Abstract
Background
Stochastic resonance whole-body vibration training (SR-WBV) was tested to reduce work-related musculoskeletal complaints.
Methods
Participants were 54 white-collar employees of a Swiss organization. The controlled crossover design comprised two groups each given 4 weeks of exercise and no training during a second 4-week period. Outcome was daily musculoskeletal well-being, musculoskeletal pain, and surefootedness. In addition, participants performed a behavioral test on body balance prior to when SR-WBV started and after 4 weeks of SR-WBV.
Results
Across the 4-week training period, musculoskeletal well-being and surefootedness were significantly increased (p < 0.05), whereas musculoskeletal pain was significantly reduced only in those who reported low back pain during the last 4 weeks prior to the study (p < 0.05). Body balance was significantly increased by SR-WBV (p < 0.05).
Conclusion
SR-WBV seems to be an efficient option in primary prevention of musculoskeletal complaints and falls at work.
Keywords: low back pain, musculoskeletal system, occupational health
1. Introduction
A recent study on musculoskeletal complaints (MSC) showed high 1-month prevalence rates in office workers mostly between 10% and 30 % when values from 18 countries were compared [1]. Thereby, MSC cause absenteeism and to an even larger extent presenteeism that increases labor costs [2]. Work-related prevention of MSC therefore becomes an increasingly important goal [3]. Waddell and Burton [4] proposed that it should be possible to reduce MSC-related sickness absence and long-term incapacity by at least 30–50%, but this would require a fundamental shift in management culture. Part of this shift is occupational health promotion that includes work hardening efforts [5]. The problem of many worksite activity trainings, however, is low participation rate and a lack of compliance with training [6,7]. Compliance suffers because participants often have to invest more than 20 minutes for a training session [8], take further time prior to training to commute to other places in work, have to change clothes prior to training and after training, to complete their warming-up and cooling down, or to take a shower. By contrast, stochastic resonance whole-body vibration training (SR-WBV) is low in nonmonetary effort when compared to conventional exercise: SR-WBV has very short exercising duration (about 10 minutes), is easily carried out in work settings, and no change of clothes is necessary. The objective of this study was to investigate possible preventive effects of SR-WBV on MSC in white-collar workers doing office work.
1.1. Stochastic resonance whole-body vibration training
SR-WBV is whole-body vibration training with randomized vibration. Because the vibration is stochastic, the direction and the force-time behavior of the vibrations are not foreseeable and the body will be constantly challenged to adapt the muscle reactions [9–11]. SR-WBV seems to provoke an interaction of different types of neurophysiologic sensors and the adjustment of afferent and efferent signals, possibly acting as “training” for the sensorimotor system [9], even more so than other conventional sinusoidal vibration [12]. A strength increase is mainly attributed to neural adaptation, leading to improved intermuscular and intramuscular coordination, allowing increased activation of prime movers in specific movements and better coordination of the activation in all relevant muscles [13]. A low injury risk and the only rare appearance of side effects make whole-body vibration training an interesting preventive intervention [14,15]. There is evidence that stochastic whole-body vibration training can reduce musculoskeletal pain in metal manufacturing workers who were exposed to biomechanical risk factors [16]. However, musculoskeletal pain is also highly prevalent in office workers who perform sedentary work at video display units [17]. Risk factors in sedentary work include lack of posture change and psychosocial work risk factors such as mental stressors (e.g., time pressure and performance constraints) [3]. Thus, the current study tests the effectiveness of SR-WBV in employees doing sedentary office work. We expected SR-WBV to reduce MSC in terms of pain and increase musculoskeletal well-being (Hypothesis 1). Evidence indicates that training effects of SR-WBV include gain in postural control [18–20], although the physiological mechanism behind it is unclear so far [11]. Therefore, it was hypothesized that SR-WBV might help to increase postural control as shown in an increase in reported surefootedness—as a measure of perceived body balance—and balance performance in a standard behavioral balance test (Hypothesis 2).
In addition to a general positive effect of SR-WBV on MSC, surefootedness, and body balance, we suggested a particular positive effect on those who had low back pain in the 6 months prior to when the training started. In these employees SR-WBV was suggested to have a therapeutic effect in addition to the general training effect. Both, SR-WBV training efficiency [21] and therapeutic effects [15] were summarized recently. Thus, in Hypothesis 3 we expected those who currently or recently suffered from low back pain to show more intense training effects than others.
2. Materials and methods
2.1. Participants
Participants were employees from a Swiss organization in manufacturing systems engineering in aviation. All employees (N = 313) doing office work within the organization were asked to participate in the study. Of 313 employees, 58 (18.5%) agreed to participate. Four participants had to be excluded because of health risks. Exclusion criteria were: acute, past, or chronic arthropathologies; cardiovascular disease; psychopathology; spondylolysis; spondylolisthesis; tumors; prolapse with neurological failure; rheumatism, articular gout; osteoporosis; activated arthrosis with inflammatory signs; stage 4 arthrosis; pregnancy; knee or hip replacement; or electronic implants. Of the remaining sample of 54 participants, 51 were employed full time. Two participants worked an 80% time schedule (4 days a week) and one participant had a 70% work schedule (3.5 days a week). Age was between 18 years and 61 years [mean = 39.8 years, standard deviation (SD) = 10.4]. The sample consisted primarily of men (85.2%), reflecting the sex ratio in the total personnel of the organization. The average tenure for participants was 7 years. Educational level was high, with most participants (60%) having a university degree. Body mass index was 24.4 on average (SD = 2.8). Mean height was 1.78 m and mean weight was 78 kg. Participants did not receive medical treatment during the study.
The 54 volunteering employees were randomly assigned to two groups with balance for work field and few a posteriori adjustments for planned vacation, to prevent absences during exercises. Randomization was based on using a list of random numbers [22]. The resulting two groups of 27 participants each did not differ substantially in demographic characteristics, frequency of low back pain episodes over the 6 months prior to SR-WBV, and values of outcome variables on Day 1 of the study.
2.2. Design and procedure
In April 2009 all 313 employees doing office work within the organization were informed about the aim of the present study. The study goals were introduced as addressing organizational health. SR-WBV was characterized as a method to be tested to enhance physical fitness. Participants were informed about their rights including the right to stop the training whenever they wanted. Participants were given a guarantee of anonymity. All participants provided informed consent prior to their inclusion in the study. The study was performed in consensus with recommendations outlined by the Declaration of Helsinki and with all requirements defined by the Swiss Society of Psychology. The ethical committee of the responsible university faculty has approved the study proposal (Proposal No. 2009-04-0006).
The research design was a switching-replication design with randomized group allocation of participants (“randomized controlled crossover design”). The training of all participants was divided into two periods, both lasting 4 weeks. In the first period, Group A trained on a SR-WBV device three times a week whereas group B received no treatment (waiting group). After 4 weeks Group B received SR-WBV, whereas group A received no treatment. The exercises were completed at the place of work.
2.3. Stochastic resonance whole-body vibration training
A special device, the SRT-Zeptor Medical plus noise (FreiSwiss AG, Zurich, Switzerland), was used for the vibration treatment (Fig. 1). Its main features are two independent, one-dimensional (up/down) stochastically oscillating footboards (3 mm amplitude), with two passive degrees of freedom (forward/backward, right/left). In addition to vertical and horizontal actions the platforms also allow medial and lateral tilting, which leads to a pluridimensional movement.
Fig. 1.

Starting position on the stochastic resonance whole-body vibration training device.
All exercising sessions were supervised. Participants were instructed to stand on the footboards with the arms hanging loose to the side and slightly bent knees (i.e., a skiing posture). The vibration frequency in each 60-second session started with 5 Hz, and after the start of the training session participants could regulate the frequency within a range of between 4 Hz and 8 Hz by themselves. A session consisted of three sets, lasting 1 minute each, with a 1-minute break in between. All sessions were conducted at the beginning of the work shift between 6:00 a.m. and 8:00 a.m. Two participants shared an exercising session, so that when one person was having the 1-minute break, the other could exercise. Three such sessions per week were planned for each person. This setting was the same as used by Burger and colleagues [16] in a study on metal manufacturing workers. The goal of performing 12 training sessions in the 4-week training period was reached for most participants. The individual number of sessions absolved ranged between 9 and 14 (mean = 11.7, SD = 0.8). The chosen frequencies had a mean of 6.4 Hz (minimum = 4 Hz, maximum = 8 Hz, SD = 0.7 Hz).
Sex, age, body weight, body height, and low back pain in the previous 6 months were assessed in a baseline questionnaire prior to the start of SR-WBV. Low back pain was assessed with one item of the Nordic Questionnaire [23]. The item asked for frequency of low back pain episodes in the past 6 months (1 = none, 2 = less than once a month, 3 = once a month, 4 = once a week, 5 = daily).
2.4. Assessment of musculoskeletal pain and surefootedness
In this study, musculoskeletal pain was assessed with a daily questionnaire including weekends. However, because the sample consisted of employees who did not receive medical treatment and because of the relative healthiness of the participants a floor-effect for pain also had to be anticipated, and therefore, an additional daily outcome for musculoskeletal well-being was introduced. Daily assessment of reported surefootedness completed the diary assessments.
The questions on current musculoskeletal pain were part of the chronic pain grade questionnaire [24]. To measure daily pain the instruction was: “Throughout the day, how do you rate your personal sensation in muscles and joints (back pain, shoulder and neck pain, pain in leg muscles etc.)?” followed by “Pain in muscles and joints.” and “Muscle stiffness”. Cronbach alpha in the pain scale was 0.90. The two questions on musculoskeletal well-being asked for “Wellness in muscles and joints” and “Muscles feel relaxed”. Cronbach alpha of the musculoskeletal well-being scale was 0.96. The question on surefootedness—a measure of perceived body balance— was “How would you rate your surefootedness/sense of balance today?” All daily questionnaire items included a 10-point numerical rating scale (1 = not at all, 10 = best possible), which shows good sensibility and responsiveness to change, is easy to administer, and shows high compliance [25].
For the collection of MSC data, all questionnaire items were combined in a short questionnaire. Participants were asked to complete all eight items after work on a daily basis. The diary thus had one page per day for 7 days, including Saturdays and Sundays. Completed diaries were collected weekly and new diaries were distributed.
2.5. Clinical test of sensory integration on balance
Body balance performance was assessed by a behavioral test of body balance that, because of restrictions from spatial arrangements, could be performed only in the training condition prior to the start and after the end of SR-WBV training sessions. The behavioral test was the clinical test of sensory integration on balance (CTSIB) [26], which has been shown to have a good test-retest reliability in community dwelling older adults and younger adults of r = 0.99 [27]. The CTSIB correlates well with dynamic posturography in a group of normal patients age 20–79 years [28]. The test included four body positions in standing with crossed arms that participants should keep during 30 seconds (stand on floor, eyes open; stand on floor, eyes closed; stand on air pad, eyes open; stand on air pad, eyes closed). The dependent variable was the time the position was maintained (0–30 seconds). If the participant lost balance the observer recorded the time the position was kept.
2.6. Data analysis
Data was analyzed with longitudinal multilevel regression analysis [29] using the MLwiN software package version 2.10 (http://www.bristol.ac.uk/cmm/software/mlwin/refs.html) [30]. The level of significance was p < 0.05 (two-tailed). Dependent variables were daily musculoskeletal well-being, musculoskeletal pain, and surefootedness, with time (i.e., days) on Level 1 nested within persons (Level 2). Musculoskeletal well-being and surefootedness did not deviate from normal distribution whereas musculoskeletal pain was skewed because 19 participants reported to experience no daily musculoskeletal pain during the study period. The sample size of Level 2 with 54 persons met the recommended minimum sample size of 50 [31]. Time was represented in days, because outcomes were collected on a daily basis. The two exercising periods were parallelized for comparability and time was centered at endpoint, because the scope of the study was on final status [32]. Time range went, therefore, from –27 (first day) to 0 (last day), with the intercept representing outcome status at the end of training. A dummy variable represented the training [no training (0) versus SR-WBV (1)].
Because differences between participants, as well as within participants, over time (day of consecutive training) in outcomes were expected, the intercept was conceptualized as random effect on both levels. In addition to the overall effect of SR-WBV, low back pain prior to SR-WBV was added as a predictor and—in order to test the third hypothesis—the interaction between prior low back pain and SR-WBV was tested. Time, prior low back pain, and training effect were set as fixed effects. Hence, the regression model assumed the decrease of MSC and increase in well-being and surefootedness over time only for those absolving SR-WBV but not for those in the control group (Hypothesis 1 and Hypothesis 2). Moreover, the three-way interaction between training condition, time, and prior low back pain tests the assumption that the effect of SR-WBV should be larger in those with prior low back pain compared with those who reported no prior low back pain (Hypothesis 3). The multilevel regression model is represented by the following equation:
| (1) |
Subscript i indicates the Level 1 (time) variable that was assessed on daily basis and j indicates the Level 2 (person) variable.
3. Results
There was no study attrition. All participants passed through the 54 days of the study. In daily assessments there were no missing values. All participants accomplished the CTSIB prior to SR-WBV and after 4 weeks of SR-WBV. However, two participants provided no response to the Nordic questionnaire item on frequency of low back pain episodes in the past 6 months, and three participants failed to report their body weight. A nonparametric U-test compared all outcome variables on the first day of SR-WBV in those who started in the training group and those who started after 4 weeks (waiting group). Groups did not differ significantly in any outcome variable. Thus, data from both groups were merged.
Frequency of low back pain episodes in the past 6 months prior to the study showed no low back pain in 22 participants (40.7%). Thirteen participants reported to experience low back pain less than once a month, eight participants reported episodes once a month, and eight individuals reported to experience low back pain once a week. One participant reported daily low back pain in the past 6 months prior to SR-WBV. Mean values and correlations between studies variables are shown in Table 1. Low back pain in the 6 months prior to the start of SR-WBV was significantly related to musculoskeletal well-being at the first day of SR-WBV (r = –0.35, p < 0.05). Surefootedness on Day 1 of SR-WBV was significantly associated with body balance performance in CTSIB after 4 weeks of SR-WBV (r = 0.28, p < 0.05) but not significantly related with balance performance prior to when SR-WBV started. Age was negatively related to body balance performance in CTSIB prior to when SR-WBV started (r = –0.31, p < 0.05). Body mass index was higher in women than in men (p < 0.001). Two of three correlations between three daily measures of MSC were significant. Musculoskeletal well-being was negatively related with musculoskeletal pain (r = –0.60, p < 0.001) and positively related with sure-footedness on day one of SR-WBV (r = 0.46, p < 0.001). There was, however, no significant correlation between musculoskeletal pain and surefootedness on first day of SR-WBV (r = –0.16, p = 0.263). Meanwhile, across the 4 weeks of SR-WBV and 4 weeks of waiting group, i.e., on day level, comprising 3024 measurements (56 daily measurements by 54 participants) Musculoskeletal well-being, musculoskeletal pain, and surefootedness were significantly interrelated (Table 2). Correlations, however, were not that close that measures could be considered redundant.
Table 1.
Means, standard deviations, and correlations among study variables (N = 54)
| Mean | SD | Musculoskeletal well-being | Pain | Surefootedness | CTSIB pretraining | CTSIB posttraining | |
|---|---|---|---|---|---|---|---|
| Musculoskeletal well-being | 7.065 | 1.943 | |||||
| Pain | 2.648 | 1.736 | −0.603† | ||||
| Surefootedness | 8.593 | 1.560 | 0.460† | −0.155 | |||
| CTSIB pretraining | 28.510 | 1.756 | 0.219 | 0.165 | 0.182 | ||
| CTSIB posttraining | 29.320 | 0.775 | 0.225 | 0.102 | 0.281* | 0.716† | |
| LBP | 2.148 | 1.188 | −0.346* | 0.264 | −0.072 | 0.031 | −0.098 |
*p < 0.05.
†p < 0.001, two-tailed.
CTSIB, clinical test of sensory integration on balance; LBP, frequency of low back pain during last 6 months prior to when the study started; pain, self-reported musculoskeletal pain on first day of the study; surefootedness, self-reported perceived body balance on first day of the study.
Table 2.
Bivariate correlations among daily measures [n = 3,024 (54 individuals from 56 days)]
| Musculoskeletal well-being | Pain | |
|---|---|---|
| Musculoskeletal well-being | ||
| Pain | −0.655* | |
| Surefootedness | 0.554* | −0.330* |
*p < 0.01 (two-tailed).
Pain, self-reported musculoskeletal pain on first day of the study; surefootedness, self-reported perceived body balance on first day of the study.
3.1. Multilevel regression analysis
A first test was whether individual musculoskeletal well-being, musculoskeletal pain, and surefootedness showed both, interindividual and intraindividual variation of scores. The proportion of the total variation that reflects intraindividual variation were 47% in musculoskeletal well-being, 58% in musculoskeletal pain, and 31% in surefootedness. Thus, total variation was due in equal parts to individual and intraindividual variation.
SR-WBV was expected to increase musculoskeletal well-being and surefootedness and to decrease musculoskeletal pain across training days. Table 3 shows that in accordance with hypothesis 1 SR-WBV (p < 0.05) as well as the interaction of SR-WBV by day of training (p < 0.01) was significant in musculoskeletal well-being. A similar result pattern appeared in the prediction of surefootedness. In agreement with the second hypothesis SR-WBV (p < 0.001) as well as the interaction of SR-WBV by the day of training (p < 0.01) was significant. In prediction of musculoskeletal pain, prior low back pain was a significant predictor (p < 0.01) but contrary to Hypothesis 1 no overall positive effect of SR-WBV and no overall linear SR-WBV influence across days of training emerged. Instead, such a linear decrease of musculoskeletal pain across days of SR-WBV was restricted to those participants who reported to have more frequent low back pain prior to SB-WBV. Thus, the three-way interaction between prior low back pain, SR-WBV, and days of training was significant (p < 0.001). In accordance with Hypothesis 3, Fig. 2 shows the expected therapeutic linear SR-WBV training effects to appear in those with higher than average levels of low back pain prior to the training, whereas there is no such effect in those who report lower than average levels or absence of low back pain (Fig. 2). Low back pain prior to the start of SB-WBV did not moderate linear SR-WBV training effects in musculoskeletal well-being and surefootedness.
Table 3.
Prediction of daily musculoskeletal well-being, musculoskeletal pain, and surefootedness in multilevel regression analyses
| Musculoskeletal well-being |
Pain |
Surefootedness |
||||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| Constant | 8.394 | 0.668 | 2.508 | 0.450 | 9.535 | 0.549 |
| Sex | −0.008 | 0.552 | −0.328 | 0.372 | −0.495 | 0.455 |
| BMI | 0.008 | 0.075 | 0.021 | 0.051 | −0.045 | 0.062 |
| Age | 0.005 | 0.018 | 0.001 | 0.012 | −0.006 | 0.015 |
| LBP | −0.230 | 0.160 | 0.302† | 0.110 | −0.109 | 0.128 |
| SR-WBV | 0.218* | 0.087 | −0.063 | 0.072 | 0.203‡ | 0.051 |
| Day | 0.016‡ | 0.004 | −0.005 | 0.003 | 0.001 | 0.002 |
| Interaction effects | ||||||
| Day × Training | 0.016† | 0.006 | 0.002 | 0.005 | 0.013† | 0.003 |
| Training × LBP | 0.176† | 0.074 | −0.102 | 0.061 | −0.026 | 0.043 |
| Day × LBP | 0.000 | 0.003 | 0.000 | 0.003 | 0.001 | 0.002 |
| Training × Day × LBP | −0.002 | 0.005 | −0.010** | 0.004 | −0.001 | 0.003 |
*p < 0.05.
†p < 0.01.
‡p < 0.001, two-tailed.
n = 3,324 daily pain ratings reported by 54 participants during 56 days.
Sex (0 = m, 1 = f), B, fixed parameter estimates of unstandardized regression coefficients; BMI, body mass index; CTSIB, clinical test of sensory integration on balance; Day, day of training period (1-28); LBP, frequency of low back pain during last 6 months prior to the study started; Pain, self-reported musculoskeletal pain on first day of the study; SE, standard error in unstandardized regression coefficients estimation. Significance levels were calculated by t-values (Parameter Estimate/SE) with j-p-1 degrees of freedom, where j is the number of units on level 2 and p is the number of explanatory variables; SR-WBV, Stochastic resonance whole-body vibration training (0 = control group, 1 = training group); surefootedness, self-reported perceived body balance on first day of the study.
Fig. 2.
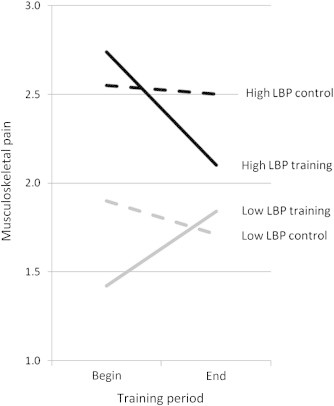
Effect of stochastic resonance whole-body vibration training (SR-WBV) condition on daily musculoskeletal pain in participants with higher levels of low back pain (LBP) prior to SR-WBV and lower levels of LBP prior to SR-WBV.
3.2. SR-WBV training affects body balance
In the CTSIB, all participants were able to maintain the position for a considerable time. Times ranged between 20 seconds and 30 seconds with many individuals reaching the 30-second mark. Thus, in measurements prior to SR-WBV and after 4 weeks of SR-WBV the distribution of data was highly skewed and nonparametric Wilcoxon test of change was used, showing that performance significantly increased after SR-WBV (Wilcoxon Z = –4.68, p < 0.001).
4. Discussion
To date, SR-WBV has been used in training contexts, e.g., in healthy students [33], athletes and 60 to 70 year old individuals [20,21], and in patients [15]. To our knowledge there is only one study on SR-WBV in occupational settings [16]. The current study showed that SR-WBV was related to increased musculoskeletal well-being and reduced musculoskeletal pain in those with low back pain. Moreover, SR-WBV corresponded better to reported surefootedness/sense of balance and also better balance performance in a standardized behavioural test. Surefootedness/sense of balance and the ability to stand in tandem position as part of the behavioral test used in this study were both shown to be reliable predictors of falls in the future [34]. Thus, SR-WBV can be suggested as beneficial in prevention not only of occupational MSC including low back pain, but also for falls at work. Considering overall usefulness, SR-WBV appeared to be more related to increased musculoskeletal well-being than to reduced musculoskeletal pain. Results are in accordance with other studies on worksite activity trainings to reduce MSC in office work [35]. SR-WBV effects on muculoskeletal pain, however, also deserved a deeper analysis that tested whether SR-WBV was linked to reduced pain in those who suffered from musculoskeletal pain prior to training whereas those who were pain free benefited less.
The overall results of SR-WBV in white-collar employees doing office work (mainly working with video display units) in predominantly sitting positions replicates findings of SR-WBV in blue-collar workers in a metal manufacturing company [16]. This finding suggests that whether or not biomechanical loads contribute to muscular complaints, SR-WBV is potentially useful. In other words, SR-WBV effectiveness seems not to be restricted to MSC that arise primarily from biomechanical strain. Studies that compared MSC in nurses who experienced considerable biomechanical loads and office workers found no evidence of different mechanisms leading to nonspecific, recurrent low back pain in the two occupations [1,36]. With respect to sedentary work, studies indicate that sitting is no worse than standing for low back pain incidence [37]. Sitting is not associated with increased pressure to spinal discs. If sitting is a greater threat for the development of low back pain than standing, the mechanism is unlikely to be raised pressure to spinal discs [37]. Physiologically, the advantages of SR-WBV hypothetically arise from large acceleration levels that can still be controlled, from the transfer of mechanical energy to the human body, from the large number of repetitive cycles within short periods of time, and from the specific effects deployed via muscle spindles and mechanoreceptors [11]. More research is needed to clarify the physiological processes behind SR-WBV related changes, especially the gain in body balance. One promising working assumption is that stochastic vibrations improve information from the periphery of the sensory system by lowering sensory thresholds in neurons located in various joints [13]. Muscles need this neuronal input to regulate force in order to stay upright.
SR-WBV has to be differentiated from the normal vibration encountered in daily life as the exposure to such vibration has been detected as being able to be deleterious [38]. Negative effects of vibration at work are caused due to chronic exposure—with long exposure and short rest cycles—with rather regular vibration that is often oscillating at large amplitude or at frequencies of mechanical resonance [21]. SR-WBV may have risks and benefits and both should be studied. A review of 112 studies on whole body vibration reported very few side effects (0.00120% of training trials and 0.00069% of training trials that used SRWBV) [14]. More serious side effects have been exclusively found in studies using sinusoidal whole body vibration but not in studies using SR-WBV. SR-WBV seems to be a safe training intervention with usually harmless adverse effects when a careful evaluation of the medical history is done prior to SR-WBV to evaluate contraindications or potential risk factors of the participants. In addition, one should avoid unnecessarily large exposures to keep the risk of side effects as low as possible. Therefore, we did the 60-second training, the shortest period known to have a training effect.
An advantage of the study is that no attrition across 56 days was observed and participants also reported no side effects of SR-WBV. Compliance presumably was maintained by the easy training procedure that afforded no change of clothes or change of location and did not last more than 10 minutes.
The limitations are typical for intense worksite training studies. The sample size is moderate and replication with a larger sample is desirable. Participation rate was also moderate and bias cannot be excluded here. Participants in the next study should be: (1) randomly selected out of the entire sample of employees, and (2) randomly assigned to the training condition and control condition. Additionally, all but one measure were based on questionnaires, which can be subject to a range of biases. Another point of limitation is that participants were blinded with respect to training condition. Participants may be biased due to their belief about the training effect.
To our knowledge, this is the first study examining SR-WBV in employees doing office work. This study indicates that SR-WBV may help to reduce musculoskeletal pain in those who suffer from low back pain Moreover, SR-WBV is likely to increase the sense of balance and body balance performance in a standardized test. SR-WBV was shown to be an economic exercise that requires very little effort in terms of infrastructure, time, and effort from participants. SR-WBV during work may help to prevent occupational low back pain and falls at work.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgments
The research reported in this article was supported by a grant from the Swiss National Accident Insurance Fund (SUVA, Project 100163) to A. Elfering, V.Schade, and L. Radlinger.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Coggon D.G., Ntani G., Palmer K.T., Felli V.E., Harari R., Barrero L.H., Felknor S.A., Gimeno D., Cattrell A., Serra C., Bonzini M., Solidaki E., Merisalu E., Habib R.R., Sadeghian F., Masood Kadir M., Warnakulasuriya S.S., Matsudaira K., Nyantumbu B., Sim M.R., Harcombe H., Cox K., Marziale M.H., Sarquis L.M., Harari F., Freire R., Harari N., Monroy M.V., Quintana L.A., Rojas M., Salazar Vega E.J., Harris E.C., Vargas-Prada S., Martinez J.M., Delclos G., Benavides F.G., Carugno M., Ferrario M.M., Pesatori A.C., Chatzi L., Bitsios P., Kogevinas M., Oha K., Sirk T., Sadeghian A., Peiris-John R.J., Sathiakumar N., Wickremasinghe A.R., Yoshimura N., Kelsall H.L., Hoe V.C., Urquhart D.M., Derrett S., McBride D., Herbison P., Gray A. Disabling musculoskeletal pain in working populations: is it the job, the person, or the culture? Pain. 2013;154:856–863. doi: 10.1016/j.pain.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wieser S., Horisberger B., Schmidhauser S., Eisenring C., Brügger U., Ruckstuhl A., Dietrich J., Mannion A., Elfering A., Tamcan Ö., Müller U. Cost of low back pain in Switzerland in 2005. Eur J Health Econ. 2011;12:455–467. doi: 10.1007/s10198-010-0258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elfering A. Work-related outcome assessment instruments. Eur Spine J. 2006;15(Suppl. 1):S32–S43. doi: 10.1007/s00586-005-1047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Waddell G., Burton A.K. Concepts of rehabilitation for the management of low back pain. Bailliere Clin Rheumatol. 2005;19:655–670. doi: 10.1016/j.berh.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Norberg M., Danuser B., Klipstein A., Läubli T., Jeanrenaud C. Interdisciplinary intervention strategy for chronic MSDS. J Bone Joint Surg Br. 2009;91(Suppl. 1):S151. [Google Scholar]
- 6.Kaewthummanukul T., Brown K.C. Determinants of employee participation in physical activity: critical review of the literature. AAOHN J. 2006;54:249–261. doi: 10.1177/216507990605400602. [DOI] [PubMed] [Google Scholar]
- 7.Robroek S.J.W., van Lenthe F.J., van Empelen P., Burdorf A. Determinants of participation in worksite health promotion programmes: a systematic review. IJBNPA. 2009;6:26. doi: 10.1186/1479-5868-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lechner L., de Vries H., Adriaansen S., Drabbels L. Effects of an employee fitness program on reduced absenteeism. J Occup Environ Med. 1997;39:827–831. doi: 10.1097/00043764-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Haas C.T., Turbanski S., Kessler K., Schmidtbleicher D. The effects of random whole-body-vibration on motor symptoms in Parkinson's disease. NeuroRehabilitation. 2006;21:29–36. [PubMed] [Google Scholar]
- 10.Ross S.E., Arnold B.L., Blackburn J.T., Brown C.N., Guskiewicz K.M. Enhanced balance associated with coordination training with stochastic resonance stimulation in subjects with functional ankle instability: an experimental trial. J Neuroeng Rehab. 2007;4:47. doi: 10.1186/1743-0003-4-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rittweger J. Vibration as an exercise modality: how it may work, and what its potential might be. Eur J Appl Physiol. 2010;108:877–904. doi: 10.1007/s00421-009-1303-3. [DOI] [PubMed] [Google Scholar]
- 12.Lauper M., Kuhn A., Gerber R., Luginbuhl H., Radlinger L. Pelvic floor stimulation: What are the good vibrations? Neurourol Urodyn. 2009;28:405–410. doi: 10.1002/nau.20669. [DOI] [PubMed] [Google Scholar]
- 13.Moss F., Milton J.G. Medical technology: Balancing the unbalanced. Nature. 2003;425:911–912. doi: 10.1038/425911a. [DOI] [PubMed] [Google Scholar]
- 14.Herren K., Radlinger L. Risks and side-effects of whole-body vibration training. Special Interest Report Poster WCPT Congress Amsterdam 2011 (Number: SI-PO-201-21-Tue) Physiotherapy. 2011;97(Suppl. S1) [Google Scholar]
- 15.Pang M.Y.C. Whole-body vibration therapy in fracture prevention among adults with chronic disease. World J Orthop. 2010;1:20–25. doi: 10.5312/wjo.v1.i1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burger C., Schade V., Lindner C., Radlinger L., Elfering A. Stochastic resonance training reduces musculoskeletal symptoms in metal manufacturing workers: a controlled preventive intervention study. Work. 2012;42:269–278. doi: 10.3233/WOR-2012-1350. [DOI] [PubMed] [Google Scholar]
- 17.Westergaard R.H. Effects of psychological demand and stress on neuromuscular function. In: Moon S.D., Sauter S.L., editors. Beyond biomechanics: psychosocial aspects of musculoskeletal disorders in office work. Taylor & Francis; London (UK): 1996. pp. 75–89. [Google Scholar]
- 18.Torvinen S., Kannus P., Sievanen H., Jarvinen T.A., Pasanen M., Kontulainen S., Järvinen T.L., Järvinen M., Oja P., Vuori I. Effect of a vibration exposure on muscular performance and body balance: a randomized cross-over study. Clin Physiol Funct Imaging. 2002;22:145–153. doi: 10.1046/j.1365-2281.2002.00410.x. [DOI] [PubMed] [Google Scholar]
- 19.Cochrane D.J. Vibration exercise: the potential benefits. Int J Sports Med. 2011;32:75–99. doi: 10.1055/s-0030-1268010. [DOI] [PubMed] [Google Scholar]
- 20.Verschueren S.M., Roelants M., Delecluse C., Swinnen S., Vanderschueren D., Boonen S. Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. J Bone Miner Res. 2004;19:352–359. doi: 10.1359/JBMR.0301245. [DOI] [PubMed] [Google Scholar]
- 21.Haas C.T. Vibrationstraining, biomechanische stimulation und stochastische resonanz therapie [Vibration training, biomechanical stimulation and stochastic resonance therapy] Zeitschrift für Physiotherapeuten. 2008;7:728–789. [in German] [Google Scholar]
- 22.Yaremko R.M., Harari H., Harrison R.C., Lynn E. Harper & Row; New York (NY): 1982. Reference handbook on research and statistical methods in psychology; p. 335. [Google Scholar]
- 23.Kuorinka I., Jonsson B., Kilbom A., Vinterberg H., Biering-Sørensen F., Andersson G., Jorgensen K. Standardised Nordic questionnaire for the analysis of musculoskeletal symptoms. Appl Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 24.Klasen B.W., Hallner D., Schaub C., Willburger R., Hasenbring M. Validation and reliability of the German version of the chronic pain grade questionnaire in primary care back pain patients. Psychosoc Med. 2004;1 Doc07. [PMC free article] [PubMed] [Google Scholar]
- 25.Haefeli M., Elfering A. Pain assessment. Eur Spine J. 2006;15:17–24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shumway-Cook A., Horak F.B. Assessing the influence of sensory interaction on balance. Suggestion from the field. Phys Ther. 1986;66:1548–1550. doi: 10.1093/ptj/66.10.1548. [DOI] [PubMed] [Google Scholar]
- 27.Cohen H., Blatchly C.A., Gombash L.L. A study of the clinical test of sensory interaction and balance. Phys Ther. 1993;73:346–351. doi: 10.1093/ptj/73.6.346. [DOI] [PubMed] [Google Scholar]
- 28.El-Kashlan H.K., Shepard N.T., Asher A.M., Smith-Wheelock M., Telian S.A. Evaluation of clinical measures of equilibrium. Laryngoscope. 1998;108:311–319. doi: 10.1097/00005537-199803000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Hox J. Lawrence Erlbaum Associates; Mahwah (NJ): 2002. Multilevel analysis: techniques and applications; p. 382. [Google Scholar]
- 30.Rasbash J., Steele F., Browne W., Prosser B. University of Bristol; Centre for Multilevel Modelling: 2005. A user's guide to MLwiN; p. 256. [Google Scholar]
- 31.Maas C.J., Hox J.J. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:86–92. [Google Scholar]
- 32.Singer J.D., Willett J.B. Oxford University Press; New York (NY): 2003. Applied longitudinal data analysis: modeling change and event occurrence; p. 644. [Google Scholar]
- 33.Elfering A., Thomann J., Schade V., Radlinger L. Stochastic resonance whole body vibration reduces musculoskeletal pain: a randomized controlled trial. World J Orthop. 2011;2:116–120. doi: 10.5312/wjo.v2.i12.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ganz D.A., Bao Y., Shekelle P.G., Rubenstein L.Z. Will my patient fall? JAMA. 2007;297:77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 35.Ketola R., Toivonen R., Häkkänen M., Luukkonen R., Takala E.-P., Viikari-Juntura E. Effects of ergonomic intervention in work with video display units. Scand J Work Environ Health. 2002;28:18–24. doi: 10.5271/sjweh.642. [DOI] [PubMed] [Google Scholar]
- 36.Schenk P., Laubli T., Hodler J., Klipstein A. Symptomatology of recurrent low back pain in nursing and administrative professions. Eur Spine J. 2007;16:1789–1798. doi: 10.1007/s00586-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Claus A., Hides J., Moseley L., Hodges P. Sitting versus standing: Does the intradiscal pressure cause disc degeneration or low back pain? J Electromyogr Kinesiol. 2008;18:550–558. doi: 10.1016/j.jelekin.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 38.Griffin M.J. Academic Press; San Diego (CA): 1996. Handbook of human vibration. [Google Scholar]


