Abstract
Background
In medically underserved regions such as Appalachia, cervical cancer incidence and mortality are higher than the general U.S. population; therefore, it is important for pediatricians to encourage parents to have their daughters vaccinated against the human papillomavirus (HPV). Unfortunately, little is known about the predictors of pediatricians’ encouragement of the HPV vaccine among medically underserved populations. The current study compared attitudes and behaviors of pediatricians with practices in Appalachia with those in non-Appalachia to identify potential strategies for reducing health disparities.
Methods
A survey was conducted with 334 pediatricians located in Appalachia and non-Appalachia counties to examine how prior behavior, perceived susceptibility, severity, self-efficacy, response-efficacy, and behavioral intentions are related to self-reported vaccine encouragement.
Results
Pediatricians in Appalachia perceived their patients to be less susceptible to HPV and reported lower rates of HPV encouragement than pediatricians in non-Appalachia. In addition, self-efficacy had a significant indirect association with vaccine encouragement for pediatricians in non-Appalachia.
Conclusion
This study’s findings emphasize the importance of increasing Appalachian pediatricians’ awareness of their patients’ susceptibility to HPV. Broader efforts to increase encouragement of the HPV vaccine among pediatricians should focus on promoting self-efficacy to encourage the HPV vaccine to parents of young females.
Introduction
Genital human papillomavirus (HPV) is a common sexually transmitted infection, with approximately 20 million men and women living in the United States currently infected and 6.2 million new cases (14–44 years old) each year (Dinh, Sternberg, Dunne, & Markowitz, 2008). Persistent HPV infection can cause a diverse range of health problems for women, with HPV types 6 and 11 causing more than 90% of genital warts, and HPV types 16 and 18 causing approximately 70% of cervical cancer cases (Dinh et al., 2008; Parkin, 2006). The U.S. Food and Drug Administration approved a quadrivalent vaccine in 2006 that protects women from HPV types 6, 11, 16, and 18 (Markowitz et al., 2010). In October of 2009, the U.S. Food and Drug Administration approved use of the quadrivalent HPV vaccine to prevent genital warts among males (U.S. Centers for Disease Control and Prevention, 2010) and recently approved the vaccine to prevent anal cancer among women and men (U.S. Food and Drug Administration, 2010). The quadrivalent HPV vaccine is administered in a three-shot series, is currently approved for females and males ages 9 to 26, and is most effective if administered before an individual initiates sexual activity (Markowitz et al., 2010; Zimet, 2005).
Among females, the ultimate success of the HPV vaccine in reducing genital warts and cervical cancer depends largely on the extent to which pediatricians recommend the vaccine and whether parents are willing to have their daughters vaccinated. The research conducted to date seems promising on both accounts. Overall, pediatricians report positive attitudes toward the HPV vaccine, but frequently report some concerns about parents’ willingness to vaccinate their daughters (Daley et al., 2006; Duval et al., 2007; Esposito et al., 2007). Among providers who do not strongly recommend the vaccine, the commonly reported barriers include a lack of time to discuss HPV vaccination, the cost of the vaccine, and perceived parental concerns about vaccine efficacy (Daley et al., 2010). Although pediatricians commonly consider parents a potential barrier to HPV vaccination, studies have shown that parents of female adolescents generally report positive attitudes and intentions toward vaccinating their daughters against HPV (Allen et al., 2010; Barnack, Reddy, & Swain, 2010; Constantine & Jerman, 2007; Rosenthal et al., 2008).
Given the seemingly positive pediatrician and parental perceptions of the HPV vaccine, it is not surprising that vaccination rates among female adolescents are on the rise (Dorell, Yankey, Cohn, & Markowitz, 2010). However, not all females are getting vaccinated at uniform rates. Recent research has identified significant socioeconomic and geographic health disparities regarding the initiation and completion of HPV vaccination. At the individual level, uninsured females are less likely to initiate vaccination (Schluterman, Terplan, Lydecker, & Tracy, 2011) and complete the three-shot HPV vaccine series (Chou, Krill, Horton, Barat, & Trimble, 2011; Widdice, 2011) than those with private or public health insurance. At the community level, there are mixed findings regarding the association between poverty and HPV vaccination rates. A recent study of vaccination rates in six states found HPV vaccination was negatively associated with living in a state with higher poverty rates, but positively associated with living in an impoverished county (Pruitt & Schootman, 2010). This suggests that states with high poverty have fewer resources to support HPV vaccination, but any state funds that are available for this purpose are being distributed to the most impoverished counties.
Thus, there is an apparent disparity between the high rates of vaccination in the general population and those of the medically underserved. Understanding vaccine recommendation behaviors among pediatricians practicing in underserved areas is vital because parents are more likely to initiate HPV vaccination if a pediatrician recommends it. Although receiving a recommendation from a pediatrician is an important predictor of HPV vaccination, a recent study found that only 22% of parents living in underserved counties in North Carolina report receiving one (Reiter, Brewer, Gottlieb, McRee, & Smith, 2009). It is unknown what factors are associated with this low rate of vaccine recommendation behaviors. One possibility is that pediatricians working in underserved areas do not perceive their patients to be at risk for HPV. Alternatively, they may perceive their patients to be at risk, but perceive recommending the vaccine to their patients or their parents to be difficult. This suggests the need for additional research on the factors that lead not only to pediatricians’ intention to recommend the vaccine, but also to whether they follow through with encouraging their female patients to be vaccinated. Thus, the purpose of this study is to examine the predictors of pediatricians’ intentions and behaviors regarding encouraging parents to get their 9- to 17-year-old daughters vaccinated against HPV.
Understanding pediatricians’ vaccine encouragement behaviors is particularly important in certain geographic regions of the United States, such as the medically underserved counties surrounding the foothills of the Appalachian mountains. People living in Appalachia experience a number of health inequities because of the complex interplay of higher poverty rates, lower levels of educational attainment, shortages of health care providers, limited availability of local health care facilities, and an elevated burden of disease (Halverson, Barnett & Casper, 2002; Halverson, Ma, & Harner, 2004). One health inequity that is of particular concern in the Appalachian region is the increased cervical cancer incidence and mortality rates (Hopenhayn, King, Christian, Huang, & Christian, 2008; Huang et al., 2002). Pediatricians can play an important role in reducing the cervical cancer inequities in the Appalachian region by encouraging parents to have their daughters vaccinated.
One factor that is likely to influence whether pediatricians practicing in Appalachia recommend the vaccine is the extent to which they are aware that their patients are at higher risk for cervical cancer. If so, it would be expected that pediatricians with practices in Appalachia would be more likely to recommend the HPV vaccine than their non-Appalachia counterparts. However, it is also possible that pediatricians are reluctant to recommend the vaccine because of certain social and cultural characteristics of the region that may negatively influence HPV vaccine uptake in Appalachia (Hopenhayn, Christian, Christian, & Schoenberg, 2007; Katz et al., 2009). For example, pediatricians with practices in Appalachian counties may have more concerns than those in non-Appalachia that parents will have negative attitudes toward the vaccine or be less able to afford it. Thus, we also examine potential differences between pediatricians practicing in Appalachian and non-Appalachian counties with regard to perceptions, intentions, and vaccine recommendation behaviors. In particular, we focus on threat and efficacy in relation to intention and behavior as specified in the risk perception attitude (RPA) framework.
The RPA framework is a theoretical perspective for understanding the effects of perceived risk and efficacy on behavior change (Rimal & Real, 2003). Perceived risk is composed of an individual’s perceptions of both susceptibility and severity and is a known motivator for behavioral action (Rimal & Real, 2003; Witte, 1992). Perceived susceptibility (or vulnerability to a given threat) refers to the likelihood that the threat will occur. Perceived severity of the threat refers to the seriousness of the consequences of the threat. The theory posits that people are most motivated to reduce risk when both vulnerability and severity are high. Consistent with this notion, perceptions of HPV severity have been found to significantly predict intention to be vaccinated (Kahn et al., 2008). Although previous research concerned with the influence of perceived risk and efficacy have traditionally focused on individuals (Witte, Berkowitz, Cameron, & Lillie, 1998; Witte & Morrison, 1995), recent research suggests that perceiving risk to others, rather than self, can effectively produce behavior change (Morrison, 2005).
The two primary barriers to reducing a risk posed by a health threat are low levels of response or self-efficacy (Rimal & Real, 2003). Response-efficacy refers to the perceived safety and effectiveness of the recommended behavior, such as potential side effects of the HPV vaccine and how long it will provide protection against HPV infections. Pediatricians who report concerns about the perceived effectiveness and safety of the HPV vaccine have decreased intentions to recommend the vaccine to parents (Feemster, Winters, Fiks, Kinsman, & Kahn, 2008). Self-efficacy refers to whether a person has the necessary skills and resources to engage in the recommended behavior, such as the ability to encourage parents to vaccinate their daughters against HPV. For example, a pediatrician who believes that she or he does not have the time to explain the HPV vaccine to parents is one factor that might foster feelings of low self-efficacy (Daley et al., 2010).
Perceived risk to others has been shown to motivate intentions and behaviors in a variety of contexts, including an unknown other, personal relationships, and physician–patient interactions (Lindsey, 2005; Morrison, 2005; Roberto & Goodall, 2009). For example, a recent study demonstrated that primary care physicians’ were more likely to recommend a routine kidney function test for patients when they perceived kidney disease to be a potential threat to the health of their patients and had confidence in the efficacy of the test and their own ability to perform the test (Roberto & Goodall, 2009). Similarly, it might be expected that pediatricians who perceive HPV to be a significant threat to their female patients and have confidence in the efficacy of the vaccine and their ability to encourage parents to vaccinate their daughters are likely to recommend that their female patients be vaccinated against HPV.
Methods
Procedures, Response Rate, and Sample Characteristics
Procedures
Data collection procedures were guided by the tailored design method (Dillman, 2006) and approved by our institutional review board. Each pediatrician was contacted up to four times in an effort to get a survey returned (although once a pediatrician returned the survey, he or she was removed from the mailing list and did not receive subsequent mailings). The initial contact consisted of mailing a prenotification postcard in May 2009, which informed the pediatricians to expect the survey within the next few days. The second contact included a consent form, a survey, and a business reply envelope so pediatricians could return the survey to the researchers at no cost. Approximately 2 weeks later, reminder postcards were sent to all pediatricians who had not yet returned the survey. Approximately 1 week later, a second copy of the consent form, survey, and another business reply envelope were sent. A follow-up postcard with one question was mailed to all participants 30 days after receiving their completed survey.
Response rate
Using these procedures, the initial survey was mailed to all physicians with a pediatrics specialty (n = 984) listed in a database of primary care providers in Kentucky and West Virginia. The response rate was calculated as the number of surveys returned divided by the number of surveys that were sent out and not returned as undeliverable (n = 43). A total of 334 pediatricians completed and returned this survey, for an overall response rate of 35.5%. A total of 222 pediatricians completed and returned the 30-day follow-up postcard for a response rate of 66.5%. This sample size and response rate compares favorably to those obtained in other survey studies of physicians (Roberto, Krieger, Katz, Goei, & Jain, 2011; Roberto & Goodall, 2009).
Sample characteristics
The final sample consisted of 334 pediatricians (n = 129 with practices located in Appalachia; n = 205 with practices located in non-Appalachia). The sample was 57.4% female, and the mean years as a practicing pediatrician was 16.89 (SD = 12.53). Pediatricians reported their race as 83.0% White, 9.6% Asian or Pacific Islander, 2.3% African American, and 5.1% “other” (e.g., American Indian, Asian Indian, Middle Eastern). In addition, 7 participants (2.3%) reported their ethnicity as Hispanic. Pediatricians practicing in Appalachia were significantly more likely than pediatricians practicing in non-Appalachia to report being a member of a racial or ethnic minority group (31.4% vs. 11.6%; χ2 = 18.66; p < .001). Participants reported that approximately 23% of their patients were girls between the ages of 9 and 17.
Measures
Pediatrician perceptions of threat and efficacy were measured using items from Witte, Cameron, McKeon, and Berkowitz’s (1996) Risk Behavior Diagnostic Scale. Pediatrician perceptions of parent response-efficacy and self-efficacy were measured using slightly modified versions of the Risk Behavior Diagnostic Scale (i.e., these items asked pediatricians about their perceptions of their patients’ levels of threat and efficacy, rather than perceptions of threat and efficacy to the pediatricians themselves). Similar modifications have been successfully used in several other studies (Lindsey, 2005; Morrison, 2005; Roberto et al., 2011), including two studies on another topic using two different physician samples (Roberto et al., 2011; Roberto & Goodall, 2009). Response categories for these items ranged from “strongly disagree” to “strongly agree” on a 7-point scale. For means, standard deviations, and bivariate correlations, see Table 1.
Table 1.
Means, Standard Deviations, and Bivariate Correlations
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PPENCOUR | 5.11 (1.53) | – | |||||||||||
| 2. PPSUS | 6.56 (.84) | .28** | – | ||||||||||
| 3. PPSEV | 5.96 (1.13) | .13* | .39** | – | |||||||||
| 4. PPSEFF | 6.14 (1.01) | .43** | .48** | .38** | – | ||||||||
| 5. PVREF | 6.33 (.96) | .32** | .45** | .41** | .63** | – | |||||||
| 6. PARSEFF | 6.32 (1.01) | .43** | .45** | .28** | .46** | .46** | – | ||||||
| 7. PARVREF | 5.09 (.92) | .28** | .21** | .17** | .50** | .42** | .44** | – | |||||
| 8. PINT | 6.32 (1.29) | .64** | .43** | .29** | .66** | .55** | .52** | .41** | – | ||||
| 9. PENCOURF | 5.11 (1.53) | .75** | .25** | .18** | .33** | .27** | .33** | .20** | .60** | – | |||
| 10. PATIENT | 22.85 (12.29) | .05 | −.07 | .11 | −.01 | −.04 | .04 | .07 | −.02 | .15* | – | ||
| 11. LOCATION | 1.11 (.39) | −.40** | −.19** | −.07 | −.14* | −.18** | −.38** | −.21** | −.28** | −.37** | −.04 | – | |
| 12. YEARS | 16.89 (12.53) | .01 | −.07 | .05 | .09 | .10 | −.08 | .05 | −.01 | .05 | .07 | .04 | – |
Abbreviations: PPENCOUR, pediatricians’ past HPV vaccine encouragement; PPSUS, pediatricians’ perceived patients’ susceptibility; PPSEV, pediatricians’ perceived patients’ severity; PPSEFF, pediatricians’ perceived self-efficacy to encourage patients; PVREF, pediatricians’ perceived vaccine response-efficacy; PARSEFF, pediatricians’ perception of parents’ self efficacy; PARVREF, pediatricians’ perception of parents’ vaccine response-efficacy; PINT, pediatricians’ intention to encourage parents to have patients vaccinated; PENCOURF, extent to which pediatricians encouraged parents to have patients vaccinated (follow-up).
p < .05.
p < .01.
Perceived patient severity was measured using two items: “Having HPV would be very harmful to my patients’ health” and “Having HPV would be a very severe threat to my patients’ health” (r = 0.60; p < .05; Cronbach’s α = 0.75). Perceived patient susceptibility was measured using the following two statements: “My patients are at risk of getting HPV at some point in their lives” and “My patients are susceptible to getting HPV at some point in their lives” (r = 0.83; p < .05; Cronbach’s α = 0.91). Pediatrician’s self-efficacy was assessed using the statements, “It would be easy for me to encourage the parents of my patients to get their daughters vaccinated against HPV,” and “I would be comfortable encouraging the parents of my patients to get their daughters vaccinated against HPV” (r = 0.54; p < .05; Cronbach’s α = 0.68). Pediatrician’s vaccine response-efficacy was measured using the items, “Encouraging the parents of my patients to get their daughters vaccinated against HPV would be an effective way to get them to do so,” and “Encouraging the parents of my patients to get their daughters vaccinated against HPV would be a good way to get them to do so” (r = 0.85; p < .05; Cronbach’s α = 0.92). Perceived parent vaccine response-efficacy was measured by asking pediatricians to respond to the following items: “The parents of my patients think the HPV vaccine is safe” and “The parents of my patients think the HPV vaccine is effective (r = 0.57; p < .05; Cronbach’s α = 0.72). Finally, perceived parent self-efficacy was measured by asking, “The parents of my patients have the ability to get their daughters vaccinated against HPV if they want to” and “It would be easy for the parents of my patients to get their daughters vaccinated against HPV if they want to” (r = 0.74; p < .05; Cronbach’s α = 0.85). Intention to encourage the HPV vaccine was measured using the following question: “In the next 30 days, I intend to regularly encourage the parents of my 9 to 17 year old female patients to get their daughters vaccinated against HPV.”
Past HPV vaccine encouragement was measured by asking pediatricians, “In the PAST 30 days, approximately how often have you encouraged the parents of your 9 to 17 year old female patients to get their daughters vaccinated against HPV? Pediatricians responded on a 6-point scale (1 = 0% of the time to 6 = 81%–100% of the time).
HPV vaccine encouragement (i.e., Time 2 behavior) was measured 30 days after pediatricians completed the initial survey. They were sent a follow-up postcard that asked: “In the past 30 days, approximately how often have you encouraged the parents of your 9 to 17 year old female patients to get their daughters vaccinated against HPV?” Response options ranged from 1 (0% of the time) to 6 (81%–100% of the time).
To assess this study’s measurement integrity, we examined a full measurement model with confirmatory factor analysis. All constructs and their corresponding indicators were included in the model as latent factors. Further, control variables (percent of pediatricians’ female patients between the ages of 9 and 17 and the distance from the physicians’ office to where the HPV vaccine is available) and HPV vaccine encouragement at times 1 and 2 were included in the model. All latent factors and observed variables were correlated. This model was evaluated based on Hu and Bentler’s (1999) guidelines for model fit. A model is considered a reasonable approximation of the data when the root mean square error of approximation (RMSEA) is smaller than 0.06, the comparative fit index (CFI) is greater than 0.95, and the standardized root mean square residual (SRMR) is smaller than 0.08. Using such criteria, we found that the full measurement model fit the data well (χ2[69] = 129.13; p < .05; RMSEA = 0.05; 90% confidence interval [CI] = 0.037–0.065; CFI = 0.96; SRMR = 0.03), and the standardized factor loadings for all latent factors were greater than 0.60. Thus, the confirmatory factor analysis results provided support for the validity of the measures in operationalizing their corresponding constructs.
Analysis Summary
For the first research question, independent sample t-tests were conducted to determine whether significant mean differences existed among Appalachian and non-Appalachian physicians with respect to threat, efficacy, intention, and encouragement. To examine the hypothesis and second research question, a mediation model was analyzed in Mplus 6.0 (Muthén & Muthén, 1998–2007), using multigroup path analysis and bootstrapping. The percent of pediatricians’ female patients between the ages of 9 and 17, as well as the distance from the physicians’ office to where the HPV vaccine was available were included as control variables in the analyses. With respect to the missingness, full information maximum likelihood was employed, as suggested by Graham (2009) and Graham, Cumsille, and Elek-Fisk (2003). The threat, efficacy, and intention variables had less than 5% missing data.
This study simultaneously examined the hypothesized RPA mediation model, while also determining whether the model operated differently based on pediatricians practicing in Appalachian counties compared with pediatricians practicing in non-Appalachian counties. First, a restricted mediation model was analyzed, examining paths from independent variables to dependent variables through potential mediators (Preacher & Hayes, 2008). For the restricted mediation model, all parameters were held equal across groups. Afterward, an unrestricted mediation model was examined, allowing the parameters to be freely estimated across groups. The models were evaluated based on Hu and Bentler’s (1999) model fit criteria. A χ2 difference test was then employed to determine whether the unrestricted mediation model significantly improved the model fit (Kline, 2005). When conducting the multigroup mediation analyses, bootstrap bias-corrected CIs were obtained, with the number of bootstrapping set to 5000. Indirect associations were considered significant when zero was not within the 95% CI.
Results
The first research question investigated whether pediatricians practicing in Appalachia and pediatricians practicing in non-Appalachia differ with regard to perceived susceptibility, severity, self-efficacy, response-efficacy, and vaccine encouragement. Significant mean differences were detected between pediatricians practicing in Appalachia counties compared with pediatricians practicing in non-Appalachia counties with respect to pediatricians’ perceived patient susceptibility [t(208) = 2.17; p < .05] and pediatricians’ past HPV vaccine encouragement [t(227) = 2.33; p < .05]. Pediatricians in Appalachia reported significantly lower means compared with pediatricians in non-Appalachia for susceptibility (M = 6.43, SD = 1.0 vs. M = 6.65, SD = 0.72) and past encouragement (M = 4.85, SD = 1.7 vs. M = 5.28, SD = 1.4). No other significant differences were found.
In this study, we also hypothesized that, from a RPA mediation framework, pediatricians’ own perceived susceptibility, severity, self-efficacy, response-efficacy, perceived parental self-efficacy, and perceived parent response-efficacy are positively related to their intention to recommend the HPV vaccine, which in turn, is positively related wit HPV vaccine encouragement. Relatedly, the second research question asked if the proposed RPA mediation model operates differently for pediatricians practicing in Appalachia and pediatricians practicing in non-Appalachia. To address this hypothesis and research question, a restricted model was examined, which did not fit the data well (χ2[64] = 116.29; p < .05; RMSEA = 0.07; 90% CI = 0.05–0.09; CFI = 0.96; SRMR = 0.09) based on the RMSEA and SRMR. Afterward, an unrestricted model was analyzed: (χ2[24] = 43.61; p < .05; RMSEA = 0.07; 90% CI = 0.04–0.10; CFI = 0.99; SRMR = 0.03). Although the RMSEA was slightly greater than 0.06, the CFI and SRMR met Hu and Bentler’s guidelines for model fit. A χ2 difference test was then employed to determine whether the unrestricted model significantly improved the model fit: χ2diff(40) = 72.68 (p < .05). Given that the difference in χ2 value and degrees of freedom was significant, the unrestricted model significantly improved the model fit; therefore, significant group differences exist (Kline, 2005).
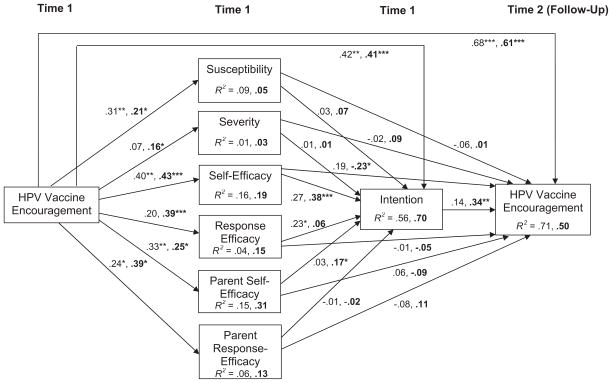
As seen in Figure 1 of the unrestricted model, the effect sizes were small for perceived susceptibility, severity, self-efficacy, and response-efficacy, as well as for perceived parent self-efficacy and perceived parent response-efficacy, regardless of whether pediatricians had practices in Appalachian or non-Appalachian regions (Cohen, 1988). For intention and HPV vaccine encouragement, the effect sizes were medium for both Appalachian and non-Appalachian pediatricians. When inspecting the hypothesized associations in the unrestricted model, significant indirect associations were not found among pediatricians in Appalachia, according to the bias-corrected bootstrap CIs (Table 2). For pediatricians in non-Appalachia, however, self-efficacy mediated the association between past vaccine encouragement and their intention to encourage patients to get the vaccine in the future. Further, intention mediated the association between self-efficacy and encouraging patients to obtain the HPV vaccine at the follow-up.
Figure 1.
A multigroup analysis of RPA among pediatricians (pediatricians in Appalachia first, pediatricians in non-Appalachia second and in bold).
Note. *p < .05, **p < .01, ***p < .001. Path coefficients are completely standardized. Although not shown here, the percent of pediatricians’ female patients between the ages of 9 and 17, as well as the distance from the pediatricians’ office to where the HPV vaccine was available were included as control variables. The threat and efficacy variables also were correlated.
Table 2.
Indirect Associations based on the Bias-corrected Bootstrap Confidence Intervals
| Non-Appalachian Pediatricians
|
Appalachian Pediatricians
|
||||
|---|---|---|---|---|---|
| Parameters | Standard Indirect Association | Standard 95% CI | Parameters | Standard Indirect Association | Standard 95% CI |
| PPENCOUR → PPSUS → PINT | .016 | −.019, .051 | PENCOUR → PPSUS → PINT | .009 | −.053, .071 |
| PPENCOUR → PPSEV → PINT | .000 | −.019, .019 | PENCOUR → PPSEV → PINT | .001 | −.012, .014 |
| PPENCOUR → PPSEFF → PINT | .162* | .072, .251 | PENCOUR → PPSEFF → PINT | .109 | −.033, .251 |
| PPENCOUR → PVREF → PINT | .024 | −.037, .085 | PENCOUR → PVREF → PINT | .045 | −.020, .111 |
| PPENCOUR → PARSEFF → PINT | .042 | −.014, .098 | PENCOUR → PARSEFF → PINT | .010 | −.060, .081 |
| PPENCOUR → PARVREF → PINT | −.004 | −.024, .017 | PENCOUR → PARVREF → PINT | −.001 | −.053, .052 |
| PPSUS → PINT → ENCOURF | .025 | −.031, .081 | PPSUS → PINT → ENCOURF | .004 | −.046, .054 |
| PPSEV → PINT → ENCOURF | .000 | −.037, .038 | PPSEV → PINT → ENCOURF | .002 | −.024, .028 |
| PPSEFF → PINT → ENCOURF | .129* | .023, .236 | PPSEFF → PINT → ENCOURF | .037 | −.072, .146 |
| PVREF → PINT → ENCOURF | .021 | −.034, .077 | PVREF → PINT → ENCOURF | .031 | −.059, .121 |
| PARSEFF → PINT → ENCOURF | .058 | −.018, .135 | PARSEFF → PINT → ENCOURF | .004 | −.046, .054 |
| PARVREF→ PINT → ENCOURF | −.006 | −.037, .035 | PARVREF→ PINT → ENCOURF | .000 | −.049, .049 |
Significant indirect associations (zero is not within the CI).
Discussion
The purpose of this study was to examine the applicability of RPA to a pediatrician sample and to assess whether this theoretical framework functioned differently for pediatricians practicing in Appalachian and non-Appalachian counties. When the pediatricians in Appalachia and non-Appalachia were compared on the key RPA constructs, we found that pediatricians practicing in Appalachian counties reported significantly lower perceptions of self-efficacy and reported encouraging the vaccine significantly less frequently as compared with pediatricians practicing in non-Appalachian counties at time 1. The finding that pediatricians in Appalachia report greater difficulty recommending the HPV vaccine to parents than their non-Appalachian counterparts may reflect religious, political, and geographic elements of Appalachian culture. For example, Katz et al. (2009) conducted focus groups in the Appalachian region and identified common concerns associated with the HPV vaccine, including the belief that the HPV vaccine promotes promiscuity and that young women who received the vaccine would become the focus of community gossip. If so, pediatricians in Appalachia may be recommending the vaccine less often owing to concerns about offending parents of their patients. From a pediatrician’s perspective, it may seem more prudent to avoid mentioning the HPV vaccine than risk offending a parent who might respond by changing providers or refusing to allow their daughter to receive other types of preventive care.
Differences in Appalachian and non-Appalachian pediatricians perceptions of self-efficacy is important because efficacy is theoretically predicted to influence behavioral intentions. We examined this relationship by examining how well the entire RPA model predicted HPV vaccine recommendation intentions and behaviors. Among pediatricians in non-Appalachian counties, prior vaccine encouragement was positively related to pediatricians’ perceptions of the threat HPV poses for their patients, their own perceptions of self-efficacy and HPV vaccine response-efficacy, as well as the perceived self-efficacy and HPV vaccine response-efficacy for parents of their patients. Self-efficacy and perceived parent self-efficacy were positively related with intentions to encourage the vaccine, and intentions were positively related to reported vaccine encouragement behavior at time 2. Theoretically, we should have observed a number of indirect associations, such as behavioral intentions mediating the relations between the threat and efficacy variables (i.e., perceived patient susceptibility, perceived patient severity, pediatrician’s self-efficacy, pediatrician’s vaccine response-efficacy, perceived parent self-efficacy, and perceived parent vaccine response-efficacy) and vaccine recommendation behaviors. However, the only significant indirect associations were for prior vaccine encouragement with intentions to encourage vaccination (mediated by self-efficacy), and for self-efficacy with self-reported encouragement behaviors at time 2 (mediated by time 1 intentions). In other words, prior vaccine encouragement was significantly associated with intentions to recommend the HPV vaccine to parents, in part, through self-efficacy. Similarly, self-efficacy was positively related to time 2 vaccine encouragement by, in part, intentions to recommend the vaccine.
Among Appalachian pediatricians, prior vaccine encouragement was positively related to perceptions of susceptibility, self-efficacy, and parental self-efficacy and response-efficacy. Only response-efficacy was related to intentions to encourage vaccination, but intentions were not significantly related to time 2 reports of vaccine encouragement. Surprisingly, none of the indirect associations were significant. One potential explanation for the observed differences between Appalachian and non-Appalachian pediatricians regarding the associations is that Appalachian pediatricians were significantly more likely to be racial and ethnic minorities (including international medical graduates). Future studies should consider how perceived cultural and linguistic differences influence the extent to which pediatricians feel comfortable recommending the HPV vaccine to parents (Jain & Krieger, 2011).
The results of this study have important theoretical and practical implications. First, this study adds to the growing body of literature that suggests that perceived risk to other can be a meaningful motivator for behavior. In this case, pediatricians can be motivated to engage in behaviors (i.e., vaccine encouragement) on behalf of another (i.e., their patients). Unlike the theoretical predictions of the RPA, however, perceived susceptibility and perceived severity of HPV were not significantly associated with intentions to encourage parents to have their daughters vaccinated. Although perceived risk was not found to be a significant predictor in the RPA model with this sample, there were important differences between pediatricians in Appalachia and non-Appalachia regarding perceived susceptibility. Given that rates of cervical cancer incidence and mortality are elevated in Appalachia, it would be expected that pediatricians in Appalachia would rate the perceived susceptibility of their patients to HPV as being higher than their non-Appalachian counterparts. On the contrary, Appalachian pediatricians perceived their patients’ susceptibility to HPV as being lower than pediatricians in non-Appalachia counties. This finding suggests that future interventions should include education for pediatricians about the increased cervical cancer incidence and mortality rates among women living in Appalachia.
Second, this study reinforces previous findings (Krieger, Kam, Katz, & Roberto, 2011) that efficacy is a key consideration in promoting communication about HPV. In this study, self-efficacy was the only intermediary variable that had a significant indirect relation to behavior. This finding was only significant for pediatricians in non-Appalachia counties. Nonetheless, the importance of self-efficacy for predicting vaccine encouragement behavior indicates that interventions to promote vaccine encouragement among pediatricians should emphasize communication skills training so that pediatricians’ can gain the required confidence to encourage parents to vaccinate their adolescent daughters against HPV without increasing visit length (Heritage, Robinson, Elliot, Beckett, & Wilkes, 2007).
This investigation benefits from at least three key strengths. First, it is theory based and extends the scope of the RPA framework to a topic (the HPV vaccine) and target audience (pediatricians) that have not been studied previously using this theory. Second, it focuses on a health topic associated with significant health inequity in the Appalachian region. Third, the rigor associated with our data collection procedures and statistical analyses provides a high level of confidence in the results. For example, our survey was designed using procedures outlined by Witte et al. (1996) and data were collected using Dillman’s (2006) Tailored Design Method.
As with any investigation, some potential limitations must be noted. One potential limitation is the sample and response rate. Information on the type of practice of the participants was not collected as part of this study, so we were unable to test whether any differences in vaccine recommendation behavior exist between pediatricians in public clinics versus private practices. Few studies have examined the influence of practice type on vaccine recommendation behavior, and this would be potentially fruitful area for future research to explore. A second limitation is that the response rate was not as high as we would have liked. However, we do not believe this is a significant cause for concern for at least two reasons. Because of increasing demands on and competition for their time, physician response rates have fallen dramatically over the past decade, and low response rates are typical when conducting surveys with randomly selected samples of physicians (Harbaugh, 2002; Tambor et al., 1993). In addition, although the response rate was seemingly low, our response rates and sample size were larger than other studies that include physicians as research participants (Roberto, Krieger, Katz, Goei, & Jain, 2011; Roberto & Goodall, 2009).
A third potential limitation is methodological. We asked pediatricians to report on their HPV vaccination intentions and behaviors for female patients age 9 to 17. It is possible that pediatrician responses may have varied if asked about specific age groups within this range (Daley et al., 2010). Furthermore, although the independent variables were measured using a 7-point scale to increase variability, the means for the threat and efficacy scales were fairly high. It is possible that statistical relations were suppressed owing to ceiling effects. Future studies should explore possible solutions for increasing variability in the data. This may be especially challenging with physician populations in which perceived threat for health risks like HPV can be expected to high.
In conclusion, this study demonstrated that pediatricians practicing in Appalachian counties perceive their patients at lower risk for HPV than do pediatricians practicing in non-Appalachian counties. This is potentially problematic given the greater rates of cervical cancer incidence and mortality among women living in the Appalachian region. In addition, this is the first investigation to consider not only predictors of pediatricians’ intentions to encourage parents to have their daughters vaccinated against HPV, but also their encouragement behaviors. The findings indicate that perceived self-efficacy for encouraging parents to vaccinate their adolescent daughters against HPV had a significant, positive indirect association with vaccine encouragement at a 30-day follow-up among pediatricians in non-Appalachia counties. This suggests that future interventions should focus on building pediatricians’ ability to communicate clearly and effectively with parents about the benefits of the HPV vaccine.
Acknowledgments
Supported by a grant from The Ohio State University Coordinating Committee for the Population and Health: Targeted Investments in Excellence Initiative (PI: Krieger), National Cancer Institute Grants K07 CA107079 (MLK), and the Behavioral Measurement Shared Resource at The Ohio State University Comprehensive Cancer Center, P30 CA016058.
Biographies
Janice L. Krieger, PhD, is an Assistant Professor in the School of Communication at The Ohio State University. Her research examines interpersonal communication and social influence in health contexts, with a focus on understanding how communication can help reduce health inequities.
Mira L. Katz, MPH, PhD, is an Associate Professor in the Division of Health Behavior and Health Promotion in the College of Public Health at The Ohio State University. Her research interest includes communication issues associated with cancer prevention, early detection, and survivorship.
Jennifer A. Kam, PhD, is an Assistant Professor in the Department of Communication at the University of Illinois, Urbana-Champaign. She examines the effects of cultural stressors on adolescents’ mental and behavioral health. She also studies the protective nature of interpersonal communication.
Anthony Roberto, PhD, is an Associate Professor in the Hugh Downs School of Human Communication at Arizona State University. His research and teaching interests focus primarily on social influence and health communication.
References
- Allen JD, Othus M, Shelton RC, Li Y, Norman N, Tom L, et al. Parental decision making about the HPV vaccine. Cancer Epidemiology, Biomarkers, & Prevention. 2010;19:2187–2198. doi: 10.1158/1055-9965.EPI-10-0217. [DOI] [PubMed] [Google Scholar]
- Barnack JL, Reddy DM, Swain C. Predictors of parents’ willingness to vaccinate for human papillomavirus and physicians’ intentions to recommend the vaccine. Women’s Health Issues. 2010;20:28–34. doi: 10.1016/j.whi.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Chou B, Krill LS, Horton BB, Barat CE, Trimble CL. Disparities in human papillomavirus vaccine completion among vaccine initiators. Obstetrics & Gynecology. 2011;118:14–20. doi: 10.1097/AOG.0b013e318220ebf3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Constantine NA, Jerman P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: A representative statewide analysis. Journal of Adolescent Health. 2007;40:101–103. doi: 10.1016/j.jadohealth.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Babbel C, et al. A national survey of pediatrician knowledge and attitudes regarding human papillomavirus vaccination. Pediatrics. 2006;118:2280–2289. doi: 10.1542/peds.2006-1946. [DOI] [PubMed] [Google Scholar]
- Daley MF, Crane LA, Markowitz LE, Black SR, Beaty BL, Barrow J, et al. Human papillomavirus vaccination practices: A survey of U.S. physicians 19 months after licensure. Pediatrics. 2010;126:425–433. doi: 10.1542/peds.2009-3500. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and internet surveys: The tailored design method. 2. New York: Wiley; 2006. updated. [Google Scholar]
- Dinh T, Sternberg M, Dunne EF, Markowitz L. Genital warts among 18- to 59-year-olds in the United States, National Health and Nutrition Examination Survey, 1999–2004. Sexually Transmitted Diseases. 2008;35:357–360. doi: 10.1097/OLQ.0b013e3181632d61. [DOI] [PubMed] [Google Scholar]
- Dorell C, Yankey D, Cohn A, Markowitz L. National, state, and local area vaccination coverage among adolescents aged 13–17 years—United States, 2009. Morbidity and Mortality Weekly Report (MMWR) 2010;59:1018–1023. [PubMed] [Google Scholar]
- Duval B, Gilca V, McNeil S, Dobson S, Money D, Gemmill IM, et al. Vaccination against human papillomavirus: A baseline survey of Canadian clinicians’ knowledge, attitudes, and beliefs. Vaccine. 2007;25:7841–7847. doi: 10.1016/j.vaccine.2007.08.041. [DOI] [PubMed] [Google Scholar]
- Esposito S, Bosis S, Pelucchi C, Begliatti E, Rognoni A, Bellasio M, et al. Pediatrician knowledge and attitudes regarding human papillomavirus disease and its prevention. Vaccine. 2007;25:6437–6446. doi: 10.1016/j.vaccine.2007.06.053. [DOI] [PubMed] [Google Scholar]
- Feemster KA, Winters SE, Fiks AG, Kinsman S, Kahn J. Pediatricians’ intention to recommend human papillomavirus (HPV) vaccines to 11-to 12-year-old girls postlicensing. Journal of Adolescent Health. 2008;43:408–411. doi: 10.1016/j.jadohealth.2008.06.012. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Graham JW, Cumsille PE, Elek-Fisk E. Methods of handling missing data. In: Schinka JA, Velicer WF, editors. Research Methods in Psychology. New York: John Wiley & Sons; 2003. pp. 87–114. [Google Scholar]
- Halverson JA, Barnett E, Casper M. Geographic disparities in heart disease and stroke mortality among black and white populations in the Appalachian region. Ethnicity & Disease. 2002;12(Suppl 3):82–91. [PubMed] [Google Scholar]
- Haverson J, Ma L, Harner EJ. An analysis of disparities in health status and access to care in the Appalachian region. Washington, DC: Appalachian Regional Commission; 2004. Available from: http://www.arc.gov/index.do?nodeId=2467&print=yes. [Google Scholar]
- Harbaugh R. Proven lessons for generating good mail survey response rates from physicians. Medical Marketing and Media. 2002;37:3–7. [Google Scholar]
- Heritage J, Robinson JD, Elliot MN, Beckett M, Wilkes M. Reducing patients’ unmet concerns in primary care: The difference one word can make. Journal of General Internal Medicine. 2007;22:1429–1433. doi: 10.1007/s11606-007-0279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopenhayn C, Christian A, Christian WJ, Schoenberg NE. Human papillomavirus vaccine: Knowledge and attitudes in two Appalachian Kentucky counties. Cancer Causes and Control. 2007;18:627–634. doi: 10.1007/s10552-007-9007-7. [DOI] [PubMed] [Google Scholar]
- Hopenhayn C, King JB, Christian A, Huang B, Christian WJ. Variability of cervical cancer rates across 5 Appalachian states, 1998–2003. Cancer. 2008;113(Suppl 10):2974–2980. doi: 10.1002/cncr.23749. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Huang B, Wyatt S, Tucker T, Bottorff D, Lengerich E, Hall HI. Cancer death rates-Appalachia 1994–1998. Morbidity and Mortality Weekly Report (MMWR) 2002;51:527–529. [PubMed] [Google Scholar]
- Jain P, Krieger JL. Moving beyond the language barrier: The communication strategies used by international medical graduates in intercultural medical encounters. Patient Education & Counseling. 2011;84:98–104. doi: 10.1016/j.pec.2010.06.022. [DOI] [PubMed] [Google Scholar]
- Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet G. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstetrics & Gynecology. 2008;111:1103–1110. doi: 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- Katz ML, Reiter PL, Heaner S, Ruffin MT, Post DM, Paskett ED. Acceptance of the HPV vaccine among women, parents, community leaders, and healthcare providers in Ohio Appalachia. Vaccine. 2009;27:3945–3952. doi: 10.1016/j.vaccine.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 2005. [Google Scholar]
- Krieger JL, Kam J, Katz M, Roberto AJ. Does mother know best? An actor-partner model of college-age females’ HPV vaccination behavior. Human Communication Research. 2011;37:107–124. [Google Scholar]
- Lindsey LLM. Anticipated guilt as behavioral motivation: An examination of appeals to help unknown others through bone marrow donation. Human Communication Research. 2005;31:453–481. [Google Scholar]
- Markowitz LE, Hariri S, Unger ER, Saraiya M, Datta D, Dunne EF. Post-licensure monitoring of the HPV vaccine in the United States. Vaccine. 2010;28:4731–4737. doi: 10.1016/j.vaccine.2010.02.019. [DOI] [PubMed] [Google Scholar]
- Morrison K. Motivating women and men to take protective action against rape: Examining direct and indirect persuasive fear appeals. Health Communication. 2005;18:237–256. doi: 10.1207/s15327027hc1803_3. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- Parkin DM. The global health burden of infection-associated cancers in the year 2002. International Journal of Cancer. 2006;118:3030–3044. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reiter PL, Brewer NT, Gottlieb SL, McRee A, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Social Science & Medicine. 2009;69:475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Rimal RN, Real K. Perceived risk and efficacy beliefs as motivators of change: Use of the risk perception attitude (RPA) framework to understand health behaviors. Human Communication Research. 2003;29:370–399. [Google Scholar]
- Roberto AJ, Krieger JL, Katz M, Goei R, Jain P. Predicting pediatricians’ communication with parents about the human papillomavirus (HPV) vaccine: An application of the theory of reasoned action. Health Communication. 2011;26:303–312. doi: 10.1080/10410236.2010.550021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto AJ, Goodall CE. Using the extended parallel process model to explain physician’s decisions to test their patients for kidney disease. Journal of Health Communication. 2009;14:400–412. doi: 10.1080/10810730902873935. [DOI] [PubMed] [Google Scholar]
- Rosenthal SL, Rupp R, Zimet G, Meza HM, Loza ML, Short MB, et al. Uptake of HPV vaccine: Demographics, sexual history and values, parenting style, and vaccine attitudes. Journal of Adolescent Health. 2008;43:239–245. doi: 10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Pruitt SL, Schootman M. Geographic disparity, area poverty, and human papillomavirus vaccination. American Journal of Preventive Medicine. 2010;38:525–533. doi: 10.1016/j.amepre.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schluterman NH, Terplan M, Lydecker AD, Tracy JK. Human papillomavirus (HPV) vaccine uptake and completion at an urban hospital. Vaccine. 2011;29:3767–3772. doi: 10.1016/j.vaccine.2011.03.032. [DOI] [PubMed] [Google Scholar]
- Tambor ES, Chase GA, Faden RR, Geller G, Hofman KJ, Holtzman NA. Improving response rates through incentive and follow-up: The effect on a survey of physicians’ knowledge of genetics. American Journal of Public Health. 1993;83:1599–1603. doi: 10.2105/ajph.83.11.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention. FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the advisory committee on immunization practices (ACIP) Morbidity and Mortality Weekly Report (MMWR) 2010 May 28;59:630–632. [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. [Accessed December 30, 2010];FDA: Gardasil approved to prevent anal cancer. 2010 Dec 22; Available: www.fda.gov.
- Widdice LE, Bernstein DI, Leonard AC, Marsolo KA, Kahn JA. Adherence to the HPV vaccine dosing intervals and factors associated with completion of 3 doses. Pediatrics. 2011;127:77–84. doi: 10.1542/peds.2010-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K. Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs. 1992;59:329–349. [Google Scholar]
- Witte K, Berkowitz J, Cameron K, Lillie J. Preventing the spread of genital warts: Using fear appeals to promote self-protective behaviors. Health Education & Behavior. 1998;25:571–585. doi: 10.1177/109019819802500505. [DOI] [PubMed] [Google Scholar]
- Witte K, Cameron KA, McKeon JK, Berkowitz JM. Predicting risk behaviors: Development and validation of a diagnostic scale. Journal of Health Communication. 1996;1:317–341. doi: 10.1080/108107396127988. [DOI] [PubMed] [Google Scholar]
- Witte K, Morrison K. The use of scare tactics in AIDS prevention: The case of juvenile detention and high school youth. Journal of Applied Communication Research. 1995;23:128–142. [Google Scholar]
- Zimet GD. Improving adolescent health: Focus on HPV vaccine acceptance. Journal of Adolescent Health. 2005;37:S17–S23. doi: 10.1016/j.jadohealth.2005.09.010. [DOI] [PubMed] [Google Scholar]