Abstract
Introduction
Theory-based research is needed to understand poor contraceptive behavior and related reproductive health sequelae. The purpose of this review was to examine the Health Belief Model (HBM) as a comprehensive, well-tested social-cognitive framework suitable for explaining and predicting contraceptive behavior.
Methods
Existing literature, including editorials and research reports, describing HBM-guided contraceptive research between January 1966 and February 2011 was retrieved from established electronic databases. After consideration of inclusion/exclusion criteria, ten articles were included in the review.
Results
Issues in original family planning applications of HBM included inconsistent conceptualizations of contraceptive behavior and limited use of all HBM constructs in research surveys, interventions and analyses. Knowledge of contraceptive behavior has evolved, warranting more comprehensive use of the HBM for pertinent reproductive health contexts, behaviors and methods.
Conclusion
With more rigorous applications, the HBM can help us understand modern contraceptive behavior determinants and facilitate strategies to prevent unintended pregnancy and promote positive family planning outcomes.
Keywords: Health Belief Model, contraceptive behavior, family planning, theory-guided research
Introduction
Theoretical frameworks are used in health sciences research to predict and explain health behavior and to provide foundations for bio-psycho-social and behavioral interventions toward improved health outcomes.1,2 Social cognitive models have been used for decades in family planning research.3,4 Shortly after the oral contraceptive pill (OC) was introduced, reproductive health professionals called for theory-based research to clarify inconsistent findings on factors relating to poor contraceptive use and to guide development of more rigorous study designs.5,6
The Health Belief Model (HBM), a well-tested, comprehensive social cognitive framework by Rosenstock and colleagues,7 was one of the first models used to predict and explain variations in contraceptive behavior among women in the 1970s and 1980s.8-10 Yet, the HBM has seldom since been applied in family planning. In a recent review of 14 studies testing theory-based contraceptive behavior interventions, none were found to use the HBM.15
Theory-driven strategies to prevent unintended pregnancy are currently needed.15,16 Along with decades of research on unintended pregnancy prevention, knowledge about poor contraceptive behavior has evolved. We are more aware of the complexities of contraceptive behavior, which may support enhanced applications of the HBM to help identify and predict factors that influence successful contraception in current populations and settings. The purpose of this conceptual, integrated review is to examine the suitability of the Health Belief Model (HBM) as a framework for explaining and predicting modern contraceptive behavior.
Methods
Primary articles on the HBM framework generally and its constructs were obtained from an electronic database search and used to provide an overview of the model. Six key articles from the literature, including original works by the theory authors, provided sufficient description and critical commentary on development and testing of the model and its constructs and on implications for health behavior research applications. Examples of non-HBM research in family planning are used to highlight the model's key constructs as they apply to contraceptive behavior.
Articles considered for inclusion in the integrated review were primary research reports or editorials applying the HBM to family planning, and more specifically contraceptive behavior research. Relevant literature was identified using a computerized search for articles published from January 1966 through February 2011 using databases of MEDLINE, Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed, Google Scholar, and PsychInfo. The following key words were searched in combination: “Health Belief Model,” “theory-guided research,” “health behavior theory” AND “contraception,” “family planning,” “birth control,” “contraceptive behavior.” Reference lists of articles from the database search were also examined for relevant citations.
Using this strategy, 82 articles were found in the initial electronic database search. From these articles, 47 were not relevant or were duplicates based upon title and abstract screens and thus excluded. Articles were also excluded if they did not directly address the HBM in a family planning context or if they did not provide at least one specific example of the model's application to original contraceptive research. Ten articles were included in the review.
Following results of the review, a discussion of more recent contraceptive behavior research which supports enhanced HBM applications is presented. Implications for future HBM contraceptive behavior research and practice are addressed.
Results
Overview of the Model
The HBM is a cognitive, interpersonal framework that views humans as rational beings who use a multidimensional approach to decision-making regarding whether to perform a health behavior.2,7 The model is appropriate for complex preventive and sick-role health behaviors such as contraceptive behavior.2,5,7,8 Its dimensions are derived from an established body of social psychology theory that relies heavily on cognitive factors oriented towards goal attainment (i.e. motivation to prevent pregnancy).8 Its constructs emphasize modifiable factors, rather than fixed variables, which enable feasible interventions to reduce public health problems (i.e. unintended pregnancy and sequelae).5
Overall, the HBM's adaptability and holistic nature facilitate applications in diverse contexts like family planning and with complex behaviors like contraceptive behavior. 2,5,7,8 Family planning is a dynamic and complex set of services, programs and behaviors towards regulating the number and spacing of children within a family. 2,7,11,12 Contraceptive behavior, one form of family planning,17 refers to activities involved in the process of identifying and using a contraceptive method to prevent pregnancy8 and can include specific actions such as contraceptive initiation (to begin using a contraceptive method), continuation or discontinuation (to maintain or stop use of a contraceptive method), misuse (interrupted, omitted or mistimed use of a contraceptive method), nonuse, and more broadly compliance and adherence (general terms often used to denote any or all of the former contraceptive behavior terms).18
Motivation to Prevent an Unwanted Pregnancy
Contraceptive behavior, viewed through the HBM, is motivated by an individual's: 1) desire to avoid pregnancy and value placed on not becoming pregnant; 2) nonspecific, stable differences in pregnancy motivations and childbearing desires; and 3) perceived ability to control fertility and reduce the threat of pregnancy by using contraception.11 Sufficient motivation must exist to make prevention of pregnancy salient and relevant and to support the contraceptive behavior decision-making process.6,7
Key Constructs of Contraceptive Behavior
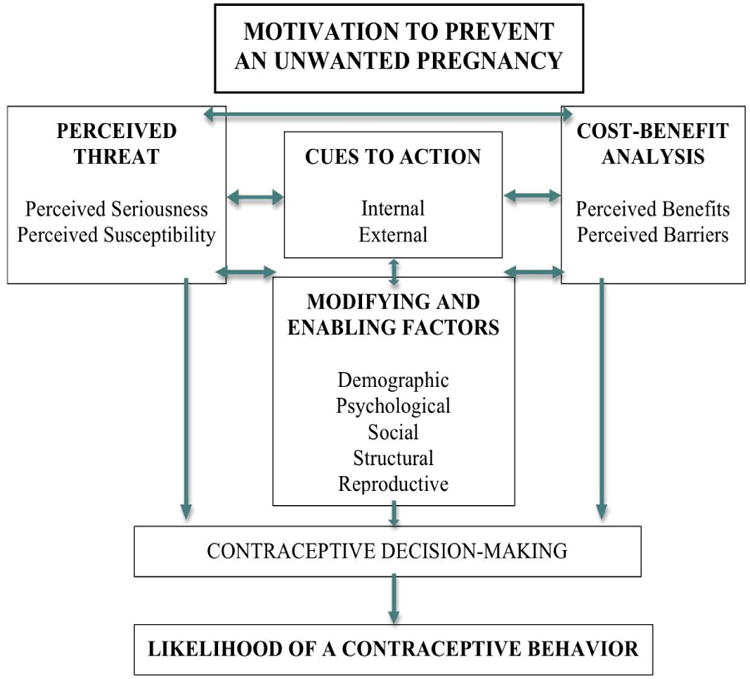
Constructs of the HBM, as applied to contraceptive behavior, are presented in Figure 1 and described below using examples from family planning literature.1,2,7,8,11,19
Figure 1. Constructs of the Health Belief Model, as Applied to Contraceptive Behavior.
Perceived Threat
Perceived threat (susceptibility and seriousness) of an unwanted pregnancy and its sequelae (i.e. birth, abortion, parenthood) provides the incentive to use contraception. This construct considers personal feelings of the seriousness of becoming pregnant, based upon subjective assessment of medical and social consequences of pregnancy and childbearing. This construct may include factors like fear of body changes or pregnancy complications, or worry of quitting school or losing a job due to increased child-rearing responsibility, which can impact the likelihood of contraceptive use.20,21 For example, an analysis of data from the National Longitudinal Study of Adolescent Health found that the 14% of teens with ambivalent attitudes about the risk and seriousness of becoming pregnant had reduced odds of using contraception consistently.20 In another similar study of 4869 high schoolers, girls with pro-pregnancy versus anti-pregnancy attitudes (such as positive perceptions of consequences like social embarrassment, increased stress and parenthood responsibilities) were at increased risk for becoming pregnant within one year.21
Cost-Benefit Analysis
Perceived Barriers
Perceived barriers are negative consequences of using contraception. This dimension includes factors such as perceived side effects of hormonal contraception (i.e. weight gain or mood swings),22-24 physiological risks of hormonal contraceptives (i.e. blood clots),23,25 inconvenience (i.e. having to remember to take a daily pill or apply a condom during intercourse),26 and limited access to methods (i.e. having to obtain a prescription for OC refills or requiring a medical procedure for intrauterine device (IUD) insertion).27 All of these potential contraceptive disadvantages have been found to inhibit contraceptive use.22-27
Perceived Benefits
Perceived benefits relate to the perceived effectiveness, feasibility and other advantages of using a contraceptive method to prevent pregnancy vis-à-vis the perceived barriers. Through a cost-benefit analysis, the perceived ratio of a contraceptive's benefits to its barriers helps determine the preferred and specific contraceptive action and method. For instance, in a study of 154 nulliparous women presenting for an IUD, Wiebe, Trouton, and Dicus found that despite the discomfort, inconvenience, and up-front costs of insertion procedures noted by the women, they chose to use an IUD because of its high contraceptive efficacy, long-term convenience and low hormonal risks.29 This construct may also include non-contraceptive, health promoting benefits of a method (i.e. protection against ovarian cancer, uterine cancer, and anemia, improvement of menstrual symptoms and acne).30 Indeed, increased knowledge of all benefits of a hormonal method like OCs have been shown to increase and improve use.23,30
Cues to Action
Cues to action are internal and external stimuli that trigger a consciousness of the perceived pregnancy threat and facilitate consideration of using contraception to remedy the threat. This may include symptoms like missed menses after intercourse (internal stimuli) or contraceptive communication from the media, and worry from a sexual partner or counseling by a health care provider (external stimuli).25,31 For example, Ndugwa et al studied a cohort of poor, urban, post-partum women in Africa and found that timing of menstrual resumption was significantly associated with contraceptive initiation.32 Women who resumed menses in the immediate post-partum period adopted a contraceptive method, on average, within one month.32
Modifying and Enabling Factors
Modifying or enabling factors interact with an individual's perceptions of pregnancy and decision-making to influence contraceptive use. This dimension includes a broad range of well researched demographic, social, structural, psychological and reproductive factors predictive of contraceptive behavior.22-37 For instance, adolescents and women of racial/ethnic minority are more likely to experience an unintended pregnancy secondary to contraceptive non- or misuse than their older and non-minority counterparts.37 Women of rural residence, with low income levels, and who are uninsured are less likely to use a highly effective contraceptive method than are urban women, of higher socioeconomic status, with insurance.36,37 Greater locus of control and knowledge of contraception support contraceptive initiation and continuation,23-25 while earlier age at menarche and coitarche, greater number of sexual partners, and prior pregnancy or abortion predict contraceptive misuse.22,37
Issues in Early Applications of the HBM for Family Planning Problems with Conceptualizing Contraceptive Behavior
Several studies reviewed were commentaries highlighting controversy over applicability of the HBM for family planning in the 1970s and 1980s.4-6,14,38 Disagreement largely arose from inconsistencies in conceptualizing contraceptive behavior as an outcome.4-6,14,38 Katasky was the first to propose the HBM as a framework that could help explain contraceptive compliance, drawing parallels between family planning and other health behaviors.5 The general argument focused on the role of motivation - that the motivation to prevent an unwanted pregnancy would predict contraceptive compliance just as the motivation to prevent a disease would predict medication therapy compliance.5 Support for how HBM constructs would be applied specifically to contraceptive behavior were not provided.6
Fisher, on the other hand, argued that the HBM was designed to predict and explain “sick role” behaviors (remedy a disease) rather than preventive health behaviors (prevent a condition).14 Fisher believed this orientation limited the model's applicability in family planning since pregnancy is not a disease which one always wishes to avoid.14 Fisher pointed to several examples of the difficulty in interpreting the HBM constructs to understand contraceptive behavior because of this inherent conceptual problem. For instance, interpreting affirmative responses to questions on pregnancy intentions (i.e. “I think it is very likely that I will become pregnant in the next year”), if guided by the model, might be misunderstood as an indication of susceptibility to pregnancy, and promote contraceptive use (which is not intuitive if one actually intends to become pregnant). He argued along similar lines for problems associated with interpreting the perceived severity and benefits/barriers constructs.14
Later, multiple other researchers, including the HBM's authors, agreed that a health condition does not have to be an undesirable condition to always be avoided in order for the HBM to have predictive and explanatory value.6-10,38 These researchers argued that the model is appropriate for family planning despite, and even because, family planning is unique as a health behavior.6-10,38 Tenets of this argument, including a theoretical foundation provided by Lin and Hingson38 and a thorough, updated application by Nathanson and Becker,8 are as follows.
There may be ambivalence that pregnancy is negative and should be avoided, as compared to other behaviors undertaken to prevent a clearly negative disease (i.e. antidepressant medication to treat depressive symptoms). 38 The HBM can, however, account for ambivalence in the perceived severity construct, using more precise assessments of pregnancy intentions and attitudes (i.e. “I intend/desire to become pregnant in the next year,” rather than, “I think it is likely I will become pregnant”).6
Contraceptive behavior may have particular constraints on individual decision-making by relationships which directly affect the behavior.38 For instance, condom use may be influenced by a partner who has a strong vested interest in preventing pregnancy (as compared to other health behaviors with implications for the individual, such as antihypertensive therapy for blood pressure management).6,8 Yet, this characteristic of contraceptive behavior can be adequately accounted for by thoroughly assessing modifying (social/relationship) factors within the HBM.8
Contraceptive use may lack ongoing reinforcement for continuing the behavior because there are no regular perceived positive effects of taking OC (as opposed to, for example, the tangible effects of daily antihistamine use to control allergy symptoms).38 However, the HBM would suggest that many other sources of motivation (i.e. internal and external cues, perceived benefits, perceived threat) would support the likelihood of continuing contraceptive use.6,8
There is a more complex degree of choice related to contraceptive behavior versus other health behaviors because of different actions (i.e. initiation, consistent/correct use, continuation) and different methods.38 For instance, OCs and the copper IUD have different traits, including costs, initiation procedures, and non-contraceptive benefits, which can impact perceived benefits and barriers of each method to influence the contraceptive behavior differently. But, with well-defined, tailored applications for a specific contraceptive behavior or method, these considerations are sufficiently addressed by the HBM.6,8
Limitations in Operationalizing HBM Constructs for Contraceptive Behavior
After some resolution of the contraceptive behavior conceptualization problem, the HBM was applied in several early family planning research studies, which are described below.9,10,13,16 Collectively, original HBM applications failed to employ all constructs or explicitly measure sufficient or appropriate variables articulated by the model.5,6,13 Limited applications may have limited the findings on the effectiveness of HBM-guided surveys and interventions in predicting and explaining contraceptive behavior.6,9,16
For example, Hester and Macrina used the HBM to guide their descriptive study of self-reported contraceptive behavior of 171 female college students in Illinois.9 The researchers employed several constructs of the HBM to assess perceived susceptibility and seriousness of pregnancy and benefits and barriers to contraceptive use. Likert scale items included questions such as, “how do you feel your chances of becoming pregnant are;” “how would you rank pregnancy as compared to failing an examination important to your major;” or “how much do you agree that using contraception is inconvenient.” In regression analyses, items from the perceived benefits/barriers construct predicted consistent contraceptive use, while perceived susceptibility of pregnancy was only weakly associated and perceived seriousness was not significant in analyses. The role of motivation and the constructs of cues to action and modifying/enabling factors were not accounted for.
In a pilot study and subsequent larger randomized trial of a community-based sex education intervention study to promote adolescents' contraceptive use, Eisen, Zellman and McAlister used the HBM as a conceptual framework to develop curriculum materials and a program evaluation survey.10,13 The HBM educational intervention or active control group components were not well-described in either report. The evaluation survey included questions on susceptibility, seriousness, benefits and barriers constructs to determine the intervention's effectiveness in modifying beliefs, motivations and behavior around pregnancy prevention. Examples of Likert items included, “how likely is it that you or your partner would get pregnant if you didn't use contraception;” “if a teen girl has an unplanned pregnancy, it's not a big problem since she can raise her baby alone;” or “the side effects of good birth control methods are a real problem.” While the pilot study (n = 120) found significant improvements in consistent contraceptive use, perceptions, and knowledge among adolescents receiving the HBM intervention,10 the larger randomized trial (n = 1,444) failed to find a difference in cognitive or behavioral outcomes between the HBM intervention and control groups.13 Moreover, the intervention's effectiveness varied by gender and sexual experience. Males in the treatment group, but not females, were less likely to initiate intercourse, and treatment group females who were sexually active, but not males, were less likely to use contraception, than control group participants.13
Finally, in a comprehensive review of school-based programs to reduce sexual risk-taking among adolescents, Kirby analyzed the above-described HBM educational intervention as one of several theory-guided intervention studies.16 He commented on the strength of Eisen et al's theoretical approach, which built upon the successes and failures of past sex education programs and was more rigorously evaluated. Yet, he also acknowledged the weak intervention, active control and mixed results as major limitations of the study.
Evolving Contraceptive Research Provides for Enhanced HBM Applications
Early limitations in conceptualizing pregnancy prevention and recognizing the complexity of contraceptive behavior determinants made rigorous applications of the HBM difficult. This may partially explain why the HBM has seldom since been used in family planning research.15 Fortunately, given the synergistic relationship of science and theory, as family planning research has evolved and measurement of predictor and outcome variables has improved, more robust applications of the HBM to contraceptive behavior are possible.39
Current perspectives of pregnancy prevention are broader and our understanding of the myriad of factors influencing contraception is more complex than when the HBM was originally used in family planning. Pregnancy is not simply an undesirable disease to be avoided; pregnancy prevention is a health behavior in its own right.5,6,8-10,40 Our more recent understanding of contraceptive behavior is through its role in health promotion -maintenance and enhancement of physical, psychological and social wellbeing.41
Researchers have discovered new determinants, challenged previously supported correlates, and gained greater understanding of how dimensions and variables interact to influence contraceptive behavior. For instance, perceived threat of pregnancy has become more precisely defined in relation to other constructs.8 Perceived threat of pregnancy can interact with cues to action (pregnancy attitudes are shaped by an intimate partner's feelings and beliefs),31 perceived benefits and barriers (understanding of a contraceptive's mechanism of action is affected by beliefs about physiologic processes of conception and pregnancy),28 and psychological modifying factors (greater locus of control is related to prioritization of life goals which impact the seriousness of potential motherhood).39 All of these interactions of HBM constructs, which have not been examined using the HBM, serve to influence the likelihood of contraceptive use and may be better understood by using the comprehensive, structured framework.
Capitalizing on advancements in contraceptive behavior science, Brown, Ottney and Nguyen published the first recent study applying the HBM to modern contraceptive research.39 The investigators designed a survey to examine patients' perceptions and contraceptive method selection using the HBM constructs. Multiple Likert items were developed to measure knowledge of fertility (susceptibility), perceived consequences of a pregnancy (severity), perceived contraceptive effectiveness, ease of use, and menstrual suppression (benefits), perceived side effects, method failure, cost, and infertility effects (barriers), seeking health counsel (cues to action), and self-efficacy (motivation). By using a more comprehensive HBM-guided approach to assess a specific contraceptive behavior, the investigators were able to clarify factors that facilitate the contraceptive selection decision-making process. Findings from this study move beyond past emphasis on pregnancy susceptibility to highlight the importance of perceived ease of use and the role of socioeconomic modifying factors in influencing contraceptive choice.
Discussion
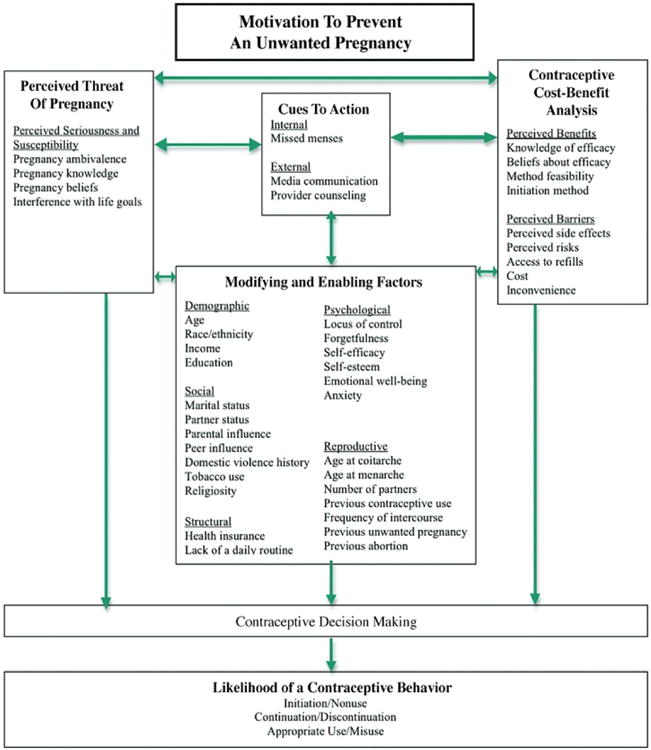
Based upon these findings, a current and inclusive contraceptive behavior HBM that can facilitate contraceptive behavior science and practice is depicted in Figure 2.
Figure 2. A Current and Inclusive Contraceptive Behavior Health Belief Model that Can Facilitate Contraceptive Behavior Science and Practice.
Implications for Research
Family planning researchers must continue to carefully define and measure contraceptive outcomes, customizing HBM applications to specific contraceptive behaviors and methods. 8,18 Measurements of contraceptive behavior have relied upon self-report histories of missed pills, timing of initiation and dosing, and discontinuation, which are unreliable estimates and contribute to statistical error and inconsistent findings.18 More reliable, appropriate and feasible measures of contraceptive use such as serum and urine hormone concentrations and electronic monitoring devices, may contribute to the most precise results and facilitate improved applications of the HBM to contraceptive behavior research.18
The HBM can be used to investigate the impact of new and improved contraceptive methods on behavior. The IUD, subdermal implant, intramuscular injection, transdermal patch, vaginal ring, and low-dose and extended-cycle OCs have features that would affect the HBM's dimensions differently to influence contraceptive behavior uniquely.6 Additionally, previous applications focused on condom use,9,10 but specific evaluations for the more effective and favored methods like OCs may better address the highest rates of unintended pregnancy due to pill discontinuation.22,43,44
For updated methodological designs, the HBM can guide development, testing and implementation of rigorously-designed contraceptive interventions which operationalize all HBM dimensions.16 HBM-guided programs that are culturally- and health literacy-sensitive, that employ multimodal learning strategies (i.e. provider counseling, written handouts, educational videos, computer-delivered information), and that are evaluated using standardized techniques are warranted.42
Constructs of the HBM should be more fully employed to test the broad spectrum of variables articulated by the model.8 For instance, understanding of environmental factors, such as settings from which to dispense contraception or geographic access to family planning clinics, 2,38 and interpersonal cues to action variables, such as provider-patient interactions,47 is needed to promote contraceptive use. Structural factors such as insurance status, coverage for preventive reproductive health visits, and benefits for contraceptive prescription coverage should systematically evaluated using the model for their the role in preventing unintended pregnancy.48,49 Finally, the HBM should be explicitly applied to vulnerable populations like minority women and adolescents who disproportionately share the burden of unintended pregnancy and who are in particular need of theory-based strategies to improve contraceptive use.6,35,43-46
Implications for Practice
While perhaps even less is known about theory-guided contraceptive practice than research, the HBM's adaptability, comprehensive nature and preventive orientation support its use in clinical practice. Here are some basic examples building upon the above-described HBM-guided contraceptive behavior science (existing and future).
Health care providers can use the HBM to understand patients' contraceptive needs, employing constructs of the model to guide patient interviewing. For instance, the health history around a contraceptive initiation visit should focus not only on fertility intentions but also on existing perceptions of method-specific benefits and barriers and on psychological, social and reproductive histories that may be relevant to contraceptive method selection.8,15,29,40 Individual patient characteristics such as fear of an invasive procedure, inability to cover a monthly co-pay, difficulty in remembering to take a daily medication, history of tobacco use, or recent pelvic inflammatory disease diagnosis may help rule out some options to determine the most patient-centered method. By obtaining health information from all HBM constructs to present a complete historical picture, providers can help patients initiate the most appropriate contraceptive to facilitate successful use from the outset.8
Following the HBM-guided health history, health care professionals can structure contraceptive education and counseling sessions by the framework to ensure comprehensiveness of approach and content. For instance, information on not only the risks of contraception but of contraceptive benefits, efficacy, proper use, mechanisms of action, and resources, as operationalized by different HBM constructs, can increase patients' contraceptive knowledge to improve use.42
The HBM also offers a comprehensive approach to long-term patient contraceptive management plans. The framework can provide ongoing structure for providers to reassess patients' contraceptive behavior patterns and their dynamic developmental, cognitive and physical health needs within complex socioeconomic, environmental and reproductive contexts.42 For example, as an adolescent transitions to college, adopts a new schedule, obtains a job, and initiates a relationship, a long-acting reversible method like the IUD might be more complementary to her situation than a method previously relied upon like condoms. By considering all of these factors through the holistic model, health providers can help patients continue to choose the most appropriate and relevant contraceptive behavior and method.
Conclusion
The HBM offers a robust theory to direct family planning science and practice, yet limitations of past HBM applications to contraceptive behavior are noteworthy. Knowledge of contraceptive behavior has evolved. Comprehensive applications of the HBM employing all constructs, evaluating diverse variables, and focusing on the most pertinent reproductive health contexts, contraceptive behaviors and methods are indicated. Ultimately, the HBM provides a framework for predicting and explaining the complex systems of modern contraceptive behavior determinants and for promoting strategies to improve family planning outcomes now.
References
- 1.Becker MH, Haefner DP, Kasl SV, Kirscht JP, Maiman LA, Rosenstock IM. Selected psychological models and correlates of individual health-related behaviors. Med Care. 1977;15(supp):27–46. doi: 10.1097/00005650-197705001-00005. [DOI] [PubMed] [Google Scholar]
- 2.Rosenstock IM. Historical origins of the health belief model. Health Ed Mono. 1974;2:328. [Google Scholar]
- 3.Fishbein M, Jaccard JJ. Theoretical and methodological considerations in theprediction of family planning intentions and behavior. Reprod Research Soc Psych. 1973;4:37–51. [PubMed] [Google Scholar]
- 4.Rogers E. Communication strategies for family planning. New York: The Free Press; 1973. pp. 296–297.pp. 389 [Google Scholar]
- 5.Katatsky ME. The Health Belief Model as a conceptual framework for explaining contraceptive compliance. Health Ed Mono. 1977;5(3):233–243. [PubMed] [Google Scholar]
- 6.Herold ES. The Health Belief Model: Can it help us to understand contraceptive use among adolescents? J School Health. 1983:19–21. doi: 10.1111/j.1746-1561.1983.tb04047.x. [DOI] [PubMed] [Google Scholar]
- 7.Rosenstock IM. The Health Belief Model and preventive health behavior. In: Becker MH, editor. The Health Belief Model and Personal Health Behavior. Thorofare, NJ: Slack; 1974. [Google Scholar]
- 8.Nathanson CA, Becker MH. Contraceptive behavior among unmarried young women: A theoretical framework for research. Pop Environ. 1983;6(1):39–58. [Google Scholar]
- 9.Hester NR, Macrina DM. The Health Belief Model and the contraceptive behavior of college women: Implications for health education. J Am College Health. 1985;33(6):245–252. doi: 10.1080/07448481.1985.9935034. [DOI] [PubMed] [Google Scholar]
- 10.Eisen M, Zellman GL, McAlister AL. A Health Belief Model approach to adolescents' fertility control: Some pilot findings. Health Ed Behav. 1985;12:185–210. doi: 10.1177/109019818501200205. [DOI] [PubMed] [Google Scholar]
- 11.Janz NK, Becker MH. The health belief model: a decade later. Health Ed Quar. 1984;11:1. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 12.Kelly JR, Mamon JA, Scott JE. The Health Belief Model in examining medication compliance among psychiatric outpatients. Soc Sci Med. 1987;25(11):1205–1211. doi: 10.1016/0277-9536(87)90367-4. [DOI] [PubMed] [Google Scholar]
- 13.Eisen M, Zellman GL, McAlister AL. A Health Belief Model-Social Learning Theory approach to adolescents' fertility control: Findings from a controlled field trial. Health Ed Behav. 1992;19:249–262. doi: 10.1177/109019819201900208. [DOI] [PubMed] [Google Scholar]
- 14.Fisher AA. The Health Belief Model and contraceptive behavior: Limits to the application of a conceptual framework. Health Ed Mono. 1977;5(3):244. doi: 10.1177/109019817700500305. - [DOI] [PubMed] [Google Scholar]
- 15.Lopez LM, Tolley EE, Grimes DA, Chen-Mok M. Theory-based strategies for improving contraceptive use: A systematic review. Contraception. 2009;80(2):108–12.250. doi: 10.1016/j.contraception.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Kirby D. School-based programs to reduce sexual risk-taking behaviors. J School Health. 1992;62(7):280–287. doi: 10.1111/j.1746-1561.1992.tb01244.x. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Family planning. 2011 Retrieved January 9, 2011 from http://www.who.int/topics/family_planning/en/
- 18.Hall KS, White KO, Reame N, Westhoff C. Studying Use of Oral Contraception: A Systematic Review of Measurement Approaches. J Women's Health. 2010;19(12):2203–2210. doi: 10.1089/jwh.2010.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenstock IM, Stretcher VJ, Becker MH. Social learning theory and the health belief model. Health Ed Quar. 1988;15(2):175–84. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 20.Brucker H, Martin A, Bearman PS. Ambivalence and pregnancy: Adolescents' attitudes, contraceptive use and pregnancy. Persp Sex Repro Health. 2004;36(6):248–57. doi: 10.1363/psrh.36.248.04. [DOI] [PubMed] [Google Scholar]
- 21.Jaccard J, Dodge T, Dittus P. Do adolescents want to avoid pregnancy? Attitudes towards pregnancy as predictors of pregnancy. J Adolesc Health. 2003;33(2):79–83. doi: 10.1016/s1054-139x(03)00134-4. [DOI] [PubMed] [Google Scholar]
- 22.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: A prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–82. doi: 10.1016/s0002-9378(98)70047-x. [DOI] [PubMed] [Google Scholar]
- 23.Bryden PJ, Fletcher P. Knowledge of the risks and benefits associated with oral contraception in a university-aged sample of users and non-users. Contraception. 2001;63:223–7. doi: 10.1016/s0010-7824(01)00194-9. [DOI] [PubMed] [Google Scholar]
- 24.Westhoff C, Heartwell S, Edwards S, et al. Oral contraceptive discontinuation: do side effects matter? Am J Obstet Gynecol. 2007;196:412e1–412e7. doi: 10.1016/j.ajog.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egarter C, Strohmer H, Lehner R, Foldy M, Leitich H, Berghammer P. Contraceptive knowledge and attitudes of Austrian adolescents after mass media reports linking third-generation oral contraceptives with an increased risk of venous thromboembolism. Contraception. 1997;56:147–152. doi: 10.1016/s0010-7824(97)00117-0. [DOI] [PubMed] [Google Scholar]
- 26.Peterson LS, Oakley D, Potter LS, Darroch JE. Women's efforts to prevent pregnancy: consistency of oral contraceptive use. Fam Plan Persp. 1998;30:19–23. [PubMed] [Google Scholar]
- 27.Westhoff C, Heartwell S, Edwards S, et al. Initiation of oral contraceptives using a Quick Start as compared with a conventional start. Obstet Gynecol. 2007;109:1270–76. doi: 10.1097/01.AOG.0000264550.41242.f2. [DOI] [PubMed] [Google Scholar]
- 28.Tessler SL, Peipert JF. Perceptions of contraceptive effectiveness and health effects of oral contraception. Women's Health Iss. 1997;7:400–6. doi: 10.1016/s1049-3867(97)00079-0. [DOI] [PubMed] [Google Scholar]
- 29.Wiebe ER, Trouton KJ, Dicus J. Motivation and experience of nulliparous women using intrauterine contraceptive devices. J Obstet Gynaecol Canada. 2010;32(4):335–338. doi: 10.1016/S1701-2163(16)34477-2. [DOI] [PubMed] [Google Scholar]
- 30.Hatcher RA, Trussell J, Stewart F, et al. Contraceptive Technology. 18th Revised. New York: Ardent Media; 2004. [Google Scholar]
- 31.Kaunitz AM. Oral contraceptive health benefits: perceptions versus reality. Contraception. 1999;59:29S–33S. doi: 10.1016/s0010-7824(98)00135-8. [DOI] [PubMed] [Google Scholar]
- 32.Kerns J, Westhoff C, Morroni C, Murphy PA. Partner influence on early discontinuation of the pill in a predominantly Hispanic population. Persp Sex Repro Health. 2003;35:256–60. doi: 10.1363/psrh.35.256.03. [DOI] [PubMed] [Google Scholar]
- 33.Zabin LS, Huggins GR, Emerson MR, Cullins VE. Partner effects on a woman's intention to conceive: ‘Not with this partner’. Fam Plan Persp. 2000;32(1):39–45. [PubMed] [Google Scholar]
- 34.Ndugwa RP, Cleland J, Madise NJ, Fosto JC, Zulu EM. Menstrual pattern, sexual behaviors and contraceptive use among postpartum women in Nairobi Urban Slums. J Urban Health. doi: 10.1007/s11524-010-9452-6. published online May 7, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walsemann KM, Perez AD. Anxiety's relationship to inconsistent use of oral contraceptives. Health Ed Behav. 2006;33:197–214. doi: 10.1177/1090198105277322. [DOI] [PubMed] [Google Scholar]
- 36.Smith JD, Oakley D. Why do women miss oral contraceptive pills? An analysis of women's self-described reasons for missed pills. J Midwifery Women's Health. 2005;50:380–5. doi: 10.1016/j.jmwh.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 37.Glei D. Measuring contraceptive use patterns among teenage and adult women. Fam Plann Persp. 1999;31:73–80. [PubMed] [Google Scholar]
- 38.Lin N, Hingson R. Diffusion of family planning innovations: Theoretical and practical issues. Stud Fam Plann. 1974;5(6):189–194. [PubMed] [Google Scholar]
- 39.Brown W, Ottney A, Nguyen S. Breaking the barrier: The Health Belief Model and patient perceptions regarding contraception. Contraception. 2011;83:453–458. doi: 10.1016/j.contraception.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 40.Ross J, Hardee K, Mumford E, Eld S. Contraceptive method choice in developing countries. Inter Persp Fam Plann. 2001;28(1):32–40. [Google Scholar]
- 41.Deijen JB, Kornaat H. The influence of type of information, somatization, and locus of control on attitudes, knowledge, and compliance with respect to the triphasic oral contraceptive Tri-Minulet. Contraception. 1997;56:31–41. doi: 10.1016/s0010-7824(97)00071-1. [DOI] [PubMed] [Google Scholar]
- 42.Hall KS, Castano P, Stone P, Westhoff C. The state of oral contraceptive knowledge measurement. Pat Ed Couns. 2010;81(3):388–394. doi: 10.1016/j.pec.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abma JC, Martinez GM, Mosher WD, et al. Teenagers in the United States: Sexual activity, contraceptive use and childbearing, 2002. Vit Health Stat. 2004;23(24) [PubMed] [Google Scholar]
- 44.Alan Guttmacher Institute (AGI) US teenage pregnancy statistics: overall trends, trends by race and ethnicity, and state-by-state information. New York: Author; 2004. [Google Scholar]
- 45.Thomas MA, Shields WC. Leadership and diversity: A call for new directions in reproductive health education and practice. Contraception. 2007;75:163–5. doi: 10.1016/j.contraception.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 46.National Adolescent Health Information Center (NAHIC), University of California, San Francisco; CDC; and the Health Resources and Services Administration, Maternal and Child Health Bureau, Office of Adolescent Health. Improving the Health of Adolescent & Young Adults: A Guide for States and Communities. Author; 2004. [Google Scholar]
- 47.Omar H, Richard J. Cultural sensitivity in providing reproductive care to adolescents. Curr Opin Obstet Gynecol. 2004;16:367–70. doi: 10.1097/00001703-200410000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Harper CC, Cheong M, Rocca C, et al. The effect of increased access to emergency contraception among young adolescents. Obstet Gynecol. 2005;106(3):483–91. doi: 10.1097/01.AOG.0000174000.37962.a1. [DOI] [PubMed] [Google Scholar]
- 49.Phillips KA, Grossman D, Weitz TA, Trussell J. Bridging evidence to the debate on abortion coverage in health reform legislation: findings from a national survey in the United States. Contraception. 2010;82:129–30. doi: 10.1016/j.contraception.2010.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


