doi: 10.1016/s0016-5107(98)70128-2. [DOI] [PubMed] [Google Scholar]
- 28.Wrobleski DE. Rubber band ligation of hemorrhoids. R I Med. 1995;78:172–3. [PubMed] [Google Scholar]
- 29.Fukuda A, Kajiyama T, Arakawa H, et al. Retroflexed endoscopic multiple band ligation of symptomatic internal hemorrhoids. Gastrointest Endosc. 2004;59:380–4. doi: 10.1016/s0016-5107(03)02818-9. [DOI] [PubMed] [Google Scholar]
- 30.Johanson JF, Rimm A. Optimal nonsurgical treatment of hemorrhoids: a comparative analysis of infrared coagulation, rubber band ligation, and injection sclerotherapy. Am J Gastroenterol. 1992;87:1600–6. [PubMed] [Google Scholar]
- 31.Bat L, Melzer E, Koler M, et al. Complications of rubber band ligation of symptomatic internal hemorrhoids. Dis Colon Rectum. 1993;36:287–90. doi: 10.1007/BF02053512. [DOI] [PubMed] [Google Scholar]
- 32.Russell TR, Donohue JH. Hemorrhoidal banding. A warning. Dis Colon Rectum. 1985;28:291–3. doi: 10.1007/BF02560424. [DOI] [PubMed] [Google Scholar]