Abstract
Background
Identification of risk factors is critical to preventing the childhood obesity epidemic. Risk factors that contribute to obesity are multifactorial. However, limited research has focused on identifying obesity risk factors using an ecological approach.
Methods
Baseline self-report survey data from the STRONG Kids program were used. The sample consisted of 329 parent-child dyads recruited from childcare programs in east-central Illinois. Child height and weight were measured and converted to age- and sex-specific z-scores using standard growth charts. An ecological model provided the theoretical framework for the selection of 22 previously reported childhood obesity risk factors. Multiple logistic regression analyses were used to identify risk factors.
Results
Of 22 potential risk factors, three were found to be significantly associated with child overweight/obesity. These included child nighttime sleep duration (χ2=8.56; p=0.003), parent BMI (χ2=5.62; p=0.01), and parental restrictive feeding for weight control (χ2=4.77; p=0.02). Children who slept for 8 hours and less were 2.2 times more likely to be overweight/obese [95% confidence interval (CI): 1.3–3.7), whereas children with an overweight/obese parent were 1.9 times more likely to be overweight/obese (95% CI: 1.12–3.2). Finally, children whose parents used restrictive feeding practices were 1.75 times more likely to be overweight/obese (95% CI: 1.06–2.9).
Conclusions
Using an ecological approach, we conclude that childhood obesity prevention efforts may benefit from targeting the key risk factors of child sleep duration, parent BMI, and parental restrictive feeding practices as focus areas for obesity prevention.
Introduction
In the United States, childhood obesity rates have tripled in the past decade, with more than one quarter of American children 2–5 years of age overweight.1 This obesity epidemic is fueled, in part, by excess childhood weight gain. Dramatic increases in childhood obesity foreshadows serious health consequences (e.g., early risk for much of adult morbidity and mortality2 and premature death,3,4 type 2 diabetes,5,6 hypertension and -lipidemia,7,8 cardiovascular disease,8–11 asthma and sleep apnea,12,13 lower self-esteem,14 and psychological and social stress.15,16 Overweight/obesity tracks from childhood into adulthood and is difficult to treat successfully in the long term.17 Therefore, the Institute of Medicine recommends that prevention is crucial to combat the childhood obesity epidemic.18
Although effective action to prevent the childhood obesity epidemic requires an evidence base of early-life risk factors, unfortunately, this evidence base is still very incomplete.19,20 Despite the increasing prevalence of obesity in preschool children, researchers have focused on risk factors in school-age children and adolescents.17,21 Existing prevention strategies, focused on late childhood and adolescence, are largely unsuccessful because eating behaviors are already established by school age.22 Further, few studies have tried to capture the complete picture of childhood obesity risk factors. Most studies have included fewer predictors of overweight, such as parental obesity,23,24 breastfeeding duration,25 childhood television use,26,27 diet,25,28 and nighttime sleep duration.29 However, these risk factors often do not occur in isolation. It is well accepted that there is no single cause of childhood obesity, but coactions at multiple levels (e.g., genetic, cellular, physiological, psychological, social, and cultural) determine outcomes.30
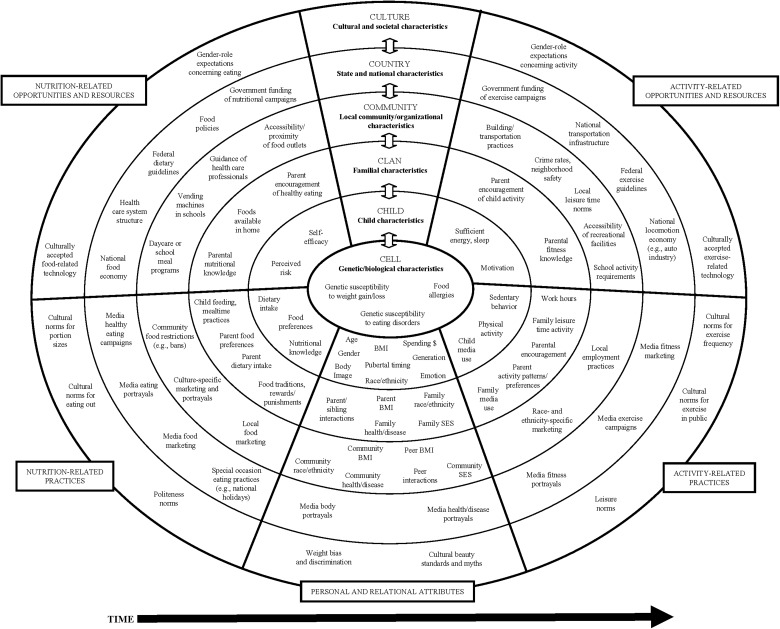
The current study fills the gap in the current literature by identifying early determinants of childhood overweight/obesity in preschool-aged children based on the Six-Cs31 ecological model as a theoretical framework for this study (Figure 1). The Six-Cs model identifies five spheres of environmental influence (child, clan, community, country, and culture) and one of genetic influence (cell) as being important determinants of childhood weight status.31 The Six-Cs model illustrates that a child's weight status is influenced by the intake and expenditure patterns of the child, but these patterns are embedded within the larger ecology of the child's family, community, and demographic characteristics.31
Figure 1.
The Six-Cs developmental ecological model of contributors to overweight and obesity in childhood.31 Reproduced with permission from John Wiley & Sons, Inc.
Using the Six-Cs ecological framework as a guiding principle for the selection of potential risk factors, we tested the hypothesis that child overweight/obesity will be associated with 22 previously reported potential risk factors, including child ethnicity,32 gender,33 nighttime sleep duration,34 time spent at home watching television (TV) per day,35 TV in view where family eats most meals,36 TV in bedroom,35 breastfeeding duration,25 family status (single parent vs. two parents),37 maternal education,38 parent BMI,39 family history of overweight/obesity,39 parent nutrition-label knowledge,40 participation in Women, Infants, and Children (WIC) supplemental assistance program,41 age of attendance in childcare,42,43 childcare nutrition policies,44,45 child's diet intake,46–51 fat content of milk,52,53 sugar, corn syrup, or honey added to baby's formula before 1 year of age,54 perceived dietary quality,55 neighborhood social cohesion,56 physical activity opportunities,57 and parental feeding practices.58,59 The aim of this study was to assess the influences of each of these previously reported potential risk factors on child overweight/obesity and to determine whether any of these risk factors would stand out as clear starting points for targeting key risk factors in future childhood obesity prevention programs.
Methods
Participants
The current study used data from the ongoing Synergistic Theory and Research on Obesity and Nutrition Group (STRONG) Kids (SK) longitudinal study of preschool children recruited at age 2 from Head Start programs and licensed childcare centers in four small urban communities in east-central Illinois. The initial wave of SK centers was recruited from a sample with unequal probability of selection among licensed preschools in a four-county diverse geographic area in the Midwest that met the following inclusion criteria: (1) Head Start program operating within the grantee agency providing Head Start services in the target communities, or childcare center licensed by the Illinois Department of Children and Family Services; (2) located within 65 miles of the study center in one of four small urban areas targeted to maximize racial/ethnic diversity; and (3) enrolled a minimum of 24 children in the targeted age range of 2–5 years to recruit into the study. These criteria identified 38 eligible preschools, 36 of which agreed to participate (94% school response rate) in the larger STRONG Kids study. Parents gave informed written consent for their children to participate. All procedures in this study protocol were approved by the University of Illinois at Urbana-Champaign Institutional Review Board (Urbana, IL). Data were collected from self-administered questionnaires with validated scales completed by the child's parent/primary caregiver. Height and weight were collected from 407 children at their respective childcare centers.
Of 407 children in our sample, we excluded 10 (2%) children because they were underweight. Sixty-eight children from some ethnic groups were excluded because of small sample size (i.e., Hispanic, 22; American Indian, 6; Hawaiian Native or Pacific Islander, 2; Asian, 38) to limit the underestimation of the effect of some risk factors prevalent in these groups. This resulted in a total sample of 329 preschool children, with 103 black and 226 white children for use in the analyses. We created a binary-dependent variable—BMI-for-age for preschool children—healthy weight (BMI-for-age 5th and <85th percentile) and overweight/obese (≥85th percentile).
Procedures and Measures
Independent variables: potential risk factors
We chose putative risk factors on the basis of previously reported associations with overweight/obesity or plausible earlier hypotheses using the Six-Cs ecological model as the theoretical framework. We cross-checked the results of our literature search against systematic reviews.60,61 Overall, we identified 27 potential risk factors. Measures for 22 of the 27 potential risk factors were available from baseline data on SK Wave 1 cohort. Forty-one variables of these 22 potential determinants were used in the regression model because some constructs were based on multiple indicators (Table 1).
Table 1.
Distribution of Potential Childhood Overweight/Obesity Risk Factors Stratified by Preschool BMI (n=329)
| |
|
Children's BMI status (%) |
|
|---|---|---|---|
| Potential risk factor | Level in Six-Cs model | Normal | Overweight/obese |
| Child ethnicity32 | Cell | ||
| NH black | 30.7 | 33.0 | |
| NH white | 69.3 | 67.0 | |
| Child gender33 | Child | ||
| Male | 53.5 | 52.3 | |
| Female | 46.5 | 47.7 | |
| Nighttime child sleep duration34 | Child | ||
| 9 and more hours | 76.3 | 56.8 | |
| 8 hours and less | 23.7 | 43.2 | |
| Time spent at home watch TV/day35 | Clan | ||
| <2 hours per day | 83.0 | 75.0 | |
| >2 hours per day | 17.0 | 25.0 | |
| TV in view where family eats most of meals35,36 | Clan | ||
| No | 56.4 | 55.7 | |
| Yes | 43.6 | 44.3 | |
| TV in bedroom35 | Clan | ||
| No | 33.2 | 27.3 | |
| Yes | 66.8 | 72.7 | |
| Breastfeeding duration25 | Clan | ||
| Never breastfed | 31.5 | 27.3 | |
| Breastfed less than 6 months | 33.6 | 40.9 | |
| Breastfed 6 months and more | 34.9 | 31.8 | |
| Family status37 | Clan | ||
| Single parent family (single, separated, divorced, widowed) | 28.6 | 40.9 | |
| Two-parent family (married, cohabiting, civil union) | 71.4 | 59.1 | |
| Maternal education38 | Clan | ||
| None, grade school, high school | 12 | 19.3 | |
| Some college, technical school | 32.8 | 38.6 | |
| College graduate, postgraduate | 55.2 | 42.0 | |
| Parent BMI39 | Clan | ||
| Normal: 18.5–24.9 kg/m2 | 48.5 | 31.8 | |
| Overweight and obese: >25 kg/m2 | 51.5 | 68.2 | |
| Family history of overweight or obesity39 | Clan | ||
| No | 70.5 | 60.2 | |
| Yes | 29.5 | 39.8 | |
| Parent nutrition-label knowledge40 | Clan | ||
| Inadequate | 12.4 | 15.9 | |
| Medium | 29.0 | 28.4 | |
| Adequate | 58.5 | 55.7 | |
| Participation in WIC41 | Community | ||
| No | 62.7 | 52.3 | |
| Yes | 37.3 | 47.7 | |
| Age of attendance in child care42,43 | Country | ||
| < 9 months | 59.8 | 53.4 | |
| ≥9 months | 40.2 | 46.6 | |
| Child care nutrition policies44,45 | Country | ||
| Non-CACFP | 33.6 | 33.0 | |
| CACFP | 54.4 | 51.1 | |
| Head Start | 12.0 | 15.9 | |
| Child diet intake, mean (SD) | Child | ||
| Milk/day52,53 | 2.41 (1.02) | 2.6 (1.01) | |
| Sugar beverages/day46,47 | 0.42 (0.77) | 0.61 (0.99) | |
| 100% juice/day48 | 1.3 (0.99) | 1.41 (1.09) | |
| Fresh fruits/day49 | 1.66 (0.86) | 1.72 (0.95) | |
| French fries/day50 | 0.36 (0.46) | 0.32 (31) | |
| Vegetables/day49 | 1.38 (0.82) | 1.48 (0.91) | |
| Fast foods/day51 | 0.25 (0.32) | 0.25 (0.19) | |
| Candy sweets/day50 | 0.71 (0.61) | 0.70 (0.57) | |
| Salty snacks/day50 | 0.55 (0.53) | 0.46 (0.44) | |
| Fat content of milk52,53 | Child | ||
| 1% or skim | 20.3 | 21.6 | |
| 2% or low fat | 65.1 | 67.0 | |
| Whole milk and flavored cow milk | 14.5 | 11.4 | |
| Sugar, corn syrup, honey added to baby's formula prior to 1 year of age54 | Child | ||
| No | 96.3 | 93.2 | |
| Yes | 3.7 | 6.8 | |
| Perceived dietary quality55 | Clan | 4.62 (6.18) | 4.84 (6.29) |
| Neighborhood social cohesion56 | Community | 3.46 (0.79) | 3.34 (0.79) |
| Physical activity opportunities57 | Clan | 2.91 (0.73) | 2.95 (0.81) |
| Parental feeding practices,58,59 mean (SD) | Clan | ||
| Monitoring | 4.13 (0.91) | 4.09 (0.95) | |
| Environment | 3.78 (0.62) | 3.72 (0.66) | |
| Child control | 2.43 (0.62) | 2.35 (0.63) | |
| Emotional regulation | 1.46 (0.57) | 1.51 (0.66) | |
| Balance and variety | 4.26 (0.65) | 4.21 (0.74) | |
| Food as reward | 2.18 (0.84) | 2.07 (0.83) | |
| Involvement | 2.90 (0.94) | 3.00 (1.03) | |
| Modeling | 3.63 (0.89) | 3.63 (0.93) | |
| Pressure | 2.49 (0.77) | 2.44 (0.87) | |
| Restriction for health | 2.83 (0.89) | 2.84 (0.93) | |
| Restriction for weight control | 1.60 (0.48) | 1.74 (0.51) | |
| Teaching about nutrition | 3.32 (1.09) | 3.38 (1.07) | |
Superscripts represent references for potential risk factors of childhood overweight/obesity included in the model.
NH, non-Hispanic; WIC, Women, Infants, and Children; CACFP, Child and Adult Care Food Program.
Dependent variable: child BMI-for-age
Height and weight were measured by trained research staff following a protocol developed by the World Health Organization for measuring children ≥2 years of age.62 SK research assistants received intensive training on height and weight measurement for preschool children, until they achieved 90% agreement with the trainer.
Overweight and obesity definition
The dependent variable was BMI, converted to age- and sex-specific z-scores using the 2000 growth charts published by the CDC.63–65 Overweight is defined as greater or equal to the 85th percentile, whereas obese is defined as greater or equal to the 95th percentile in accord with CDC guidelines.64 Several expert and advisory groups have recommended BMI as the preferred measure for evaluating overweight/obesity among children and adolescents 2–19 years of age.66–68
Statistical Analysis
Descriptive statistics [mean, standard deviation (SD), and frequencies] were calculated for all variables. Missing values for 41 risk variables used in the final model ranged from 3 to 10.4%. We examined missingness by using Little's missing completely at random (MCAR) test and determined that the values were not MCAR. We then used multiple imputation to analyze patterns of missing values, and the pattern chart revealed monotonicity in the data. Therefore, we used a multiple imputation with logistic regression model to impute less than 10% of the data. The imputed data were used for further analysis. Before running the regression model, data-screening procedures were performed to identify outliers, test for normality, and correlations between risk variables. Variance inflation factors were used to check for multicollinearity.69,70 This procedure indicated that no serious multicollinearity problems existed among the independent variables. We calculated internal consistency statistics (Cronbach's alpha) for measures such as parental feeding practices. Proposed risk factors were entered into the final model, in which all variables were analyzed simultaneously using multiple logistic regression using stepwise regression with forward selection. We used binary logistic regression because our dependent variable (child weight status) was dichotomous (i.e., healthy weight vs. overweight/obese). Statistical analyses were performed using the Statistical Package for the Social Sciences (Version 17; SPSS, Inc., Chicago, IL) and the Statistical Analysis System statistical software (Version 9.3; SAS Institute Inc., Cary, NC).
Results
Two hundred forty-one children (73.3%) were healthy weight, whereas 88 (26.7%) were overweight/obese (i.e., 17.6% overweight and 9.1% obese). We combined overweight and obese children, based on previous research suggesting that children who are overweight are at risk of becoming obese.60 There were no outliers, the final Cronbach's alpha for all survey measures was acceptable (≥0.65), and the potential risk variables included in the regression model were not significantly correlated. Distribution of the 22 potential risk factors categorized based on preschool BMI is shown in Table 1.
We entered the 22 risk factors (41 variables) into the regression model, where we analyzed all variables using multiple logistic regression. Of 22 risk factors, we found three to be significantly associated with child overweight/obesity (Table 2). These significant risk factors included child nighttime sleep duration (χ2=8.56; p=0.003), parent BMI (χ2=5.62; p=0.01), and parental feeding-practice restriction for weight control (χ2=4.77; p=0.02), where parents control the child's food intake with the purpose of decreasing or maintaining the child's weight.
Table 2.
Relationship between Risk Factors and Overweight/Obesity in Preschool Children (2–5 Years) Using Multiple Logistic Regression (n=329)
| Risk factor | β | SE | Wald's χ2 | p-value | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Nighttime child sleep duration | 0.7877 | 0.2692 | 8.5615 | 0.0034 | 2.198 | 1.297 | 3.726 |
| Parent BMI | 0.6399 | 0.2698 | 5.6262 | 0.0177 | 1.896 | 1.118 | 3.218 |
| Restriction for weight control | 0.5611 | 0.2567 | 4.7767 | 0.0288 | 1.753 | 1.060 | 2.899 |
OR, odds ratio; CI, confidence interval; SE, standard error.
These results suggest the risk for development of overweight/obesity in preschool-aged children who slept for 8 hours and less per night was approximately 2.2 times of that preschool-aged children who slept for 9 and more hours (odds ratio [OR], 2.2; 95% confidence interval [CI]: 1.3–3.7). Further, the risk for development of overweight/obesity in preschool children with an overweight/obese parent was approximately 1.9 times higher than preschool children of parents with normal BMI (OR, 1.9; 95% CI: 1.12–3.2). Finally, the risk for development of overweight/obesity in preschool children where parents use restrictive feeding practices for weight control was 1.75 times higher, as compared to parents not using controlling feeding practices (OR, 1.75; 95% CI: 1.06–2.9).
Discussion
Using an ecological model, we simultaneously considered a broad set of early-childhood risk factors for obesity, a key developmental period for prevention. We found that 3 (nighttime sleep duration, parental BMI, and parent feeding-practice restriction for weight control) of 22 putative early-childhood obesity risk factors were significantly associated with overweight/obesity. Because these factors were examined simultaneously, our results support using an ecological framework to identify risk factors, as compared to bivariate relationships, because risk factors do not occur in isolation. This study identifies specific influences in early life that might be suitable targets for childhood obesity prevention efforts.
Nighttime Sleep Duration
A positive association between nighttime sleep duration and overweight/obesity risk in preschool children was revealed. This result is consistent with current literature.29,34,71–76 A meta-analysis conducted to evaluate current evidence for the relationship between child sleep duration and overweight/obesity risk concluded that current studies from around the world show that short sleep duration is consistently associated with development of overweight/obesity in children and young adults, but not in older adults.29 In school-age children, several studies have consistently reported that short sleep duration was an independent risk factor for obesity,29,34,71 yet few studies have examined the relationship between short sleep duration and obesity in preschool children.
Drawing from a nationally representative sample of 2281 children 3–12 years of age, Snell and colleagues74 concluded sleeping less than 8 hours a night was correlated with higher BMI and being overweight at time 1 (baseline) and 2 (after 5.5 years), whereas sleeping between 10 and 11 hours a night was correlated with not being overweight at time 1 (baseline) and 2 (after 5.5 years).74 Therefore, for the purpose of our analyses, we defined “short sleep” as 8 hours or less. Although daytime napping is very common in preschool children, previous studies did not find an association between daytime sleep and obesity.72 Aforementioned evidence indicates that insufficient nighttime sleep among preschool-aged children may be a lasting risk factor for subsequent obesity.
Shortened sleep duration has been hypothesized to influence weight status through decreased physical activity as a result of tiredness and increased energy intake given greater opportunity to eat.29,71 Another pathway is through influence on the hypothalamic mechanisms that regulate body weight and metabolism by key hormones, such as leptin and ghrelin.77,78 Hunger and appetite increase with lower leptin levels and higher ghrelin levels, and both low leptin and high ghrelin levels have been linked to short sleep duration.77,78
Parent BMI
Confirming previous observations,79,80 a significant risk factor that emerged in this study was parental overweight/obesity. There is an extensive evidence base to support the relationship between parental obesity and childhood overweight. Parental obesity is also related to children's fat intake,81 snack food consumption,79 and a higher preference for high-fat foods and a lower preference for vegetables.23 Children of overweight parents are also less active82 and more likely to prefer sedentary activities23 than children of parents with normal weight. The family environment, including parental modeling of eating, can influence children's dietary behaviors.83 Children's dietary intake is also associated with parental diet.84 Therefore, the link between parent and child BMI identified in this study most certainly represents genetic, as well as environmental, influences on childhood overweight/obesity. Therefore, engaging parents in child- or family-focused prevention efforts is an effective strategy for childhood obesity prevention.
Restriction for Weight Control
Consistent with previous research, findings from the current study suggest parental feeding-practice restriction for weight control is a risk factor for overweight/obesity during the preschool years. This is concerning, given that previous research has shown that restrictive feeding practices have negative outcomes in the context of both child weight and child eating behaviors. In the context of child weight, Faith and colleagues in 2004 showed that higher restriction at age 5 years predicted higher BMI z-scores at age 7 years among low-risk children (defined as having a normal-weight mother).85 Likewise, Francis and Birch in 2005 reported higher child weight and adiposity was associated with higher use of restrictive feeding.80 High levels of control over children's food intake have been linked with subsequent disinhibited child eating86,87 and childhood overweight.88–90
In the context of child eating in children ages 3–5, Fisher and Birch demonstrated that children made more requests for, and more attempts to obtain, the restricted food than unrestricted food, whereas restricted access increased subsequent intake and greater increases in behavioral response to restricted food.86,87 However, most of this evidence comes from cross-sectional studies, and it is unclear whether parents are restrictive in response to children's unhealthy weight gain or whether restriction leads to unhealthy weight gain.
There are several strengths of this study (e.g., high effect size in primary findings and an ecological framework that acknowledges that obesity is a multifactorial disease) that provide valuable new insights into the determinants of early-childhood obesity. However, this study is not without limitations. Cross-sectional studies, such as the current investigation, are limited to identifying associations, rather than confirming causality. Risk factors, such as diet and physical activity, were assessed using self-reports that might be the reason for some nonsignificant findings. Other childhood obesity risk factors identified by previous studies, such as parity, smoking during pregnancy, and maternal BMI prepregnancy, could not be assessed because of unavailability of data. Future studies should focus on including these risk factors as well as identifying mediational and moderational processes. The current sample was recruited from advertisements given to parents using center-based child care for their preschool children, so generalization is limited. Finally, the current results can only be generalized to black and white ethnicities, because other ethnic minority groups in our sample were excluded because they were under-represented. Other studies would benefit from using an ecological approach to identify potential risk factors. Future interventions that focus on child sleep, parental feeding practices, and engaging parents, in addition to improving nutrition and increasing physical activity, might lead to desired results and long-term healthful behaviors for obesity prevention in children. Future larger longitudinal and observation studies should also focus on extending findings to ethnic minority groups as well as determining predictors of restrictive feeding practices and short sleep duration.
Conclusion
This study identifies three key early-life risk indicators for childhood overweight/obesity in preschool children (i.e., parent BMI, child nighttime sleep duration, and parental restrictive feeding), using an ecological approach with a simultaneous analysis of 22 risk factors that acknowledges that obesity is a multifactorial disease. Engaging and educating parents about the importance of sleep, and not using restrictive feeding practices, may add to the efficacy of childhood obesity prevention and intervention programs. Childhood obesity prevention efforts may benefit from targeting these key risk factors as focus areas for obesity prevention. Although excess weight gain is an outcome of an energy imbalance resulting from consumption of energy-dense foods and decreased physical activity, it is important to extend the overweight/obesity prevention efforts to engage parents in child- or family-focused obesity prevention efforts; establish sleep routines for children, and increase awareness about the negative effect of restrictive feeding practices. When parents are involved in childhood obesity prevention efforts, the shared familial characteristics in the environment, such as improved nutrition and increased physical activity, can help prevent excess weight gain in children. Similarly, shortened nighttime sleep duration in early life is a modifiable risk factor with important implications for overweight/obesity prevention. Increasing parental awareness of the importance of sleep and helping parents to establish an appropriate sleep schedule for young children may be useful in preventing childhood obesity. These three risk indicators can provide an effective starting point for childhood obesity prevention efforts that would allow for the optimal use of limited resources targeting young children. Future interventions might focus on environmental changes targeted in early childhood, which are independently related to the risk of overweight/obesity.
Acknowledgments
This research was funded, in part, by grants from the US Department of Health and Human Services (grant no.: 90YR0052) and the Illinois Transdisciplinary Obesity Prevention Program (I-TOPP) Seed Grant (to D.D. and B.M.). The larger STRONG Kids research initiative was funded, in part, by grants from the Illinois Council for Food and Agricultural Research (to K.H., principal investigator; PI) and the University of Illinois Health and Wellness Initiative and USDA [Hatch 793-328; to B.F. (PI) and S.D.] and the US Department of Agriculture (Hatch 793-328; to B.F., PI).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL. Carroll MD. Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biro FM. Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91:1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franks PW. Hanson RL. Knowler WC, et al. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reilly JJ. Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int J Obes (Lond) 2010;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 5.Goran MI. Ball GDC. Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab. 2003;88:1417–1427. doi: 10.1210/jc.2002-021442. [DOI] [PubMed] [Google Scholar]
- 6.van Vliet M. Van der Heyden JC. Diamant M, et al. Overweight is highly prevalent in children with type 1 diabetes and associates with cardiometabolic risk. J Pediatr. 2010;156:923–929. doi: 10.1016/j.jpeds.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Freedman DS. Serdula MK. Srinivasan SR, et al. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: The Bogalusa Heart Study. Am J Clin Nutr. 1999;69:308–317. doi: 10.1093/ajcn/69.2.308. [DOI] [PubMed] [Google Scholar]
- 8.Morrison JA. Sprecher DL. Barton BA, et al. Overweight, fat patterning, and cardiovascular disease risk factors in black and white girls: The National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 1999;135:458–464. doi: 10.1016/s0022-3476(99)70168-x. [DOI] [PubMed] [Google Scholar]
- 9.Steinberger J. Daniels SR. Obesity, insulin resistance, diabetes, and cardiovascular risk in children: An American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism) Circulation. 2003;107:1448–1453. doi: 10.1161/01.cir.0000060923.07573.f2. [DOI] [PubMed] [Google Scholar]
- 10.Freedman DS. Dietz WH. Srinivasan SR, et al. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 11.Bao W. Srinivasan SR. Wattigney WA, et al. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood: The Bogalusa Heart Study. Arch Intern Med. 1994;154:1842–1847. [PubMed] [Google Scholar]
- 12.Leung AK. Robson WL. Childhood obesity. Postgrad Med. 1990;87:123–130. doi: 10.1080/00325481.1990.11704600. , 133. [DOI] [PubMed] [Google Scholar]
- 13.Taveras EM. Camargo CA., Jr Rifas‐Shiman SL, et al. Association of birth weight with asthma‐related outcomes at age 2 years. Pediatr Pulmonol. 2006;41:643–648. doi: 10.1002/ppul.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.French SA. Story M. Perry CL. Self-esteem and obesity in children and adolescents: A literature review. Obes Res. 1995;3:479–490. doi: 10.1002/j.1550-8528.1995.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 15.Puhl RM. Latner JD. Stigma, obesity, and the health of the nation's children. Psychol Bull. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 16.Puhl RM. Heuer CA. The stigma of obesity: A review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 17.Gordon-Larsen P. Adair LS. Nelson MC, et al. Five-year obesity incidence in the transition period between adolescence and adulthood: The national longitudinal study of adolescent health. Am J Clin Nutr. 2004;80:569–575. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- 18.Koplan JP. Liverman CT. Kraak VI. Preventing Childhood Obesity: Health in the Balance. National Academies Press; Washington, DC: 2005. [PubMed] [Google Scholar]
- 19.Isganaitis E. Levitsky LL. Preventing childhood obesity: Can we do it? Curr Opin Endocrinol Diabetes Obes. 2008;15:1–8. doi: 10.1097/MED.0b013e3282f44a07. [DOI] [PubMed] [Google Scholar]
- 20.Koplan J. National Academies Press; Washington, DC: 2007. Progress in Preventing Childhood Obesity: How Do We Measure Up? [Google Scholar]
- 21.Lytle LA. Kubik MY. Perry C, et al. Influencing healthful food choices in school and home environments: Results from the TEENS study. Prev Med. 2006;43:8–13. doi: 10.1016/j.ypmed.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 22.Birch LL. Ventura AK. Preventing childhood obesity: What works? Int J Obes (Lond) 2009;33:S74–S81. doi: 10.1038/ijo.2009.22. [DOI] [PubMed] [Google Scholar]
- 23.Wardle J. Guthrie C. Sanderson S, et al. Food and activity preferences in children of lean and obese parents. Int J Obes Relat Metab Disord. 2001;25:971–977. doi: 10.1038/sj.ijo.0801661. [DOI] [PubMed] [Google Scholar]
- 24.Berkowitz RI. Stallings VA. Maislin G, et al. Growth of children at high risk of obesity during the first 6 y of life: Implications for prevention. Am J Clin Nutr. 2005;81:140–146. doi: 10.1093/ajcn/81.1.140. [DOI] [PubMed] [Google Scholar]
- 25.Harder T. Bergmann R. Kallischnigg G, et al. Duration of breastfeeding and risk of overweight: A meta-analysis. Am J Epidemiol. 2005;162:397–403. doi: 10.1093/aje/kwi222. [DOI] [PubMed] [Google Scholar]
- 26.Dennison BA. Erb TA. Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 27.Janz KF. Levy SM. Burns TL, et al. Fatness, physical activity, and television viewing in children during the adiposity rebound period: The Iowa Bone Development Study. Prev Med. 2002;35:563–571. doi: 10.1006/pmed.2002.1113. [DOI] [PubMed] [Google Scholar]
- 28.Welsh JA. Cogswell ME. Rogers S, et al. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics. 2005;115:e223–e229. doi: 10.1542/peds.2004-1148. [DOI] [PubMed] [Google Scholar]
- 29.Cappuccio FP. Taggart FM. Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Birch LL. Anzman SL. Learning to eat in an obesogenic environment: A developmental systems perspective on childhood obesity. Child Dev Perspect. 2010;4:138–143. [Google Scholar]
- 31.Harrison K. Bost KK. McBride BA, et al. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six‐Cs model. Child Dev Perspect. 2011;5:50–58. [Google Scholar]
- 32.Kumanyika S. Ethnicity and obesity development in children. Ann N Y Acad Sci. 1993;699:81–92. doi: 10.1111/j.1749-6632.1993.tb18839.x. [DOI] [PubMed] [Google Scholar]
- 33.Reilly JJ. Armstrong J. Dorosty AR, et al. Early life risk factors for obesity in childhood: Cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nielsen LS. Danielsen KV. Sørensen TIA. Short sleep duration as a possible cause of obesity: Critical analysis of the epidemiological evidence. Obes Rev. 2010;12:78–92. doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 35.Caroli M. Argentieri L. Cardone M, et al. Role of television in childhood obesity prevention. Int J Obes (Lond) 2004;28:S104–S108. doi: 10.1038/sj.ijo.0802802. [DOI] [PubMed] [Google Scholar]
- 36.Dubois L. Farmer A. Girard M, et al. Social factors and television use during meals and snacks is associated with higher BMI among pre-school children. Public Health Nutr. 2008;11:1267–1279. doi: 10.1017/S1368980008002887. [DOI] [PubMed] [Google Scholar]
- 37.Gerald LB. Anderson A. Johnson GD, et al. Social class, social support and obesity risk in children. Child Care Health Dev. 1994;20:145–163. doi: 10.1111/j.1365-2214.1994.tb00377.x. [DOI] [PubMed] [Google Scholar]
- 38.Lamerz A. Kuepper-Nybelen J. Wehle C, et al. Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. Int J Obes (Lond) 2005;29:373–380. doi: 10.1038/sj.ijo.0802914. [DOI] [PubMed] [Google Scholar]
- 39.Danielzik S. Czerwinski-Mast M. Langnäse K, et al. Parental overweight, socioeconomic status and high birth weight are the major determinants of overweight and obesity in 5–7 y-old children: Baseline data of the Kiel Obesity Prevention Study (KOPS) Int J Obes (Lond) 2004;28:1494–1502. doi: 10.1038/sj.ijo.0802756. [DOI] [PubMed] [Google Scholar]
- 40.Variyam JN. Overweight children: Is parental nutrition knowledge a factor? Food Rev. 2001;24:18–22. [Google Scholar]
- 41.Dinour LM. Bergen D. Yeh MC. The food insecurity-obesity paradox: A review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107:1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 42.Gubbels JS. Kremers SPJ. Stafleu A, et al. Child-care use and the association with body mass index and overweight in children from 7 months to 2 years of age. Int J Obes (Lond) 2010;34:1480–1486. doi: 10.1038/ijo.2010.100. [DOI] [PubMed] [Google Scholar]
- 43.Kim J. Peterson KE. Association of infant child care with infant feeding practices and weight gain among US infants. Arch Pediatr Adolesc Med. 2008;162:627–633. doi: 10.1001/archpedi.162.7.627. [DOI] [PubMed] [Google Scholar]
- 44.Dev DA. McBride BA. The STRONG Kids Research Team. Academy of Nutrition and Dietetics benchmarks for nutrition in child-care 2011: Are child-care providers across contexts meeting recommendations? J Acad Nutr Diet. 2013 Aug 2; doi: 10.1016/j.jand.2013.05.023. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 45.Frisvold DE. Lumeng JC. Expanding exposure: Can increasing the daily duration of Head Start reduce childhood obesity? J Hum Resour. 2011;46:373–402. [Google Scholar]
- 46.Malik VS. Schulze MB. Hu FB. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am J Clin Nutr. 2006;84:274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van der Horst K. Kremers S. Ferreira I, et al. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Educ Res. 2007;22:295–304. doi: 10.1093/her/cyl080. [DOI] [PubMed] [Google Scholar]
- 48.Dennison BA. Rockwell HL. Baker SL. Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity. Pediatrics. 1997;99:15–22. [PubMed] [Google Scholar]
- 49.Tohill BC. Dietary Intake of Fruit and Vegetables and Management of Body Weight. World Health Organization; Geneva: 2005. [Google Scholar]
- 50.Newby PK. Are dietary intakes and eating behaviors related to childhood obesity? A comprehensive review of the evidence. J Law Med Ethics. 2007;35:35–60. doi: 10.1111/j.1748-720X.2007.00112.x. [DOI] [PubMed] [Google Scholar]
- 51.Bowman SA. Gortmaker SL. Ebbeling CB, et al. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113:112–118. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 52.Berkey CS. Rockett HR. Willett WC, et al. Milk, dairy fat, dietary calcium, and weight gain: A longitudinal study of adolescents. Arch Pediatr Adolesc Med. 2005;159:543–550. doi: 10.1001/archpedi.159.6.543. [DOI] [PubMed] [Google Scholar]
- 53.Mace K. Shahkhalili Y. Aprikian O, et al. Dietary fat and fat types as early determinants of childhood obesity: A reappraisal. Int J Obes (Lond) 2006;30:S50–S57. doi: 10.1038/sj.ijo.0803519. [DOI] [PubMed] [Google Scholar]
- 54.Popkin BM. Gordon-Larsen P. The nutrition transition: Worldwide obesity dynamics and their determinants. Int J Obes (Lond) 2004;28:S2–S9. doi: 10.1038/sj.ijo.0802804. [DOI] [PubMed] [Google Scholar]
- 55.York-Crowe EE. White MA. Paeratakul S, et al. The diet and health knowledge survey: Development of a short interview format. Eating Behav. 2006;7:235–242. doi: 10.1016/j.eatbeh.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 56.Gundersen C. Mahatmya D. Garasky S, et al. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12:e54–e63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- 57.Steinbeck KS. The importance of physical activity in the prevention of overweight and obesity in childhood: A review and an opinion. Obes Rev. 2001;2:117–130. doi: 10.1046/j.1467-789x.2001.00033.x. [DOI] [PubMed] [Google Scholar]
- 58.Johannsen DL. Johannsen NM. Specker BL. Influence of parents' eating behaviors and child feeding practices on children's weight status. Obesity (Silver Spring) 2012;14:431–439. doi: 10.1038/oby.2006.57. [DOI] [PubMed] [Google Scholar]
- 59.Cachelin FM. Thompson D. Predictors of maternal child‐feeding practices in an ethnically diverse sample and the relationship to child obesity. Obesity (Silver Spring) 2013 Mar 21; doi: 10.1002/oby.20385. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 60.Hawkins SS. Law C. A review of risk factors for overweight in preschool children: A policy perspective. Int J Pediatr Obes. 2006;1:195–209. doi: 10.1080/17477160600943351. [DOI] [PubMed] [Google Scholar]
- 61.Van der Horst K. Oenema A. Ferreira I, et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ Res. 2007;22:203–226. doi: 10.1093/her/cyl069. [DOI] [PubMed] [Google Scholar]
- 62.World Health Organization. Training Course on Child Growth Assessment. World Health Organization; Geneva: 2008. [Google Scholar]
- 63.Ogden CL. Kuczmarski RJ. Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 64.Kuczmarski RJ. Flegal KM. Criteria for definition of overweight in transition: Background and recommendations for the United States. Am J Clin Nutr. 2000;72:1074–1081. doi: 10.1093/ajcn/72.5.1074. [DOI] [PubMed] [Google Scholar]
- 65.Kuczmarski RJ. Ogden CL. Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;8:1–27. [PubMed] [Google Scholar]
- 66.Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 67.Koplan JP. Liverman CT. Kraak VI Committee on Prevention of Obesity in Children and Youth. Preventing childhood obesity: health in balance: Executive Summary. J Am Diet Assoc. 2005;105:131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 68.McCarthy A. Hughes R. Tilling K, et al. Birth weight; postnatal, infant, and childhood growth; and obesity in young adulthood: Evidence from the Barry Caerphilly Growth Study. Am J Clin Nutr. 2007;86:907–913. doi: 10.1093/ajcn/86.4.907. [DOI] [PubMed] [Google Scholar]
- 69.Liu R. Kuang J. Gong Q, et al. Principal component regression analysis with SPSS. Comput Methods Programs Biomed. 2003;71:141–147. doi: 10.1016/s0169-2607(02)00058-5. [DOI] [PubMed] [Google Scholar]
- 70.Schroeder MA. Lander J. Levine-Silverman S. Diagnosing and dealing with multicollinearity. West J Nurs Res. 1990;12:175–187. doi: 10.1177/019394599001200204. [DOI] [PubMed] [Google Scholar]
- 71.Bell JF. Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med. 2010;164:840–845. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 72.Jiang F. Zhu S. Yan C, et al. Sleep and obesity in preschool children. J Pediatr. 2009;154:814–818. doi: 10.1016/j.jpeds.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 73.Taveras EM. Rifas-Shiman SL. Oken E, et al. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305–311. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Snell EK. Adam EK. Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–323. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 75.Taheri S. The link between short sleep duration and obesity: We should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–884. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gangwisch JE. Malaspina D. Boden-Albala B, et al. Inadequate sleep as a risk factor for obesity: Analyses of the NHANES I. Sleep. 2005;28:1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 77.Spiegel K. Tasali E. Penev P, et al. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 78.Spiegel K. Leproult R. L'Hermite-Balériaux M, et al. Leptin levels are dependent on sleep duration: Relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–5771. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 79.Francis LA. Lee Y. Birch LL. Parental weight status and girls' television viewing, snacking, and body mass indexes. Obes Res. 2003;11:143–151. doi: 10.1038/oby.2003.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Francis LA. Birch LL. Maternal weight status modulates the effects of restriction on daughters' eating and weight. Int J Obes (Lond) 2005;29:942–949. doi: 10.1038/sj.ijo.0802935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nguyen VT. Larson DE. Johnson RK, et al. Fat intake and adiposity in children of lean and obese parents. Am J Clin Nutr. 1996;63:507–513. doi: 10.1093/ajcn/63.4.507. [DOI] [PubMed] [Google Scholar]
- 82.Klesges RC. Eck LH. Hanson CL, et al. Effects of obesity, social interactions, and physical environment on physical activity in preschoolers. Health Psychol. 1990;9:435–449. doi: 10.1037//0278-6133.9.4.435. [DOI] [PubMed] [Google Scholar]
- 83.Campbell KJ. Crawford DA. Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. Int J Obes (Lond) 2006;30:1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- 84.Oliveria SA. Ellison RC. Moore LL, et al. Parent-child relationships in nutrient intake: The Framingham Children's Study. Am J Clin Nutr. 1992;56:593–598. doi: 10.1093/ajcn/56.3.593. [DOI] [PubMed] [Google Scholar]
- 85.Faith MS. Berkowitz RI. Stallings VA, et al. Parental feeding attitudes and styles and child body mass index: Prospective analysis of a gene-environment interaction. Pediatrics. 2004;114:e429–e436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- 86.Fisher JO. Birch LL. Restricting access to foods and children's eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- 87.Fisher JO. Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 88.Johnson SL. Krebs NF. Internal versus external influences on energy intake: Are disinhibited eaters born or created? J Pediatr. 2009;155:608–609. doi: 10.1016/j.jpeds.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 89.Shunk JA. Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc. 2004;104:1120–1126. doi: 10.1016/j.jada.2004.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Birch LL. Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48:893–907. doi: 10.1016/s0031-3955(05)70347-3. [DOI] [PubMed] [Google Scholar]