Abstract
Background
Increased intra-abdominal pressure during laparoscopic surgery causes cephalad displacement of the diaphragm, resulting in the formation of atelectasis, which can be overcome by positive end-expiratory pressure (PEEP). The aim of this prospective study was to investigate the level of optimal PEEP to maintain adequate arterial oxygenation and hemodynamics during robot-assisted laparoscopic radical prostatectomy (RLRP).
Methods
One hundred patients undergoing RLRP were randomly allocated to one of five groups (n = 20) (0, 3, 5, 7 and 10 cmH2O of PEEP). Hemodynamic variables and respiratory parameters were measured at baseline with the patient in the supine position; at 30 min, 1, 2, 3 and 4 h during CO2 insufflation with the patient in the post-Trendelenburg position; and after deflation in the supine position with increasing PEEP.
Results
The PaO2 levels and alveolar-arterial difference in oxygen tension (AaDO2) were improved in patients with PEEPs compared with patients in whom PEEP was not used. The application of PEEP (10 cmH2O) resulted in higher PaO2 levels compared to those with lower PEEP levels, but excessive peak airway pressure (PAP) was sometimes observed. The application of a PEEP of 7 cmH2O resulted in similar PaO2 levels without causing excessive PAP. There was a significant difference in central venous pressure between the groups, but there were no significant differences in heart rate, mean arterial pressure or minute ventilation between the groups.
Conclusions
A PEEP of 7 cmH2O is associated with the greater improvement of PaO2 and AaDO2 without causing excessive PAP during RLRP.
Keywords: Hemodynamics, Laparoscopy, Positive end-expiratory pressure, Robotics, Prostatectomy
Introduction
Robot-assisted laparoscopic radical prostatectomy (RLRP) is frequently used in the treatment of prostate cancer; the advantages of the procedure include nerve sparing, reduced blood loss, less postoperative pain, and shorter hospital stays [1]. However, the increase in intra-abdominal pressure during laparoscopic procedures caused by a steep Trendelenburg position and pneumoperitoneum enhances the cranial displacement of the diaphragm. This displacement can cause decreased lung volumes, including a decrease in functional residual capacity, decreased compliance, increased resistance and ventilation-perfusion mismatch [2]. A few clinical studies have reported the respiratory and hemodynamic effects of mechanical ventilation with and without positive end-expiratory pressure (PEEP) during prolonged pneumoperitoneum [3-6]. The application of a PEEP of 5 or 10 cmH2O preserves arterial oxygenation during the establishment of pneumoperitoneum and while the patient is in the Trendelenburg position [3,4]. However, patients presenting for RLRP are usually elderly and often have cardiovascular and respiratory dysfunction [7]. PEEP increases intrathoracic pressure, thereby decreasing left ventricular preload and afterload in patients with cardiomyopathy [8]. The prevalence of cardiovascular disease is 25 to 35% higher in geriatric patients undergoing non-cardiac surgery [9]. Therefore, it is very important to determine the proper PEEP level that provides the maximum beneficial effect of the oxygen transport while minimizing cardio-pulmonary side effects during RLRP.
The aim of this study was to investigate the optimal level of PEEP in patients undergoing procedures that require a prolonged pneumoperitoneum and steep Trendelenburg position.
Materials and Methods
After gaining approval from the Hospital Ethics Committee and obtaining written informed consent for the clinical research, the study was conducted prospectively on 100 patients (American Society of Anesthesiologists [ASA] physical status I-III, aged 49-75 years) who underwent general anesthesia for RLRP. The patients were randomly allocated to one of five groups (n = 20), comparable with respect to patient characteristics (Table 1). No patients were excluded from the analysis due to complications; hence, the data for all 100 patients is presented. In the 3 PEEP, 5 PEEP, 7 PEEP and 10 PEEP groups, a constant PEEP of 3, 5, 7 and 10 cmH2O was used, respectively, whereas in the ZEEP group no PEEP was used. Patients with pulmonary disease, primary valvular heart disease, uncontrolled hypertension, peripheral vascular disease, expected difficult intubation, immunosuppressive therapy, renal failure or who had a body mass index > 31 kg/m2 were excluded from the investigation.
Table 1.
Patient Characteristics
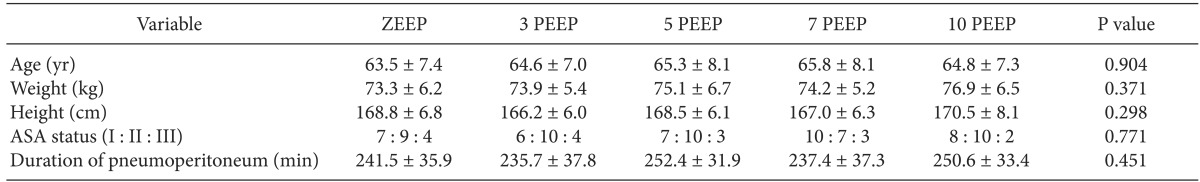
Values are mean ± SD or number. The subjects of each group are 20 patients, respectively. ASA: American Society of Anesthesiologists, ZEEP, 3 PEEP, 5 PEEP, 7 PEEP, 10 PEEP: positive end-expiratory pressure with 0 cmH2O, 3 cmH2O, 5 cmH2O, 7 cmH2O, 10 cmH2O.
Without premedication, anesthesia was induced with propofol 1-2 mg/kg, remifentanil 0.2 µg/kg/min and rocuronium 0.6 mg/kg. After induction, the lungs were ventilated in volume-controlled mode with a tidal volume of 8 ml/kg, a respiratory rate of 12 bpm, I : E time = 1 : 2, a fraction of inspired oxygen (FiO2) of 0.5 in the air, and the ETCO2 was kept below 45 mmHg. These ventilatory parameters were adjusted according to arterial blood gas levels throughout the operation to maintain physiologic pH, base excess (BE), HCO3- and PaCO2 (7.35-7.45, ± 3 mmol/L, 21-27 mmol/L and 35-40 mmHg). In the PEEP groups, a constant PEEP of 3, 5, 7 or 10 cmH2O was applied, respectively, whereas in the ZEEP group, the patients' lungs were ventilated without PEEP. Intraoperative monitoring used in the present study included a 5-lead ECG, invasive and noninvasive arterial pressure, central venous pressure (CVP), pulse oximetry, nasopharyngeal temperature, infrared CO2 analysis, inspired oxygen fraction, bispectral index (BIS), minute ventilation (MV) and peak airway pressure (PAP). Anesthesia was maintained with sevoflurane (1.0-1.5 vol%) and remifentanil 0.05-0.10 µg/kg/min with 50% oxygen, and dosages were adjusted according to clinical status. In all patients, depth of anesthesia was adjusted to obtain a BIS (Model A 2000, Aspect Medical Systems, Natick, USA) between 40 and 60. To maintain body temperature, an air warmer (Bair Hugger 505 warming unit, Arizant Healthcare, Kentucky, USA) was used.
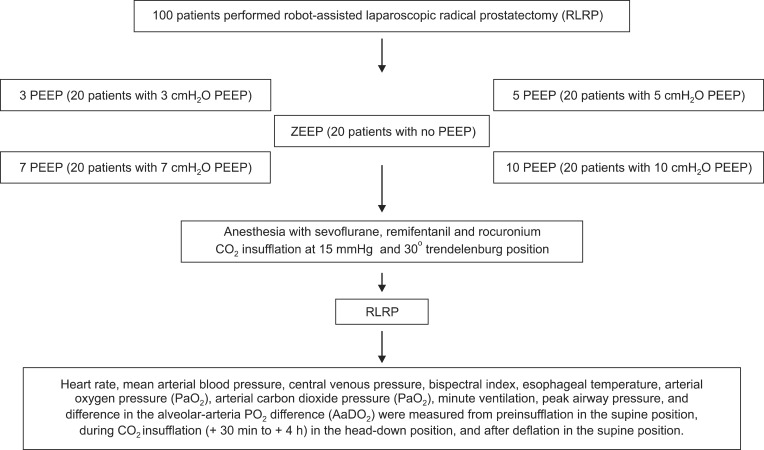
The surgical exposure was achieved by insufflation of CO2 to an intraperitoneal pressure of 15 mmHg with automatically adjusted gas flow in all groups. Intraoperative characteristics including heart rate (HR), mean arterial blood pressure (MAP), CVP, MV and PAP were recorded during surgery. These values represent the average measurements over a 15-s interval. Arterial blood gas analyses including pH, BE, HCO3-, PaCO2 and PaO2 were performed in the operating room with a Critical Care Xpress® (Nova biomedical, Waltham, MA, USA). The alveolar-arterial difference in oxygen tension (AaDO2) was also calculated as follows; AaDO2 = [barometric pressure (760 mmHg) - 47] × FiO2 - PaCO2 - PaO2. Measurements were recorded at seven different times during the procedure. The first measurement was a baseline measurement and was recorded with the patient in a supine position after endotracheal intubation. Measurements were also made at 30 min, 1, 2, 3 and 4 h after CO2 insufflation to an intra-abdominal pressure of 15 mmHg and the patient in the Trendelenburg position with a table tilt of 30° (+30 min, +1 h, +2 h, +3 h, +4 h). The final measurement was made at the end of surgery after release of the pneumoperitoneum and a return to the supine position. The process is described in the diagram (Fig. 1).
Fig. 1.
Flow chart of the study. PEEP: positive end-expiratory pressure, ZEEP: no PEEP, RLRP: robot-assisted laparoscopic radical prostatectomy.
Our statistical analyses were performed using SPSS statistical software, version 17.0 (SPSS Inc, Chicago, IL, USA). In this study, the sample size calculation was taken from the preliminary results for the first 10 patients. On the basis of a relevant 25% change (20% change of SD) in respiratory mechanics properties, we calculated that 17 patients could test the null hypothesis at 0.05 significance with a power of 0.80. We enrolled 20 patients to account for a 10% drop out rate. Analysis of variance (ANOVA) was performed on the demographic data using the ANOVA test for continuous variables (i.e., age, weight, height, and duration of pneumoperitoneum) and the Kruskal-Wallis rank test for ASA status. To study the effects of time and group allocation on each of the variables, repeated-measure ANOVA was used to compare the respiratory mechanics parameters between baseline values and time (six levels). When an overall difference was detected, the Student-Newman-Keuls post-test was used to localize the significant differences. One-way ANOVA was used between groups, and multiple comparisons were made with the Dunn's method when the results were significant. The data were expressed as mean ± SD (number). Differences were considered statistically significant if P < 0.05.
Results
Cardiac arrhythmias, usually ventricular ectopic beats or bradyarrhythmias, were noted after abdominal insufflation in 10 patients: 2 in the ZEEP group, 1 in the 3 PEEP group, 2 in the 5 PEEP group, 2 in the 7 PEEP group, and 3 in the 10 PEEP group. CO2 subcutaneous emphysema occurred in 1 patient in the 10 PEEP group and quickly resolved with cessation of insufflations. There were no deaths in the series.
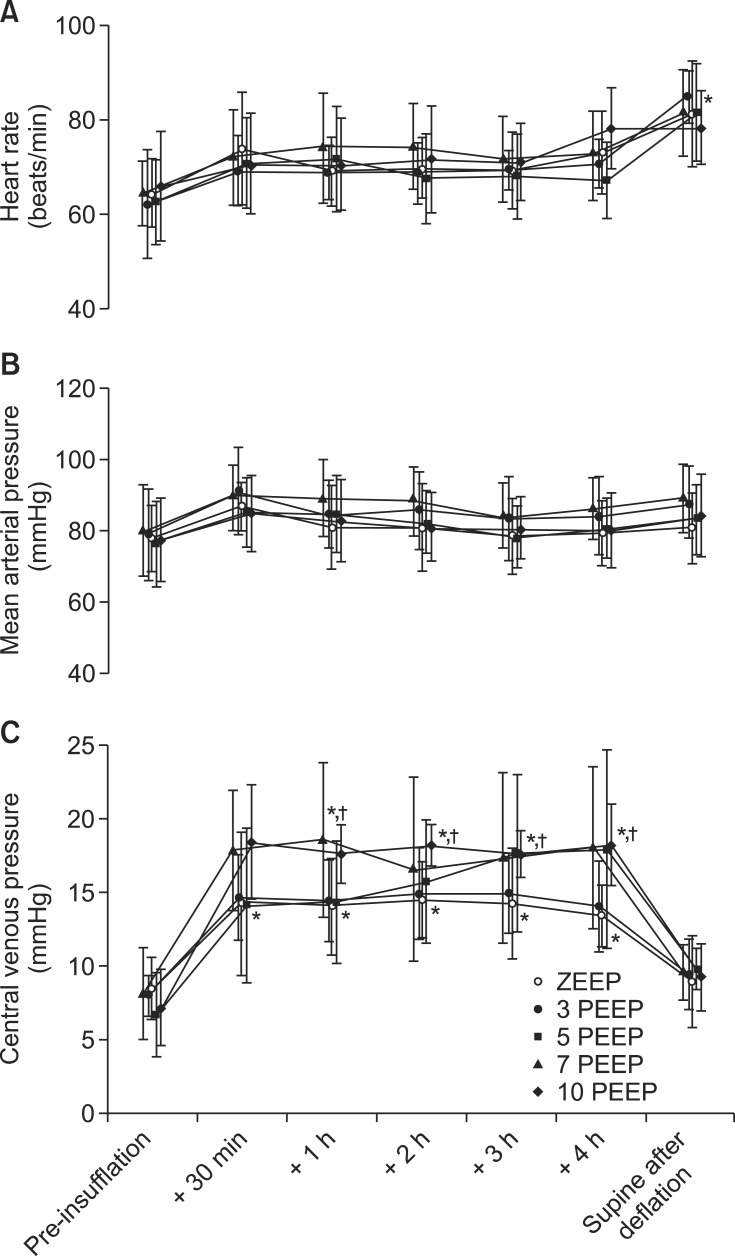
Heart rate and MAP were higher compared to preinsufflation levels during CO2-insufflation in all groups, but there were no significant differences. Abdominal desufflation caused significant increases in HR in all groups compared to baseline values (P < 0.05). There were no significant differences in HR or MAP between the groups. The CVP was significantly increased during peritoneal CO2-insufflation compared with preinsufflation levels in all groups (P < 0.001). Baseline values for CVP in the 7 PEEP and 10 PEEP groups increased significantly compared with those in the ZEEP and 3 PEEP groups during pneumoperitoneum (P < 0.001) (Fig. 2).
Fig. 2.
Changes in heart rate (A), mean arterial pressure (B) and central venous pressure (C) from pre-insufflation in the supine position, during carbon dioxide insufflation (+ 30 min to + 4 h) in the head-down position, and after deflation in the supine position with increasing PEEP. PEEP: positive end-expiratory pressure, ZEEP: no PEEP, Data are expressed as mean ± SD. *P < 0.001 versus pre-insufflation. †P < 0.001 versus the ZEEP and three PEEP groups.
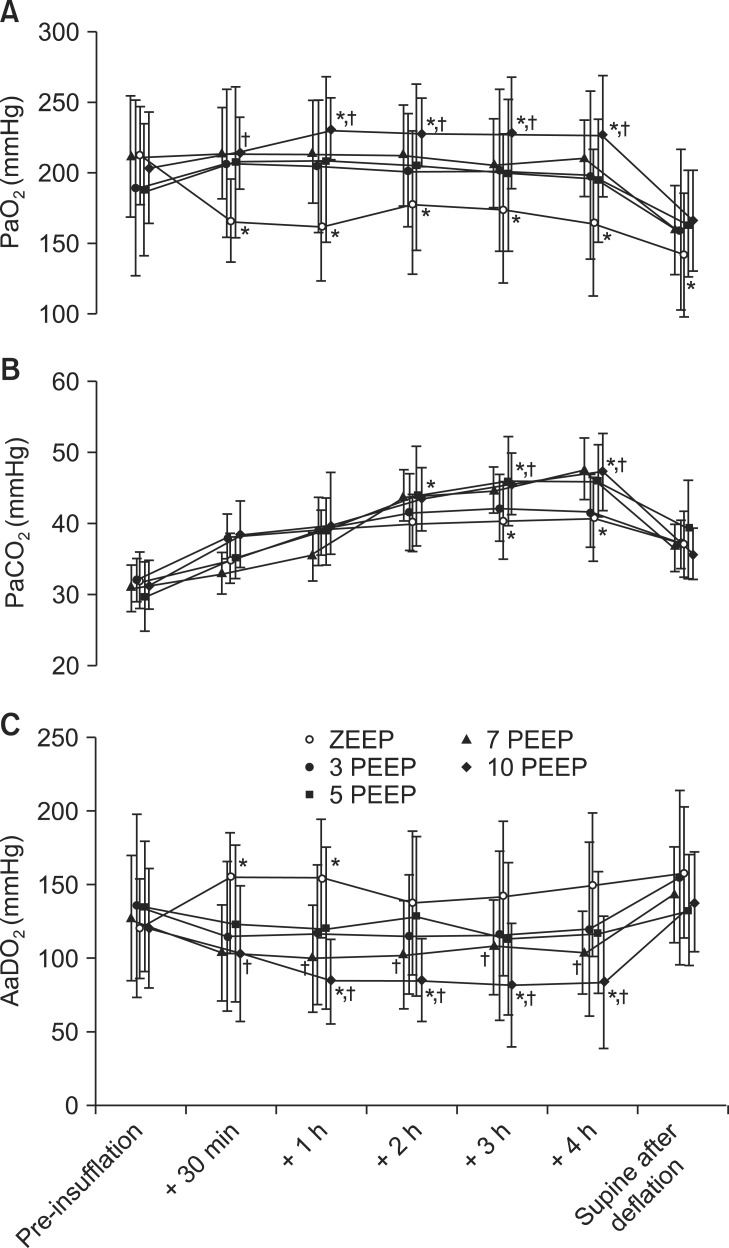
The PaO2 levels were significantly lower during peritoneal insufflation and after CO2-desufflation compared with preinsufflation levels in the ZEEP group (P < 0.05). In the 10 PEEP group, the PaO2 levels were significantly higher after 1 h of CO2-insufflation compared with preinsufflation levels (P < 0.05), but there were no significant differences among the PEEP groups. The PaO2 levels in the 10 PEEP group were higher compared with those in the ZEEP group during 4 h of CO2-insufflation (P < 0.05). The PaO2 levels in other PEEP groups were higher compared with those in the ZEEP group in the same duration, but there were no significant differences. The PaCO2 levels when pneumoperitoneum was established significantly increased compared with preinsufflation levels in all groups after 2 h of CO2-insufflation (P < 0.05). The PaCO2 levels in the 5, 7 and 10 PEEP groups showed significantly higher levels compared with those in the ZEEP and 3 PEEP groups after 3 h of CO2-insufflation (P < 0.05). The AaDO2 was significantly increased for 1 h after CO2-desufflation compared with preinsufflation levels in the ZEEP group (P < 0.05). In the 10 PEEP group, the AaDO2 was significantly lower after 1 h of CO2-insufflation compared with preinsufflation levels (P < 0.05), but there were no significant differences among the PEEP groups. The AaDO2 in the 7 and 10 PEEP groups showed significantly lower levels compared with those in the ZEEP group after 1 h of CO2-insufflation (P < 0.05) (Fig. 3).
Fig. 3.
Changes in arterial oxygen pressure (PaO2, A), arterial carbon dioxide pressure (PaCO2, B) and difference in the alveolar-arterial PO2 difference (AaDO2, C) from pre-insufflation in the supine position, during carbon dioxide insufflation (+ 30 min to + 4 h) in the head-down position, and after deflation in the supine position with increasing PEEP. PEEP: positive end-expiratory pressure, ZEEP: no PEEP, Data are expressed as mean ± SD. *P < 0.05 versus pre-insufflation. †P < 0.05 versus the ZEEP group.
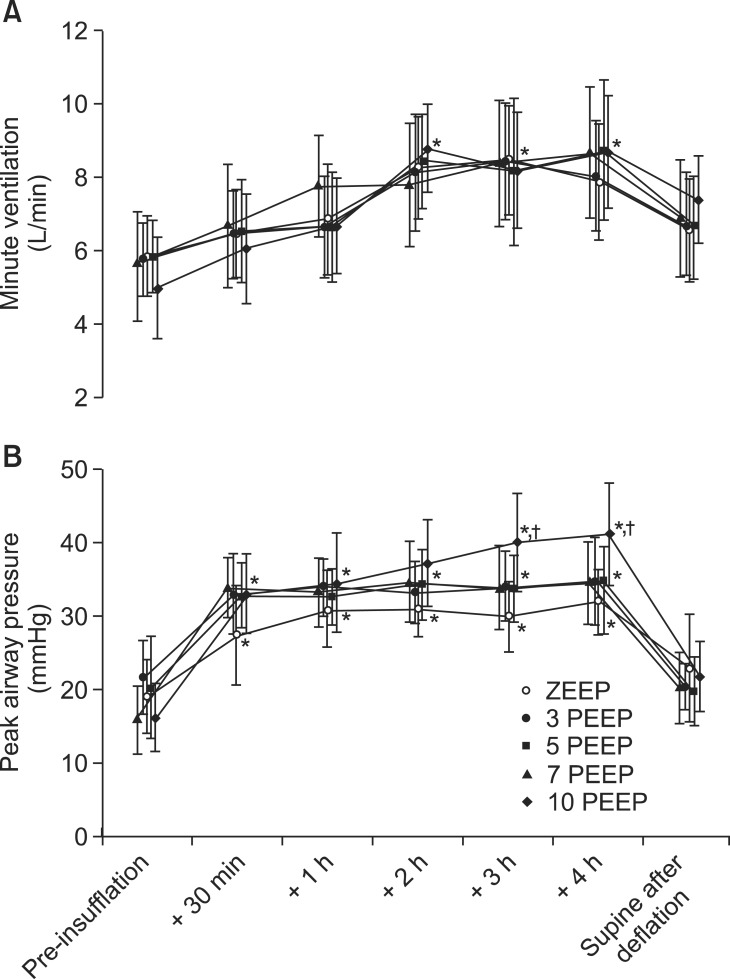
The MV levels during pneumoperitoneum were significantly increased compared with preinsufflation levels in all groups after 2 h of CO2-insufflation (P < 0.05). The PAP levels were significantly increased during peritoneal CO2-insufflation compared with preinsufflation levels in all groups (P < 0.05). The PAP levels in the 10 PEEP group were significantly higher than those in the ZEEP group after 3 h of CO2-insufflation (P < 0.05) (Fig. 4). In the 10 PEEP group, the PAP levels were greater than 45 mmHg in 6 patients during CO2-insufflation.
Fig. 4.
Changes in minute ventilation (A) and peak airway pressure (B) from pre-insufflation in the supine position, during carbon dioxide insufflation (+ 30 min to + 4 h) in the head-down position, and after deflation in the supine position with increasing PEEP. PEEP: positive end-expiratory pressure, ZEEP: no PEEP, Data are expressed as mean ± SD. *P < 0.05 versus pre-insufflation. †P < 0.05 versus the ZEEP group.
The BIS was maintained at a constant level (29-54) during the study period in all groups. None of the patients had recall during anesthesia, occurred the postoperative barotrauma or complained about anesthesia provided during the operation.
Discussion
This study showed that respiratory parameters in patients undergoing prolonged laparoscopic surgical procedures improve with PEEP. In this study, a PEEP of 7 cmH2O was the optimal, because this level of improved arterial oxygenation without excessive PAP during RLRP.
The typical effects of general anesthesia on gas exchange parameters and lung mechanics during prolonged pneumoperitoneum with PEEP were confirmed in this study. PEEP prevents end-expiratory airway closure and helps the airways to remain open. Keeping the airways open at the end of the expiratory period is fundamentally important for maintaining adequate gas exchange [10]. PEEP preserves arterial oxygenation during prolonged pneumoperitoneum in animal models with minimal adverse hemodynamic effects [11]. The application of a constant positive airway pressure of 5 cmH2O preserves arterial oxygenation during prolonged pneumoperitoneum [3]. A high PEEP (10 cmH2O) during pneumoperitoneum produced a significant improvement in the respiratory system elastance and resistance [4]. However, the most common complications of high PEEP are hemodynamic effects, especially in hypovolemic patients, and barotrauma [12]. Moreover, increased intra-abdominal pressure along with cephalad movement of the diaphragm produced greater than 50% increases in peak and plateau pressure during laparoscopic surgery [13]. CO2-induced subcutaneous emphysema is a complication of laparoscopic surgery, with an estimated incidence of 2.3%. Predictors of the development of subcutaneous emphysema are a high abdominal pressure, an end tidal CO2 pressure greater than 50 mmHg, an operative time greater than 200 min, and the use of six or more surgical ports [14,15]. In the present study, the PAP levels in the 10 PEEP group were greater than 45 mmHg in 6 patients during CO2-insufflation, and 1 of these patients developed subcutaneous emphysema. The postoperative barotrauma has not occurred in these patients, but this high pressure can lead to effects such as hemodynamic change or barotrauma.
In the present study, the high values (more than 140 mmHg) of AaDO2 were especially associated with ventilation-perfusion imbalance and impaired diffusion across the alveolar-capillary membrane in the ZEEP group. This may be associated with greater atelectasis formation in patients ventilated without PEEP. A similar high AaDO2 value (greater than 130 mmHg) during RLRP has been reported in other studies [3]. On the other hand, a relatively low AaDO2 (greater than 70 mmHg) has been reported during laparoscopic cholecystectomy, which may be due to the surgical position [16]. The results of this study suggest even a minor PEEP of 3 cmH2O can reduce or prevent pulmonary atelectasis formation in patients undergoing prolonged laparoscopic procedures. The use of PEEP in the presence of pneumoperitoneum induced greater ventilation, lead to less atelectasis in the dependent lung regions, and resulted in better ventilation/perfusion matching [3]. Although a PEEP of 10 cmH2O showed the lowest AaDO2 value compared to other PEEPs, this PEEP resulted in PAP levels that were too high (greater than 45 mmHg). However, a PEEP of 7 cmH2O led to similar levels of AaDO2 without causing excessive PAP levels. Our results indicate that a PEEP of 7 cmH2O is the optimal PEEP during prolonged pneumoperitoneum for RLRP.
The combination of increased intra-abdominal pressure (10-15 mmHg) and PEEP (8 cmH2O) markedly depressed the hemodynamic variables during laparoscopic pelvic lymphadenectomy in a dog model [17]. However, MAP substantially increased despite increasing PEEP levels (5, 10, 15, and 20 cmH2O) at a 15 mmHg insufflator pressure state during laparoscopic cholecystectomy [18]. The addition of a PEEP of 5 cmH2O to an intra-abdominal pressure of 12 mmHg produced only minor hemodynamic changes [3]. Previous study demonstrated that even 10 cmH2O of PEEP provided the smallest impairment of hemodynamics [19]. We also found minimal hemodynamic changes with increasing levels of PEEP. However, the hemodynamic responses to peritoneal insufflation during laparoscopic surgery resulted in serious changes in the SVR, cardiac index, and ejection fraction in an elderly population with coexisting cardiopulmonary diseases [20]. High-risk patients under general anesthesia should have expanded cardiopulmonary monitoring.
The limitation of the present study is that more than 60% of the subjects are elderly, and we were unable to completely standardize their cardiovascular diseases and drug use.
In conclusion, the application of a PEEP of 7 cmH2O resulted in significant arterial oxygenation augmentation without excessive peak airway pressure or depression of hemodynamic parameters during prolonged laparoscopic procedures with pneumoperitoneum. Our data indicate that a PEEP of 7 cmH2O may be recommended as the optimal PEEP.
References
- 1.Menon M, Hemal AK. Vattikuti Institute prostatectomy: a technique of robotic radical prostatectomy: experience in more than 1000 cases. J Endourol. 2004;18:611–619. doi: 10.1089/end.2004.18.611. [DOI] [PubMed] [Google Scholar]
- 2.Lestar M, Gunnarsson L, Lagerstrand L, Wiklund P, Odeberg-Wernerman S. Hemodynamic perturbations during robot-assisted laparoscopic radical prostatectomy in 45° Trendelenburg position. Anesth Analg. 2011;113:1069–1075. doi: 10.1213/ANE.0b013e3182075d1f. [DOI] [PubMed] [Google Scholar]
- 3.Meininger D, Byhahn C, Mierdl S, Westphal K, Zwissler B. Positive end-expiratory pressure improves arterial oxygenation during prolonged pneumoperitoneum. Acta Anaesthesiol Scand. 2005;49:778–783. doi: 10.1111/j.1399-6576.2005.00713.x. [DOI] [PubMed] [Google Scholar]
- 4.Maracajá-Neto LF, Roncally AC, Giannella A, Bozza FA, Lessa MA. Beneficial effects of high positive end-expiratory pressure in lung respiratory mechanics during laparoscopic surgery. Acta Anaesthesiol Scand. 2009;53:210–217. doi: 10.1111/j.1399-6576.2008.01826.x. [DOI] [PubMed] [Google Scholar]
- 5.Hazebroek EJ, Haitsma JJ, Lachmann B, Bonjer HJ. Mechanical ventilation with positive end-expiratory pressure preserves arterial oxygenation during prolonged pneumoperitoneum. Surg Endosc. 2002;16:685–689. doi: 10.1007/s00464-001-8174-y. [DOI] [PubMed] [Google Scholar]
- 6.Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, et al. Influence of steep Trendelenburg position and CO(2) pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433–439. doi: 10.1093/bja/aeq018. [DOI] [PubMed] [Google Scholar]
- 7.Wittgen CM, Naunheim KS, Andrus CH, Kaminski DL. Preoperative pulmonary function evaluation for laparoscopic cholecystectomy. Arch Surg. 1993;128:880–885. doi: 10.1001/archsurg.1993.01420200054010. [DOI] [PubMed] [Google Scholar]
- 8.Fellahi JL, Valtier B, Beauchet A, Bourdarias JP, Jardin F. Does positive end-expiratory pressure ventilation improve left ventricular function? A comparative study by transesophageal echocardiography in cardiac and noncardiac patients. Chest. 1998;114:556–562. doi: 10.1378/chest.114.2.556. [DOI] [PubMed] [Google Scholar]
- 9.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery. J Am Coll Cardiol. 2007;50:e159–e242. [Google Scholar]
- 10.Schibler A, Henning R. Positive end-expiratory pressure and ventilation inhomogeneity in mechanically ventilated children. Pediatr Crit Care Med. 2002;3:124–128. doi: 10.1097/00130478-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Hazebroek EJ, Haitsma JJ, Lachmann B, Bonjer HJ. Mechanical ventilation with positive end-expiratory pressure preserves arterial oxygenation during prolonged pneumoperitoneum. Surg Endosc. 2002;16:685–689. doi: 10.1007/s00464-001-8174-y. [DOI] [PubMed] [Google Scholar]
- 12.Safcsak K, Nelson LD. High-level positive end expiratory pressure management in the surgical patient with acute respiratory distress syndrome. AACN Clin Issues. 1996;7:482–494. doi: 10.1097/00044067-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110:810–815. doi: 10.1378/chest.110.3.810. [DOI] [PubMed] [Google Scholar]
- 14.Murdock CM, Wolff AJ, Van Geem T. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax, and pneumomediastinum during laparoscopy. Obstet Gynecol. 2000;95:704–709. doi: 10.1016/s0029-7844(00)00781-x. [DOI] [PubMed] [Google Scholar]
- 15.Lu L, Zhou D, Jian X, Deng J, Yang P, Ding W. Laparoscopic colorectomy for colorectal cancer: retrospective analysis of 889 patients in a single center. Tohoku J Exp Med. 2012;227:171–177. doi: 10.1620/tjem.227.171. [DOI] [PubMed] [Google Scholar]
- 16.Karsten J, Luepschen H, Grossherr M, Bruch HP, Leonhardt S, Gehring H, et al. Effect of PEEP on regional ventilation during laparoscopic surgery monitored by electrical impedance tomography. Acta Anaesthesiol Scand. 2011;55:878–886. doi: 10.1111/j.1399-6576.2011.02467.x. [DOI] [PubMed] [Google Scholar]
- 17.Luz CM, Polarz H, Böhrer H, Hundt G, Dörsam J, Martin E. Hemodynamic and respiratory effects of pneumoperitoneum and PEEP during laparoscopic pelvic lymphadenectomy in dogs. Surg Endosc. 1994;8:25–27. doi: 10.1007/BF02909488. [DOI] [PubMed] [Google Scholar]
- 18.Lim CH, Koh Y, Lee HW, Khil JY, Suh SO, Kim YC, et al. Effect of positive end expiratory pressure on intra-abdominal pressure and abdominal perfusion pressure at an increased intra-abdominal pressure. Korean J Anesthesiol. 2007;53:S31–S35. [Google Scholar]
- 19.Loeckinger A, Kleinsasser A, Hoermann C, Gassner M, Keller C, Lindner KH. Inert gas exchange during pneumoperitoneum at incremental values of positive end-expiratory pressure. Anesth Analg. 2000;90:466–471. doi: 10.1097/00000539-200002000-00042. [DOI] [PubMed] [Google Scholar]
- 20.Harris SN, Ballantyne GH, Luther MA, Perrino AC., Jr Alterations of cardiovascular performance during laparoscopic colectomy: a combined hemodynamic and echocardiographic analysis. Anesth Analg. 1996;83:482–487. doi: 10.1097/00000539-199609000-00007. [DOI] [PubMed] [Google Scholar]