Abstract
Background
To elucidate the relationship between seven occupational dermatoses (ODs) and 20 types of work in Greece.
Methods
This was a prevalence epidemiologic study of certain ODs among 4,000 workers employed in 20 types of enterprise, in 104 companies, in 2006–2012, using data from company medical records, questionnaires, occupational medical, and special examinations. The χ2 test was applied to reveal statistically significant relationships between types of enterprises and occurrence of ODs.
Results
A high percentage (39.9%) of employees included in the study population suffered from ODs. The highest prevalence rates were noted among hairdressers (of contact dermatitis: 30%), cooks (of contact dermatitis: 29.5%), bitumen workers (of acne: 23.5%), car industry workers (of mechanical injury: 15%), construction workers (of contact urticaria: 29.5%), industrial cleaning workers (of chemical burns: 13%), and farmers (of malignant tumors: 5.5%). We observed several statistical significant correlations between ODs (acute and chronic contact dermatitis, urticaria, mechanical injury, acne, burns, skin cancer) and certain types of enterprises. There was no statistically significant correlation between gender and prevalence of ODs, except for dermatoses caused by mechanical injuries afflicting mainly men [χ2 (1) = 13.40, p < 0.001] and for chronic contact dermatitis [χ2 (1) = 5.53, p = 0.019] afflicting mainly women.
Conclusion
Prevalence of ODs is high in Greece, contrary to all official reports by the Greek National Institute of Health. There is a need to introduce a nationwide voluntary surveillance system for reporting ODs and to enhance skin protection measures at work.
Keywords: environmental health, occupational dermatoses, occupational epidemiology, occupational exposure, prevention and control
1. Introduction
The National Institute for Occupational Safety and Health has classified skin diseases as one of the most significant problems faced by workers in the USA [1]. Since 1982, skin diseases have been recognized as one of the top 10 diseases related to work based on the incidence and severity of the disease. Hazardous substances are largely responsible for 350 million working days lost due to poor occupational health and are also responsible for the appearance of occupational diseases in 7 million people [1].
Industrial dermatitis (21%) resulted in the absence from work with a median of 3 days away from work in Singapore [2]. Skin disease and asthma constitute the major part of occupational diseases in the member states of the European Union and result in long absences from work. The presence of skin diseases as a percentage of all occupational diseases is calculated at 7% [3]. Skin diseases are listed as the second most common occupational health problem in Europe [4]. The occurrence of occupational dermatoses has been reported in the United Kingdom (UK) to be the highest among health professionals and hairdressers and to impact heavily on the working lives of patients [5].
Occupational skin diseases affect workers of all ages in a wide variety of work settings. Industries in which workers are at highest risk include manufacturing, food production, construction, machine tool operation, printing, metal plating, leather work, engine service, and forestry [6,7]. History of illness and occupational history may reveal a close association between a skin condition and a specific work exposure known to produce skin effects [8].
The occurrence of occupational allergic contact dermatitis was reported to be 6% among laboratory workers due to the exposure to nickel [6], 70% among forestry workers due to the exposure to Rhus genus (e.g., poison oak) [9], and 10–17% among health service workers following an exposure to latex [10].
Kitchen staff may suffer from photoallergic dermatitis, which may continue long after the photoallergy is eliminated [11]. Common photoallergic substances include fruits, vegetables, and drugs [6,11].
Exposure to solvents and lubricants (oils and greases) and resultant mechanical blockage of pilosebaceous units can lead to “oil acne” [12,13]. Irritants or sensitizing agents in oils and greases can also cause contact dermatitis.
Skin tumors can result from an exposure to substances such as polycyclic hydrocarbons, inorganic metals, and arsenicals [6,14]. These lesions can also develop because of trauma, burns, and exposure to ultraviolet light or ionizing radiation [6,14]. Co-carcinogenesis, such as the interaction of sunlight and tar, is often implicated. Frequently, the skin tumors do not appear until two or three decades after the exposure [15].
Occupational contact dermatitis constitutes over 90% of the wider spectrum of occupational dermatoses, the other 10% includes contact urticaria, oil acne, chemical burns, and epidermal tumors [16]. Infectious skin diseases may cause illness to other employees, to customers, and contaminate products. Physical, biological, chemical, and mechanical factors are risk factors that cause occupational dermatoses. Skin diseases are common among cleaning workers, hairdressers, building, metal, and tanning industries, and food handlers [17].
In 1991, a pilot scheme, known as the OCC-DERM project, was initiated in Manchester, UK, by 17 consultants in dermatology who reported new cases of work-related skin diseases [18,19].
Skin disorders were reported in 33% of catering staff, in 35% of cleaners [20], and in 42% of construction workers [21]. Two cleaning workers, who suffered from burns caused by acids contained in bleach, were presented in a case study [22]. Skin photoaging was diagnosed in farmers occupationally exposed to ultraviolet radiation [23].
Skin diseases affect almost all industrial and business sectors and force many workers to change jobs [24]. Affected persons often experience severe impairment in their quality of life. Many adults afflicted by eczema believe that they have been subjected to discrimination at work, including being stared at and being excluded by colleagues. Employers may be inflexible about medical appointments and unsympathetic about the need of these patients to have time off work. In some cases, eczema can hinder chances at job interviews, limit career progression, and even restrict their choice of career. Patients suffering from eczema are more likely to avoid socializing or being touched by a partner during flare-ups, and may have an increased sense of isolation [25].
Diagnosis of occupational dermatoses requires cooperation between occupational physicians and workers. Recommendations for further investigations, management, and review are then made as appropriately. The main goal of diagnosis, treatment, and prevention of occupational dermatoses is to prevent them from becoming chronic. Prevention is of great importance because of their poor prognosis.
Recognizing the many repercussions of dermatoses, we initiated a surveillance project studying occupational dermatoses on a daily basis to obtain more specific information about cases of occupational skin diseases, in 104 companies in September 2006. Evaluation of all contact irritants (thermal, chemical, mechanical) and contact allergens (existing in the workplace, protective garments, barrier cream products) was carried out concurrently to investigate causal or contributory factors. We used data from this project for the present study, with the objective to elucidate the relationship between seven occupational skin diseases and 20 types of work in Greece.
2. Materials and methods
2.1. Study population and collection of data
We carried out a prevalence epidemiologic study. The data for this study were obtained by reviewing in house routine medical records by the use of a specially designed questionnaire administered to 4,000 full-time employees (200 white-collar and 3,800 blue-collar employees), who were employed in 104 small and medium size companies during the period 2006–2012. These firms included 20 different types of enterprise in various branches of economic activity (Table 1). We studied occupational dermatoses in bitumen laying workers, metal workers, carpenters, carbonated drinks bottling industry workers, detergent manufacturing industry workers, car repair shop workers, forestry workers, pesticide application workers, hairdressers, kitchen staff, plastic manufacturing industry workers, food industry workers, printers, footwear artisan factory workers, pharmaceutical industry workers, paint manufacturing industry workers, industrial cleaning workers, office workers, and construction workers. Our criterion for the selection of the aforementioned 20 types of enterprises was a high risk for occupational dermatoses indicated by international medical literature. Of the total, 2,550 were men and 1,450 were women. We initially gathered the company's medical files of all current and former employees. We then selected only current employees working in the aforementioned firms during the period 2006–2012, each of whom had worked in each type of enterprise for 5 years (no more, no less) and had never previously worked in a similar type of enterprise. This ensured that the period of exposure to any possible noxious agents was the same for each study participant, i.e., 5 years. Afterwards we defined a study population, i.e., a target population of 4,000, by randomly sampling 200 employees from each target population in each type of enterprise and examined their data. Original numbers of employees in each type of the 20 types of enterprise were different. In certain types of enterprise, the 200 employees worked in separate firms, e.g., hairdressers worked in several beauty salons. Distribution of study population by type of enterprise and number of firms is shown in Table 1.
Table 1.
Distribution of study population by type of enterprise and number of firms
| Type of enterprise | No. of firms | No. of employees |
Type of enterprise | No. of firms | No. of employees |
||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Males | Females | ||||
| Bitumen laying workers | 4 | 200 | 140 | 60 | Carpenters | 4 | 200 | 185 | 15 |
| Μetal industry workers | 2 | 200 | 190 | 10 | Carbonated drinks bottling industry workers | 2 | 200 | 115 | 85 |
| Pesticide application workers | 10 | 200 | 160 | 40 | Detergent industry workers | 4 | 200 | 105 | 95 |
| Hairdressers | 8 | 200 | 50 | 150 | Plastic manufacturing industry workers | 10 | 200 | 100 | 100 |
| Kitchen staff | 10 | 200 | 130 | 70 | Pharmaceutical industry workers | 2 | 200 | 110 | 90 |
| Industrial cleaning workers | 5 | 200 | 30 | 170 | Paint manufacturing industry workers | 1 | 200 | 140 | 60 |
| Office workers | 10 | 200 | 80 | 120 | Footwear artisan factory workers | 2 | 200 | 150 | 50 |
| Construction workers | 5 | 200 | 200 | 0 | Printers | 5 | 200 | 130 | 70 |
| Car repair shop workers | 10 | 200 | 200 | 0 | Forestry workers | 10 | 200 | 185 | 15 |
In accordance with Greek law, which stipulates that all employees must be examined on employment by the enterprise physician, all 4,000 workers filled in their individual health card and were examined by the company physicians who participated in the study. This resulted in a response rate of 100%.
One experienced specialist in occupational medicine, a former Factory Health Inspector of the Greek Ministry of Labor, assisted by three doctors specializing in occupational medicine were the enterprise physicians of the 104 firms and participated as researchers in this study. They personally administered specially designed occupational skin disease questionnaires (pertaining to occupational and medical history of present dermatoses) to workers, during interviews held in the company surgeries. They also recorded any skin condition that was caused or exacerbated by the patient's work, and asked their opinion as to which agents might have caused the condition. Employees gave their consent to them for the data to be collectively, anonymously, and statistically analyzed.
2.2. Diagnosis of cases of occupational dermatoses
Occupational dermatoses are caused by adverse working conditions. Other skin diseases caused by factors operating outside the workplace may be exacerbated by working conditions. Diagnosis of occupational dermatoses was made as follows: the clinical diagnosis of contact urticaria was made on the presence of wheals, triggered by physical stimuli (mechanical or thermal), which afflicted the skin mucous membranes [26]. The enterprise physicians recognized flares of atopic eczema (increased dryness, itching and redness, swelling, and general irritability) on physical examination after the interviews. Furthermore, they detected symptoms and signs of bacterial infection (weeping, pustules and crusts, atopic eczema failing to respond to therapy, rapidly worsening atopic eczema, fever, and malaise). They looked for signs of diseases in exposed skin areas. They examined previous medical records, personal history (atopy, sensitivity to several allergens), family history, and occupational history. They made an accurate assessment of the degree and extent of skin contact. They considered the type and duration of skin exposure to suspected causal factors, time of onset, and site of any initial skin complaint and of secondary spread. They also documented and considered in sufficient detail any temporal relationship between manifestation of skin disease and work activity (i.e., periods of clinical improvement after the cessation of work), and cleaning substances used, and any cluster of cases in the same work place. They also considered descriptions of work tasks and practices and evaluated materials, products, and working processes, and thermal working environment. They made risk assessments of exposures to chemicals used or other occupational skin health hazards and related factors. These included young age, history of atopic dermatitis, frequency of washing hands (>15 times a day), and not using protective measures (personal protective equipment). They carried out occupational hygiene work and assessed the magnitude of harmful agents. They carried out workplace inspections to diagnose any possible airborne induced skin reactions following actual exposure to chemicals, plastics, preservatives, metals, rubbers, plants, wood allergens, natural resins, or glues. They used any existing measurement results to assess the relationship between occupational hazards and dermatoses. They also identified potential risks for occupational skin diseases, reviewed existing relevant medical management and preventive, control measures and made relevant recommendations. They evaluated occupational stress factors possibly contributing to symptoms of occupational skin disease in workers. Stress may exacerbate atopic eczema, which itself may be a cause of psychological distress [27]. Living with skin diseases can evoke a host of negative feelings. Feelings such as unhappiness, embarrassment, worthlessness, frustration, anxiety and anger can lead to low self-esteem, stress, and even depression, and can have a severe impact on quality of life [28]. People with eczema often have a feeling of social isolation as a result of feeling unable to form friendships and relationships [29].
In cases where enterprise physicians could not make a specific diagnosis of a skin disease, they would refer the worker to a specialist dermatologist. Cases of occupational skin diseases were diagnosed initially by the occupational physicians or by skin specialists and then confirmed by the occupational physicians. Dermatologists performed patch tests with standard and related allergens related to chemicals in each enterprise or prick tests, in Dermatology Outpatient Departments of National Health Service Hospitals or State certified laboratories to diagnose certain cases of occupational contact dermatitis and dermatoses. The occupational physicians diagnosed occupational allergic contact dermatitis in workers showing a positive result, which was reported to them by the dermatologists, only in cases where there was evidence that the sensitization occurred at work. They also revisited the workplaces to assess the relevance of previously unexplained positive patch test reactions, to identify missed allergens in order to diagnose non-typical cases of occupational allergic dermatitis. Following consideration of industrial relations, psychological, social, and economic factors, they recommended (jointly with safety officers, in certain instances) appropriate measures for the improvement of working environment and practices, the work organization, and for the use of personal protective equipment. Their recommendations, whenever applied and combined with sound medical management, resulted in the improvement of prognosis of skin diseases of afflicted workers.
All workers with dermatitis had their blood tested (in National Health Service or State-certified private laboratories) for erythrocyte sedimentation rate, antinuclear antibodies, C-reactive protein, urea, creatinine and glucose, so that systemic disease could be excluded or diagnosed. Estimation of immunoglobulin E and specific radio-allergo-sorbant tests were carried out, so that atopy could be confirmed in certain cases.
In addition, we examined the medical records of the 4,000 employees, which were securely kept in the medical departments of the firms, for the purpose of detecting any additional cases of occupational dermatoses.
Each occupational physician was asked to diagnose whether a worker suffered from one or more of seven occupational dermatoses: acute and chronic contact dermatitis, contact urticaria, mechanical or traumatic injury, acne, burns, and malignant tumors. These skin diseases are also included in the official list of compensatable occupational dermatoses specified by law in Greece. The company occupational physicians were asked to record the diagnosis, which was then coded using the international classification of diseases, 10th Revision (ICD-10) [30]. The companies included in our study were geographically spread over all regions of Greece. They were considered to be a representative sample of Greek companies of the same type, regarding size of workforce, years of operation, working practices, and weather conditions (temperature, relative humidity, sunshine).
2.3. Statistical analysis
We recorded and analyzed all cases of skin diseases associated with occupational exposures manifested during employment in the 104 firms. We calculated prevalence rates of occupational skin diseases in different enterprises. We then applied the χ2 test to detect statistically significant differences in occupational dermatoses by examining the correlation between two variables, i.e., type of enterprise (or occupation) and diagnosed occupational dermatoses. Continuous variables are presented as mean ± standard deviation and categorical variables as counts and percentages. The differences between the groups were assessed with a two-sided χ2 test or Fisher's exact test for categorical data. All statistical analyses were performed with the use of SPSS software (version 12.0, SPSS Inc., Chicago, IL, USA). Statistical significance was considered at p < 0.05 (for two-tailed hypothesis). In view of the internal validity of the study, statistically significant differences shown by the χ2 test reinforce the importance of actual differences found in so far as they may determine priorities for future research.
3. Results
Prevalence rates of occupational skin diseases by type of work are presented in Table 2. There is a statistically significant correlation between each occupational skin disease and all types of enterprises studied, as shown in Table 2 (χ2 value significant at p < 0.001). We diagnosed 266 cases of acute contact dermatitis, 480 cases of chronic contact dermatitis, 580 cases of urticaria, 323 cases of mechanical injury, 413 cases of acne, 200 cases of burns, and 64 cases of tumors, i.e., 2,326 cases of occupational dermatoses in total among the 4,000 workers studied (Table 2). Investigation of the 4,000 workers revealed that those who suffered from two occupational dermatoses from 2006 to 2012. Of the 580 workers with contact urticarial, 300 also suffered from contact dermatitis. Of the 323 workers with dermatoses caused by mechanical injuries, 200 also suffered from contact dermatitis. Of the 413 workers with acne, 200 also suffered from contact dermatitis. Of the 64 workers with malignant skin tumors, 50 suffered from burns. i.e., 39.9% of our total study population (Table 2 and Fig. 1). Of the 746 total cases of contact dermatitis 300 were confirmed by direct skin tests, i.e., patch tests, performed by dermatologists. Thus, the total number of workers suffering from occupational dermatoses was 1,596.
Table 2.
Distribution of prevalence of occupational dermatoses by type of enterprise and application of the χ2 test (p < 0.001)
| Type of Enterprise | Prevalence of contact dermatitis acute–chronic |
Prevalence of other types of dermatoses |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Acute dermatitis | Chronic dermatits | Total no. of cases | Contact urticaria | Mechanical injury | Acne | Burns | Malignant tumors | Total no. of participants | |
| Bitumen laying workers | 11 (5.5) | 29 (14.5) | 40 (20.0) | 29 (14.5) | 12 (6.0) | 47 (23.5) | 13 (6.5) | 6 (3.0) | 200 (100) |
| Μetal workers | 15 (7.5) | 17 (8.5) | 35 (16) | 22 (11.0) | 23 (11.5) | 13 (6.5) | 10 (5.0) | 3 (1.5) | 200 (100) |
| Carpenters | 9 (4.5) | 16 (8.0) | 24 (12) | 18 (9.0) | 18 (9.0) | 35 (17.5) | 0 (0.0) | 4 (2.0) | 200 (100) |
| Farmers | 11 (5.5) | 14 (7.0) | 25 (12.5) | 30 (15.0) | 9 (4.5) | 0 (0.0) | 15 (7.5) | 11 (5.5) | 200 (100) |
| Carbonated drinks bottling industry workers | 11 (5.5) | 20 (10.0) | 31 (15.5) | 27 (13.0) | 14 (7.0) | 10 (5.0) | 28 (14.0) | 2 (1.0) | 200 (100) |
| Detergent manufacturing industry workers | 13 (6.5) | 15 (7.5) | 28 (14.0) | 19 (9.5) | 7 (3.5) | 7 (3.5) | 6 (3.0) | 2 (1.0) | 200 (100) |
| Car repair shop workers | 10 (5.0) | 30 (15.0) | 40 (20.0) | 20 (10.0) | 30 (15) | 15 (7.5) | 5 (2.5) | 3 (1.5) | 200 (100) |
| Forestry workers | 11 (5.5) | 19 (9.5) | 30 (15) | 32 (16.0) | 22 (11) | 16 (8.0) | 10 (5.0) | 7 (3.5) | 200 (100) |
| Pesticide application workers | 11 (5.5) | 13 (6.5) | 24 (12) | 13 (6.5) | 13 (6.5) | 27 (13.5) | 13 (6.5) | 3 (1.5) | 200 (100) |
| Hairdressers | 27 (13.5) | 33 (16.5) | 60 (30) | 32 (16.0) | 7 (3.5) | 10 (5.0) | 4 (2.0) | 0 (0.0) | 200 (100) |
| Kitchen staff | 30 (15) | 29 (14.5) | 59 (29.5) | 29 (14.5) | 15 (7.5) | 11 (5.5) | 14 (7.0) | 0 (0.0) | 200 (100) |
| Plastic manufacturing workers | 6 (3.0) | 18 (9.0) | 24 (12.0) | 25 (12.5) | 8 (4.0) | 5 (2.5) | 8 (4.0) | 1 (0.5) | 200 (100) |
| Food industry workers | 12 (6.0) | 23 (11.5) | 35 (17.5) | 30 (15.0) | 10 (5.0) | 4 (2.0) | 0 (0.0) | 0 (0.0) | 200 (100) |
| Printers | 11 (5.5) | 48 (24.0) | 59 (29.5) | 41 (20.5) | 20 (10) | 24 (12.0) | 0 (0.0) | 0 (0.0) | 200 (100) |
| Footwear artisan factory workers | 5 (2.5) | 26 (13.0) | 31 (15.5) | 22 (11.0) | 12 (6.0) | 47 (23.5) | 8 (4.0) | 3 (1.5) | 200 (100) |
| Pharmaceutical industry workers | 13 (6.5) | 22 (11) | 35 (17.5) | 37 (18.5) | 12 (6.0) | 38 (19) | 7 (3.5) | 3 (1.5) | 200 (100) |
| Paint manufacturing industry workers | 11 (5.5) | 29 (14.5) | 40 (20) | 29 (14.5) | 12 (6.0) | 47 (23.5) | 13 (6.5) | 6 (3.0) | 200 (100) |
| Industrial cleaning workers | 11 (5.5) | 27 (13.5) | 38 (19) | 26 (13) | 24 (12) | 32 (16) | 26 (13) | 0 (0.0) | 200 (100) |
| Office workers | 18 (9.0) | 32 (16) | 50 (25) | 40 (20) | 25 (12.5) | 25 (12.5) | 20 (10) | 15 (7) | 200 (100) |
| Construction workers | 20 (10) | 20 (10) | 40 (20) | 59 (29) | 30 (15) | 20 (10) | 20 (10) | 10 (5.0) | 200 (100) |
| Total | 266 (6.7) | 480 (12) | 746 (18) | 580 (14) | 323 (8.1) | 413 (10.9) | 200 (5.3) | 64 (1.7) | 4000 (100) |
| χ2 (19 degrees of freedom)∗ | 58.9 | 64.3 | 85.3 | 78.0 | 69.4 | 223.7 | 114.0 | 59.3 | |
Data are presented as n (%).
* All χ2 values statistically significant at p < 0.001.
Fig. 1.
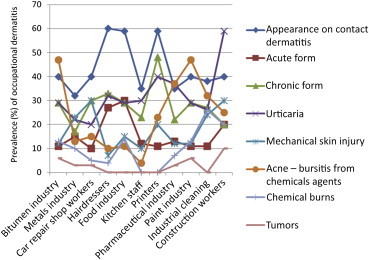
Types of enterprises with the highest prevalence of occupational skin diseases studied.
The highest prevalence rates of contact dermatitis, as shown in Table 2 and Fig. 1, are among hairdressers (30.0%), kitchen staff (29.5%), and printers (29.5%). Only 6.7% of all workers studied suffered from occupational acute contact dermatitis, with the highest prevalence rate (15.0%) observed among kitchen staff; 12.0% suffered from occupational chronic contact dermatitis, with the highest rate observed among printers (24.0%); 14.5% suffered from occupational contact urticaria, with the highest rate observed among construction workers (29.0)%. Furthermore, 8.1% of all workers developed occupational mechanical injury 15.0% of construction workers and 15.0% of car repair shop workers. Of all workers, 10.9% suffered from acne, the highest rates recorded among bitumen workers (23.5%), footwear artisan factory workers (23.5%), and workers in the paint manufacturing industry (23.5%). Of all workers, 5.3% suffered from chemical burns, the highest rates observed among carbonated drinks bottling industry workers (14.0%) and industrial cleaning workers (13.0%). The prevalence rate of malignant skin tumors among all workers was 1.7%, the highest rates being recorded among farmers (5.5%), and construction workers (5.0%).
Distribution of the prevalence of occupational skin diseases by sex and type of dermatoses is presented in Table 3. There was a statistically significant difference in the prevalence of mechanical injuries between genders, men being mainly afflicted [χ2 (1 degree of freedom) = 13.4 and p = 0.001] and in the prevalence of occupational chronic contact dermatitis, women being mainly afflicted [χ2 (1 degree of freedom) = 5.53 and p = 0.019].
Table 3.
Distribution of prevalence of occupational dermatoses by sex and type of dermatose
| Type of dermatose | Total no. of contact dermatitis | Acute contact dermatitis | Chronic contact dermatitis | Contact urticaria | Mechanical injury | Acne | Burns | Malignant tumors | Total no. of participants |
|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||
| M | 466 (18.2) | 182 (7.1) | 284 (11.1) | 388 (15.2) | 237 (9.3) | 281 (11.3) | 134 (5.4) | 47 (1.9) | 2560 (100) |
| F | 280 (19.4) | 84 (5.8) | 196 (13.6) | 192 (13.3) | 86 (6.0) | 132 (10) | 66 (5) | 17 (1.3) | 1440 (100) |
| Total | 745 (18.6) | 266 (6.7) | 480 (12) | 580 (14.5) | 323 (8.1) | 413 (10.9) | 200 (5.3) | 64 (1.7) | 4000 (100) |
| χ2 | 1.00 | 2.40 | 5.53 | 2.47 | 3.40 | 1.58 | 0.20 | 1.92 | |
| p* | 0.318 | 0.119 | 0.019 | 0.116 | <0.001 | 0.210 | 0.596 | 0.166 | |
Data are presented as n (%).
*p = p level at which the value of the χ2 test was statistically significant.
4. Discussion
This is the first study to reveal the occurrence of occupational dermatoses in workers practicing many different occupations in Greece. It concerns only cases of occupational dermatoses. We studied occupational dermatoses in workers who were at a high risk for occupational dermatitis on account of their occupational exposure, which was similar within each type of enterprise. We found a high overall prevalence rate, which can be accounted for by the hazardous working conditions prevailing in many of the 104 companies studied, resulting also from a limited compliance with Greek occupational health law pertaining to the application of health protection at work. It is noted that no data on skin diseases by occupation are analyzed by the national statistical service of Greece [31]. Furthermore, very few cases of dermatoses are compensated annually as occupational skin diseases by the National Institute of Health (IKA), which is the national insurance scheme of Greece and reported only 17 cases of contact dermatitis in 2005 [32]. Interestingly, no cases of other types of occupational dermatoses were reported to the IKA This stands in sharp contrast with the 1,596 cases of occupational dermatoses and the 746 cases of contact dermatitis diagnosed in our study in 4,000 workers, in the period 2006–2012. This discrepancy can be accounted for by the under-diagnosing and under-reporting of all cases of occupational diseases in Greece to date. We found that cases of occupational contact dermatitis constituted 32.1% of total cases of occupational dermatoses. We demonstrated a statistically significant correlation between seven occupational skin diseases and 20 types of enterprises (i.e., types of work). The different prevalence rates indicate different risks prevailing in the various enterprises studied.
Several prospective cohort and cross-sectional studies on contact dermatitis have reported high occurrences in workers employed in various occupations: 9% in metal working apprentices in car industry [23], 15% in dentists [24], 18% in hairdressers [25], 20% in metal workers (turners, machinists and toolmakers) [30], 28% in veterinarians [31], and 25–30% in nurses [33].
Active medical surveillance and workplace visits resulted in identifying substances to which workers may have been continuously exposed inadvertently. In conventional printing technology, allergens, including formaldehyde, methyl-chloro-iso-thiazolinone, chromate cobalt, and organic solvents used to clean down machinery, were found to create chronic contact dermatitis in printers. Nethercott et al [34] in Toronto, Canada, recorded the occurrence of dermatitis in the printing industry. Following an investigation, kitchen staff were observed handling raw and moist food for many hours each day. They used cleansers, detergents, frequent hand washing, and rarely wore gloves. Contact dermatitis was a frequent disorder among patients who handled food. Of them, 5.7% suffered from irritant contact dermatitis, 2.4% from contact urticaria, and 1.8% from allergic contact dermatitis [35].
We found, in agreement with another study [36], that hairdressers presented contact dermatitis, which was confirmed by dermatologists who performed patch tests. These tests revealed allergies to preservatives such as formaldehyde, fragrances, rubber chemicals, methyl-di-bromo-glutaronitrile in shampoos and to leave-on products. Most hairdressers who wore costume jewelry showed nickel sensitization.
The current study confirmed that prevalence of chemical burns among industrial cleaning workers is high (13.0%) due to exposure to organic solvents, acids, alkali, detergents, and oxidizing agents among those who were not wearing rubber gloves, a finding compatible with other studies [6,22]. Annual incidence of occupational contact dermatitis among cleaning workers was reported to be 43.5/100,000 employees in France [37].
High occurrence of malignant tumors among farmers was attributed to exposure to solar radiation, pesticides, chemical fertilizers, and machinery fuels [38,39]. Hogan et al [40] in Florida, USA, found that contact dermatitis and nonmelanoma skin cancer were the most common occupational skin disorders in North American workers.
Cement containing chromate salts and chlorinated hydrocarbons was suspected as the cause of acne in bitumen laying workers, a finding compatible with the findings reported by Stocks et al [8,41].
Lazzarini et al [42] also found a high incidence of allergic contact dermatitis among construction workers who had a high frequency of sensitization to cement, in Brazil.
Mechanical wear and tear, light oils, degreasing solvents, and synthetic mineral fibers have been found to frequently cause irritation of the skin [43]. Mechanical injuries in car repair workers were triggered by mechanical factors causing friction, pressure, blisters, callus, and myositis.
Prevalence rates of certain occupational skin diseases were higher among specific types of enterprises. This indicates a need for preventive measures to be applied, aiming at the improvement of working conditions in these enterprises. Our findings might be of significant importance for Greece, because no data on occupational diseases by type of economic activity or occupation are collected or analyzed by the national statistical service of Greece. We found the largest number of cases of occupational skin diseases among construction workers, although the highest incidence has been reported in agriculture, forestry, and fishing [29].
We found that the top five enterprises with the highest prevalence rates for skin mechanical injury were the metal industry, wood industry, car industry (where all 200 workers were men), cooks, and construction workers (where all 200 workers were men). Previous research has produced similar results, i.e., a high incidence of prevalence rates of occupational dermatitis in manufacturing and processing industries [31,44–47]. Wigger-Alberti et al [47] found cases of irritant contact dermatitis among metal workers in Switzerland.
We found a higher prevalence rate for mechanical injury among men than that among women. This can be accounted for by the fact that mainly men were employed in most of the high-risk types of enterprises studied. We found the highest prevalence rates of chronic contact dermatitis among printers (130 of who were men), paint industry workers (140 of who were men), and car repair workers (all 200 were men). Prevalence rates of acne from chemical causes were the highest among bitumen laying workers, carpenters, artisan factory workers, paint manufacturing workers and construction workers. Prevalence rates of chemical burns were the highest among carbonated drinks bottling industry workers, pesticide application workers, bitumen laying workers, cooks, construction workers, and farmers.
Our study was based on national reporting schemes of occupational skin diseases across the UK [18,48,49]. To improve the discovery of new cases of occupational dermatitis, the occupational physicians were encouraged to carry out active medical surveillance of workers at risk, with the help of a recently adopted guideline [46,50]. The data collection method that we used entailed systematic reporting by occupational physicians in a broad range of enterprises (occupations). Participating occupational physicians diagnosed and recorded all cases of occupational dermatoses. As in other voluntary surveillance schemes, reliable reporting was dependent on sustaining enthusiasm and discipline in the participants. We recommend that a national voluntary skin health surveillance system of workers at risk be established in Greece to provide insights into the occurrence, distribution, and secular trends of occupational dermatoses in different occupational groups; to produce more accurate estimates of the contribution of work to the overall burden of work-related dermatitis; to improve the diagnosis of new cases of occupational dermatoses; and to obtain reliable data on occupational dermatoses. Relevant guidelines should be issued. Such a system would also have an alarm function, as it would reveal either unknown agents causing occupational dermatoses or new occupational groups at risk.
Further research, also in Greece, can contribute to the discovery of new risk factors for occupational dermatoses. It is also necessary to evaluate whether, and to what extent, workplace interventions can reduce to skin related working conditions. Occupational physicians liaising with dermatologists should jointly inform workers about work related skin health hazards. Articulating the need for action, regarding the implementation of worker protection systems in small and medium sized enterprises, whose workers have a significantly higher risk of developing occupational skin diseases when handling skin affecting substances, is of crucial importance [51].
4.1. Limitations and strengths of the study
We did not identify, measure, or control for variables in the analysis, which could have acted as confounding factors. Therefore, conclusions resulting from the comparison between values of prevalence rates and the correlation between occupational dermatoses and type of enterprise might be biased. This deficiency could be rectified in further research. Nevertheless, there is no reason to assume that the proportion of employees with dermatoses (either occupational or nonoccupational) manifested prior to their appointment in the enterprises studied was significantly different among the 20 types of enterprises included in our study. Therefore, prior dermatoses were not considered as a confounding factor.
Clearly, our target populations allowed us to perform a more valid study compared with any study that would have been carried out in one enterprise only. Based on our own study, industry specific studies of occupational dermatoses could be carried out in Greece.
Another limitation of this study concerns its external validity. Its internal validity has some value as regards the study population studied, i.e., the 104 firms, it has no external validity. Our findings are only indicative with regard to the prevalence of dermatoses in all the enterprises of the same type in this country. Nevertheless, our study revealed an occupational health problem in Greece, i.e., that many cases of occupational diseases do exist. It has two valid conclusions: there is a need for the establishment of a systematic voluntary occupational disease recording system in Greece; and more attention should be paid to the prevention of occupational dermatoses. Similar circumstances may exist in the same types of enterprises in other countries, where our study might also be of some use.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Paananen S., editor. Dangers at work: perceived occupational diseases, accidents and violence at work in 1999. Statistics Finland; Helsinki (Finland): 2000. 15 p. [in Finnish] [Google Scholar]
- 2.Goh C.L. Occupational skin disease in Singapore. Epidemiology and causative agents. Ann Acad Med Singapore. 1987;16:303–305. [PubMed] [Google Scholar]
- 3.De Craecker W., Roskams N., Op de Beek R. European Risk Observatory Report; Brussels (Belgium): 2009. Occupational skin diseases and dermal Exposure in the European Union (EU-25): policy and practice overview; p. 79. [Google Scholar]
- 4.De Craecker W., Roskams N., Op de Beek R. European Agency for Safety and Health at Work; Bilbao (Spain): 2008. Occupational skin diseases and dermal exposure in the EU (EU-25) European Risk Observatory Report; pp. 16–17. [Google Scholar]
- 5.Health and Safety Executive (HSE) HSE; London (UK): 2009. Report: dermatitis and other skin disorders—working days lost, Skin at work. 461 p. [Google Scholar]
- 6.Hathaway G.J., Proctor N.H., Hughes J.P., Fischman M.L. 3rd ed. Van Nostrand Reinhold; New York (NY): 1991. Proctor and Hughes' chemical hazards of the workplace. 531 p. [Google Scholar]
- 7.Adams R.M. In: Occupational skin disease. 2nd ed. Adams R.M., editor. W.B. Saunders; Philadelphia (PA): 1990. pp. 26–31. [Google Scholar]
- 8.Stocks S.J., Turner S., McNamee R., Carder M., Hussey L., Agius R.M. Occupation and work-related ill-health in UK construction workers. Occup Med. 2011;61:407–415. doi: 10.1093/occmed/kqr075. [DOI] [PubMed] [Google Scholar]
- 9.Epstein W.L., Byers V.S., Frankart W. Induction of antigen specific hyposensitization to poison oak in sensitized adults. Arch Dermatol. 1982;118:630–633. [PubMed] [Google Scholar]
- 10.Turjanmaa K. Incidence of immediate allergy to latex gloves in hospital personnel. Contact Dermat. 1987;17:270–275. doi: 10.1111/j.1600-0536.1987.tb01476.x. [DOI] [PubMed] [Google Scholar]
- 11.Mathias C.G. Food substances may cause skin reactions among handlers. Occup Health Saf. 1984;53:53–56. [PubMed] [Google Scholar]
- 12.Jansen T., Kreuter A., Altmeyer P. When no therapy helps the acne patient, ask him if he works at McDonald's! MMW Fortschr Med. 2000;42:37–39. [in German] [PubMed] [Google Scholar]
- 13.Kokelj F. Occupational acne. Clin Dermatol. 1992;10:213–217. doi: 10.1016/0738-081x(92)90108-b. [DOI] [PubMed] [Google Scholar]
- 14.Alam M., Ratner D. Cutaneous squamous-cell carcinoma. N Engl J Med. 2001;344:975–983. doi: 10.1056/NEJM200103293441306. [DOI] [PubMed] [Google Scholar]
- 15.Jerant A.F., Johnson J.T., Sheridan C.D., Caffrey T.J. Early detection and treatment of skin cancer. Am Fam Physician. 2000;62:357–368. [PubMed] [Google Scholar]
- 16.Gawkrodger D.J. Occupational skin cancers. Occup Med (Lond) 2004;54:458–463. doi: 10.1093/occmed/kqh098. [DOI] [PubMed] [Google Scholar]
- 17.Fonds voor de Beroepsziekten . 2006. Het Jaarverslag. Van het fonds voor de beroepsziekten, FBZ; pp. 109–112. [in German] [Google Scholar]
- 18.Meyer J.D., Chen Y., Holt D.L., Beck M.H., Cherry N.M. Occupational contact dermatitis in the UK: a surveillance report from EPIDERM and OPRA. Occup Med (Lond) 2000;50:265–273. doi: 10.1093/occmed/50.4.265. [DOI] [PubMed] [Google Scholar]
- 19.Cherry N., Meyer J.D., Adisesh A., Brooke R., Owen-Smith V., Swales C., Beck M.H. Surveillance of occupational skin disease: EPIDERM and OPRA. Br J Dermatol. 2000;142:1128–1134. doi: 10.1046/j.1365-2133.2000.03537.x. [DOI] [PubMed] [Google Scholar]
- 20.Gawkrodger D.J., Lloyd M.H., Hunter J.A. Occupational skin disease in hospital cleaning and kitchen workers. Contact Dermat. 1986;15:132–135. doi: 10.1111/j.1600-0536.1986.tb01312.x. [DOI] [PubMed] [Google Scholar]
- 21.Noe R., Cohen A.L., Lederman E., Gould L.H., Alsdurf H., Vranken P., Ratard R., Morgan J., Norton S.A., Mott J. Skin disorders among construction workers following Hurricane Katrina and Hurricane Rita: an outbreak investigation in New Orleans, Louisiana. Arch Dermatol. 2007;143:1393–1398. doi: 10.1001/archderm.143.11.1393. [DOI] [PubMed] [Google Scholar]
- 22.Fujimoto K., Yasuhara N., Kawarada H., Kosaka S., Kawana S. Burns caused by dilute hydrofluoric acid in the bleach. J Nippon Med Sch. 2002;69:180–184. doi: 10.1272/jnms.69.180. [DOI] [PubMed] [Google Scholar]
- 23.Sartorelli P., Romeo R., Paolucci V., Puzzo V., Di Simplicio F., Barabesi L. Skin photoaging in farmers occupationally exposed to ultraviolet radiations. Med Lav. 2013;104:24–29. [PubMed] [Google Scholar]
- 24.European Agency for Safety and Health at Work (EASHW) Bilbao (Spain); 2003. Technical report, No. 40, Skin sensitizers; pp. 175–182. [Google Scholar]
- 25.Simon J. International Study of Life with Atopic Eczema (ISOLATE) J Eur Acad Dermatol Venereol. 2004;1:45–50. [Google Scholar]
- 26.Williams J.D., Lee A.Y., Matheson M.C., Frowen K.E., Noonan A.M., Nixon R.L. Occupational contact urticaria: Australian data. Br J Dermatol. 2008;159:125–131. doi: 10.1111/j.1365-2133.2008.08583.x. [DOI] [PubMed] [Google Scholar]
- 27.Beltrani V.S., Boguneiwicz M. Atopic dermatitis. Dermatol Online J. 2003;9:1. [PubMed] [Google Scholar]
- 28.O'Donnell B.F., Lawlor F., Simpson J., Morgan M., Greaves M.W. The impact of chronic urticaria on the quality of life. Br J Dermatol. 1997;136:197–201. [PubMed] [Google Scholar]
- 29.Rycroft R.J.G. Rook/Wilkinson/Ebling textbook of dermatology. 6th ed. Blackwell Science, Inc.; Oxford: 1998. Occupational Dermatoses; pp. 861–879. [Google Scholar]
- 30.World Health Organisation, Forty-third World Health Assembly. Washington, DC: Bureau of Labor Statistics, US Department of Labor. Survey of Occupational Injuries and Illness; 1997. p. 65–70.
- 31.Hellenic Statistic Authority . ELSTAT; Athens (Greece): 2007. 2008. Statistics of Social Welfare and Health—Categories of diseases and groups of discharged patients; pp. 91–100. [Google Scholar]
- 32.Alexopoulos C.G., Rachiotis G., Valassi M., Drivas S., Behrakis P. Under-registration of occupational diseases: the Greek case. Occup Med (Lond) 2005;55:64–65. doi: 10.1093/occmed/kqh126. [DOI] [PubMed] [Google Scholar]
- 33.Jungbauer F.H., Lensen G.J., Groothoff J.W., Coenraads P.J. Hand dermatitis in the healthcare sector. Tijdschrift Bedrijfs. 2004;12:135–139. [in Dutch] [Google Scholar]
- 34.Nethercott J.R. Dermatitis in the printing industry. Dermatol Clin. 1988;6:61–66. [PubMed] [Google Scholar]
- 35.Vester L., Thyssen J.P., Menné T., Johansen J.D. Occupational food-related hand dermatitis seen over a 10-year period. Contact Dermat. 2012;66:264–270. doi: 10.1111/j.1600-0536.2011.02048.x. [DOI] [PubMed] [Google Scholar]
- 36.Lyons G., Roberts H., Palmer A., Matheson M., Nixon R. Hairdressers presenting to an occupational dermatology clinic in Melbourne, Australia. Contact Dermat. 2013;68:300–306. doi: 10.1111/cod.12016. [DOI] [PubMed] [Google Scholar]
- 37.Halioua B., Bensefa-Colas L., Crepy M., Bouquiaux B., Assier H., Billon S., Chosidow O. Occupational dermatitis in cleaning and maintenance workers. Analysis of 769 cases declared to the Caisse Nationale d'Assurance Maladie des Travailleurs Salaries between 2004 and 2007. Ann Dermatol Venereol. 2012;139:526–531. doi: 10.1016/j.annder.2012.05.004. [in French] [DOI] [PubMed] [Google Scholar]
- 38.Spiewak R. Pesticides as a cause of occupational skin diseases in farmers. Ann Agric Environ Med. 2001;8:1–5. [PubMed] [Google Scholar]
- 39.Woolley T., Lowe J., Raasch B., Glasby M., Buettner P.G. Workplace sun protection policies and employees' sun-related skin damage. Am J Health Behav. 2008;32:201–208. doi: 10.5555/ajhb.2008.32.2.201. [DOI] [PubMed] [Google Scholar]
- 40.Hogan D.J., Tanglertsampan C. The less common occupational dermatoses. Occup Med. 1992;7:385–401. [PubMed] [Google Scholar]
- 41.Stocks S.J., McNamee R., Turner S., Carder M., Agius R.M. Has European legislation to reduce exposure to chromate in cement been effective in reducing the incidence of allergic contact dermatitis attributed to chromate in the UK? Occup Environ Med. 2012;69:150–152. doi: 10.1136/oemed-2011-100220. [DOI] [PubMed] [Google Scholar]
- 42.Lazzarini R., Duarte I.A., Sumita J.M., Minnicelli R. Allergic contact dermatitis among construction workers detected in a clinic that did not specialize in occupational dermatitis. An Bras Dermatol. 2012;87:567–571. doi: 10.1590/s0365-05962012000400008. [DOI] [PubMed] [Google Scholar]
- 43.Sagransky M.J., Pichardo-Geisinger R.O., Muñoz-Ali D., Feldman S.R., Mora D.C., Quandt S.A. Pachydermodactyly from repetitive motion in poultry processing workers: a report of 2 cases. Arch Dermatol. 2012;148:925–928. doi: 10.1001/archdermatol.2012.983. [DOI] [PubMed] [Google Scholar]
- 44.Grimshaw J.M., Russell I.T. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 45.Burnett C.A., Lushniak B.D., McCarthy W., Kaufinan J. Occupational dermatitis causing days away from work in U.S. private industry, 1993. Am J Ind Med. 1998;34:568–573. doi: 10.1002/(sici)1097-0274(199812)34:6<568::aid-ajim4>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 46.Fregert S. Occupational dermatitis in a 10-year material. Contact Dermat. 1975;1:96–107. doi: 10.1111/j.1600-0536.1975.tb05334.x. [DOI] [PubMed] [Google Scholar]
- 47.Wigger-Alberti W., Hinnen U., Elsner P. Predictive testing of metal working fluids: a comparison of 2 cumulative human irritation models and correlation with epidemiological data. Contact Dermat. 1997;36:14–20. doi: 10.1111/j.1600-0536.1997.tb00916.x. [DOI] [PubMed] [Google Scholar]
- 48.McDonald J.C., Beck M.H., Chen Y., Cherry N.M. Incidence by occupation and industry of work-related skin diseases in the United Kingdom, 1996–2001. Occup Med (Lond) 2006;56:398–405. doi: 10.1093/occmed/kql039. [DOI] [PubMed] [Google Scholar]
- 49.Mathias C.G., Morrison J.H. Occupational skin diseases, United States, Results from the Bureau of Labor Statistics Annual Survey of Occupational Injuries and Illnesses, 1973 through 1984. Arch Dermatol. 1988;124:1519–1524. doi: 10.1001/archderm.124.10.1519. [DOI] [PubMed] [Google Scholar]
- 50.Betts R.F., Penn R.L. 5th ed. 2003. A practical approach to infectious diseases; pp. 97–102. New York (NY) [Google Scholar]
- 51.Smith H.A., Burdorf A., Coenraads P.J. Prevalence of hand dermatitis in different occupations. Int J Epidemiol. 1993;22:288–293. doi: 10.1093/ije/22.2.288. [DOI] [PubMed] [Google Scholar]


