Summary
Background:
Lymphocytic vasculitis of the central nervous system is an uncommon subtype of primary angiitis of the central nervous system (PACNS) – a rare inflammatory disorder affecting parenchymal and leptomeningeal arteries and veins.
Case Report:
Establishing diagnosis on the basis of neuroimaging only is difficult, as it can mimic a brain tumor. Thus, histological diagnosis is essential for appropriate management.
We present a case of biopsy-proven lymphocytic vasculitis mimicking a brain tumor on neuroimaging that was subsequently successfully treated with steroid therapy. We also discuss the findings in perfusion MR (PWI) and MR spectroscopy (MRS).
Conclusions:
Regional hypoperfusion on PWI and elevation of glutamate and glutamine levels on MRS (without associated typical tumor spectra) are common findings in inflammatory disorders, including PACNS, and can be useful in differential diagnosis with tumors.
Keywords: primary angiitis of central nervous system (PACNS), brain tumor diagnostics, proton magnetic resonance spectroscopy (1H MRS), diffusion weighted imaging, perfusion weighted imaging, magnetic resonance imaging (MRI)
Background
Lymphocytic vasculitis of the central nervous system is an uncommon subtype of primary angiitis of the central nervous system (PACNS) – a rare inflammatory disorder affecting parenchymal and leptomeningeal arteries and veins.
Establishing diagnosis on the basis of neuroimaging only is difficult and histological diagnosis is essential for initiation of appropriate management.
We present a case of biopsy-proven lymphocytic vasculitis mimicking a brain tumor on neuroimaging that was subsequently successfully treated with steroid therapy. We also discuss findings in perfusion MR (PWI) and MR spectroscopy (MRS).
Case Report
A 46-year-old woman with progressive confusion, headache, dizziness and nystagmus underwent brain MR examination with a 1.5 Tesla system (Philips Intera Gyroscan) using axial and coronal FSE T2 weighted (w), axial and sagittal SE T1, axial FLAIR T2 sequences, as well as axial DWI/ADC and axial and sagittal FLAIR T1 after injection of paramagnetic contrast agent.
MRI showed a tumor-like lesion characterized by increased signal on FLAIR T2-weighted images (Figure 1A) and low signal on T1-weighted images in the right temporal lobe; FLAIR T1 sequence following injection of paramagnetic contrast agent revealed signal intensification (Figure 1B).
Figure 1.
(A) FLAIR T2-weighted image. (B) FLAIR T1 sequence image after contrast injection. Presence of a tumor-like lesion in the right temporal lobe, characterized by increased signal on FLAIR T2-weighted image, enhancing after injection of contrast agent.
Diffusion weighted imaging (DWI) with echo-planar spin-echo technique (b value =0 and 1000) showed no areas of restricted diffusion (Figure 2).
Figure 2.
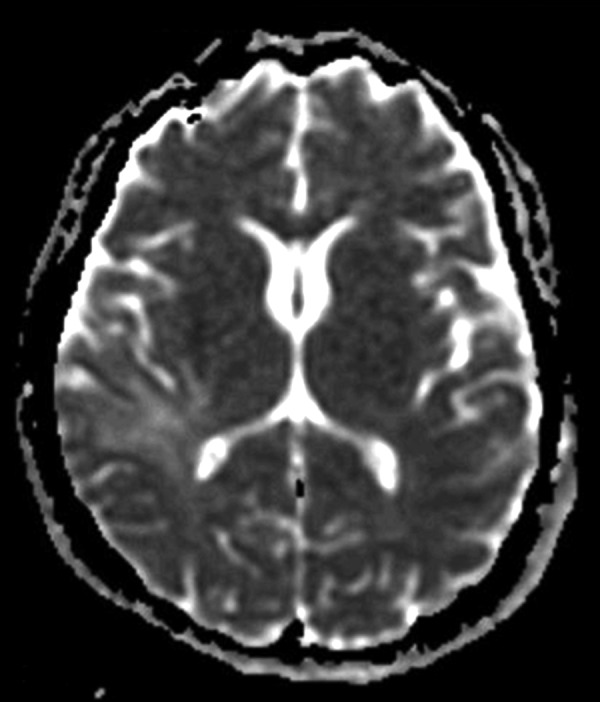
Diffusion weighted imaging – ADC map. The lesion does not show areas of restricted diffusion.
The PWI study carried out with an EPI-SE sequence (TR 1900, TE 80, matrix 192×128, 1,7-mm thickness, 40 acquisitions, 67-sec. acquisition time, 0.1 mmol/kg of gadobutrol at a flow rate of 5 ml/s, 8-sec. acquisition delay) showed low relative cerebral blood volume (rCBV) within the lesion and in the peripheral region, indicating hypoperfusion (Figure 3).
Figure 3.
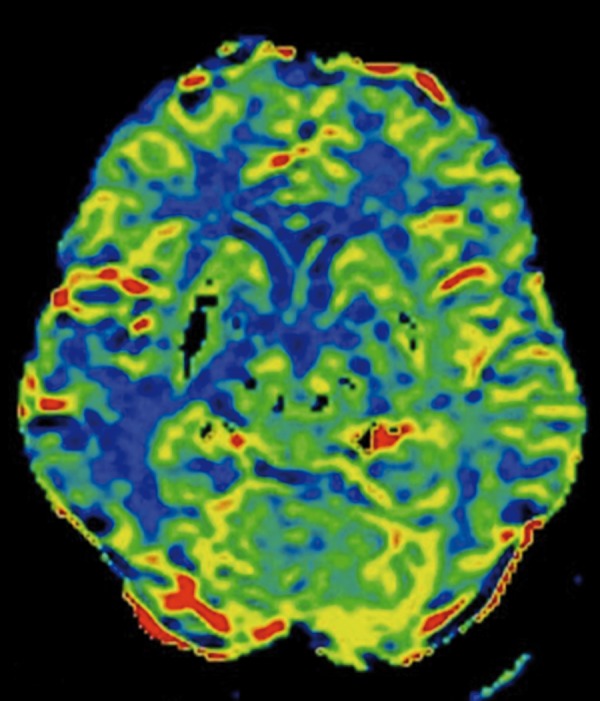
Perfusion weighted imaging (PWI study). Presence of low cerebral blood volume (rCBV), indicating hypoperfusion within and around the lesion.
Single-voxel MRS using a point resolved spectroscopy (PRESS) protocol with short (35 ms) TE revealed a slight elevation of lactate peak and elevation of glutamate and glutamine peaks (2.1–2.5 ppm).
Stereotaxic biopsy of the lesion demonstrated perivascular lymphocytic infiltration without evidence of malignancy or foreign organisms (Figure 4).
Figure 4.
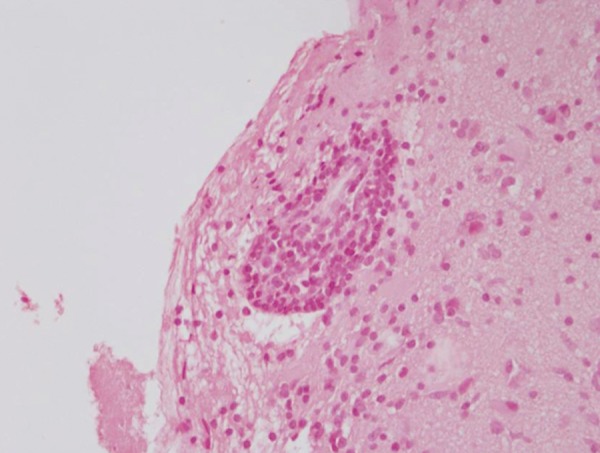
Histological diagnosis obtained by stereotaxic biopsy of the lesion. Presence of perivascular lymphocytic infiltration.
Steroid treatment was instituted and follow-up imaging three months later showed regression of the lesion.
Discussion
Lymphocytic vasculitis, also known as lymphocytic angiitis, is a subtype of PACNS – a rare inflammatory disorder affecting parenchymal and leptomeningeal arteries and veins [1].
The cause of this extremely rare inflammatory disorder is unclear. The correct diagnosis is essential because most patients respond to appropriate therapy. Diagnosis of PACNS is difficult due to its rarity and variability of clinical and imaging findings. MR images commonly show an area of vasogenic edema with mass effect and with contrast enhancement that can be misinterpreted as a brain tumor [2,3].
Various protocols have been suggested to improve the diagnosis of central nervous system vasculitis (CNVS) using conventional MR imaging and angiography. Harris et al. [4] reported that a negative MR excludes intracranial vasculitis with greater certainty than angiographic findings. In our opinion, results of angiography are unimportant in a patient with normal MR findings and it is indicated only if MR results are abnormal.
On the contrary, Greenan et al. [5], found that some patients with CNVS may have normal MR examination and positive angiographic findings. Authors concluded that angiography should be the technique of choice for the diagnosis of patients with suspected CNVS.
Small vessels are predominantly involved in CNS vasculitis, resulting in ischemic lesions that can be depicted on conventional MR or, even better, by using DW technique [6,7]. These MR findings are not specific for CNSV and uninfarcted tissue is frequently present in CNSV.
Angiography exhibits low resolution in detecting small-vessel abnormalities in CNSV and provides evidence for the presence of lesions of medium-to-large blood vessels [8]. Therefore, angiography is less sensitive than MR, but more specific for CNSV.
Pomper et al. [8] suggested that the two techniques provide different information about CNVS, complementing each other in the diagnosis of vasculitis.
A definitive diagnosis frequently requires brain biopsy, but histological confirmation depends on the site of inflammatory lesion, from which biopsy was obtained and timing of biopsy during active inflammation [6].
In the presented case, MRI showed a tumor-like enhancing lesion associated with moderate vasogenic edema and low rCBV, which can also be observed in low-grade gliomas.
MRS revealed an increased peak of glutamate and glutamine suggesting non-neoplastic lesion. There are only two reports of spectroscopy patterns of glutamate and glutamine elevation associated with inflammatory processes of the CNSV [2,9].
According to literature, MRS pattern of CNSV shows conflicting results: in a report of lymphocytic vasculitis, MR spectroscopy did not reveal significant elevation of the choline (Cho) peak [9]. On the contrary, Beppu et al. [2] reported a marked elevation of Cho in case of CNSV.
PWI has been suggested as a non-invasive technique to gather information about hypoperfusion caused by small vessel involvement in CNSV. Yuh et al. [6] reported a case of CNSV diagnosed on the basis of PWI findings in a patient with a stroke-like lesion on conventional MRI and negative angiogram.
In our case, PWI showed reduced rCBV within the lesion as well as in the adjacent cerebral tissue, indicating regional tissue hypoperfusion caused by a small vasculitic lesion.
Conclusions
In conclusion, our report emphasizes that elevation of glutamate and glutamine on MRS and regional hypoperfusion on PWI may constitute MR features of CNSV that neuroradiologists have to take in account in the differential diagnosis with brain tumors, which may appear similar in conventional MRI.
References:
- 1.Vollmer TL, Guarnaccia J, Harrington W, et al. Idiopathic granulomatous angiitis of the central nervous system: diagnostic challenges. Arch Neurol. 1993;50:925–30. doi: 10.1001/archneur.1993.00540090032007. [DOI] [PubMed] [Google Scholar]
- 2.Beppu T, Inoue T, Nishimoto H, et al. Primary granulomatosis angiitis of the central nervous system: findings of magnetic resonance spectroscopy and fractional anisotropy in diffusion tensor imaging prior to surgery: case report. J Neurosurg. 2007;107(4):873–77. doi: 10.3171/JNS-07/10/0873. [DOI] [PubMed] [Google Scholar]
- 3.Pinto A, Caranci F, Romano L, et al. Learning from errors in radiology: a comprehensive review. Semin Ultrasound CT MRI. 2012;33:379–82. doi: 10.1053/j.sult.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Harris KG, Tran DD, Sickels WJ, et al. Diagnosing intracranial vasculitis: the roles of MR and angiography. AJNR Am J Neuroradiol. 1994;15:317–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Greenan TJ, Grossman RI, Goldberg HI. Cerebral vasculitis: MR imaging and angiographic correlation. Radiology. 1992;182:65–72. doi: 10.1148/radiology.182.1.1727311. [DOI] [PubMed] [Google Scholar]
- 6.Yuh WTC, Ueda T, Maley JE. Perfusion and diffusion: a potential tool for improved diagnosis of CNS vasculitis. Am J Neuroradiol. 1999;20:87–89. [PubMed] [Google Scholar]
- 7.White ML, Hadley WL, Zhang YD, et al. Analysis of central nervous system vasculitis with diffusion-weighted imaging and apparent diffusion coefficient mapping of the normal appearing brain. Am J Neuroradiol. 2007;28:933–37. [PMC free article] [PubMed] [Google Scholar]
- 8.Pomper MG, Miller TJ, Stone JH, et al. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. Am J Neuroradiol. 1999;20:75–85. [PubMed] [Google Scholar]
- 9.Panchal NJ, Niku S, Imbesi SG. lymphocytic vasculitis mimicking aggressive multifocal cerebral neoplasm: MR imaging and MR spectroscopy appearance. Am J Neuroradiol. 2005;26:642–45. [PMC free article] [PubMed] [Google Scholar]



