Abstract
Although cognitive ability is a known predictor of real-world functioning in schizophrenia, there has been an expanded interest in understanding the mechanisms by which it explains real-world functioning in this population. We examined the extent to which functional capacity (i.e., skills necessary to live independently) mediated the relationship between cognitive ability and both observer and self-reported real-world functioning in 138 outpatients with schizophrenia. Functional capacity significantly mediated the relations between cognitive ability and observer rated real world functioning, but not self-reported real world functioning, with small to medium effect sizes observed for all outcomes. The role of cognitive ability in observer vs. self-reported real-world functioning may be explained by different mechanisms.
Keywords: Functioning, Impairment, Cognition, Self-report, Observer report
INTRODUCTION
According to the World Health Organization’s report on the global burden of disease in 2004 (Mathers, Fat, & Boerma, 2008), schizophrenia affects 16.7% of the world’s population, establishing it as one of the main contributors of disability and impairment of quality of life. Marked by positive symptoms such as hallucinations and delusions (i.e., psychosis), negative symptoms such as flat affect, and selective cognitive deficits, individuals with schizophrenia often fail to meet important developmental milestones that are important for independent, self-sufficient living as an adult (Häfner & Nowotny, 1995). As a result, persons with schizophrenia are often dependent on others (e.g., disability services, government institutions, family members) to help them with functions of daily living, not limited to the domains of medication management, self-care and hygiene, financial management, and transportation. These fundamental capabilities, as well as one’s ability to engage in social interactions and participate in and contribute to society (e.g., being employed) will be referred to as real-world functioning in this article.
Cognitive deficits and negative symptoms are two core features of schizophrenia that are believed to confer significant impairment in real-world functioning to those with the illness (Harvey, Green, Keefe, & Velligan, 2004; Liddle, 1987; Tamminga, Buchanan, & Gold, 1998). Fundamentally a neurodevelopmental disorder, schizophrenia is characterized by a pattern of generalized cognitive deficit with more severe deficits in memory and higher-order cognitive ability including attention, working memory, and executive functioning (Dickinson, Ramsey, & Gold, 2007). Basic reading-writing skills, vocabulary, and general information remain relatively spared throughout the course of the disease (Harvey et al., 2000; O’Carroll et al., 1992). As a group, individuals with schizophrenia perform one to three standard deviations below the mean of controls (HCs) across cognitive measures, although it is estimated that approximately 20–25% of schizophrenia cognitive profiles are in the normal range (Palmer, Dawes, & Heaton, 2009). However, even in “cognitively normal” adults with schizophrenia, cognitive ability is not tantamount with adults who are “cognitively unaffected by schizophrenia” (Kremen, Seidman, Faraone, Toomey, & Tsuang, 2000). Accordingly, the consensus is that schizophrenia is a neurobiological disorder comprised of a robust cognitive component (Harrison & Weinberger, 2004; Keshavan, Tandon, Boutros, & Nasrallah, 2008). Global cognitive deficits have been found to predict up to 60 percent of variance in real-world functional outcomes, such as work performance and instrumental activities of daily living (IADLS; Green, Kern, Braff, & Mintz, 2000; Fett et al., 2011; Twamley, Jeste, & Bellack, 2003; Velligan et al., 1997).
While it appears clear that cognition plays a role in the prognosis of schizophrenia, there exists wide heterogeneity of real world functional outcomes even in persons with high cognitive ability. In particular, individuals with high cognitive ability may not achieve a high level of real-world functioning outcomes (e.g., having a job, living independently rather than in a board-and-care facility) as one would expect. Thus, explanatory models are needed to understand how cognitive ability translates to real-world functional outcomes. More recent research has turned to examination of the mechanisms by which cognitive deficits bestow poorer real-world functioning in schizophrenia through the use of mediation models. One mechanism through which cognitive deficits (independent variable; IV) may reduce real-world functioning (dependent variable; DV) in schizophrenia is through increased negative symptom severity (mediator), as indicated by elevated total scale scores for negative symptoms. Results of a meta-analysis showed that negative symptom severity independently accounted for 17.6% of the variance in real-world functioning, as well as partially mediated the relationship between cognitive ability and real-world functioning (Ventura, Hellemann, Thames, Koellner, & Nuechterlein, 2009). Others propose that cognitive ability relates to the ability to acquire the skills necessary to carry out functions of daily living (i.e., functional capacity), which in turn impacts one’s real-world functional outcomes. Bowie, Reichenberg, Patterson, Heaton, and Harvey (2006) used path analyses in an effort to identify the mechanistic properties of the aforementioned relationships, and found functional capacity to mediate the relationship between global cognitive ability and real-world functioning in the domains of interpersonal functioning, work, and participation in community activities. Bowie and colleagues (2008) later used path analyses to show that functional capacity also mediated the relationship between specific cognitive domains and real-world functioning as measured by observer report. It has been demonstrated that the ability of functional capacity measures to predict real-world functioning remains after controlling for demographic variables (Gould, Bowie, & Harvey, 2012). These studies suggest that the severity of cognitive deficits appear to be the primary determinant of impairments in functional capacity, which predict poor real-world functioning as rated by observers.
As the testing of mediation models involving cognitive ability and real world functional outcomes is a relatively new endeavor, it is important to see if these results can be replicated. Moreover, the mediation models tested in these previous studies did not address the issue of using observer-reported real world functional outcomes vs. self-reported real world functional outcomes. While it is largely agreed upon that quality of life (QOL), including real-world outcomes, is a multi-dimensional construct (Test, Greenberg, Long, Brekke, & Burke, 2005), distinctions between self-report and observer reported measures of real-world functional outcomes have recently become an area of focus in schizophrenia research. Self-report versus informant report of wellbeing is a longstanding point of discussion in other clinical populations. In schizophrenia research, there has been considerable debate due to the concerns over the level of insight that an individual with schizophrenia has regarding his or her own real-world functioning. Of the commonly employed methods, self-report has been shown to be minimally correlated with observer-reported real-world functional outcomes in persons with schizophrenia (Sabbag et al., 2012). Thus, many studies rely on observer report by raters to gauge functional outcomes in persons with schizophrenia. Determining the most reliable and accurate sources regarding patients’ real-world functional impairment remains a major challenge in the field of schizophrenia. Thus, the current study attempted to replicate the findings by Bowie and colleagues (2006), as well as compare the validity of observer and self-reported outcomes through supported mediation models (IV=cognitive ability, Mediator=functional capacity, DV= observer/self-reported outcomes). A commonly used technique of testing the validity of self-reported functional outcomes has been to compare and correlate these measures with observer reported outcomes. Disparate findings are interpreted as evidence against the validity of self-report. However, an additional and more rigorous test of the validity in self-reported outcomes would be to see whether or not self-rated measures behave similarly to observer-reported outcomes when they are included in theoretical models. With observer-reported outcomes, we sought to compare the correlations between objective measures of cognitive ability and functional capacity and real-world functional outcomes as rated by family members vs. board-and-care managers vs. case managers to further delineate the possible differences that may exist in observer ratings.
The analyses in this study examine the relationships of cognitive ability, functional capacity, and psychiatric symptoms to multi-dimensional real-world functional outcomes: 1. observer ratings of everyday functional behavior and 2. self-report ratings of functional impairment. Thus, the current study sought to investigate whether or not patients’ cognitive ability is related to self-reported real-world functional impairment, and furthermore, whether or not this relationship is mediated by an objective performance-based measure of functional capacity. We hypothesized that functional capacity would significantly mediate the relationship between a global measure of cognition and informant reported real-world functional outcomes of work skills and participation in community activities based on findings from previous studies. We further hypothesized that functional capacity would not mediate the relationship between cognitive ability and self-reported real-world functional impairment in the domains of work and social interactions.
Novel features of this study include the use of kappa squared (κ2) as an effect size for mediation, which exhibits many favorable properties compared to RM and R2 (Preacher & Kelly, 2011). Additionally, abbreviated cognitive batteries have received considerable attention in the schizophrenia literature as producing comparable results to lengthy assessment batteries in relation to functional capacity and functional outcomes (Harvey, Keefe, Patterson, Heaton, & Bowie, 2009; Keefe et al., 2004; Keefe, Poe, Walker, Kang, & Harvey, 2006). Therefore, we used a brief cognitive battery (Randolph, 1998) in this study to advance the predictive ability of abbreviated cognitive assessment methods.
METHOD
Participants
The sample consisted of 138 middle-aged and older community-dwelling adults with schizophrenia. Participants were enrolled in a randomized clinical trial examining the effectiveness of psychosocial skills-based interventions for improving functioning and all data were procured at baseline. To be eligible, participants were required to be 40 years of age or older and have a DSM-IV chart diagnosis of schizophrenia or schizoaffective disorder that was confirmed by the patient’s psychiatrist. Participants were further required to be psychiatrically stable (e.g., taking antipsychotic medications and not residing in an inpatient setting). Exclusion criteria for the study were: (a) a primary DSM-IV Axis I diagnosis other than schizophrenia or schizoaffective disorder, (b) a co-morbid diagnosis of dementia, (c) were judged to be a serious suicide risk, (d) unable to complete the assessment battery, or (e) currently participating in any other psychosocial intervention or medication research at the time of intake.
The study protocol was approved by the University of California, San Diego Institutional Review Board (IRB), and all participants provided written, informed consent prior to participating. Assessments were completed at Board and Care facilities, clubhouses or recovery-based day programs, and mental health clinics in the San Diego community. Demographic information and psychiatric history (i.e., age of illness onset) was obtained by interview.
Measures
Observer Ratings of Real-World Functioning
Informant ratings of real-world functioning was measured using the Specific Level of Functioning Scale (SLOF; Scheider & Struening, 1983). The SLOF was used to assess real-world functional impairment of the participants, as observed by others. An informant familiar with participants’ skills of everyday living (i.e., caretakers, family members) rated the participant on 43-items across the following six domains: Physical Functioning, Personal Care Skills, Social Appropriateness, Interpersonal Relationships, Work Skills, and Participation in Community Activities. Informants were blind to the other assessment data, and the research assistant who administered the other assessments was blind to the SLOF ratings. Of the 138 informants, 77 were staff members at board and care facilities, and the remaining 61 informants were either case managers or family members familiar with participants’ real-world functioning. Informants were asked to rate their level of familiarity with the participants’ real-world functioning on a Likert-type scale from 1–5, with 3 = fairly well (n = 28), 4 = well (n = 52), and 5 = very well (n = 58). The SLOF has demonstrated excellent interrater reliability, factorial validity, and internal consistency (Schneider & Struening, 1983) and has been recommended as the most valid tool for measuring real-world functioning in schizophrenia (Sabbag et al., 2012). In this study, only the Work Skills, and Participation in Community Activities subscales were examined as the other domains have been shown to exhibit ceiling effects in outpatient samples (Bowie et al., 2008).
Self-reported Ratings of Real-World Functioning
Self-reported real-world functioning was measured using the Work and Social Impairment subscales of the Behavioral Activation for Depression Scale (BADS; Kanter, Mulick, Busch, Berlin, & Martell, 2007). These scales consist of 5 items each. Participants rated the extent to which each statement was true for them during the past week on a 7-point scale from 0 = not at all to 6 = completely. For the Work and Social Impairment subscales, scores range from 0–30, with a higher score indicating greater impairment in that particular domain. An example of an item from the Work Impairment subscale is: “My work/schoolwork/chores/responsibilities suffered because I was not as active as I needed to be.” Because few subjects were employed or attending school, this item was read to the participant as, “My chores/responsibilities suffered because I was not as active as I needed to be.” Moreover, an example item from the Social Impairment subscale is: “I did things to cut myself off from other people.” The BADS has been shown to have acceptable one-week test-retest reliability, acceptable internal consistency, good construct validity, and structural validity (Kanter, Mulick, Busch, Berlin, & Martell, 2007). Finally, the BADS work and social impairment scales has been used to examine self-reported impairment in those with schizophrenia (Cardenas et al., 2012).
Cognitive ability
Global cognitive ability was measured using the Repeatable Battery for the Assessment of Cognitive Status (RBANS; Randolph, 1998). The RBANS is a brief cognitive screening battery that assesses overall current cognitive status as well as current ability in the domains of immediate and delayed memory, attention, visuospatial/constructional skills, and language. This battery consists of twelve subtests assessing both immediate and delayed auditory (unstructured word list and contextual verbal material) and visual memory, basic auditory trace attention, confrontation naming, semantic fluency, copy of a simple geometric figure, judgment of line and angles in space, and psychomotor coding. Scores range from severely impaired to above average with higher scores indicating better performance. The RBANS total score is a standardized score that is calculated by adding age-adjusted scores for the different test domains. This score was used for analyses in the current study. The RBANS has demonstrated excellent reliability and validity for assessing cognitive impairment in patients with schizophrenia (Wilk et al., 2004). The RBANS has been found to be highly correlated (r = 0.79, p < 0.001) with a composite score of global cognition derived from scores on 22 well-established cognitive measures, providing evidence that it is a useful measure of assessing global cognitive ability (Hobart, Golberg, Bartko, & Gold, 1999).
Clinical Symptoms
Symptoms of schizophrenia were measured using the Positive and Negative Syndrome Scale (PANSS; Kay, 1987). For the present study, a single research assistant conducted a structured interview and provided ratings for positive, negative and general symptoms of schizophrenia. The PANSS consists of 30-items which are rated on level of psychopathology from 1 = absent to 7 = extreme, with higher scores indicating greater severity of symptoms. The PANSS has demonstrated good internal consistency and test-retest reliability (Kay, 1987; Mass, Schoemig, Hitschfeld, Wall, & Haasen, 2000). For the present study, the total positive and negative domain scores were used.
Functional Capacity
The UCSD Performance-Based Skills Assessment (UPSA; Patterson, Goldman, McKibbin, Hughs, & Jeste, 2001) was used to assess functional capacity for everyday tasks. Developed for use in people with schizophrenia and other serious mental illnesses, the UPSA is a role-play test of functional capacity. The UPSA uses real-world props (e.g., telephone, bus schedule) to assess skills/abilities in the following five domains which have been deemed important elements for independent living: planning/organization, finances, communication skills, transportation, and household chores (Patterson, Goldman, McKibbin, Hughs, & Jeste, 2001). Scores range from 0–100, with lower scores indicating greater difficulties with the ability to live independently in the community. Interrater reliability is considered good (Harvey, Velligan, & Bellack, 2007; Patterson et al., 2001).
Depressive Symptoms
Depressive symptoms were assessed using the Calgary Depression Scale for Schizophrenia (CDSS; Addington & Addington, 1990). A nine-item structured interview measure that has demonstrated good inter-rater reliability and validity, the CDSS is able to assess depressive symptoms independent of other symptoms of psychopathology, (i.e., Beck Depression Inventory, Hamilton Rating Scale for Depression; Addington, Addington, Maticka-Tyndale, & Joyce, 1992; Kim et al., 2006). Participants’ symptoms are rated on a four-point scale from ‘0’ = absent to ‘3’ = severe on each item and scores are summed, with higher scores indicative of greater depressive symptoms.
Data Analysis
SPSS Statistics Version 19 was used to carry out all analyses. To analyze the relationships between the study variables, we first conducted Pearson correlations. Multiple regression analyses were used to test our hypothesis that functional capacity (measured by the UPSA) mediates the associations of cognitive ability [independent variable (IV), measured by the RBANS] to real-world functioning [dependent variable (DV), measured by subscales of the SLOF and BADS], with PANSS positive, PANSS negative, depressive symptoms, and age included as covariates in all analyses. Mediation was tested using the Sobel test (Preacher & Hayes, 2004), which examines the null hypothesis that there will be no difference between the total effect of the regression model (c path: IV to DV) and the direct effect of the model (c’ path: IV and DV mediated by UPSA). In this way, the significance of the indirect effect of the mediator is evaluated. It must be noted that results from the Sobel test can be misleading if data are non-normal, which is often the case (Preacher & Hayes, 2004). As recommended by MacKinnon, Lockwood, Hoffman, West, and Sheets (2002), the current study used 5,000 bootstrapping samples to obtain a sampling distribution for the indirect effect and included confidence intervals derived from this method. We used the SPSS macro for bootstrapping mediated effects provided by Preacher and Hayes (2004) to conduct these analyses. Additionally, effect size of mediation was calculated using the κ2 statistic as described and recommended by Preacher and Kelly (2004).κ2 represents the magnitude of the indirect effect relative to the maximum possible indirect effect. Unlike R2 and RM values reported by previous mediation studies, an advantage of using κ2 includes the fact that it can be accurately interpreted as a proportion, and that it is bounded between 0 and 1. While Preacher and Kelly (2011) hesitate to recommend a specific method of interpreting κ2, they ultimately argue that values for κ2 can be interpreted similarly to the squared correlation coefficient, with small, medium, and large effects being represented by Cohen’s values of .01, .09, and .25, respectively. Because of these properties, the κ2 is arguably a more useful mediation effect size statistic for future meta-analyses and literature reviews that are interested in studying the mechanisms through which cognitive deficits lead to impairments in real-world functional outcomes in schizophrenia.
RESULTS
Summary statistics of participant demographics and performance on measures are displayed in Table 1. Table 2 displays the zero-order correlations between primary study variables. As can be seen in Table 2, the UPSA was correlated with all study variables. To account for the effects of demographic variables on both observer-reported and self-reported real-world functional outcomes, we included sex and race as covariates in alternate models and found that they did not alter the primary findings.
Table 1.
Summary of Sample Characteristics
| Variable | N=138 |
|---|---|
| Age (years), M (SD) | 50.9 (6.9) |
| Race, n (%) | |
| Caucasian-not Hispanic/Latino | 82 (59.4%) |
| African American | 25 (18.1%) |
| Caucasian-Hispanic/Latino | 19 (13.8%) |
| American Indian | 3 (2.2%) |
| Asian/Pacific Islander | 4 (2.9%) |
| Other | 5 (3.6%) |
| Male, n (%) | 93 (67.4%) |
| Measures | |
| Schizoaffective Disorder, n (%) | 22 (15.9%) |
| RBANS Total, M (SD) | 63.9 (12.7) |
| UPSA | 65.6 (17.0) |
| SLOF Work Skills | 22.5 (5.1) |
| SLOF Activities | 46.3 (8.5) |
| BADS Work | 10.6 (6.5) |
| BADS Social | 11.6 (7.4) |
Table 2.
Correlations of Independent Variables with Outcome Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. RBANS | -- | ||||||||
| 2. UPSA | .63* | -- | |||||||
| 3. BADS Work | −.30* | −.33* | -- | ||||||
| 4. BADS Social Impairment | −.36* | −.39* | .67* | -- | |||||
| 5. SLOF Work | .15 | .26* | −.12 | .01 | -- | ||||
| 6. SLOF Activities | .26* | .34* | −.19* | −.14 | .61* | -- | |||
| 7. CDSS | .05 | .05 | .30* | .34* | .03 | .11 | -- | ||
| 8. PANSS Positive | −.15 | −.17 | .27* | .37* | .05 | .05 | .27* | -- | |
| 9. PANSS Negative | −.26* | −.40* | .30* | .35* | −.19* | −.15 | .14 | .31* | -- |
Note:
p < .05. RBANS= Repeatable Battery for the Assessment of Cognitive Status, UPSA=UCSD Performance-based Skills Assessment, SLOF=Specific Level of Functioning, BADS= Behavioral Activation for Depression Scale
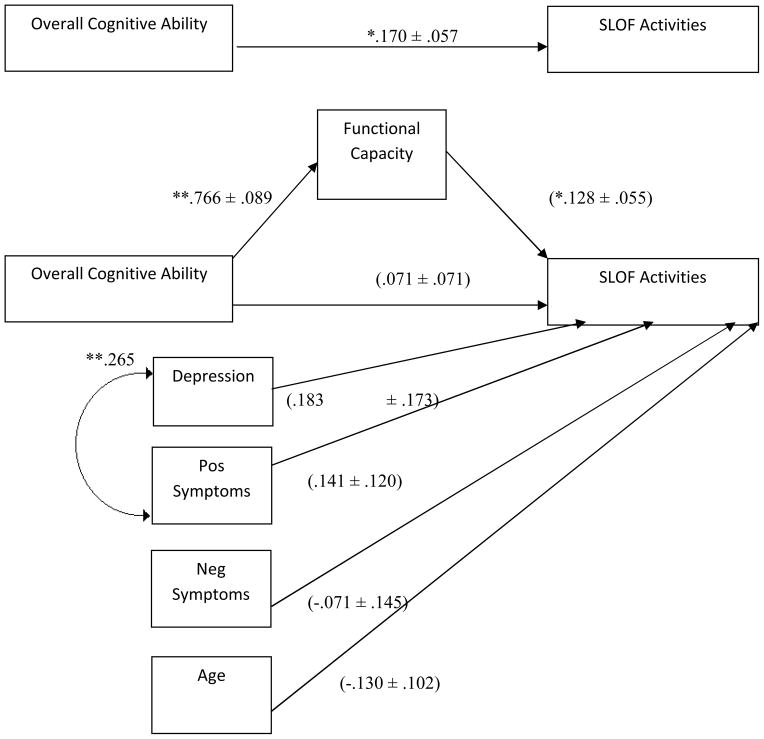
UPSA as a mediator between Overall Cognitive Ability and Observer Rated Real-world Functioning
Results for all tests of mediation are presented in Table 3. Figure 1 displays the a, b, c, and c′ paths involved in the mediation model being tested. The c path shows the predictive relationship of the IV (RBANS) on the DV (SLOF Activities), as tested by a simple regression. The a path displays the predictive relationship of the IV (RBANS) on the mediator (UPSA), as tested by a simple regression. The b path displays the predictive relationship of the mediator (UPSA) on the DV (SLOF Activities), as tested by a simple regression. Last, the c′ path is of main interest and displays the relationship between the IV (RBANS) and DV (SLOF Activities) after removing the variance accounted for by the mediator (UPSA), as tested by a multiple regression that includes both the IV (RBANS) and mediator (UPSA). For our first model, the bootstrapping 95% confidence interval [.018, .206] revealed that the UPSA significantly mediated the relationship between the RBANS (cognitive ability) and SLOF Activities (observer rated participation in community activities). As indicated by κ2 = .118, the strength of this effect was in the medium range. Notably, the significant relationship between the RBANS and SLOF Activities in the c path (b = .170, t(131) = 2.953, p < .05) became nonsignificant in the c′ path (b = −.004, t(131) = 1.009, p = .936) after including the UPSA in the model. Path a indicated that the RBANS significantly predicts performance on the UPSA, and path b indicated that performance on the UPSA significantly predicted informant rated real-world functioning in participation in community activities (SLOF Activities). The relations of clinical symptoms (PANSS Negative, PANSS Positive, and CDSS) and age to real-world functioning were accounted first, and then the regression model tested if the UPSA mediated the relationship between the RBANS and functioning. We found that neither age nor symptoms significantly predicted participation in community activities. The overall fit of the model was significant with F(6, 131) = 3.794, p = .002 and R2 = .148.
Table 3.
Summary of Mediation Model Tests
| IV | Mediator | DV | b | SE | Bootstrap 95% CI | K2 | |
|---|---|---|---|---|---|---|---|
| RBANS | UPSA | SLOF ACTIVITIES* | .103 | .043 | .026 | .196 | 0.118 |
| RBANS | UPSA | SLOF WORK SKILLS* | .053 | .027 | .004 | .111 | 0.103 |
| RBANS | UPSA | BADS SOCIAL IMPAIRMENT | −.064 | .037 | −.139 | .007 | 0.082 |
| RBANS | UPSA | BADS WORK IMPAIRMENT | −.051 | .036 | −.126 | .013 | 0.083 |
Note. IV = Independent Variable. DV = Dependent Variable. b = Unstandardized Regression Coefficient. SE = Standard Error. CI = Confidence Interval. K2= Kappa Squared Effect Size
p < .05
Figure 1. Prediction of Observer Reported Participation Community Activities.
Note. Values depicted on single-headed paths are unstandardized regression coefficients and their standard errors: B ±. Values on double-headed paths are zero-order correlation coefficients. Values in parentheses are unstandardized coefficients for the full model. ** indicates p<.01. * indicates p<.05.
Exploratory analyses were conducted to examine if the relationships between cognitive ability and real world functioning in the domains of participation in community activities and work skills vary depending on informants’ familiarity with the patient’s functioning. We performed r to z transformations and tested for significant differences in correlations between cognitive ability and participation in community activities in raters who rated their familiarity as a “3” = fairly well, “4” = well, and “5” = very well. The correlations between cognitive ability and observer reported participation in community activities were: r(26) = .40 for score = 3, r(50) = .24 for score = 4, r(56) = .24 for score = 5. All p-values were greater than .46, indicating that there were no significant differences found in the correlations based on familiarity with the participant. Identical results were found for the correlation between cognitive ability and observer reported work skills. Thus, we concluded that level of familiarity with the participant did not influence the correlation between cognitive ability and real world functioning in participant in community activities or work skills.
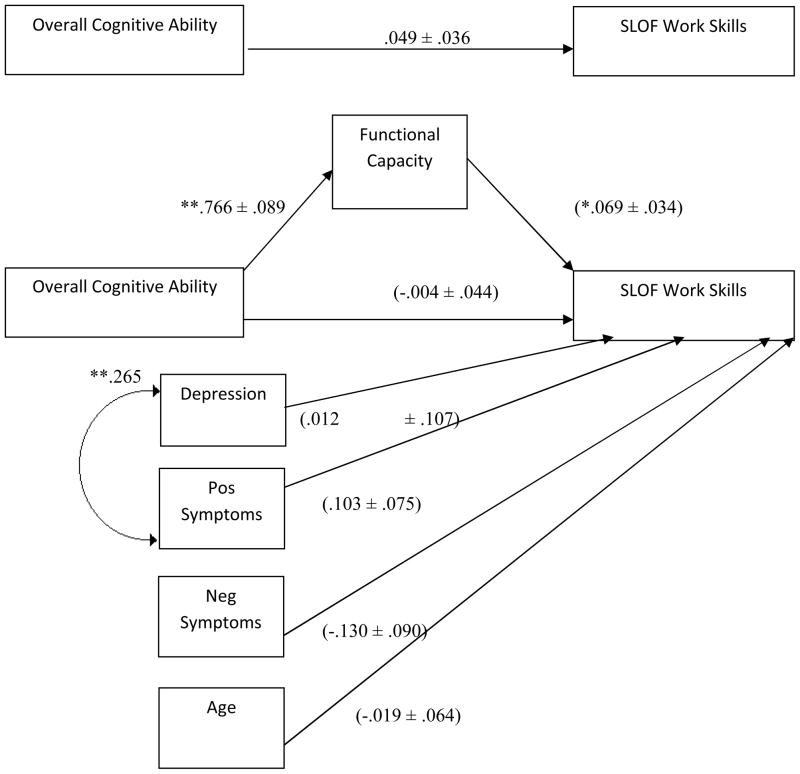
Also consistent with our hypotheses, the bootstrapping 95% confidence interval [.001, .110] revealed that the UPSA significantly mediated the relationship between the overall cognitive ability (RBANS) and observer reported real-world functioning in work (SLOF Work Skills), with a medium effect size of κ2= .103. It was found that the RBANS did not independently predict SLOF Work Skills, as indicated by the c path (b = .049, t(131) = 1.383, p = .169). Moreover, the c′ path showed no significant relationship between the RBANS and SLOF Work Skills after controlling for the UPSA (b = −.004, t(131) = −.081, p = .936). Path a indicated that the RBANS significantly predicts performance on the UPSA, and path b indicated that performance on the UPSA significantly predicted informant rated real-world functioning in work skills (SLOF Work Skills). Again, age and symptoms did not significantly predict SLOF Work Skills after the model partialed out the mediated effects (see Figure 2). The overall fit of the model was significant with F(6, 131) = 2.22, p = .045 and R2 = .092.
Figure 2. Prediction of Observer Reported Work Skills.
Note. Values depicted on single-headed paths are unstandardized regression coefficients and their standard errors: B ±. Values on double-headed paths are zero-order correlation coefficients. Values in parentheses are unstandardized coefficients for the full model. ** indicates p<.01. * indicates p<.05.
UPSA as Mediator of Overall Cognitive Ability and Self-reported Impairment
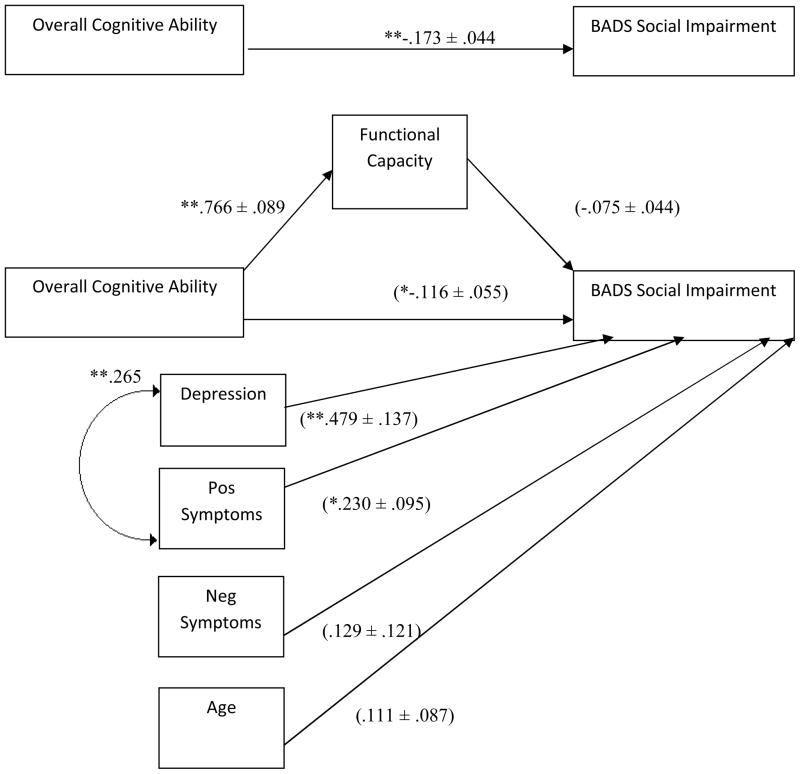
Contrary to our hypotheses, the bootstrapping results indicated that the UPSA did not significantly mediate the relationship between overall cognitive ability (RBANS) and self-reported real-world social impairment (BADS Social Impairment), and the effect size was in the small range: κ2= .082. Figure 3 displays the model that was tested. Path c indicated that the RBANS significantly predicted BADS Social Impairment (b = −.173, t(122) = −3.885, p < .001). Moreover, path c′ indicated that the RBANS significantly predicted BADS Social Impairment even after accounting for the effect of the UPSA (b = −.116, t(122) = −2.088, p = .039). Path a indicated that the RBANS significantly predicted performance on the UPSA, but path b indicated that performance on the UPSA did not significantly predict self-rated real-world social impairment (BADS Social Impairment). PANSS Positive Symptoms and CDSS significantly predicted BADS Social Impairment after accounting for the relationships with the UPSA and RBANS, with greater symptoms predicting more severe impairment. The overall model fit for BADS Work Impairment was significant for BADS Social Impairment, with F(6, 122) = 11.120, p < .001 and R2 = .354.
Figure 3. Prediction of Self-Reported Social Impairment.
Note. Values depicted on single-headed paths are unstandardized regression coefficients and their standard errors: B ±. Values on double-headed paths are zero-order correlation coefficients. Values in parentheses are unstandardized coefficients for the full model. ** indicates p<.01. * indicates p<.05.
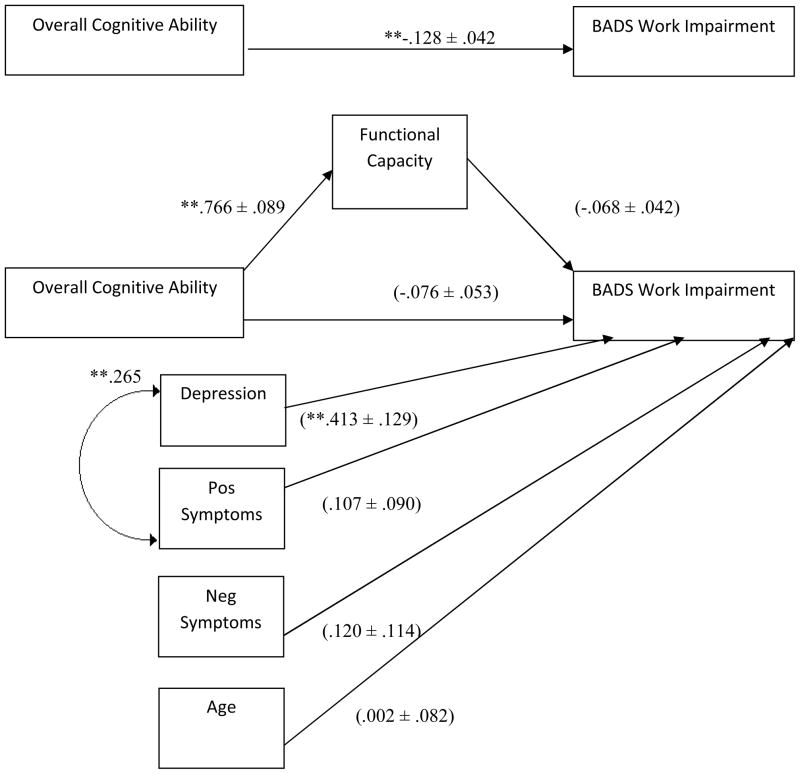
Bootstrapping results indicated that the UPSA did not significantly mediate the relationship between overall cognitive ability (RBANS) and self-reported real-world work impairment (BADS Work Impairment), and the effect size was in the small range: κ2 = .083. Figure 4 displays the model that was tested. Performance on the RBANS significantly predicted BADS Work Impairment independently in the c path (b = −.128, t(123) = −3.031, p = .003). However, after including the UPSA into the model, the relationship between the RBANS and self-reported work impairment became nonsignificant as illustrated in the c′ path (b = −.076, t(123) = −1.447, p = .150). Path a indicated that the RBANS significantly predicted performance on the UPSA, but path b indicated that performance on the UPSA did not significantly predict self-rated real-world work impairment (BADS Work Impairment). Depressive symptoms (CDSS) significantly predicted BADS Social Impairment after accounting for the relationships with the UPSA and RBANS, with greater symptoms predicting more severe impairment. The overall model fit for BADS Work Impairment was significant with F(6, 123) = 6.55, p < .001 and R2 = .242.
Figure 4. Prediction of Self- Reported Work Impairment.
Note. Values depicted on single-headed paths are unstandardized regression coefficients and their standard errors: B ±. Values on double-headed paths are zero-order correlation coefficients. Values in parentheses are unstandardized coefficients for the full model. ** indicates p<.01. * indicates p<.05.
DISCUSSION
We first tested the meditational role of functional capacity in the relationship between overall cognitive ability and observer ratings of behavior in the domains of work skills and participation in community activities. The findings of the current study replicated those of Bowie and colleagues (2006), showing that functional capacity partially mediates the relationship between cognitive ability and observer reported real-world functioning in work skills and community participation. It appears as though cognitive deficits may be a precursor to poor acquisition of functional capacity (i.e., what a person is capable of doing) which subsequently affects real-world functioning (i.e., what a person actually does). Conversely, some individuals with schizophrenia have cognitive abilities in the normal range and still exhibit deficits in real-world functioning similar to cognitively impaired individuals (Keefe, Eesley, & Poe, 2005). Establishing causality of the models tested will require future study utilizing longitudinal data to establish the chronology of cognitive deficits, functional capacity deficits, and problems with real-world functioning.
In regard to the possible mediation of the relationship between cognitive ability and self-reported real-world work and social impairment, as measured by the BADS, we found no significant mediation using bootstrapping methods. This finding is consistent with the notion that self-reported outcomes in persons with schizophrenia may not be valid indicators of one’s level of real-world functioning. Moreover, the effect sizes of mediation appeared much larger when observer-rated functional outcomes were used as the dependent variable (K2 = .118) than when self-reported functional outcomes were used as the dependent variable (K2 = .083). Again, this is evidence against the validity of self-report as a measure of real-world functional outcomes.
In terms of how comparable the self-reported and observer-reported outcome measures were, we found that SLOF Work (observer-reported functional outcomes) was not significantly correlated with the self-reported functional outcomes of BADS Work. If these measures were capturing a similar construct, we would expect a significant negative correlation. However, the lack of relationship is evidence against the convergent validity of the self-report measure BADS in capturing real-world functioning in persons with schizophrenia. Moreover, we found that the observer-reported SLOF Activities was significantly negatively correlated with self-reported BADS Work Impairment (self-reported functional outcomes). This relationship provides some evidence of the validity of the self-reported BADS Work Impairment scale for measuring one’s success in engaging in occupation-related activities.
Given these results, it is likely that the SLOF and BADS are capturing different constructs (Campbell & Fiske, 1959; Heeler & Ray, 1972). Self-reported real-world functional outcomes are impacted by the patients’ cognitive ability, level of insight, feelings of self-efficacy, and other factors that will affect the accuracy of their perceived level of impairment. Perhaps patients’ perceptions of how well they are functioning in real-world domains may be more representative of the subjective experience of schizophrenia rather than their cognitive ability, functional capacity, and others’ perceptions of their level of real-world functioning (Fitzgerald et al., 2001).
In further support of the need to distinguish between pathways for arriving at self-reported and observer-reported real-world functioning, we found that level of depression significantly predicted self-reported social impairment and work impairment, but not informant-reported work skills or involvement in community activities. These results are consistent with the assertion that self-reported outcome measures are related to subjective experiences of schizophrenia whereas observer-reported outcome measures are more related to objective measures of functioning (Bowie et al., 2007; McKibbin, Brekke, Sires, Jeste, & Patterson, 2004). Our study also found that negative symptom severity did not significantly predict poor observer reported real-world functioning in work skills and participation in community activities after accounting for the effects of cognitive ability and functional capacity. However, increased depression was significantly associated with decreased self-reported real-world functioning in the social and work domains. It is likely that shared method variance (i.e., the fact that both these measures are self-reported) contributed to this finding, but it is also possible that these findings suggest that depression and positive symptoms may have more of an impact on the self-reported experience and impairment of schizophrenia, but not observer reports and objective outcomes.
Limitations
A limitation of the current study includes the fact that it yields modest findings, which may be a result of the choice to test models that relate objective measures of functioning (e.g., cognitive ability and functional capacity) to self-reported and observer-reported outcomes (e.g., BADS and SLOF, respectively). Mediation models only partially account for the variability in observer-reported real-world outcomes. Self-reported outcomes may be biased by lack of insight and severity of psychosis. Furthermore, observer-reported outcomes may be impacted by environmental obstacles, social support received by the participant, and other determinants of observable real-world outcomes that were not accounted for in this study. Another limitation of the current study is the sparseness of information on the informants and how informant characteristics may impact ratings of participants’ levels of real-world functioning.
Future studies may benefit from testing alternate models for mediation using variables that have been shown to be related to the subjective experience of schizophrenia, comparing observer and self-reported ratings on the same measure, taking into account observers’ familiarity with participants, and examining the individual observer characteristics that may impact their ratings of participants’ level of real-world functioning. Additionally, the variance observed in cognitive ability may be affected by exclusion of individuals who did not complete the battery. These individuals may comprise a subgroup of schizophrenia with severe cognitive deficits that may be informative for understanding the illness and differential outcomes. Moreover, our study may be limited by the fact that self-reported real-world functioning measures are impacted by the participants’ level of insight, as well as the fact that observer ratings of real-world functioning may vary based on the observer’s familiarity with the patient, biases, caregiver burden, and time spent with the patient. Despite these limitations, our study further suggests that self-reported functional outcomes by patients with schizophrenia do not seem to validly capture how they are doing in the real world. Predicting real-world functioning in individuals with schizophrenia is a complex issue that cannot be explained by overall cognitive ability alone, and patient’s self-perceptions of how they are doing may be better understood by more subjective measures that capture the experience of living with schizophrenia rather measures of objective ability.
Conclusions
Both objective measures of functioning (e.g., SLOF) and subject measures of functioning (e.g., BADS) may be crucial to understanding impairment in schizophrenia. Overall, the results of this study indicate that the relationship between cognitive deficits and informant rated measures of real-world functional outcomes can be explained by objective measures such as functional capacity. Additionally, it may be that subjective self-reported outcomes may be better predicted by and mediated by measures that capture the subjective experience of schizophrenia such as insight and positive and depressive symptoms. Because schizophrenia is a heterogeneous disease, characterized by wide individual variability in both symptoms and functioning, it is imperative to understand the mechanisms that determine both the self-reported experience of the disease as well as observer-rated outcomes. It is recommended that future studies also report the κ2 mediation effect size for each mediation model, which may be useful for meta-analyses. Understanding the variables that account for a significant proportion of variance in both self-reported and informant reported real-world functioning may allow for the development of more effective interventions for schizophrenia.
Acknowledgments
This research was supported by the the National Institute of Mental Health (NIMH) through award R01 MH084967.
Footnotes
Conflict of interest
The authors affirm that there exists no conflict of interest in writing this article.
References
- Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. Journal of Abnormal Psychology; Journal of Abnormal Psychology. 1978;87(1):49. [PubMed] [Google Scholar]
- Addington D, Addington J. A depression rating scale for schizophrenics. Schizophrenia Research. 1990;3:247–251. doi: 10.1016/0920-9964(90)90005-r. Retrieved from http://dx.doi.org/10.1016/0920-9964(90)90005-R. [DOI] [PubMed] [Google Scholar]
- Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophrenia Research. 1992;6:201–208. doi: 10.1016/0920-9964(92)90003-n. Retrieved from http://dx.doi.org/10.1016/0920-9964(92)90003-N. [DOI] [PubMed] [Google Scholar]
- Borison RL, Arvanitis LA, Milier BG. ICI 204,636, an atypical antipsychotic: Efficacy and safety in a multicenter, placebo-controlled trial in patients with schizophrenia. Journal of Clinical Psychopharmacology. 1996;16(2):158–169. doi: 10.1097/00004714-199604000-00008. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, Harvey PD. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biological Psychiatry. 2008;63(5):505–511. doi: 10.1016/j.biopsych.2007.05.022. Retrived from http://dx.doi.org/10.1016%2Fj.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functioning performance in Schizophrenia: Correlations with cognition, functional capacity, and symptoms. The American Journal of Psychiatry. 2006;163(3):418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Twamley EW, Anderson H, Halpern B, Patterson TL, Harvey PD. Self-assessment of functional status in schizophrenia. Journal of Psychiatric Research. 2007;41(12):1012–1018. doi: 10.1016/j.jpsychires.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin. 1959;56(2):81–105. doi: 10.1037/h0046016. [DOI] [PubMed] [Google Scholar]
- Cardenas V, Abel S, Bowie C, Tiznado D, Depp CA, Patterson TL, Mausbach BT. When functional capacity and real-world functioning converge: The role of self-efficacy. Schizophrenia Bulletin. 2012 doi: 10.1093/schbul/sbs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: A meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Archives of General Psychiatry. 2007;64(5):532–542. doi: 10.1001/archpsyc.64.5.532. [DOI] [PubMed] [Google Scholar]
- Fett AKJ, Viechtbauer W, Dominguez MG, Penn DL, Van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: A meta-analysis. Neuroscience & Biobehavioral Reviews. 2011;35(3):573–588. doi: 10.1016/j.neubiorev.2010.07.001. Retrieved from http://dx.doi.org/10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Fitzgerald PB, Williams C, Corteling N, Filia S, Brewer K, Adams A, Kulkarni J. Subject and observer-rated quality of life in schizophrenia. Acta Psychiatrica Scandinavica. 2001;103(5):387–392. doi: 10.1034/j.1600-0447.2001.00254.x. [DOI] [PubMed] [Google Scholar]
- Gould F, Bowie CR, Harvey PD. The influence of demographic factors on functional capacity and everyday functional outcomes in schizophrenia. Journal of Clinical and Experimental Neuropsychology. 2012;34(5):467–475. doi: 10.1080/13803395.2011.651102. [DOI] [PubMed] [Google Scholar]
- Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry. 1996;153(3):321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the ‘right stuff’? Schizophrenia Bulletin. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Häfner H, Nowotny B. Epidemiology of early-onset schizophrenia. European archives of psychiatry and clinical neuroscience. 1995;245(2):80–92. doi: 10.1007/BF02190734. [DOI] [PubMed] [Google Scholar]
- Harrison P, Weinberger D. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Molecular Psychiatry. 2004;10(1):40–68. doi: 10.1038/sj.mp.4001558. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Green MF, Keefe RSE, Velligan DI. Cognitive functioning in schizophrenia: A consensus statement on its role in the definition and evaluation of effective treatments for the illness. Journal of Clinical Psychiatry. 2004;65(3):361–372. doi: 10.4088/JCP.v65n0312. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Keefe RSE, Patterson TL, Heaton RK, Bowie CR. Abbreviated neuropsychological assessment in schizophrenia: Prediction of different aspects of outcome. Journal of Clinical and Experimental Neuropsychology. 2009;31(4):462–471. doi: 10.1080/13803390802251386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Moriarty PJ, Friedman JI, White L, Parrella M, Mohs RC, Davis KL. Differential preservation of cognitive functions in geriatric patients with lifelong chronic schizophrenia: Less impairment in reading compared with other skill areas. Biological Psychiatry. 2000;47(11):962–968. doi: 10.1016/s0006-3223(00)00245-6. Retrieved from http://dx.doi.org.libproxy.sdsu.edu/10.1016/S00063223(00)00245-6. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Velligan DI, Bellack AS. Performance-based measures of functional skills: Usefulness in clinical treatment studies. Schizophrenia Bulletin. 2007;33(5):1138–1148. doi: 10.1093/schbul/sbm040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeler RM, Ray ML. Measure validation in marketing. Journal of Marketing Research. 1972:361–370. [Google Scholar]
- Hobart MP, Golberg R, Bartko JJ, Gold JM. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia, II: Convergent/discriminant validity and diagnostic group comparisons. The American Journal of Psychiatry. 1999;156(12):1951–1957. doi: 10.1176/ajp.156.12.1951. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The Behavioral Activation for Depression Scale (BADS): Psychometric properties and factor structure. Journal of Psychopathology and Behavioral Assessment. 2007;29(3):191–202. doi: 10.1007/s10862-006-9038-5. [DOI] [Google Scholar]
- Kay S, Fiszbein A, Lewis OA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biological Psychiatry. 2005;57(6):688–691. doi: 10.1016/j.biopsych.2005.01.003. http://dx.doi.org/10.1016/j.biopsych.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophrenia Research. 2004;68(2):283–297. doi: 10.1016/j.schres.2003.09.011. [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Poe M, Walker TM, Kang JW, Harvey PD. The Schizophrenia Cognition Rating Scale: An interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. American Journal of Psychiatry. 2006;163(3):426–432. doi: 10.1176/appi.ajp.163.3.426. [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Tandon R, Boutros NN, Nasrallah HA. Schizophrenia,“just the facts”: What we know in 2008: Part 3: Neurobiology. Schizophrenia Research. 2008;106(2):89–107. doi: 10.1016/j.schres.2008.07.020. [DOI] [PubMed] [Google Scholar]
- Kim SW, Kim SJ, Yoon BH, Kim JM, Shin IS, Hwang MY, Yoon JS. Diagnostic validity of assessment scales for depression in patients with schizophrenia. Psychiatry research. 2006;144(1):57–63. doi: 10.1016/j.psychres.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Kremen WS, Seidman LJ, Faraone SV, Toomey R, Tsuang MT. The paradox of normal neuropsychological function in schizophrenia. Journal of Abnormal Psychology. 2000;109(4):743. doi: 10.1037/0021-843X.109.4.743. [DOI] [PubMed] [Google Scholar]
- Liddle PF. Schizophrenic syndromes, cognitive performance and neurological dysfunction. Psychological Medicine. 1987;17(1):49–57. doi: 10.1017/s0033291700012976. Retrieved from http://dx.doi.org/10.1017/S0033291700012976. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mass R, Schoemig T, Hitschfeld K, Wall E, Haasen C. Psychopathological syndromes of schizophrenia: Evaluation of the dimensional structure of the Positive and Negative Syndrome Scale. Schizophrenia Bulletin. 2000;26(1):167–177. doi: 10.1093/oxfordjournals.schbul.a033437. [DOI] [PubMed] [Google Scholar]
- Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 update. World Health Organization; 2008. [Google Scholar]
- McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: Relevance to persons with schizophrenia. Schizophrenia Research. 2004;72(1):53–67. doi: 10.1016/j.schres.2004.09.011. Retrieved from http://dx.doi.org/10.1016/j.schres.2004.09.011. [DOI] [PubMed] [Google Scholar]
- O’Carroll R, Walker M, Dunan J, Murray C, Blackwood D, Ebmeier KP, Goodwin GM. Selecting controls for schizophrenia research studies: The use of the national adult reading test (NART) is a measure of pre-morbid ability. Schizophrenia Research. 1992;8(2):137–141. doi: 10.1016/0920-9964(92)90030-9. Retrieved from http://dx.doi.org/10.1016/0920-9964(92)90030-9. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Dawes SE, Heaton RK. What do we know about neuropsychological aspects of schizophrenia? Neuropsychology Review. 2009;19(3):365–384. doi: 10.1007/s11065-009-9109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: Development of a new measure of everyday functioning for severely mentally ill adults. Schizophrenia Bulletin. 2001;27(2):235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16(2):93. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Randolph C. Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) Psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, Harvey PD. Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophrenia Research. 2012;137(1–3):190–195. doi: 10.1016/j.schres.2012.02.002. Retrieved from http://dx.doi.org/10.1016/j.schres.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider LC, Struening EL. SLOF: A behavioral rating scale for assessing the mentally ill. Social Work Research and Abstracts. 1983;6:9–21. doi: 10.1093/swra/19.3.9. [DOI] [PubMed] [Google Scholar]
- Small JG, Hirsch SR, Arvanitis LA, Miller BG, Link CGG. Quetiapine in patients with schizophrenia: A high-and low-dose double-blind comparison with placebo. Archives of General Psychiatry. 1997;54(6):549–557. doi: 10.1001/archpsyc.1997.01830180067009. [DOI] [PubMed] [Google Scholar]
- Tamminga CA, Buchanan RW, Gold JM. The role of negative symptoms and cognitive dysfunction in schizophrenia outcome. International Clinical Psychopharmacology. 1998;13(3):S21–S26. doi: 10.1097/00004850-199803003-00004. [DOI] [PubMed] [Google Scholar]
- Test MA, Greenberg JS, Long JD, Brekke JS, Burke SS. Construct validity of a measure of subjective satisfaction with life of adults with serious mental illness. Psychiatric Services. 2005;56(3):292–300. doi: 10.1176/appi.ps.56.3.292. [DOI] [PubMed] [Google Scholar]
- Tolman AW, Kurtz MM. Neurocognitive predictors of objective and subjective quality of life in individuals with schizophrenia: A meta-analytic investigation. Schizophrenia Bulletin. 2012;38(2):304–315. doi: 10.1093/schbul/sbq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley EW, Jeste DV, Bellack AS. A review of cognitive training in schizophrenia. Schizophrenia Bulletin. 2003;29(2):359–382. doi: 10.1093/oxfordjournals.schbul.a007011. [DOI] [PubMed] [Google Scholar]
- Velligan DI, Mahurin RK, Diamond PL, Hazleton BC, Eckert SL, Miller AL. The functional significance of symptomatology and cognitive function in schizophrenia. Schizophrenia Research. 1997;25(1):21–31. doi: 10.1016/S0920-9964(97)00010-8. [DOI] [PubMed] [Google Scholar]
- Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: A meta-analysis. Schizophrenia Research. 2009;113(2–3):189–199. doi: 10.1016/j.schres.2009.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilk CM, Gold JM, Humber K, Fenton WS, Buchanan RW, Dickerson F. Brief cognitive assessment in schizophrenia: Normative data for the Repeatable Battery for the Assessment of n Status. Schizophrenia Research. 2004;70(2):175–186. doi: 10.1016/j.schres.2003.10.009. [DOI] [PubMed] [Google Scholar]