Abstract
Introduction:
The great majority of smokers relapse when they make quit attempts. Therefore, understanding the process of relapse may guide the development of more effective smoking cessation or relapse prevention treatments. The goal of this research is to extend our understanding of the context of initial lapses that occur within 8 weeks of quitting by using more comprehensive assessments of context, a contemporary sample, and sophisticated analytic techniques.
Methods:
Participants from a randomized controlled smoking cessation trial completed baseline assessments of demographics and tobacco dependence, a daily smoking calendar to determine latency to lapse and relapse (7 consecutive days of smoking), and an assessment of initial lapse context (affect, location, activity, interpersonal, smoke exposure, and cigarette availability). Latent class analysis (LCA) was used to analyze the 6 early lapse (within the first 8 weeks; N = 551) context dimensions; logistic regression and Cox regression were used to relate context to cessation outcomes.
Results:
LCA revealed 5 distinct initial lapse context classes (talking, with friends, angry; social; alone; with spouse, angry; and with smoking spouse) that were differentially related to cessation outcome. The easy availability of cigarettes characterized almost 75% of lapses, but being with friends, drinking, and not being at home were associated with a lower likelihood of progression to relapse.
Conclusions:
Early lapsing is highly related to ultimate relapse, and lapsing in frequently experienced contexts seemed most strongly linked with progression to full relapse.
INTRODUCTION
Despite continued public health and clinical efforts, data suggest that more than 20% of adults in the United States currently smoke cigarettes (Plies, Ward, & Lucas, 2010). More than 40% of smokers report failed quit attempts in the preceding year (Hughes & Callas, 2010). Relapse is decidedly the most common outcome among smokers attempting to quit; even the most effective combinations of pharmacotherapy and psychosocial interventions result in relapse rates of 70% or higher (Fiore et al., 2008; Piasecki, 2006). These data reflect the fact that effective relapse prevention remains an unrealized goal of smoking treatment research (Hajek, Stead, West, Jarvis, & Lancaster, 2009). Increased knowledge regarding the determinants of relapse may hold the key to improved relapse prevention interventions.
The process of smoking relapse necessarily involves several stages: establishment of initial cessation, an initial lapse (smoking a first cigarette), and ultimate relapse (a return to regular smoking; Shiffman et al., 2006). The study of each of these is worthy in its own right, because each is a necessary condition of relapse and because these steps appear to be associated with different risk factors or vulnerabilities (Japuntich et al., 2011a; Japuntich, Piper, Leventhal, Bolt, & Baker, 2011b; Shiffman et al., 2006). In this article, we focus on factors associated with the occurrence of a lapse within the first 8 weeks of a cessation attempt (i.e., early lapse) and how these are related to transition to relapse.
Previous research on lapsing using ecological momentary assessment (EMA) methods has shown that lapse vulnerability (vs. merely being tempted to smoke, but not smoking) is powerfully associated with tobacco dependence (e.g., morning craving) and smoking cues (e.g., others smoking; Shiffman et al., 1997; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996c) and that lapse risk was significantly signaled by a drop in self-efficacy several days prior to the lapse (Gwaltney, Shiffman, Balabanis, & Paty, 2005). Other research has found that lapsing is associated with tobacco dependence, being female, non-White, and less educated and with several environmental or contextual features (e.g., smokers and supportive individuals in the social network, smoking in the home or work environment; Japuntich et al., 2011a). Relatively few factors, none of them context factors, have been found to predict the transition from lapse to relapse (e.g., tobacco dependence, female gender; Japuntich et al., 2011a). EMA data show that a more rapid lapse-to-relapse progression is predicted by severe tobacco dependence (e.g., heavy smoking, strong urges), stressors, flagging self-efficacy, and mounting demoralization or hopelessness (Gwaltney et al., 2001, 2005; Kirchner, Shiffman, & Wileyto, 2012; Shiffman et al., 1996a, 1996b).
Shiffman (2005) notes the essential importance of the initial lapse—it is not only the first episode of smoking but it is highly predictive of ultimate failure given the high rate at which lapses lead to ultimate relapse (Kenford et al., 1994). This apparent inability to recover from a lapse may be due to multiple factors, acting alone or in concert. The lapse may merely index a host of vulnerabilities (e.g., nicotine dependence) that themselves directly cause relapse. Or, the lapse may actually instigate or spur processes that contribute to relapse progression, such as a decrease in self-efficacy (Gwaltney et al., 2005; Kirchner et al., 2012; Shiffman, 2005). Finally, a lapse might reinstate withdrawal processes or serve to “prime” appetitive motivational processes (de Wit & Stewart, 1981; Kirchner et al., 2012).
Much of the recent research in this area has focused on dynamic symptom patterns or trait-like person factors as they are related to lapse and relapse (Gwaltney et al., 2005; Japuntich et al., 2011a; Shiffman, 2005). Yet, there is strong evidence that momentary or situational factors, as well as interactions among trait-like person factors and contextual factors, play a major role in determining lapse occurrence, and perhaps, lapse consequences. Unfortunately, relatively little research has been directed at understanding the nature of the contextual influences on lapsing. Much of the work in this area is based on EMA data, which allows researchers to capture real-time data and reduce the threat of certain biases, but limits the amount of information that can be reasonably obtained (e.g., participants in Ferguson and Shiffman’s [2010] research were only able to report one primary trigger of a particular lapse). In addition, the relations between features of the lapse context, symptom dynamics, and person factors have been inadequately explored. Research has focused on variable-centered approaches to this topic, that is, on examining correlations and moderated effects among such variables (cf. Shiffman, 1986). However, person-centered approaches could also shed light on this topic; that is, approaches that create a typology of persons based on the contexts in which they lapse. Finally, it is important to update our knowledge about lapse contexts. In today’s world of smoking restrictions, smoking contexts have, no doubt, changed dramatically since the relapse process studies of the 1980s and 1990s (Bliss, Garvey, Heinold, & Hitchcock, 1989; O’Connell & Martin, 1987).
The current research, using a paper-and-pencil assessment collected from 2005–2007, taps multiple dimensions of the initial lapse context in a fairly current sample of smokers. Latent class analysis (LCA; Collins & Lanza, 2010) was used to help identify a structure or taxonomy of persons based on lapse context. LCA is a statistical model that identifies underlying subgroups of individuals based on multiple indicators. Previously, LCA has been used to identify subgroups characterized in terms of their smoking patterns (Chen et al., 2004; Henry & Muthen, 2010). In this study, subgroups will be identified based on early lapsers’ affect, smoking availability, and environmental context at initial lapse. We also examined whether person factors such as gender, age, race, educational attainment, and level of tobacco dependence are related to lapse and ultimate relapse risk. Therefore, the current research used a person-centered approach to synthesize relatively rich data on the symptoms, locations, social features, and activities that characterized the features of lapse contexts that occurred within the first 8 weeks of a quit attempt. Synthetic classes were then related with relapse likelihood and person factors that have previously been associated with relapse. Such information could be important for understanding relapse mechanisms and tailoring treatment.
METHODS
Participants
Daily smokers (N = 1,504) who were motivated to quit were recruited via advertisements using several types of media to participate in a smoking cessation randomized placebo-controlled trial (see Piper et al., 2009). Participants were randomized to one of six treatment conditions: Bupropion SR (n = 264); Nicotine lozenge (n = 260); Nicotine patch (n = 262); Nicotine patch + Nicotine lozenge (n = 267); Bupropion SR + Nicotine lozenge (n = 262), or Placebo (five placebo conditions that matched the five active conditions; n = 189). All medications were provided for 8 weeks postquit except the nicotine lozenge, which was provided for 12 weeks postquit (consistent with prescribing instructions). Participants also received six brief (10-min) counseling sessions. Early lapsers were defined as those who had established 24hr of abstinence during the first week of their cessation attempt and reported smoking their first cigarette within 8 weeks of the target quit day.
Procedure
At study visits 1, 2, 4, and 8 weeks postquit, participants completed a timeline followback assessment of smoking on each day following the target quit day. The initial lapse was defined as the first cigarette smoked after waking on the target quit day. Participants who lapsed completed a paper-and-pencil assessment of the initial lapse context. If a participant missed a study visit, this procedure was completed at the next visit. The median latency between the initial lapse and lapse assessment was 5 days (range: 1–56; mean = 8.5). Seven-day point- prevalent abstinence at 6 months was biochemically confirmed with an exhaled carbon monoxide level less than 10 parts per million.
Assessments
Initial Lapse Context Data
For the lapse context assessment, participants were asked: How were you feeling? What were you doing? Where were you? Who were you with? Was anyone else smoking? Were cigarettes available? For each of the six context dimensions, participants received a list of possible responses. On four questions, participants were allowed to endorse all responses that applied: affective states (angry/irritable/frustrated; happy/excited; sad/lonely; worried/anxious; bored; restless; hungry; don’t know), concurrent activities (work/school; chores; driving/riding; TV/music; telephone; eating; drinking—coffee, alcohol, other; exercise; leisure; talking; inactive), and presence of others and other smokers (spouse/partner; other family; friend; stranger; other; no one). Participants were required to choose only one location (home; work/school; vehicle; bar/restaurant; public place; others’ home; outside; other) and one of three levels of cigarette availability (easily available = 1, available with difficulty = 2, and not available = 3).
Tobacco Dependence
Tobacco dependence was assessed at baseline using the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991) and the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68; Piper et al., 2004). We analyzed the WISDM-68 Primary Dependence Motives (PDM) scale and specific Secondary Dependence Motives subscales that we believed a priori would be related to relapse context: Cue Exposure (smoking because of nonsocial smoking cues), Negative Reinforcement (smoking to ameliorate negative states), Positive Reinforcement (smoking to experience positive effects, e.g., “buzz” or “high”), and Social/Environmental Goads (smoking because of social cues).
Analytic Plan
We examined the relative frequency of initial lapse contexts (i.e., affect, activities, location, others present, other smokers present, and cigarette availability) and conducted LCAs using SAS PROC LCA (Lanza, Collins, Lemmon, & Schafer, 2007; Lanza, Dziak, Huang, Xu, & Collins, 2011) to identify subgroups of smokers based on their pattern of responses to six lapse context variables. Latent class models estimate the relative size of each subgroup and the probability of endorsing each response option to each item, conditional on latent class membership. Model identification was assessed using 100 sets of random starting values for each candidate model. The final model was selected by comparing models with different numbers of latent classes using the Akaike’s information criterion (AIC; Akaike, 1974) and Bayesian information criterion (BIC; Schwarz, 1978), where smaller values indicate more optimal balance between model fit and parsimony. A comprehensive introduction to LCA and details about the mathematical model can be found elsewhere (Collins & Lanza, 2010; Lanza et al., 2007).
Participants were assigned to a specific latent class based on their posterior probabilities. Logistic regression and Cox regression analyses were conducted to determine whether lapse contexts and lapse class membership were related to 6-month point prevalence abstinence and latency to relapse. Finally, we examined whether individual difference variables were related to lapse classes or any lapse context that was endorsed by at least 10% of the sample. The individual difference variables were ones that had previously been associated with relapse vulnerability and included: gender, race (Whites vs. non-Whites), education (no more than high school degree/general equivalency degree vs. some college vs. 4-year college degree or more), age and the dependence markers, FTND score, and specific WISDM scale scores. To control for Type I error in the individual differences analyses, we used the false discovery rate of error control (Benjamini & Hochberg, 1995; Keselman, Cribbie, & Holland, 2002) within each family of analyses (e.g., analyses of anger, work, drinking). All reported p values comparing individual difference variables have been corrected using the false discovery rate error control and can be evaluated as p < .05 indicating statistical significance.
RESULTS
Of the 1,504 enrolled in the clinical trial, 1,190 people successfully quit smoking for at least 24hr in the first week of the cessation attempt. Approximately 63% (753/1,190) of participants who established initial cessation subsequently lapsed during the first 8 weeks postquit (mean days until lapse = 9.75, SD = 13.93) and 73.2% of early lapsers (551/753) provided contextual information about their initial lapse. See Table 1 for baseline demographics and smoking information comparing early lapsers (n = 753) to those who were continuously abstinent for the first 8 weeks postquit (n = 437).
Table 1.
Demographic and Smoking Information
| Initial lapse within 8 weeks (n = 753) | Continuously abstinent through 8 weeks (n = 437) | Group comparisons | |
|---|---|---|---|
| Female % | 60.4 | 52.9 | χ2 = 6.48, p = .011 |
| Married % | 41.5 | 56.8 | χ2 = 26.38, p < .001 |
| Biochemically confirmed point-prevalent abstinence at 6 months % | 21.6 | 70.7 | χ2 = 278.14, p < .001 |
| Race | |||
| White % | 83.5 | 89.5 | χ2 = 11.78, p = .038 |
| Black % | 14.0 | 8.0 | |
| Other race % | 2.5 | 2.0 | |
| Education | |||
| High school education or less % | 29.5 | 23.4 | χ2 = 18.26, p < .001 |
| Some college/2-year degree % | 50.3 | 46.1 | |
| 4-year college graduate % | 20.2 | 30.5 | |
| Age (M [SD]) | 44.62 (10.84) | 45.01 (11.91) | Ns |
| Cigarettes/day (M [SD]) | 21.18 (8.67) | 20.76 (8.99) | Ns |
| FTND (M [SD]) | 5.39 (2.10) | 5.07 (2.15) | t = 2.51, p = .012 |
| Number of previous quit attempts (M [SD]) | 5.18 (7.07) | 6.71 (12.02) | t = 2.43, p = .016 |
| Motivation (M [SD]) | 9.07 (1.06) | 9.18 (0.99) | ns |
Note. FTND = Fagerström Test for Nicotine Dependence; ns = not statistically significant.
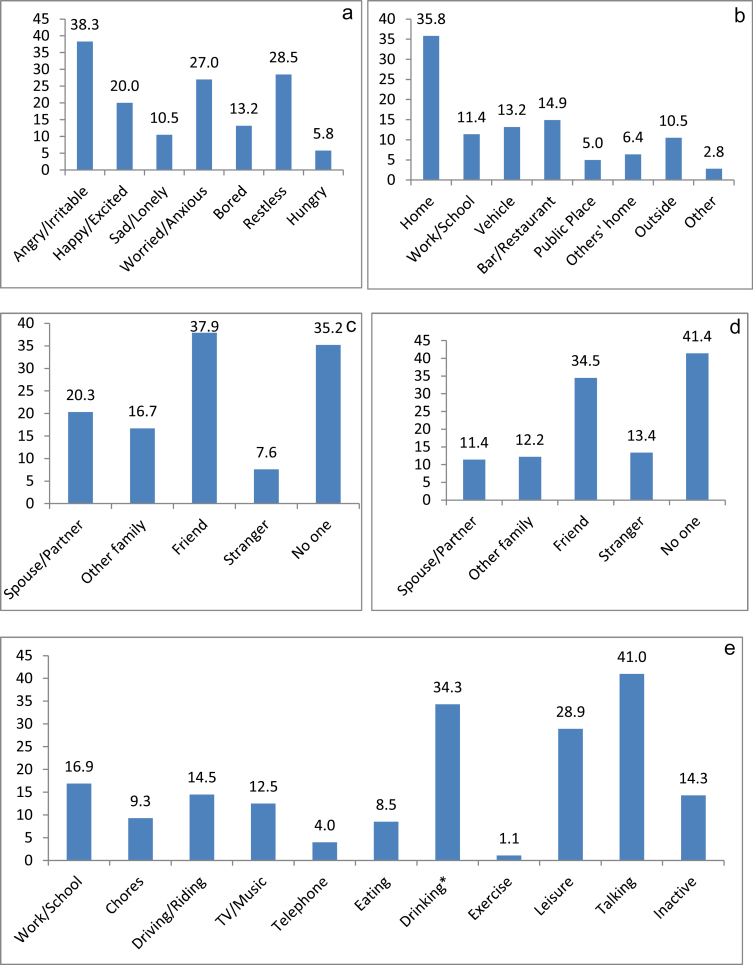
Lapse Contexts
Figure 1 illustrates participants’ reported affect, activities, location, access to cigarettes, and exposure to others’ smoking during their first lapse. The most common affective or symptom states during an initial lapse were feeling angry, irritable, and/or frustrated and feeling worried and/or anxious. Overall, 47.2% of participants endorsed negative affect (i.e., anger, sadness, and worrying), whereas 20.0% reported positive affect (i.e., feeling happy and/or excited) at the time of lapse. The two most common activities reported at the time of the first lapse were talking and “drinking—coffee, alcohol, other.” Home was the most common lapse location, followed by bar/restaurant and vehicle. Participants reported that they were most likely to be alone or with a friend at the time of the lapse. Similar proportions of all first lapses occurred when a friend was smoking (37.9%) or when no one was smoking (35.2%). The vast majority (74.9%) of participants reported that cigarettes were easily available at the time of initial lapse.
Figure 1.
Percentage of early lapsers reporting each context at the time of first lapse. (a) depicts affective or symptom context, (b) depicts location, (c) depicts who the participant was with at the time of the lapse, (d) depicts who was smoking around the participant at the time of the lapse, and (e) depicts activity context. For (b), participants were forced to select a single location, but for all other figures, participants were allowed to select all that applied. *Drinking any beverage, not exclusively alcoholic or caffeinated beverages.
Models with two through five latent classes were compared; the six-class solution was not sufficiently identified. Model fit information criteria indicated that a five-class solution was optimal (for models with 2, 3, 4, and 5 classes, respectively, AIC = 1,593, 1,330, 1,152, and 1,071 and BIC = 1,718, 1,519, 1,406, and 1,390). This solution (see Table 2) yielded five latent classes that were qualitatively distinct in terms of their lapse context profile. Class 1 (“Angry, Talking with Friend”; 20% of lapsers) represents smokers who lapsed while they were talking with a friend, feeling angry, and who had cigarettes readily available. Class 2 (“Social”; 28% of lapsers) represents smokers who lapsed when they were out in public, having fun with friends, feeling happy, and who had cigarettes easily available. Class 3 (“Alone”; 35% of lapsers) represents participants who lapsed while at home, alone, and who had cigarettes available to them. Class 4 (“Angry, With Spouse”; 6% of lapsers) represents participants who lapsed while at home with their spouse, feeling angry, with no one else smoking, and for whom cigarettes were available only with difficulty. Finally, Class 5 (“With Spouse Smoking”; 11% of lapsers) represents participants who lapsed while at home and talking with their spouse, and the spouse was smoking.
Table 2.
Latent Class Analysis of Smoking Contexts
| Indicators of context | Class 1: angry, talking with friend | Class 2: social | Class 3: alone | Class 4: angry, with spouse | Class 5: with spouse smoking |
|---|---|---|---|---|---|
| Latent class prevalences | |||||
| 19% | 28% | 35% | 7% | 11% | |
| Item-response probabilities | |||||
| Smoking availability | |||||
| Easily available | 0.79 | 0.91 | 0.64 | 0.34 | 0.86 |
| Available with difficulty | 0.17 | 0.08 | 0.24 | 0.55 | 0.11 |
| Not available | 0.04 | 0.01 | 0.12 | 0.11 | 0.03 |
| Location | |||||
| Home/vehicle/other’s home | 0.44 | 0.29 | 0.85 | 0.90 | 0.65 |
| Work/school/other | 0.37 | 0.06 | 0.12 | 0.03 | 0.07 |
| Bar/restaurant/public place | 0.19 | 0.64 | 0.03 | 0.07 | 0.28 |
| Probability of a yes response | |||||
| Talking | 0.55 | 0.65 | 0.07 | 0.39 | 0.65 |
| Leisure activities | 0.06 | 0.53 | 0.22 | 0.25 | 0.34 |
| Drinking | 0.07 | 0.75 | 0.16 | 0.24 | 0.45 |
| With spouse | 0.02 | 0.17 | 0.00 | 0.60 | 1.00 |
| With friend | 0.50 | 0.86 | 0.00 | 0.16 | 0.27 |
| With no one | 0.02 | 0.00 | 1.00 | 0.00 | 0.00 |
| Spouse was smoking | 0.00 | 0.00 | 0.01 | 0.00 | 1.00 |
| No one was smoking | 0.08 | 0.02 | 0.94 | 1.00 | 0.00 |
| Angry | 0.64 | 0.14 | 0.41 | 0.59 | 0.34 |
| Happy | 0.01 | 0.52 | 0.05 | 0.00 | 0.31 |
Because entropy for the five-class model was very high (.93), individuals could be assigned to latent classes with little classification error. We assigned individuals to the class with their maximum posterior probability of membership for subsequent analyses. There was a significant difference in latency to lapse among the classes (F(4, 546) = 2.42, p = .047), but post-hoc analyses revealed no significant differences in days to lapse among any pair of latent classes (Class 1: M = 12.11, SD = 13.69; Class 2: M = 14.72, SD = 15.78; Class 3: M = 10.74, SD = 13.94; Class 4: M = 9.16, SD = 13.87; Class 5: M = 10.05, SD = 12.66).
Lapse Context and Relapse
Compared with those who were continuously abstinent for the first 8 weeks, early lapsers were significantly more likely to have relapsed by 6 months (see Table 1). We examined the relation between latency to relapse and the most commonly endorsed lapse context features: negative affect, talking, drinking, location, being with friends, being alone, being with friends smoking, and cigarette availability. Cox regression analyses showed that smokers were more likely to relapse when they reported an initial lapse context in which they were not drinking (hazard ratio [HR] = 0.73, Wald = 7.00, p = .01, 95% CI = 0.58–0.92) and there was a trend to be more likely to relapse when they experienced negative affect at the time of the lapse (HR = 0.82, Wald = 3.15, p = .08, 95% CI = 0.66–1.02). None of the other specific lapse contexts we assessed were related to relapse latency.
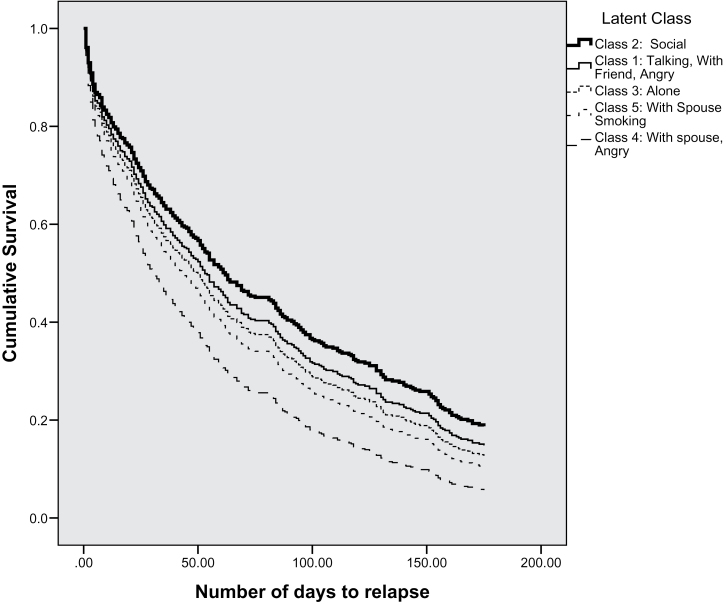
Latent class membership was significantly associated with 6-month point prevalence abstinence (Wald = 11.22, p = .02), even after controlling for treatment. (It should be noted that there was no significant difference in lapse class distribution among treatment groups.) Classes 1 (“Angry, Talking with Friend”) and 2 (“Social”) had higher abstinence rates (25.2% and 29.7%, respectively) than did Classes 3 (“Alone”; 17.5% abstinent), 4 (“Angry, With Spouse”; 10.8% abstinent), and 5 (“With Spouse Smoking”; 17.7%). Latent class was not significantly related to latency to relapse (χ2 = 7.30, p = .12). The survival curves in Figure 2 illustrate that there does appear to be some separation among the classes on latency to relapse, but there may not be sufficient statistical power to detect these effects (Ns range: 29–152).
Figure 2.
Survival curves for latency to relapse by latent class (N = 407).
Lapse Context Features and Individual Difference Variables
Specific Context Variables
We determined the relations between person factors and endorsement of specific lapse context features among early lapsers (see Supplementary Table 1). Men were significantly more likely to have their initial lapse at work than were women. White smokers were significantly more likely to lapse when feeling restless or drinking (alcohol, coffee, etc.) than were non-Whites. Younger smokers were more likely to report lapsing while feeling happy, drinking any beverage, being with friends, being with friends who were smoking, and in a bar/restaurant versus at home. Older smokers were more likely to report lapsing when they were alone and no one was smoking around them at the time of lapse. Smokers with higher FTND scores were more likely to lapse when feeling restless or sad, not drinking, and reporting inactivity. Smokers with higher WISDM Cue Exposure scores were more likely to lapse when feeling restless and while drinking. Higher WISDM Negative Reinforcement scores were associated with lapsing while feeling restless or sad, and higher WISDM Positive Reinforcement scores were associated with lapsing while feeling restless and drinking. Finally, higher WISDM Social/Environmental Goads scores were associated with lapsing while feeling happy, drinking, being with friends, and being with smoking friends. Conversely, lower WISDM Social/Environmental Goads scores were associated with lapsing alone when no one was smoking. There were no significant differences in lapse context by education or WISDM PDM score.
Lapse Latent Classes
The latent classes differed significantly in mean age (F(4, 549) = 4.81, p = .001); those in Class 2 (“Social”) were significantly younger than those who were at home, alone, and cigarettes were easily available (Class 3; p = .001). There was also a significant difference in WISDM Social/Environmental Goads scores among the latent classes (F(4, 549) = 6.26, p < .001), with significantly higher Goads scores in Class 5 (“With Spouse Smoking”) and Class 2 (“Social”) compared with Class 3 (“Alone”; ps < .01).
DISCUSSION
The findings with respect to contextual features of lapse events are consistent with those reported earlier—lapses tend to occur in contexts associated with negative affect, being alone, drinking any beverage, and having cigarettes readily available (Brandon, Tiffany, Obremski, & Baker, 1990; Mermelstein & Lichtenstein, 1983; Shiffman et al., 1996c). Importantly, some of these contextual features were associated with greater likelihood of progression to relapse; greater relapse likelihood was associated with negative affect and when not drinking various beverages (Ferguson & Shiffman, 2010; Mermelstein & Lichtenstein, 1983; Shiffman et al., 1996b, 2007).
The person-centered LCAs, which show how groups of contextual features tend to cohere around lapse events, provided additional insight into lapse contexts. For instance, the most common lapse context (Class 3) was characterized by smoking at home, alone when cigarettes are easily available. Such lapsers are somewhat older and have fewer social or environmental goads for smoking. “Social” lapsers (Class 2), a large class of smokers who lapse while talking and drinking with friends out at a bar or restaurant, tend to be younger and report more smokers in their environment than other classes. Interestingly, they were also less likely to be smoking at 6 months postquit, compared with other latent classes, and had the longest latency to lapse and to relapse. Progressing to a full relapse was also less likely if the smoker was talking with a friend, angry, and cigarettes were readily available at the time of the initial lapse (Class 1).
These results seem to suggest that: (a) it is relatively less dangerous to lapse with a friend or in a social situation than when alone or with a spouse; (b) it is much more dangerous to lapse at home or in one’s car than in a different, presumably less familiar, context (see Table 2); and (c) it is fairly dangerous to lapse when no one else is smoking. From these findings, one could surmise that it is best to lapse in unusual circumstances, based on the assumption that being with one’s spouse, being at home or in one’s car, and/or being alone, are probably high base-rate occurrences. Therefore, if one lapses in such circumstances, it may be predictive of more smoking down the road since these lapse-provoking contexts will occur with high frequency. Because previous research has focused on identifying lapse context features that are especially related to relapse (features that occur much more frequently with lapses than in daily life in general; Shiffman et al., 1996a), the field may have underestimated the role of some high base-rate contextual features that are commonly encountered and that accompany the majority of lapses (e.g., being alone and at home: see Limitations section). If relapse provocation reflects both the motivational impact of a stimulus and the likelihood of future encounters, then a context feature with modest motivational impact could account for numerous relapses if it is ubiquitous.
There are suggestions, though, that some contextual features may be especially linked with lapse—beyond their rate of occurrence. For instance, lapsing when one is angry, with a spouse who is not smoking, and cigarettes are not readily available (i.e., Class 4), seems like a rare but very risky combination of contextual features. However, this may have less to do with such features magnifying the effects of smoking but rather may reflect the force of motivation that leads to smoking despite a lack of environmental affordances that would promote it. In other words, some contextual factors may illustrate instances where motivation to lapse is extremely high. It is this high level of motivation that likely leads to a high risk of later relapse.
Based on this interpretation, we should perhaps focus skill training less on rare, dramatic events and more on prosaic but common events or contextual features. Interventions such as exposure/extinction therapy or coping training might be focused on the most common contexts in a person’s life, including the pervasive availability of cigarettes. From a research perspective, perhaps we should attempt to construct a taxonomy of lapse and relapse risk factors that more consistently reflect the contribution of encounter rate. The data on the rate of occurrence of the lapse classes (see Table 2) suggest that the classes that are least likely to be associated with relapse progression (Classes 1 & 2) are also relatively common classes. A proper calculation of risk would demand a synthesis of information on frequency of encounter of the contextual feature and its motivational force.
This research was done with a fairly modern sample and some of the effects we observed suggest changes in lapse contexts that reflect secular changes. Unlike Ferguson and Shiffman (2010), we found that talking was the most common activity during a lapse, not working, which was the fifth most common response. This may be related to an increase in smoking restrictions in workplaces and in the home. We also found that person factors, such as age and the number of smokers in the environment, influenced lapse context and subsequent relapse. Therefore, clinicians may need to assess prequit factors that could identify risk situations: a younger smoker who frequently spends time with other smokers may be at greater risk in social situations rather than when s/he is alone.
It should be noted that, among those who established initial abstinence within the first week of the quit attempt, lapsing within the first 8 weeks of a quit attempt was common (63%) and associated with a greater risk of relapsing by 6 months. Approximately 78% of smokers who lapsed within the first 8 weeks were smoking by 6 months postquit. This research is consistent with earlier data showing that 67% of smokers lapse after 35 days (Shiffman et al., 2006) and that 83%–97% of those who smoked in the first 2 weeks were smoking by 6 months postquit (Kenford et al., 1994).
It is important to acknowledge the limitations of the current research. First, these reports were retrospective. While these reports occurred within, at most, 8 weeks of the relapse, this assessment is more susceptible to memory biases than reports based on real-time data. Second, given the nature of the assessment plan, we were not able to separate out baseline patterns of context exposure from patterns that characterized lapse events. Therefore, the data indicate the contexts in which individuals reported lapses, but did not highlight contexts that were especially associated with lapses; that is, the contextual feature with lapse association did not control for time spent in the presence of the contextual feature. While this limits certain inferences that can be drawn, we believe that it is important to determine the contexts of lapses—even if those contexts reflect habitual patterns of behavior or contextual exposure patterns. Third, while we assessed a wide array of context variables, we did not assess all possible contexts and we may have missed key constructs linked to the lapse process (e.g., “Drinking” included drinking any beverage, which limits our ability to make inferences about the influence of alcohol on lapse risk). In addition, we did not sample symptomatic changes or situational self-efficacy surrounding the lapse events, and thus we are no doubt reporting underspecified models. Fourth, while this was based on a large clinical trial and our sample size was more than double that of previous lapse research (Ns = 108, 214; Shiffman et al., 1996c, 2007), we still had limited power to detect significant differences in the various latent classes, which were quite small (e.g., Class 4: n = 37). Finally, participants were all highly motivated to quit and participated in intensive smoking cessation treatment that included individual counseling and pharmacotherapy. Therefore, these results may not generalize to all smokers trying to quit, especially those who try to quit without support.
The goal of this research was to contribute to the understanding of current lapse contexts and thereby identify potential relapse mechanisms and possible treatment targets. We were able to identify five latent classes of lapse contexts that are differentially related to relapse risk and specific individual differences. These data suggest that it may be possible to use baseline information to predict situations that might place particular groups of smokers at risk for an early lapse. In sum, this research, while exploratory and in need of replication, is consistent with previous research in many respects and offers some interesting insight into potential areas for targeted behavioral interventions.
SUPPLEMENTARY MATERIAL
Supplementary Table 1 can be found online at http://www.ntr.oxfordjournals.org
FUNDING
This research was conducted at the University of Wisconsin, Madison and was supported by grants P50 DA019706 and P50-DA010075-16 from National Institutes of Health/National Institute on Drug Abuse and by grant M01 RR03186 from the General Clinical Research Centers Program of the National Center for Research Resources, National Institutes of Health and by the Wisconsin Partnership Program. Drs. Piper and Lanza were supported via National Cancer Institute (1R01CA168676). Dr. Baker was supported via National Cancer Institute (1K05CA139871). The funders had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. Medication was provided to patients at no cost under a research agreement with GlaxoSmithKline (GSK); GSK had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
DECLARATION OF INTERESTS
None declared.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Nicole Butera for her assistance with the latent class analyses and Stevens S. Smith for his consultations.
REFERENCES
- Akaike H. (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19, 716–723 [Google Scholar]
- Benjamini Y., Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B, 57, 289–300.10.2307/2346101 [Google Scholar]
- Bliss R. E., Garvey A. J., Heinold J. W., Hitchcock J. L. (1989). The influence of situation and coping on relapse crisis outcomes after smoking cessation. Journal of Consulting and Clinical Psychology, 57, 443–449.10.1037/0022-006X.57.3.443 [DOI] [PubMed] [Google Scholar]
- Brandon T. H., Tiffany S. T., Obremski K. M., Baker T. B. (1990). Post cessation cigarette use: The process of relapse. Addictive Behaviors, 15, 105–114.10.1016/0306-4603(90)90013-N [DOI] [PubMed] [Google Scholar]
- Chen X., Li X., Stanton B., Mao R., Sun Z., Zhang H., … Thomas R. (2004). Patterns of cigarette smoking among students from 19 colleges and universities in Jiangsu Province, China: A latent class analysis. Drug and Alcohol Dependence, 76, 153–163.10.1016/j.drugalcdep.2004.04.013 [DOI] [PubMed] [Google Scholar]
- Collins L. M., Lanza S. T. (2010). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. New York, NY: Wiley; [Google Scholar]
- de Wit H., Stewart J. (1981). Reinstatement of cocaine-reinforced responding in the rat. Psychopharmacology, 75, 134–143 [DOI] [PubMed] [Google Scholar]
- Ferguson S. G., Shiffman S. (2010). Effect of high-dose nicotine patch on the characteristics of lapse episodes. Health Psychology, 29, 358–366.10.1037/a0019367 [DOI] [PubMed] [Google Scholar]
- Fiore M. C., Jaén C. R., Baker T. B., Bailey W. C., Benowitz N. L., Curry S. J., … Wewers M. E. (2008). Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services; [Google Scholar]
- Gwaltney C. J., Shiffman S., Balabanis M. H., Paty J. A. (2005). Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. Journal of Abnormal Psychology, 114, 661–675.10.1037/0021-843X.114.4.661 [DOI] [PubMed] [Google Scholar]
- Gwaltney C. J., Shiffman S., Norman G. J., Paty J. A., Kassel J. D., Gnys M., … Balabanis M. (2001). Does smoking abstinence self-efficacy vary across situations? Identifying context-specificity within the Relapse Situation Efficacy Questionnaire. Journal of Consulting and Clinical Psychology, 69, 516–527.10.1037/0022-006X.69.3.516 [PubMed] [Google Scholar]
- Hajek P., Stead L. F., West R., Jarvis M., Lancaster T. (2009). Relapse prevention interventions for smoking cessation. Cochrane Database of Systematic Reviews, (1), CD003999.10.1002/14651858.CD003999.pub3 [DOI] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K. (1991). The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction, 86, 1119–1127.10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- Henry K. L., Muthen B. (2010). Multilevel latent class analysis: An application of adolescent smoking typologies with individual and contextual predictors. Structural Equation Modeling, 17, 193–215.10.1080/10705511003659342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Callas P. W. (2010). Data to assess the generalizability of samples from studies of adult smokers. Nicotine & Tobacco Research, 12, 73–76.10.1093/ntr/ntp168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japuntich S. J., Leventhal A. M., Piper M. E., Bolt D. M., Roberts L. J., Fiore M. C., Baker T. B. (2011a). Smoker characteristics and smoking-cessation milestones. American Journal of Preventive Medicine, 40, 286–294.10.1016/ j.amepre.2010.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japuntich S. J., Piper M. E., Leventhal A. M., Bolt D. M., Baker T. B. (2011b). The effect of five smoking cessation pharmacotherapies on smoking cessation milestones. Journal of Consulting and Clinical Psychology, 79, 34–42.10.1037/a0022154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenford S. L., Fiore M. C., Jorenby D. E., Smith S. S., Wetter D., Baker T. B. (1994). Predicting smoking cessation: Who will quit with and without the nicotine patch. Journal of the American Medical Association, 271, 589–594.10.1001/jama.1994.03510320029025 [DOI] [PubMed] [Google Scholar]
- Keselman H. J., Cribbie R., Holland B. (2002). Controlling the rate of type I error over a large set of statistical tests. British Journal of Mathematical and Statistical Psychology, 55, 27–40.10.1348/000711002159680 [DOI] [PubMed] [Google Scholar]
- Kirchner T. R., Shiffman S., Wileyto E. P. (2012). Relapse dynamics during smoking cessation: Recurrent abstinence violation effects and lapse-relapse progression. Journal of Abnormal Psychology, 121, 187–197.10.1037/a0024451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S. T., Collins L. M., Lemmon D. R., Schafer J. L. (2007). PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling, 14, 671–694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S. T., Dziak J. J., Huang L., Xu S., Collins L. M. (2011). PROC LCA & PROC LTA users’ guide ( version 1.2.7) University Park: The Methodology Center, Pennsylvania State University; Retrieved from http://methodology.psu.edu [Google Scholar]
- Mermelstein R., Lichtenstein E. (1983, April). Slips vs. relapses in smoking cessation: A situational analysis and coping strategies. Paper presented at the Annual Meeting of the Western Psychological Association, San Francisco, CA [Google Scholar]
- O’Connell K. A., Martin E. J. (1987). Highly tempting situations associated with abstinence, temporary lapse, and relapse among participants in smoking cessation programs. Journal of Consulting and Clinical Psychology, 55, 367–371.10.1037/0022-006X.55.3.367 [DOI] [PubMed] [Google Scholar]
- Piasecki T. M. (2006). Relapse to smoking. Clinical Psychology Review, 26, 196–215.10.1016/j.cpr.2005.11.007 [DOI] [PubMed] [Google Scholar]
- Piper M. E., Piasecki T. M., Federman E. B., Bolt D. M., Smith S. S., Fiore M. C., Baker T. B. (2004). A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68). Journal of Consulting and Clinical Psychology, 72, 139–154.10.1037/0022-006X.72.2.139 [DOI] [PubMed] [Google Scholar]
- Piper M. E., Smith S. S., Schlam T. R., Fiore M. C., Jorenby D. E., Fraser D., Baker T. B. (2009). A randomized placebo-controlled clinical trial of 5 smoking cessation pharmacotherapies. Archives of General Psychiatry, 66, 1253–1262.10.1001/archgenpsychiatry.2009.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plies J. R., Ward B. W., Lucas J. W. (2010). Summary health statistics for U.S. adults: National Health Interview Survey, 2009 (DHHS Publication No. PHS 2011-1577). National Center for Health Statistics. Vital Health Stat 10(249) Retrieved from http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf [PubMed] [Google Scholar]
- Schwarz G. (1978). Estimating the dimension of a model. Annals of Statistics, 6, 461–464 [Google Scholar]
- Shiffman S. (1986). A cluster-analytic classification of smoking relapse episodes. Addictive Behaviors, 11, 295–307.10.1016/0306-4603(86)90057-2 [DOI] [PubMed] [Google Scholar]
- Shiffman S. (2005). Dynamic influences on smoking relapse process. Journal of Personality, 73, 1715–1748.10.1111/j.0022-3506.2005.00364.x [DOI] [PubMed] [Google Scholar]
- Shiffman S., Balabanis M. H., Gwaltney C. J., Paty J. A., Gnys M., Kassel J. D., … Paton S. M. (2007). Prediction of lapse from associations between smoking and situational antecedents assessed by ecological momentary assessment. Drug and Alcohol Dependence, 91, 159–168.10.1016/j.drugalcdep.2007.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Gnys M., Richards T. J., Paty J. A., Hickcox M., Kassel J. D. (1996a). Temptations to smoke after quitting: A comparison of lapsers and maintainers. Health Psychology, 15, 455–461.10.1037/0278-6133.15.6.455 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Hickcox M., Paty J. A., Gnys M., Kassel J. D., Richards T. J. (1996b). Progression from a smoking lapse to relapse: Prediction from abstinence violation effects, nicotine dependence, and lapse characteristics. Journal of Consulting and Clinical Psychology, 64, 993–1002.10.1037/0022-006X.64.5.993 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Hickcox M., Paty J. A., Gnys M., Richards T., Kassel J. D. (1997). Individual differences in the context of smoking lapse episodes. Addictive Behaviors, 22, 797–811.10.1016/S0306-4603(97)00063-4 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Paty J. A., Gnys M., Kassel J. A., Hickcox M. (1996c). First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology, 64, 366–379.10.1037/0022-006X.64.2.366 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Scharf D. M., Shadel W. G., Gwaltney C. J., Dang Q., Paton S. M., Clark D. B. (2006). Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult smokers. Journal of Consulting and Clinical Psychology, 74, 276–285.10.1037/0022-006X.74.2.276 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.