Abstract
Objective To evaluate the efficacy of oral anti-inflammatory or antibiotic treatment compared with placebo in the resolution of cough in patients with uncomplicated acute bronchitis and discoloured sputum.
Design Multicentre, parallel, single blinded placebo controlled, randomised clinical trial.
Setting Nine primary care centres in Spain.
Participants Adults aged 18 to 70 presenting symptoms associated with respiratory tract infection of less than one week’s duration, with cough as the predominant symptom, the presence of discoloured sputum, and at least one other symptom of lower respiratory tract infection (dyspnoea, wheezing, chest discomfort, or chest pain).
Interventions Patients were randomised to receive either ibuprofen 600 mg three times daily, amoxicillin-clavulanic acid 500 mg/125 mg three times daily, or placebo three times daily for 10 days. The duration of symptoms was measured with a diary card.
Main outcome measure Number of days with frequent cough after the randomisation visit.
Results 416 participants were randomised (136 to ibuprofen, 137 to antibiotic, and 143 to placebo) and 390 returned their symptom diaries fully completed. The median number of days with frequent cough was slightly lower among patients assigned to ibuprofen (9 days, 95% confidence interval 8 to 10 days) compared with those receiving amoxicillin-clavulanic acid (11 days, 10 to 12 days) or placebo (11 days, 8 to 14 days), albeit without statistically significant differences. Neither amoxicillin-clavulanic acid nor ibuprofen increased the probability of cough resolution (hazard ratio 1.03, 95% confidence interval 0.78 to 1.35 and 1.23, 0.93 to 1.61, respectively) compared with placebo. Adverse events were observed in 27 patients, and were more common in the antibiotic arm (12%) than ibuprofen or placebo arms (5% and 3%, respectively; P<0.01).
Conclusion No significant differences were observed in the number of days with cough between patients with uncomplicated acute bronchitis and discoloured sputum treated with ibuprofen, amoxicillin-clavulanic acid, or placebo.
Trial registration Current Controlled Trials ISRCTN07852892.
Introduction
Acute bronchitis implies a self limiting infection of the large airways and is characterised by cough without pneumonia.1 It is a prevalent disease and one of the most common reasons for visits in primary care.2 3 Patients often return to their doctor or seek other medical help as symptoms may persist for two or three weeks, mainly cough, which may be bothersome for some patients and could last for up to four weeks or more.4
Acute bronchitis is mainly a viral infection.5 6 The role of bacteria in this infection continues to be controversial since bronchial biopsy samples have never shown bacterial invasion.1 It is thought that acute bronchitis reflects an inflammatory response of the epithelium of the bronchi to infections. Microscopic examination shows a thickening of the bronchial and tracheal mucosa corresponding to the inflamed areas. These findings are consistent with proximal lower airway inflammation observed with positron emission tomography.7
Most of these infections are self limiting, and several studies have suggested that the benefit of antimicrobial treatment is marginal.8 However, most patients with acute bronchitis receive antibiotics, even in countries with low rates of antibiotic prescribing.9 This over-prescription constitutes a global problem and is an important factor in increasing the levels of antibiotic resistance.10 Several approaches for controlling acute cough have included narcotic cough suppressants, expectorants, antihistamines, decongestants, herbal remedies, and β2 agonists.11 12 Even though all these drugs are widely prescribed in patients with acute bronchitis, evidence is scant that their use may be helpful for adults with cough. A Cochrane review of the use of antitussives in patients with acute cough showed no clear benefit for duration of cough.11 Some studies did report the beneficial effects of expectorants, but these studies were small and had methodological flaws.11 Another Cochrane review of β2 agonists showed little evidence for their efficacy in adults with acute cough. These agents may reduce symptoms, including cough, in people with evidence of airflow obstruction. However, their potential benefit in patients without chronic airway disease is not well supported by the data available and must be weighed against the adverse effects associated with their use.12 There is therefore an urgent need to identify novel treatment measures to deal with this common infectious disease, particularly in light of growing patient expectations and increasing antibiotic resistance. Non-steroidal anti-inflammatory drugs are widely prescribed in patients with lower respiratory tract infections, mainly for alleviating fever and chest pain as well as other common complaints such as cough.13 Notwithstanding, the effectiveness of these drugs for reducing the duration and intensity of cough has not been analysed in randomised clinical trials. No sufficiently powered studies have been published comparing the role of non-steroidal anti-inflammatory drugs with that of antibiotics. We therefore compared the efficacy of ibuprofen and amoxicillin-clavulanic acid with placebo in a group of otherwise healthy adults with acute bronchitis and discoloured sputum.
Methods
The study protocol has been published elsewhere.14 In brief, we used a prospective, parallel group, single blinded, placebo controlled design. The patients were randomised to one of three treatment arms: ibuprofen 600 mg three times daily, amoxicillin-clavulanic acid 500 mg/125 mg three times daily, or placebo three times daily for 10 days. The pharmacy unit of the Hospital Vall d’Hebron (Barcelona, Catalonia) prepared the drugs. A block randomisation method was used and the various treatments and placebo blocks were then issued with a drug number and assigned to consecutive patients in sequential order. Patients were masked to treatment allocation. Twenty five general practitioners from nine primary care centres in Catalonia recruited participants from April 2010 to January 2012.
Participant selection
Eligible participants were adults aged 18 to 70 without associated respiratory comorbidity or immunosuppression. They had to present symptoms associated with respiratory tract infection of less than one week’s duration, with cough as the predominant symptom and discoloured sputum and at least one other criterion of lower respiratory tract infection such as dyspnoea, wheezing, chest discomfort, or chest pain. Written informed consent was obtained from all participants.
Exclusion criteria were antibiotic, anti-inflammatory, or corticosteroid use in the previous two weeks; the presence of radiological signs of pneumonia; signs of severe infection such as confusion; respiratory rate >25 breaths per minute or pulse >120 beats per minute; history of gastrointestinal haemorrhage or intolerance to anti-inflammatory treatment; hypersensitivity to β lactams or intolerance to clavulanic acid or lactose; pregnancy, lactation, and absence of contraception in women of fertile age; associated comorbidity (bronchial asthma, chronic obstructive pulmonary disease, moderate-severe heart failure, dementia, stroke, immunosuppression or the use of immunosuppressive drugs); emergency situation; in residential care; unable to provide informed consent; difficulty in attending the programmed visits; previous participation in the study; and refusal to participate.
Concomitant drugs, except for non-steroidal anti-inflammatory drugs and antibiotics, were allowed at the discretion of the investigators.
Procedures
At the inclusion visit, the doctors carried out a clinical examination and a C reactive protein rapid test in capillary blood (QuikRead CRP analysers; Orion Diagnostica, Espoo, Finland). In cases of suspected pneumonia we instructed the doctors to request chest radiography. In addition, patients received a symptom diary and instructions on how to complete it.
The first follow-up visit was scheduled at 2-4 days. At this visit the doctors evaluated the clinical course of symptoms and the presence of adverse events. Compliance with the study drug and the diary cards was reinforced. The second visit, at days 11-13, was to review adherence to the study drug, assess the clinical course of symptoms, and evaluate the presence of adverse events.
At the second follow-up visit patients were classified as cure, defined as the disappearance of the acute signs and symptoms related to the infection (complete return to the previous situation of stability); improvement, defined as the non-complete resolution of the symptoms but without the need for new treatment; or failure, with an insufficient reduction in the signs and symptoms of infection requiring further intervention.15 Clinical success was considered when either cure or improvement was observed.
The patients classified as clinical failures at any of the follow-up visits were either referred to hospital or considered, unblinded, for treatment with an antibiotic. Patients classified as cured at the end of the second visit finished the study, whereas those classified as improved were encouraged to continue filling out the diary and were given an appointment at 30 days (late follow-up), with that visit considered the last of the study.
We evaluated five items in the symptom diary: disease severity, daytime cough, night time cough, limitation in daily activities, and febrile sensation. Each of the items was scored from 0 to 4. This symptom diary has previously been described and used in other studies16 and has been validated in its Spanish version.17
The patients were required to return all the unused drugs not presented to the investigator. If remaining drugs were not returned, we considered compliance to be insufficient. The intention to treat population included all randomised patients receiving at least one dose of the study drug. The per protocol population included patients who received neither systemic antimicrobial agents nor anti-inflammatory drugs other than the study drug for at least three days in the case of clinical failure or ≥80% of study drug in the case of cure, with adequate assessment of compliance and absence of major protocol violations. Both the intention to treat and per protocol analysis for the main outcome were carried out for those patients who returned and had completed the diaries.
Outcomes
The primary outcome was the number of days with frequent cough in the intention to treat population—that is, the number of days from the randomisation visit until the last day the patient scored ≥1 in both the daytime and the night time cough items in the symptom diary. Secondary outcomes were the efficacy of the treatment at the end of the second follow-up visit and the time of resolution of the total symptom scores (time until the last day the patient scored ≥1 in any of the five items). Other secondary outcomes were the results observed in the per protocol population. We recorded adverse effects at all visits and these were ranked by intensity (mild, moderate, severe, and serious) and relation to the study drug.
Statistical analyses
Sample size calculation
We accepted a null hypothesis if the number of days of frequent cough in the anti-inflammatory arm or antibiotic arm was the same or two days either way of that observed in the placebo arm. Based on the literature, the standard deviation of the duration of frequent cough was 5.5 days in patients with bronchitis and discoloured sputum.18 For an α of 0.05 and a β of 0.2 and accepting possible losses of 15%, we calculated that we required a sample size of 140 patients per group (total of 420 patients).
Main analyses
We evaluated the main outcome in the intention to treat population. Results are presented as percentages, means (standard deviation), or medians (interquartile range). In addition, we carried out bivariate baseline analysis. We compared baseline variables between the groups by the ANOVA test for continuous variables and the χ2 test for categorical variables (exact Fisher test with observed frequencies <5).
To analyse the time until cure of the different symptoms and for the main result variable (days from the randomisation visit until the patient last scored ≥1 in the boxes related to cough in the symptom diary) we carried out survival analysis using the Kaplan-Meier method. We compared the three survival curves using the log rank test. Cox proportional hazards regression survival models were used to calculate the hazard ratio and 95% confidence intervals for the probability of cough resolution, using the placebo group as the reference group. We included potential confounders in progressive models. The Cox proportional hazards regression assumptions were tested using Schoenfeld residuals.19 All analyses were performed with the IBM SPSS Statistics v.19 program (Chicago, USA) and R programme v. 2.10.1.
Results
Recruitment and follow-up
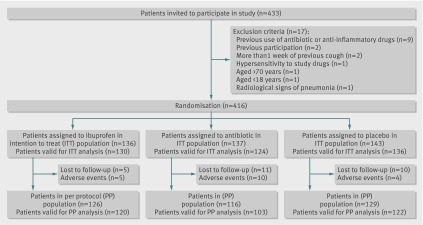
A total of 433 people were screened for inclusion in the study. Seventeen did not fulfil any of the inclusion criteria or had at least one of the exclusion criteria and were excluded from the study. Chest radiography was performed in seven people, one of whom was positive for consolidation and was therefore excluded from the study. Figure 1 shows the flow of patients in the study and reasons for exclusion.
Fig 1 Flow of patients through study
Characteristics of participants
Overall, 416 patients were randomised (136 to the ibuprofen arm, 137 to the amoxicillin-clavulanic acid arm, and 143 to the placebo arm) and constituted the intention to treat population. The mean age was 45.1 (SD 14.3) years and 185 were men (44%). The personal and clinical characteristics of the randomised population were well matched among the groups (table 1). A total of 390 patients had information on symptoms in the diary (94%) and constituted the intention to treat population valid for the primary outcome. Twenty six patients were lost during follow-up and another 19 stopped taking the study drugs because of adverse events and were excluded from the per protocol population (fig 1).
Table 1.
Baseline characteristics of intention to treat population. Values are numbers (percentages) unless stated otherwise
| Characteristics | Ibuprofen arm (n=136) | Amoxicillin-clavulanic acid arm (n=137) | Placebo arm (n=143) |
|---|---|---|---|
| Mean (SD) age (years) | 44.8 (14.5) | 46.1 (14.7) | 44.5 (13.7) |
| Male sex | 60 (44) | 54 (39) | 71 (50) |
| Smoking status: | |||
| Current smoker | 50 (37) | 55 (40) | 53 (37) |
| Former smoker | 20 (15) | 21 (15) | 20 (14) |
| Non-smoker | 66 (48) | 61 (45) | 70 (49) |
| Diabetes mellitus | 5 (4) | 16 (12) | 13 (9) |
| Drugs administered: | |||
| Mucolytics | 45 (33) | 36 (26) | 54 (38) |
| Antihistamines | 6 (4) | 6 (4) | 9 (6) |
| β2 agonists | 28 (21) | 20 (15) | 26 (18) |
| Antitussives | 33 (24) | 29 (21) | 39 (27) |
| Analgesics | 50 (37) | 59 (43) | 75 (52) |
| Mean (SD) days with cough before randomisation visit | 4.1 (1.8) | 4.0 (1.8) | 3.8 (1.9) |
| Increase of dyspnoea | 41 (30) | 46 (34) | 53 (37) |
| Wheezing | 43 (32) | 36 (26) | 53 (37) |
| Chest discomfort | 115 (85) | 117 (85) | 111 (78) |
| Temperature >38ºC* | 5 (4) | 15 (11) | 8 (6) |
| C reactive protein (mg/L)*†: | |||
| <8 | 61 (60) | 46 (45) | 69 (63) |
| 8-20 | 18 (18) | 23 (23) | 20 (18) |
| 21-50 | 19 (19) | 20 (20) | 15 (14) |
| >50 | 3 (3) | 12 (12) | 6 (5) |
*P<0.05.
†Available in 312 patients.
Primary outcome
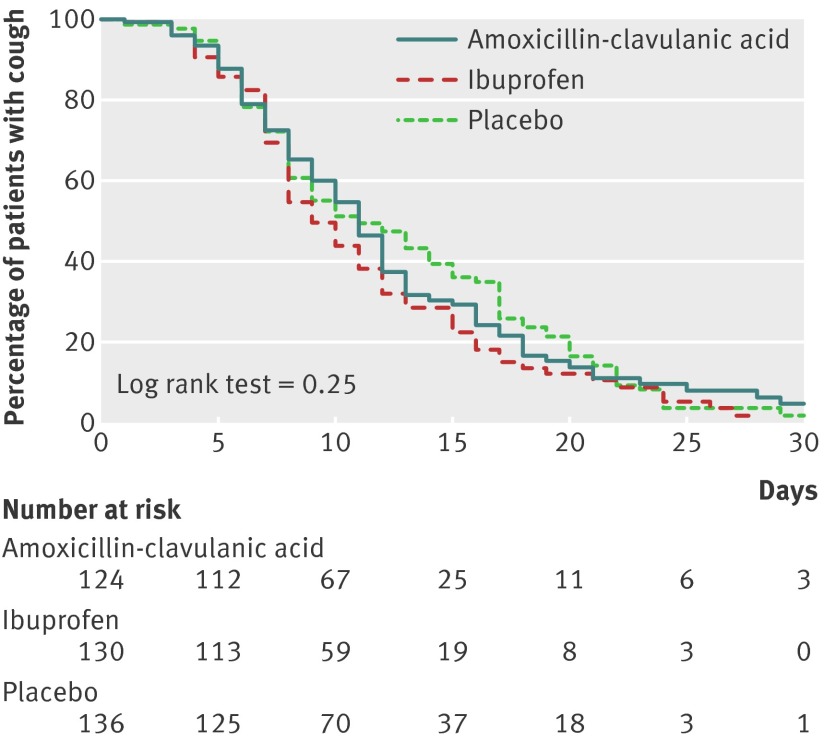
The mean duration of cough was 14.6 (SD 6) days. Figure 2 shows the time with frequent cough, using the Kaplan-Meier survival analysis. The median number of days until the last day patients scored ≥1 in both daytime and night time cough after the baseline visit was 10 days (95% confidence interval 9 to 11 days). The days with frequent cough were slightly lower among patients assigned to ibuprofen (9 days, 8 to 10 days) than those receiving amoxicillin-clavulanic acid (11 days, 10 to 12 days) or placebo (11 days, 8 to 14 days) (table 2). However, no statistically significant differences were observed between the study groups (log rank test=0.25).
Fig 2 Kaplan-Meier survival analysis of days with frequent cough—that is, time (days) with cough from baseline visit until patient last scored ≥1 for both daytime and night time cough
Table 2.
Summary of clinical efficacy results at end of treatment visit in study arm. Values are medians (95% confidence interval) unless stated otherwise
| Outcomes | Intention to treat population (n=416) | Per protocol population (n=371) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Ibuprofen arm | Amoxicillin-clavulanic acid arm | Placebo arm | P value | Ibuprofen arm | Amoxicillin-clavulanic acid arm | Placebo arm | P value | ||
| Primary outcome: | |||||||||
| Days with cough after first visit* | 9 (8 to 10) | 11 (10 to 12) | 11 (8 to 14) | 0.25 | 9 (8 to 10) | 11 (10 to 12) | 10 (7 to 13) | 0.29 | |
| Secondary outcomes: | |||||||||
| No (%) with clinical success at end of treatment day | 117/136 (86) | 107/137 (78) | 123/143 (86) | 0.13 | 116/126 (92) | 106/116 (91) | 122/129 (95) | 0.59 | |
| Time of overall symptom score resolution* (days) | 10 (8 to 12) | 11 (10 to 12) | 13 (10 to 16) | 0.12 | 10 (8 to 12) | 11 (10 to 12) | 13 (10 to 16) | 0.14 | |
*Both intention to treat and per protocol analyses carried out on patients who returned diary (390 and 345, respectively).
Neither amoxicillin-clavulanic acid nor ibuprofen was associated with an increased likelihood of cough resolution compared with placebo (hazard ratio 1.03, 95% confidence interval 0.78 to 1.35 and 1.23, 0.93 to 1.61, respectively). To investigate the hazard ratio for the probability of cough resolution adjusting for potential confounders we calculated three models: model 1 (crude model), model 2 (including treatment group, C reactive protein ≥8 mg/L, and temperature >38ºC as independent variables in the model), and model 3 (treatment group and baseline severity defined as the presence of two or more of C reactive protein ≥8 mg/L; temperature >38ºC; age ≥55 years; current smoker; and dyspnoea or wheezing, or both). No differences were observed in two adjusted Cox proportional models (table 3).
Table 3.
Cox proportional hazards regression models for days with frequent cough, with placebo arm as reference
| Models | Hazard ratio (95% CI) | ||
|---|---|---|---|
| Placebo arm | Amoxicillin-clavulanic acid arm | Ibuprofen arm | |
| Model 1 (crude model) | 1 (reference) | 1.03 (0.78 to 1.35) | 1.23 (0.93 to 1.61) |
| Model 2 (adjusted for temperature >38ºC and C reactive protein ≥8 mg/L) | 1 (reference) | 0.99 (0.73 to 1.34) | 1.23 (0.91 to 1.67) |
| Model 3 (adjusted by baseline severity*) | 1 (reference) | 0.97 (0.71 to 1.32) | 1.22 (0.90 to 1.65) |
*Presence of two or more of C reactive protein ≥8 mg/L; temperature >38ºC; age ≥55 years; current smoker; dyspnoea or wheezing, or both.
Secondary outcomes
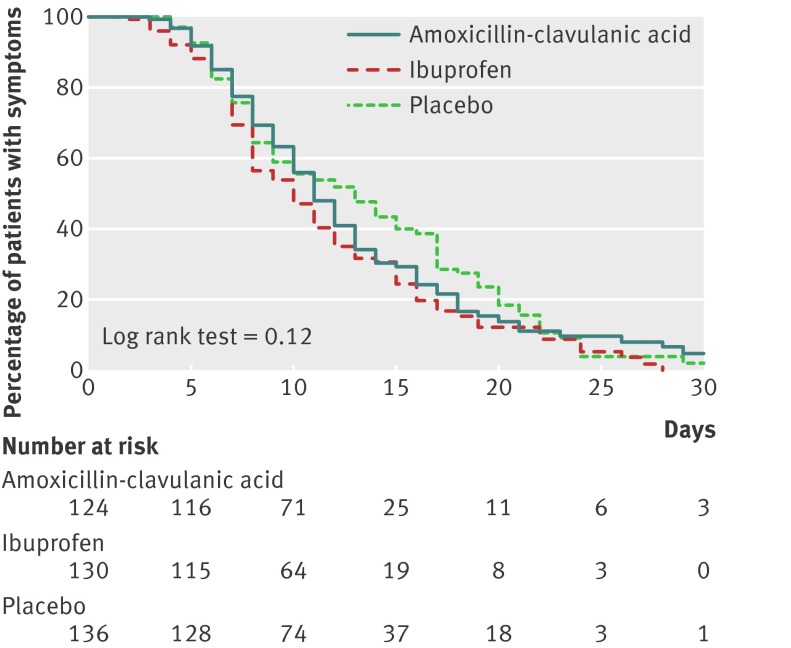
The median number of days reporting any symptom from the initial visit was 11 (95% confidence interval 10 to 12 days). The duration of days with symptoms was slightly lower among patients assigned to the ibuprofen arm (10 days, 8 to 12 days) and was greater among those receiving placebo (13, 10 to 16 days), although the differences were not statistically significant (log rank test=0.12). Figure 3 shows the Kaplan-Meier survival analysis revealing the time in days from the baseline visit until the last day the patient scored ≥1 in any of the boxes of the symptom diary. Clinical success at the second follow-up (end of therapy) visit was also similar in the three study groups (table 2). The results were similar for the per protocol population (table 2).
Fig 3 Kaplan-Meier survival analysis of days with any symptom—that is, time (days) from baseline visit until patient last scored ≥1 in any of five items in symptom diary
Adverse events
Twenty seven patients reported 34 adverse events that were possibly drug related. Of these, 27 reported adverse gastrointestinal events, two suspected allergic reactions, and five other reasons. Among the patients assigned to amoxicillin-clavulanic acid, 16 reported an adverse event (12%), being more common than in the ibuprofen group (seven cases (5%) and in the placebo group (four cases (3%); P=0.008). Most of the adverse events were mild except one case of digestive haemorrhage requiring admission to the intensive care unit in a patient assigned to the antibiotic arm.
Discussion
This study found no differences in the number of days with frequent cough among patients with uncomplicated acute bronchitis and discoloured sputum treated with ibuprofen, amoxicillin-clavulanic acid, or placebo. The trial was sufficiently powered and, to the best of our knowledge, the first to allow conclusions on the efficacy of a non-steroidal anti-inflammatory drug in patients with acute bronchitis compared with an antibiotic and placebo.
Strengths and limitations of this study
This study used drugs that have been in on the market for more than 20 years. Moreover, we took into account the most commonly used agent for each of the two drug groups: ibuprofen among the non-steroidal anti-inflammatory drugs and amoxicillin-clavulanic acid as the antibiotic used in lower respiratory tract infections.20 We did not consider macrolides because we wanted to exclude the possibility of clinical improvement due to an anti-inflammatory effect, thereby avoiding the possibility of overlapping with the group assigned to a non-steroidal anti-inflammatory drug.21
This study does have some limitations. Firstly, it was a single blinded clinical trial. Owing to budget constraints, it was not possible for the drugs to be produced identically. The tablets were, however, similar in size and colour for the three types of drugs and were placed in numbered black pill containers of identical appearance prepared by an independent pharmacist and sealed before dispatch to the investigators. The investigators were instructed to give the containers to the patients while sealed. The possibility of intentioned bias by the investigator was unlikely because the outcomes (responses in the diary) were not evaluated by the investigator. In addition, no commercial or scientific interest was in favour of any of the treatment arms, and the similarity of the results among the three treatment arms also suggests that no such source of bias occurred.
The main outcome was based on information collected from symptom diaries and even though the diary contained only five items some patients found it difficult to complete it appropriately. Another limitation was that we could not rule out pneumonic infections because chest radiography was not requested in all cases. However, given the good and similar results in all three arms it is unlikely that pneumonia may have been unrecognised in an important number of patients. Only patients with acute cough were taken into account in this trial. This makes the generalisability of these results only valid for patients with uncomplicated acute bronchitis.
Regarding the outcome measure used, objective markers of cough, such as the capsaicin test, are not available in the primary care setting. The primary outcome measure used in this study, the daily cough score, is subjective. However, cough scores have been validated against microphone recorders and digital sound pressure level meters for cough frequency and intensity.22
Comparison with other studies
One of the results of this study is that antibiotic treatment was not more effective than placebo in shortening the duration of cough. Systematic analyses of clinical trials also suggest that antibiotics may achieve a reduction, albeit marginal, in the duration of the symptoms.8 23 A review of the Cochrane Library showed that patients given antibiotics were less likely to have a cough than were those given placebo (risk ratio 0.64, 95% confidence interval 0.49 to 0.85), but these results came from only four clinical trials with 275 participants in total.8 Another randomised clinical trial, based on data from the genomics to combat resistance against antibiotics in community-acquired lower respiratory tract infections in Europe (GRACE) study, not included in the Cochrane Library review, has recently been published.24 It constitutes, by far, the largest study carried out, including 16 networks in 12 European countries with 2061 adults aged 18 or older with acute cough of less than one month’s duration as the prominent symptom, and once pneumonia was excluded on the basis of clinical grounds. Symptoms rated moderately bad or worse, which was considered as the main outcome, lasted a median of six days in the group allocated to amoxicillin 3 g daily and seven days in the placebo group, with a non-significant difference (hazard ratio 1.06, 95% confidence interval 0.96 to 1.18). Similar to our study design, Stott and colleagues included only patients with acute bronchitis and purulent sputum and did not observe any statistically significant differences in the resolution of cough between the group treated with antibiotics and the group assigned to the control.18 Current guidelines, endorsed by several national societies, including the National Institute for Health and Care Excellence, the European Respiratory Society, and the Infectious Diseases Society of America, do not recommend the routine use of antibiotics for uncomplicated acute bronchitis in otherwise normal people.2 25 26 None the less, after their introduction in the 1940s, antibacterial agents were rapidly embraced for treatment of acute bronchitis. At present, more than 60% of patients receive antibiotics for acute bronchitis, and it is currently one of the five most commonly cited infections for excessive antibiotic use in outpatients.26 27 28 29 30 31 Many doctors may not give antibiotics on the first visit, but are more likely to prescribe these antibacterials on subsequent visits, mainly if discoloured sputum is present. In a prospective study of more than 3000 adults with acute cough due a lower respiratory tract infection in 13 European countries, Butler and colleagues observed that patients who presented discoloured sputum were prescribed antibiotics 3.2 times more often than those patients without discoloured sputum.32 In other studies this odds ratio of antibiotic prescribing in the presence of discoloured sputum ranged from 2.1 to 4.8.33 34 35 36 37 This aspect is even more important since more than half of the patients with acute bronchitis report the production of purulent sputum.38 Peroxidase released by the leucocytes in sputum causes the colour changes; hence, colour alone should not be considered indicative of bacterial infection.39 Another explanation for the frequent prescription of antibiotics is the lack of distinction between acute and chronic bronchitis. This may explain why clinicians perceive antibiotics to be more beneficial to smokers.40
The efficacy of antibiotics is well established in purulent exacerbations of severe chronic obstructive pulmonary disease,41 and recently our group demonstrated the efficacy of antibiotic treatment in outpatients with mild to moderate chronic obstructive pulmonary disease with acute exacerbations and increased purulence.42 However, in the current study we show that these results in patients with purulent sputum cannot be extrapolated to people with milder acute bronchitis without underlying pulmonary disease, even if they produce discoloured sputum.
Evidence of the effectiveness of non-steroidal anti-inflammatory drugs in this acute respiratory tract infection is lacking. More studies have been published on the common cold, but these studies failed to show a consistent benefit. In a meta-analysis including six clinical trials comparing the effectiveness of non-steroidal anti-inflammatory drugs with placebo and other treatments on the signs and symptoms of the common cold, these drugs failed to shorten the duration of cough but significantly relieved discomfort and pain.43 In a placebo controlled double blind trial in experimental rhinovirus infection, the combination of ibuprofen (400 mg) plus chlorpheniramine (12 mg), administered every 12 hours for 4-5 days, reduced cough significantly, although the effect was optimal when combined with an intranasal antiviral compound (interferon alfa).44 Two clinical trials comparing oral non-steroidal anti-inflammatory drugs with antibiotics in acute bronchitis were published some time ago. In a small clinical trial carried out in Italy, Girbino and colleagues showed a more rapid regression of bronchial inflammation in participants treated with amoxicillin (one 1 g tablet twice daily) and a non-steroidal anti-inflammatory drug (one 700 mg tablet of morniflumate twice daily) compared with those treated only with antibiotic.45 In another double blind, placebo controlled trial carried out in 45 adults admitted to hospital and requiring antibiotic therapy for acute or chronic respiratory tract infections, those assigned to antibiotic treatment with the concomitant use of nimesulide (100 mg twice daily) over 15 to 23 days had a significantly greater and more rapid improvement in the signs and symptoms of respiratory tract infection such as chest pain and cough, than those treated with antibiotic plus placebo.46 As in our study, adverse events were infrequent but more common among patients treated with non-steroidal anti-inflammatory drugs plus antibiotics.
Some studies have evaluated the efficacy of inhaled steroids in patients with cough lasting three weeks or longer. One randomised clinical trial showed a small effect on cough severity in patients taking fluticasone in the second week of disease, but this favourable effect was only detectable in non-smokers.47 In another study, budesonide taken for four weeks did not reduce cough scores compared with placebo in patients coughing for three weeks or longer after an upper respiratory tract infection.48 Two other studies evaluated the effect of inhaled beclomethasone dipropionate on cough score in patients with post-infectious acute cough (less than three weeks’ duration).49 50 In one of the studies treatment with inhaled steroid resulted in a greater reduction of cough frequency than placebo, but in the other study there was no benefit. In a Cochrane review published recently, in which eight clinical trials were included with a total of 570 patients with subacute or chronic cough, inhaled corticosteroids resulted in a slight decrease in cough score, but data about its duration were not available.51
A dose effect cannot be ruled out since the two trials that detected benefits used high dose inhaled steroids (fluticasone diproprionate 500 µg twice daily and beclomethasone dipropionate 400 µg twice daily),47 49 whereas the trial where no benefit was observed used a medium level dose of beclomethasone (100 µg four times daily.).50 In our clinical trial, the possibility of a type II error cannot be discarded, since no statistically significant differences were observed on cough duration with the usual dose of ibuprofen (600 mg three times daily) compared with antibiotic therapy or placebo, but the percentage of adverse events was statistically lower than in the antibiotic arm. Whether the use of higher doses of ibuprofen or other stronger non-steroidal anti-inflammatory drugs would have resulted in statistically significant reduction of cough duration compared with the other arms for patients with uncomplicated acute bronchitis remains unanswered, but it should be weighed against the possibility of more serious side effects.52
Conclusions
Cough is the most common symptom reported by patients with lower respiratory tract infections. To the best of our knowledge, the present randomised clinical trial is the first study to show that an oral anti-inflammatory treatment or an antibiotic are not more effective than placebo for shortening the duration of cough in patients with otherwise non-complicated acute bronchitis with discoloured sputum. These results have important implications for the daily clinical practice of doctors.
What is already known on this topic
Although acute bronchitis is common in primary care and is usually viral in origin, antibiotics are prescribed in more than half of the cases, mainly when sputum is purulent
Recently, bronchitis has been considered more an inflammatory than infectious process and non-steroidal anti-inflammatory drugs (NSAIDs) have been shown to be marginally effective in reducing the duration and intensity of cough in patients with respiratory tract infections
The efficacy of NSAIDs in patients with acute bronchitis has not been assessed in randomised clinical trials
What this study adds
The use of NSAIDs or antibiotics in patients with uncomplicated acute bronchitis and discoloured sputum was not superior to placebo in reducing the number of days with cough
The percentage of adverse events was low but significantly higher among patients treated with antibiotics than those receiving NSAIDs or placebo
We thank the study investigators of the BAAP Study: Francesc López, Anna Vall- Llossera, Xavier Castan, José Manuel Pérez (Primary Care Centre Bon Pastor), Pere Torán (Primary Care Centre Gatassa), Josep Maria Cots, Ylenia Garcia, Consuelo Simón, Isabel Duaso (Primary Care Centre La Marina), Carol Bayona, Concepción Rambla, M. Mar Juárez (Primary Care Centre Valls Urbà), Albert Boada (Primary Care Centre Passeig Maragall), Luis Villanueva, Juan José Montero, M. Carmen Barreiro (Primary Care Centre Rocafonda-Palau), Esperanza Almerich (Primary Care Centre Pineda de Mar), Daniel Colomer, Albert Alum, Dolors López (Primary Care Centre Tordera), Ana Moragas, Carl Llor, Silvia Hernández, Ramon Antón, and Yvonne Fernández (Primary Care Centre Jaume I). We also thank the Consorcio de Apoyo a la Investigación Biomédica en Red (CAIBER) del Instituto de Salud Carlos III) for its support.
Contributors: CL, AM, and MM designed the study. CL and AM coordinated the trial. AM, CL, CB, JMC, and HP were responsible for the recruitment and follow-up of the participants. RM supervised the packaging and labelling of the study drug and contributed to the data analysis. OP-R analysed the data. CL and MM wrote the manuscript. All the authors had access to the data and contributed substantially to the submitted report. CL and MM are the guarantors.
Funding: This clinical trial was supported by a grant from the Instituto de Salud Carlos III (Spanish Ministry of Health) (EC07/90333). The funder had no role in the design, conduct, or analysis of this study.
Competing interests: CL receives research grants from the European Commission (Sixth and Seventh Programme Frameworks), Catalan Society of Family Medicine, and Instituto de Salud Carlos III (Spanish Ministry of Health). Dr. Moragas reports receiving research grants from the Spanish Society of Family Medicine, Fundació Jordi Gol i Gurina, and Instituto de Salud Carlos III (Spanish Ministry of Health). Dr. Miravitlles reports receiving: honoraria for lectures from Bayer-Schering, Boehringer Ingelheim, Pfizer, Nycomed, AstraZeneca, and Novartis, payment for the development of educational presentations from Bayer-Schering, serving on the advisory boards of Bayer-Schering, Boehringer Ingelheim, Pfizer, Nycomed, GlaxoSmithKline, Almirall, AstraZeneca, and Novartis; and receiving consulting fees from Bayer-Schering, Boehringer-Ingelheim, Pfizer, Nycomed, GlaxoSmithKline, Almirall, AstraZeneca, and Novartis. The other authors do not report disclosures.
Ethical approval: This study was approved by the Research and Ethics Committee of Primary Care Fundació Jordi Gol i Gurina (Barcelona, Spain; project No P07/15). Approval was also obtained from the Spanish Agency of Medicines and Health Products and the EudraCT (ref: 2007-006727-12).
Data sharing: No additional data available.
Cite this as: BMJ 2013;347:f5762
References
- 1.Macfarlane J, Holmes W, Gard P, Macfarlane R, Rose D, Weston V, et al. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax 2001;56:109-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, et al; Joint Taskforce of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases. Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect 2011;17(Suppl 6):E1-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashworth M, Charlton J, Ballard K, Latinovic R, Gulliford M. Variations in antibiotic prescribing and consultation rates for acute respiratory infection in UK general practices 1995-2000. Br J Gen Pract 2005;55:603-8. [PMC free article] [PubMed] [Google Scholar]
- 4.Chalmers JD, Hill AT. Investigation of “non-responding” presumed lower respiratory tract infection in primary care. BMJ 2011;343:d5840. [DOI] [PubMed] [Google Scholar]
- 5.Boivin G, Abed Y, Pelletier G, Ruel L, Moisan D, Côté S, et al. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect Dis 2002;186:1330-4. [DOI] [PubMed] [Google Scholar]
- 6.Bastien N, Ward D, Van Caeseele P, Brandt K, Lee SH, McNabb G, et al. Human metapneumovirus infection in the Canadian population. J Clin Microbiol 2003;41:4642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kicska G, Zhuang H, Alavi A. Acute bronchitis imaged with F-18 FDG positron emission tomography. Clin Nucl Med 2003;28:511-2. [DOI] [PubMed] [Google Scholar]
- 8.Smith S, Fahey T, Smucny J, Becker L. Antibiotics for acute bronchitis. Cochrane Database Syst Rev 2012;(4):CD000245. [DOI] [PubMed] [Google Scholar]
- 9.Butler CC, Hood K, Verheij T, Little P, Melbye H, Nuttall J, et al. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries. BMJ 2009;338:b2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goossens H, Ferech M, Vander Stichele R, Elseviers M, ESAC project group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 2005;365:579-87. [DOI] [PubMed] [Google Scholar]
- 11.Smith SM, Schroeder K, Fahey T. Over-the-counter (OTC) medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev 2012;(4):CD001831. [DOI] [PubMed] [Google Scholar]
- 12.Becker LA, Hom J, Villasis-Keever M, van der Wouden JC. Beta2-agonists for acute bronchitis. Cochrane Database Syst Rev 2011;(7):CD001726. [DOI] [PubMed] [Google Scholar]
- 13.Raherison C, Poirier R, Daurès JP, Romand P, Grignet JP, Arsac P, et al. Lower respiratory tract infections in adults: non-antibiotic prescriptions by GPs. Respir Med 2003;97:995-1000. [DOI] [PubMed] [Google Scholar]
- 14.Llor C, Moragas A, Bayona C, Morros R, Pera H, Cots JM, et al. Effectiveness of anti-inflammatory treatment versus antibiotic therapy and placebo for patients with non-complicated acute bronchitis with purulent sputum. The BAAP Study protocol. BMC Pulm Med 2011;11:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chow AW, Hall CB, Klein JO, Kammer RB, Meyer RD, Remington JS. Evaluation of new anti-infective drugs for the treatment of respiratory tract infections. Infectious Diseases Society of America and the Food and Drug Administration. Clin Infect Dis 1992;15:S62-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nduba VN, Mwachari CW, Magaret AS, Park DR, Kigo A, Hooton TM, et al. Placebo found equivalent to amoxicillin for treatment of acute bronchitis in Nairobi, Kenya: a triple blind, randomised, equivalence trial. Thorax 2008;63:999-1005. [DOI] [PubMed] [Google Scholar]
- 17.Moragas A, Llor C, Gabarrús A, Miravitlles M. Reliability of a self-administered diary of symptoms for assessing the evolution of acute bronchitis. Arch Bronconeumol 2012;48:261-2. [DOI] [PubMed] [Google Scholar]
- 18.Stott NC, West RR. Randomised controlled trial of antibiotics in patients with cough and purulent sputum. BMJ 1976;2:556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Therneau TM, Grambsch PM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515-26. [Google Scholar]
- 20.Miravitlles M, Monsó E, Mensa J, Aguarón Pérez J, Barberán J, Bárcena Caamaño M, et al. Antimicrobial treatment of exacerbation in chronic obstructive pulmonary disease: 2007 consensus statement. Arch Bronconeumol 2008;44:100-8. [DOI] [PubMed] [Google Scholar]
- 21.Sevilla-Sánchez D, Soy-Muner D, Soler-Porcar N. Usefulness of macrolides as anti-inflammatories in respiratory diseases. Arch Bronconeumol 2010;46:244-54. [DOI] [PubMed] [Google Scholar]
- 22.Freestone C, Eccles R. Assessment of the antitussive efficacy of codeine in cough associated with common cold. J Pharm Pharmacol 1997;49:1045-9. [DOI] [PubMed] [Google Scholar]
- 23.Bent S, Saint S, Vittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med 1999;107:62-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Little P, Stuart B, Moore M, Coenen S, Butler CC, Godycki-Cwirko M, et al; GRACE consortium. Amoxicillin for acute lower-respiratory-tract infection in primary care when pneumonia is not suspected: a 12-country, randomised, placebo-controlled trial. Lancet Infect Dis 2013;13:123-9. [DOI] [PubMed] [Google Scholar]
- 25.Centre for Clinical Practice at NICE (UK). Respiratory tract infections—antibiotic prescribing: prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care. (NICE Clinical Guideline No 69.) NICE; 2008. www.ncbi.nlm.nih.gov/books/NBK53632/. [PubMed]
- 26.Snow V, Mottur-Pilson C, Gonzales R; American Academy of Family Physicians; American College of Physicians-American Society of Internal Medicine; Centers for Disease Control; Infectious Diseases Society of America. Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med 2001;134:518-20. [DOI] [PubMed] [Google Scholar]
- 27.Macfarlane JT, Worboys M. The changing management of acute bronchitis in Britain, 1940-1970: the impact of antibiotics. Med Hist 2008;52:47-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linder JA. Editorial commentary: antibiotics for treatment of acute respiratory tract infections: decreasing benefit, increasing risk, and the irrelevance of antimicrobial resistance. Clin Infect Dis 2008;47:744-6. [DOI] [PubMed] [Google Scholar]
- 29.Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 2001;33:757-62. [DOI] [PubMed] [Google Scholar]
- 30.Mainous AG 3rd, Zoorob RH, Hueston WJ. Current management of acute bronchitis in ambulatory care: the use of antibiotics and bronchodilators, Arch Fam Med 1996;5:79-83. [DOI] [PubMed] [Google Scholar]
- 31.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997;278:901-4. [PubMed] [Google Scholar]
- 32.Butler CC, Kelly MJ, Hood K, Schaberg T, Melbye H, Serra-Prat M, et al. Antibiotic prescribing for discoloured sputum in acute cough/lower respiratory tract infection. Eur Respir J 2011;38:119-25. [DOI] [PubMed] [Google Scholar]
- 33.Gonzales R, Barrett PH, Steiner JF. The relation between purulent manifestations and antibiotic treatment of upper respiratory tract infections. J Gen Intern Med 1999;14:151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hummers-Pradier E, Pelz J, Himmel W, Kochen MM. Treatment of respiratory tract infections: a study in 18 general practices in Germany. Eur J Gen Pract 1999;5:15-20. [Google Scholar]
- 35.Fischer T, Fischer S, Kochen MM, Hummers-Pradier E. Influence of patient symptoms and physical findings on general practitioners’ treatment of respiratory tract infections: a direct observation study. BMC Fam Pract 2005;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coenen S, Michiels B, Renard D, Denekens J, Van Royen P. Antibiotic prescribing for acute cough: the effect of perceived patient demand. Br J Gen Pract 2006;56:183-90. [PMC free article] [PubMed] [Google Scholar]
- 37.Dosh SA, Hickner JM, Mainous AG, Mainous AG 3rd, Ebell MH. Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis—an UPRNet study. J Fam Pract 2000;49:407-14. [PubMed] [Google Scholar]
- 38.Dunlay J, Reinhardt R. Clinical features and treatment of acute bronchitis. J Fam Pract 1984;18:719-22. [PubMed] [Google Scholar]
- 39.Miravitlles M, Kruesmann F, Haverstock D, Perroncel R, Choudhri S, Arvis P. Sputum colour and bacteria in chronic bronchitis exacerbations: a pooled analysis. Eur Respir J 2012;39:1354-60. [DOI] [PubMed] [Google Scholar]
- 40.Stanton N, Hood K, Kelly MJ, Nuttall J, Gillespie D, Verheij T, et al. Are smokers with acute cough in primary care prescribed antibiotics more often, and to what benefit? An observational study in 13 European countries. Eur Respir J 2010;35:761-7. [DOI] [PubMed] [Google Scholar]
- 41.Anthonisen NR, Manfreda J, Warren CPW, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987;106:196-204. [DOI] [PubMed] [Google Scholar]
- 42.Llor C, Moragas A, Hernández S, Bayona C, Miravitlles M. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate COPD. Am J Respir Crit Care Med 2012;186:716-23. [DOI] [PubMed] [Google Scholar]
- 43.Kim SY, Chang YJ, Cho HM, Hwang YW, Moon YS. Non-steroidal anti-inflammatory drugs for the common cold. Cochrane Database Syst Rev 2009;(3):CD006362. [DOI] [PubMed] [Google Scholar]
- 44.Gwaltney JM Jr, Winther B, Patrie JT, Hendley JO. Combined antiviral-antimediator treatment for the common cold. J Infect Dis 2002;186:147-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Girbino G, Oliani C, Lauriello G, Condoluci M. [A new anti-inflammatory-analgesic-antipyretic for the treatment of acute disease of the bronchi ]. Riv Eur Sci Med Farmacol 1990;12:359-66. [PubMed] [Google Scholar]
- 46.Reiner M. Nimesulide and antibiotics in the treatment of acute infections of the respiratory tract. Curr Med Res Opin 1983;8:487-92. [DOI] [PubMed] [Google Scholar]
- 47.Ponsioen BP, Hop WC, Vermue NA, Dekhuijzen PN, Bohnen AM. Efficacy of fluticasone on cough: a randomised controlled trial. Eur Respir J 2005;25:147-52. [DOI] [PubMed] [Google Scholar]
- 48.Pornsuriyasak P, Charoenpan P, Vongviva K, Thakkinstian A. Inhaled corticosteroid for persistent cough following upper respiratory tract infection. Respirology 2005;10:520-4. [DOI] [PubMed] [Google Scholar]
- 49.Gillissen A, Richter A, Oster H. Clinical efficacy of short-term treatment with extra-fine HFA beclomethasone dipropionate in patients with post-infectious persistent cough. J Physiol Pharmacol 2007;58 Suppl 5(Pt 1):223-32. [PubMed]
- 50.Frank A, Dash CH. Inhaled beclomethasone dipropionate in acute infections of the respiratory tract. Respiration 1985;48:122-6. [DOI] [PubMed] [Google Scholar]
- 51.Johnstone KJ, Chang AB, Fong KM, Bowman RV, Yang IA. Inhaled corticosteroids for subacute and chronic cough in adults. Cochrane Database Syst Rev 2013;(3):CD009305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.El-Gohary M, Hay AD, Coventry P, Moore M, Stuart B, Little P. Corticosteroids for acute and subacute cough following respiratory tract infection: a systematic review. Fam Pract 2013;30:492-500. [DOI] [PubMed] [Google Scholar]