Abstract
Percutaneous endoscopic gastrostomy (PEG) is a relatively safe and effective method of providing nutrition to patients with neurologic deficits or proximal gastrointestinal pathology. Complications that follow this common procedure include dislodgement, dysfunction, infection and aspiration. The “Buried Bumper Syndrome” (BBS) is an infrequent and late complication of PEG tubes that can result in tube dysfunction, gastric perforation, bleeding, peritonitis or death. The emergency physician should be aware of historical and exam features that suggest BBS and distinguish it from other, more benign, PEG-tube related complaints. We report a case of a woman presenting with BBS 3 weeks after having a PEG tube placed.
CASE
A 76-year-old woman presented to the emergency department (ED) because of pain and drainage at her percutaneous endoscopic gastrostemy (PEG) tube site and inability to instill fluid. Three weeks prior, she had undergone a laryngectomy for recurrent laryngeal cancer. At the same time she had a tracheostomy and PEG performed. Three hours prior to arrival, she noticed peritubal leakage and localized discomfort with attempts to flush the tube. She denied prior complications with the tube.
On examination, the patient had normal vital signs and appeared comfortable. Her head, chest, and extremity exams were normal. Her neck showed a well-healing surgical incision. Her abdomen was soft with no appreciable tenderness. There was no evidence of distention or palpable masses. The patient’s PEG site was not indurated and showed no erythema or drainage. The external bolster was approximately 1 centimeter from the skin surface. The tube was not mobile within the stoma.
Attempts to flush the tube with warm water and then soda resulted in peritubal leakage. It also caused the patient sharp, instantaneous abdominal pain at the site of the PEG. When the provider palpated the PEG site during flushing, transient distention and gurgling was felt within the abdominal wall.
A tube study was performed. Based on this study, a computed tomography (CT) was performed (Figure) to determine the exact location of the PEG tube as well as any secondary complications resulting from its misplacement.
Figure.
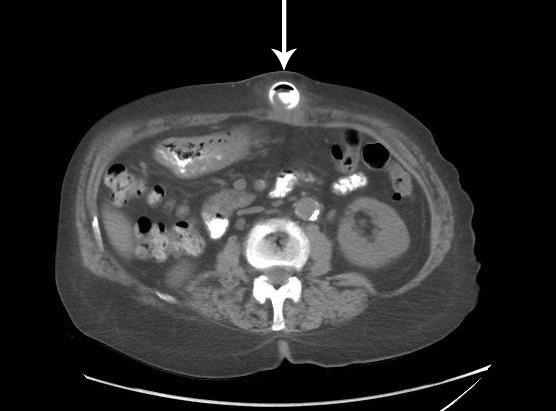
Axial contrast computed tomography demonstrates internal bolster in the subcutaneous tissue of the anterior abdominal wall without evidence of contrast extravasation.
General surgery was consulted for the malfunctioning PEG tube. The surgical attending recognized this as “Buried Bumper Syndrome,” an uncommon and dangerous complication of PEG tube placement. The patient was admitted to the hospital for intravenous (IV) antibiotics and fluid hydration. Her PEG tube was removed operatively and was not replaced.
DISCUSSION
PEG tube placement is performed 250,000 times per year in the United States.1 It permits enteral access for patients who are unable to take food, water and medications by mouth. It may be indicated in patients with a persistent neurologic deficit, a fistula or malignant obstruction proximal to the stomach, or for gastric decompression, such as with severe bowel dysmotility. The percutaneous technique in particular, introduced in 1980, permits non-surgical placement of enteral feeding tubes in a population of patients who are undernourished but are suboptimal candidates for laparoscopic feeding tube placement because they are likely to demonstrate poor wound healing.2
Overall, serious complications secondary to PEG tube placement are uncommon. Immediate complications from upper endoscopy or from the PEG tube placement itself, such as acute bleeding, esophageal perforation, or aspiration, are generally diagnosed prior to discharge and do not present to the ED.3 However, other complications occur later, and it is not uncommon for patients to present to the ED with a complaint referable to their PEG tube weeks to months or even years after placement.4
BBS is a rare complication of PEG tube placement that occurs in 0.3–2.4% of patients. This phenomenon occurs when the bolster inside the stomach produces ischemic necrosis of the gastric mucosa and migrates into the gastric wall or subcutaneous tissue. Although this has been described in the gastroenterology literature as a late complication of PEG tube placement, it has been reported in 1 case to occur 8 days after placement.5 In our patient, it occurred 3 weeks after her procedure. That said, the vast majority of cases present more than a year after PEG tube placement.6,7
The etiology of the syndrome appears to be related to traction on the internal bolster during placement, manipulation or when abdominal adipose sags in the upright posture. This traction creates pressure between the internal bolster and the gastric wall, ultimately leading to pressure necrosis. Recent studies have identified risk factors associated with BBS, including obesity, multiple gauze or other dressings between the external bolster and the abdominal wall, manipulation of the tube by inexperienced personnel, and even chronic cough.8
BBS may mimic stomal infection, uncomplicated tube leakage, or tube obstruction.3,6 It may also present with peritonitis, gastrointestinal bleeding, or sepsis.9 The most common symptom is pain, which may be persistent secondary to dissection of instilled feeds or medications within the abdominal wall or may be intermittent, as in our patient.10 Early in the course of pathogenesis, the patient may not experience tube obstruction, but as the gastric mucosa slowly grows over the internal bolster, the device eventually becomes non-functional. Abscess and abdominal wall infections have also been reported as complications of BBS, and there has been a case report of death resulting from the syndrome.9
Although radiographic studies such as CT or tube studies may assist in finding the exact location of the PEG tube, the diagnosis of BBS is a clinical one.11 Although its clinical presentation overlaps those of other PEG tube complications, a careful physical exam will reveal that the PEG tube cannot rotate within or slide through the stoma in patients with BBS.10 This is because the buried bumper causes the tube to become fixed in place. This is in contrast to patients with localized wound infection, uncomplicated PEG tube leakage, and tube obstruction, in whom the PEG tube should be freely mobile in the stoma on physical exam and should not be painful with installation of fluids.
In the emergency setting, suspicion of this entity should prompt consultation with surgery and admission of the patient to the hospital. IV access should be obtained, and the patient should not be given any medications or fluids through the PEG tube. Some surgeons recommend patients receive antibiotics even in the absence of infectious symptoms, as the pathophysiology of this disease assumes abdominal wall contamination with tube feeds. The definitive treatment of BBS is removal of the PEG tube. This can be accomplished with surgery, endoscopy, or a combination of the two, depending on the location of the bumper and the complications encountered.3
CONCLUSION
Complications of PEG tubes are commonly encountered by the emergency physician. Although most complications are minor, BBS is a potentially life-threatening process that may mimic more benign conditions. The emergency physician should have a high index of suspicion for this entity, and should be aware of historical and physical exam features that suggest BBS. Early diagnosis and surgical consultation for the management of BBS may help avoid repeated ED visits and more serious complications.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Lynch CR, Fang JC. Prevention and management of complications of percutaneous endoscopic gastrostomy (PEG) tubes. Pract Gastroenterol. 2004;28:66–76. [Google Scholar]
- 2.Gauderer MWL, Ponski J, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 3.Schrag SP, Sharma R, Jaik NP, et al. Complications related to percutaneous endoscopc gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16(4):407–418. [PubMed] [Google Scholar]
- 4.Hull MA, Rawlings J, Murray FE, et al. Audit of outcome of long-term enteral nutrition by percutaneous endoscopic gastrostomy. Lancet. 1993;341(8849):869–872. doi: 10.1016/0140-6736(93)93072-9. [DOI] [PubMed] [Google Scholar]
- 5.Venu RP, Brown RD, Pastika BJ, et al. The buried bumper syndrome: a simple management approach in two patients. Gastrointest Endosc. 2002;56:582–584. doi: 10.1067/mge.2002.128109. [DOI] [PubMed] [Google Scholar]
- 6.Pop GH. Buried bumper syndrome: can we prevent it? PPract Gastroenterol. 2010;84:8–13. [Google Scholar]
- 7.Lee TH, Lin JT. Clinical manifestations and management of buried bumper syndrome in patients with percutaneous endoscopic gastrostomy. Gastrointest Endosc. 2008;68(3):580–584. doi: 10.1016/j.gie.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Ma MM, Semlacher EA, Pedorak RN. The buried gastrostomy bumper syndrome: prevention and endoscopic approaches to removal. Gastrointest Endosc. 1995;41:505–508. doi: 10.1016/s0016-5107(05)80012-4. [DOI] [PubMed] [Google Scholar]
- 9.Anagnostopoulos GK, Kostopoulos P, Arvanitidis DM. Buried bumper syndrome with a fatal outcome, presenting early as gastrointestinal bleeding after percutaneous gastrostomy placement. J Postgrad Med. 2003;49:325–327. [PubMed] [Google Scholar]
- 10.Fireman Z, Yunis N, Coscas D, et al. The buried gastrostomy bumper syndrome. Harefuah. 1996;131:92–93. [PubMed] [Google Scholar]
- 11.McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58:739–751. doi: 10.1016/s0016-5107(03)02147-3. [DOI] [PubMed] [Google Scholar]


