Abstract
Background
The Post-operative Morbidity Index (PMI) is a quantitative utility measure of a complication burden created by severity weighting. The Fistula Risk Score (FRS) is a validated model that predicts whether a patient will develop a post-operative pancreatic fistula (POPF). These novel tools might provide further discrimination of the ISGPF grading system.
Methods
From 2001 to 2012, 1021 pancreaticoduodenectomies were performed at four institutions. POPFs were categorized by ISGPF standards. PMI scores were calculated based on the Modified Accordion Severity Grading System. FRS scores were assigned according to the relative influence of four recognized factors for developing a clinically relevant POPF (CR-POPF).
Results
In total, 231 patients (22.6%) developed a POPF, of which 54.1% were CR-POPFs. The PMI differed significantly between the ISGPF grades and patients with no or non-fistulous complications (P < 0.001). 64.9% of POPFs and 84.0% of CR-POPFs contributed the highest Accordion grade to the PMI. Overall, the FRS correlated well with PMI (R2 = 0.81, P < 0.001).
Conclusion
These data quantitatively reinforce the ISGPF grades that were developed qualitatively around the concept of clinical severity. CR-POPFs usually reflect the patient's highest Accordion score whereas biochemical POPFs are often superseded. The correlation between FRS and PMI indicates that risk factors for a fistula contribute to overall pancreaticoduodenectomy morbidity.
Introduction
A post-operative pancreatic fistula (POPF) is considered one of most foreboding complications after a pancreatic resection. This morbid problem has previously been shown to contribute to the development of other complications and significant mortality.1,2 To develop a common system of classifying POPF, the International Study Group on Pancreatic Fistula (ISGPF) designed a new and universal set of standards to reconcile the myriad of preexisting definitions.3,4 The result was a comprehensive description of a pancreatic fistula and a system of grading for POPF based on severity of the clinical impact on the patient. Predicated on evidence of fluid containing elevated amylase activity, POPFs are classified as grade A (least severe, biochemical fistulae) or grades B and C, which have a greater clinical impact – also referred to as clinically relevant post-operative pancreatic fistula (CR-POPF). These grades have been qualitatively validated and generally globally accepted as proper nomenclature for POPF severity.5,6 However, like other post-operative complications to date, POPF suffer from the inability to be compared quantitatively.
The Post-operative Morbidity Index (PMI) is a measure of complication burden.7 This system features utility weighting scores which operate continuously from 0 to 1 to quantitatively relate the clinical significance and duration of outcomes. A PMI for post-operative complications is predicated upon the Modified Accordion Severity Grading System, an extension of the T92 and Clavien–Dindo scales which assess the clinical impact of a patient's post-operative course based on the therapeutics and resources used to manage it.8–11 The Accordion system assigns each patient a grade from zero to six based on the severity of their complication profile. Derived by expert opinion, each Accordion grade has been assigned a numeric value (weight) that reflects its relative burden on the utility scale. The aggregate of these values determines the PMI for any given population studied (e.g. complications, surgical procedures and institutions), which can then be used in a comparative fashion. The first application of a PMI utilized the rigorous standards of the ACS NSQIP database to accrue complications.12 However, in theory the PMI can be derived from any practice or institutional complication database.
The Fistula Risk Score (FRS) is a prospectively validated model that strongly predicts whether a patient will develop a CR-POPF after a pancreaticoduodenectomy (PD).13 This scale is based upon four discrete risk factors for CR-POPF previously identified in the context of the ISGPF framework.7,14,15 These variables include small pancreatic duct size, soft gland texture, high-risk pathology (any pathology exclusive of pancreatic cancer or chronic pancreatitis) and increased blood loss. The FRS is a 10-point scale that relies on the relative influence of these four variables and has been shown to effectively predict CR-POPF development and its sequelae. While pre-operative risk assessments for POPF rarely rule out patients needing a resection, or reroute the course of post-operative care, the FRS can be calculated at the point of pancreatic anastomotic creation and therefore be utilized to tailor intra- and post-operative management of this morbid complication.13–15
Both the ISGPF grading system and the FRS prediction tool have been qualitatively validated but have yet to be scrutinized quantitatively. Using the experience in PD at four high-volume North American pancreatic specialty centres, the present study aims to use the PMI as a tool to: (i) quantitatively determine the soundness of the ISGPF framework of tiered severity; and (ii) show the relationship between risk of CR-POPF (as determined by the FRS) and its subsequent morbidity burden.
Methods
This study was approved by the Institutional Review Board (IRB) at the Hospital of the University of Pennsylvania (HUP). Patients were identified from four IRB-approved, prospectively accrued, retrospectively reviewed pancreatic surgery databases from HUP, Beth Israel Deaconess Medical Center (BIDMC) in Boston, the University of Alabama at Birmingham (UAB) and the Baptist Memorial Hospital, The University of Tennessee Health Science Center, Memphis (UTHSC). Six pancreatic surgical specialists performed pancreaticoduodenectomies with duct-to-mucosa pancreatojejunostomy for all surgical indications between 2001 and 2012. Alternative methods of ductal management (i.e. pancreatogastrostomy; duct occlusion) were excluded.
Post-operative complications within 90 days were accrued for each patient by clinical research associates according to definitions set forth in our previous work.5,7 and were then graded according to the six-point Modified Accordion Severity Grading System.10 Grades were assigned by, or under the supervision of, attending surgeons with complication severity grading expertise. These scores ranged from zero to six with a zero indicating no complications and a six indicating post-operative death directly as a result of a complication of the resection (Table 1). Patients were assigned a single Accordion grade even if they suffered numerous complications. In such an event, only the complication type leading to the patient's overall highest Accordion grade was used for calculations. Complications were separated into two categories (pancreatic fistulous complications and non-fistulous complications) and analysed both together and separately.
Table 1.
The Modified Accordion Grading System and associated severity weighting
| Grade | Description | Severity weight |
|---|---|---|
| 0 | No complications | 0.000 |
| 1 | Treatment of complication requires only minor invasive procedures that can be done at the bedside, such as insertion of intravenous lines, urinary catheters, and nasogastric tubes, and drainage of wound infections. Physiotherapy and antiemetics, antipyretics, analgesics, diuretics, electrolytes, and physiotherapy are permitted. | 0.110 |
| 2 | Complication requires pharmacologic treatment with drugs other than such allowed for minor complications, e.g. antibiotics. Blood transfusions and total parenteral nutrition are also included. | 0.260 |
| 3 | No general anaesthesia is required to treat the complication: requires management by an endoscopic,interventional procedure, or reoperation without general anaesthesia. | 0.370 |
| 4 | General anaesthesia is required to treat complication. Alternately, single-organ failure has developed. | 0.600 |
| 5 | General anaesthesia is required to treat complication and single organ failure has developed. Alternately, multisystem organ failure (2 or more organ systems) has developed. | 0.790 |
| 6 | Post-operative death occurred. | 1.000 |
Modified from Pembroke et al. JACS, 2010.
When a complication was determined to be a POPF, it was first categorized using the guidelines set forth by the ISGPF based on the clinical effect of the POPF; they are grade A (biochemical fistula), or grades B and C (CR-POPF).4 Each previously defined POPF was then assigned a POPF-specific Accordion grade regardless of whether the POPF denoted the highest grade complication for the patient or not. These particular grades were derived using a logical matching process between the ISGPF categorization standards and six levels of clinical impact defined in the Accordion grading system. Using these criteria there are only certain possibilities of Accordion levels for each grade of POPF. Grade A POPFs can only be an Accordion grade 0 or 1 (denoting operative drain presence at discharge); grade B CR-POPFs are only comprised of Accordion grades 1 (prolonged drainage – in this case beyond three weeks), 2 (therapeutic medications applied) and 3 (usually percutaneous drainage); grade C CR-POPFs include only Accordion grades 4 (usually re-operations), 5 (usually multi-organ failure) and 6 (death from a fistula). It is important to note that while these are the only possible grades directly as a result of a POPF, a patient with a POPF may have a higher overall Accordion grade owing to other, more severe complications. Thus, each patient who manifests a POPF would have a POPF-specific grade as well as an overall severity grade, which might be higher, lower, or equivalent.
PMI scores reflect the average of the weighted Accordion scores of any particular group and can possibly range from 0 to 1.00 continuously. These scores were calculated based on the protocol similar to that used to derive in the first descriptions of the PMI.8–12,16 Under these guidelines each Accordion grade is granted a specific quantified value (Table 1). These individual weighted Accordion scores were then summed to create a total severity burden score, and then divided by the number of patients to calculate the aggregate PMI.
The risk factors for development of CR-POPF necessary to determine the FRS (small duct size, soft pancreas texture, high-risk pathology and increased blood loss) were accrued from the individual databases of the four institutions as described by the attending surgeon in their operative note. These were then assigned discrete numerical values based on a predetermined weighting system that is summarized in Table 2. FRS scores were then tabulated by summing the numerical value contributed by each individual risk factor and could range from zero (no risk) to 10 (maximum risk). FRS scores were then further grouped into four possible risk zones for more practical utilization. These categories are Negligible Risk (0 points), Low Risk (1–2 points), Moderate Risk (3–6 points) and High Risk (7–10 points).
Table 2.
Fistula Risk Score for prediction of clinically-relevant pancreatic fistula (CR-POPF) after a pancreatoduodenectomy
| Risk factor | Parameter | Points |
|---|---|---|
| Gland texture | Firm | 0 |
| Soft | 2 | |
| Pathology | Pancreatic adenocarcinoma or pancreatitis | 0 |
| Ampullary, duodenal, cystic, islet cell | 1 | |
| Pancreatic duct diameter | ≥5 mm | 0 |
| 4 mm | 1 | |
| 3 mm | 2 | |
| 2 mm | 3 | |
| ≤1 mm | 4 | |
| Intra-operative blood loss | ≤400 ml | 0 |
| 401–700 ml | 1 | |
| 701–1,000 ml | 2 | |
| >1,000 ml | 3 | |
| Total 0 to 10 points | ||
From Callery et al. JACS, 2013.
Statistical analyses were performed using IBM SPSS, version 20 (SPSS Inc., Chicago, IL, USA). Qualitative and descriptive statistics were tabulated and analysed to determine rates of complications. Differences between ISPGF groups, FRS groups and PMI were scrutinized using analysis of variance (anova) and paired t-tests. All tests were considered significant at P < 0.05.
Results
In total, 1021 patients underwent a PD with P-J reconstruction at four institutions (N = 444, 306, 136 and 135). Out of these patients, 231 (22.6%) developed any sort of POPF (ISGPF grades A, B or C); 125 (54.1%) of these were clinically relevant, equating to 12.2% of the total cohort. A grade A (biochemical) fistula occurred in 106 patients (10.4%), whereas 101 patients (9.8%) developed a grade B fistula and 24 patients (2.4%) suffered a grade C fistula. Beyond POPFs, 424 other patients (41.5%) developed a complication which was not attributed to a pancreatic fistula and 367 patients (35.9%) incurred no complication of any kind. There were 28 deaths in the series (2.7%), of which 7 were directly attributable to a POPF (0.7%). Malignancy or chronic pancreatitis was the indication for surgery in 54.6% of the patients.
As Table 3 illustrates, the PMI for the entire series of PDs was 0.211. By definition, the cohort of patients who developed no complications has a PMI of 0.000. Overall, the PMI for the patients who developed any sort of POPF was lower than the PMI for the patients who developed a CR-POPF. The PMI value escalated steadily across the progression of ISGPF grades up to a high of 0.780 for the most severe Grade C fistulae. Patients who suffered a complication exclusive of a fistula had an overall PMI approximately equal to the overall PMI of POPF. The PMI differed significantly between the individual ISGPF grades, A, B, and C, and patients with no complications or non-fistulous complications (P < 0.001 for all comparisons; Fig. 1). Figure 2 illustrates how patients who developed either a POPF, or any other complication, displayed unique spectrums of Accordion grades.
Table 3.
Patient outcomes grouped by complication category
| Patient complication profile | N (% of total) | PMI value | PMI value when Accordion grade of fistula is highest (POPF-specific PMI) | Contribution of fistulas to highest severity score N (% contribution) |
|---|---|---|---|---|
| No complications | 367 (35.9) | 0.00 | NA | NA |
| Non-fistulous Complications | 424 (41.5) | 0.323 | NA | NA |
| All POPFs | 231 (22.6) | 0.341 | 0.320 | 150 (64.9) |
| ISGPF Grade A | 106 (10.4) | 0.208 | 0.032 | 45 (42.5) |
| CR-POPF | 125 (12.2) | 0.453 | 0.357 | 105 (84.0) |
| ISGPF Grade B | 101 (9.8) | 0.375 | 0.257 | 81 (80.2) |
| ISGPF Grade C | 24 (2.4) | 0.780 | 0.780 | 24 (100) |
| All patients | 1021 (100) | 0.211 | 0.055 | 150 (14.7) |
PMI, Post-operative Morbidity Index; POPF, post-operative pancreatic fistula; CR-POPF, clinically relevant ISGPF, International Study Group Pancreatic Fistula; NA, not applicable.
Figure 1.
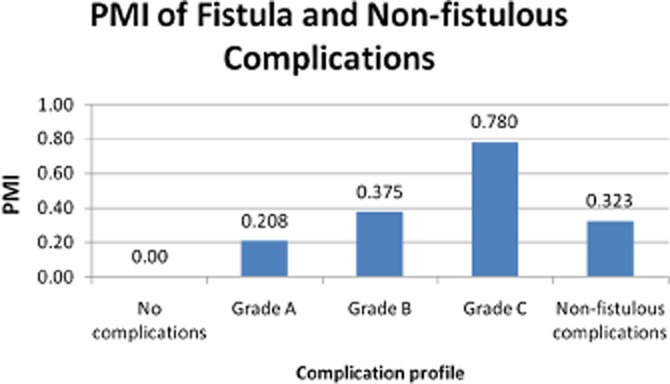
Post-operative Morbidity Index (PMI) of fistula and non-fistulous complications. The difference between all separate comparisons was significant at P < 0.001
Figure 2.
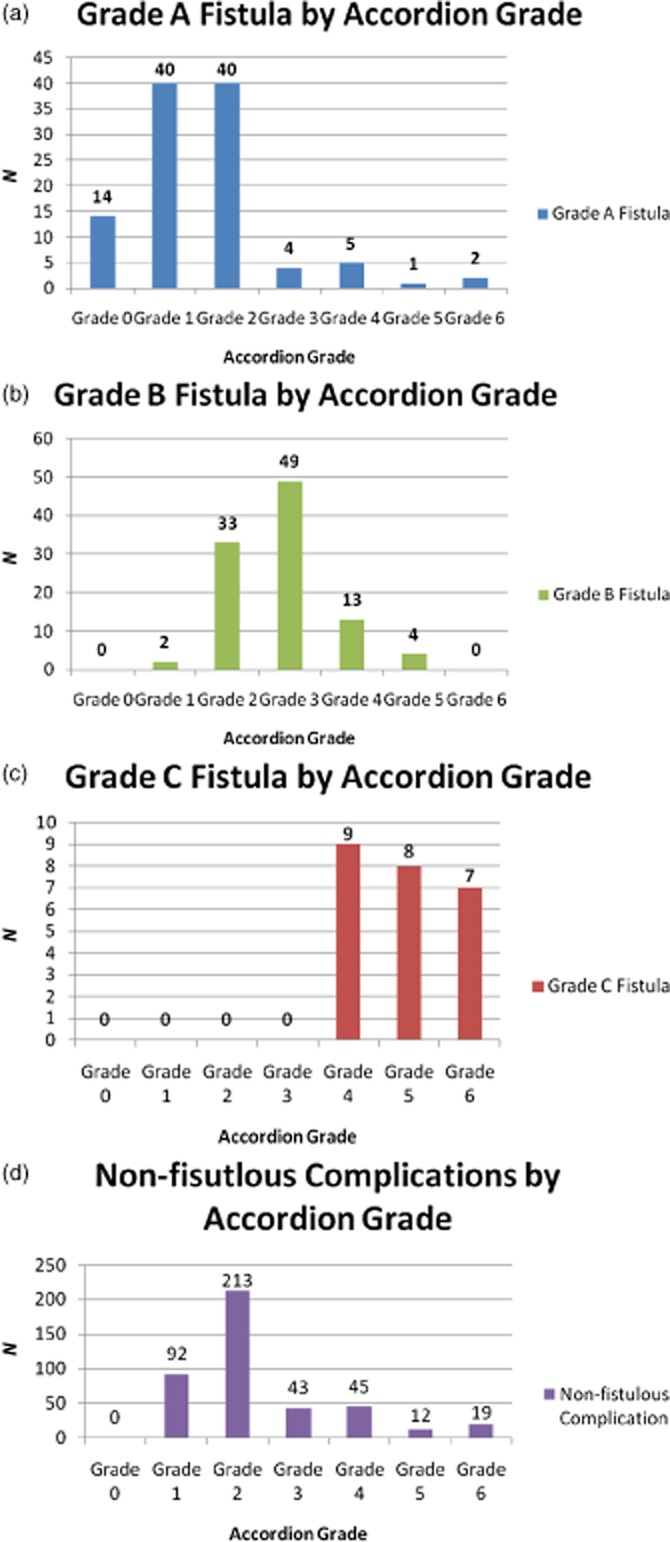
(a) Grade A fistula by Accordion grade. (b) Grade B fistula by Accordion grade. (c) Grade C fistula by Accordion grade. (d) Non-fistulous complications by Accordion grade. Overall frequency of accordion grades by complication category
When looking specifically at the contribution of the fistula to each ISGPF grade's PMI, grade A fistulae had the lowest PMI on account of the fistula alone and the fistula provided the highest Accordion value to the PMI less than half of the time (Table 3). The PMI rose for the 101 patients with a grade B fistula, and was the most severe complication by Accordion grade most of the time. Grade C fistulae had the highest PMI and provided the highest Accordion grade to the overall PMI of that particular cohort every time. Overall, in 64.9% of POPFs the fistula accounted for the patient's highest Accordion grade to the PMI calculation. However, this contribution rose to 84.0% when considering CR-POPFs exclusively.
Accordion grades (attributed specifically to fistula) distinctly segregated for the various ISGPF grades. The 106 patients with a Grade A POPF were composed nearly equally of Accordion 0 and Accordion 1 severity grades. For patients who developed Grade B POPFs, just 5.0% were Accordion 1 (representing the clinical scenario of prolonged drainage beyond 3 weeks), whereas 40.6% were Accordion 2. However, the majority reflected the need for a non-operative intervention (Accordion 3). The composition of Grade C fistulae was distributed equally between Accordion classes 4, 5, and 6 indicating a reoperation, organ failure or death occurred. In terms of pathology, high-risk pathology (anything exclusive of pancreatic cancer and clinical pancreatitis) prevailed both in POPFs overall and in CR-POPFs (65.4% and 72.8%, respectively). The opposite is true in those whom had no complications or only non-fistulous complications; the majority of these post-operative courses were in patients with pancreatic cancer or clinical pancreatitis (both 60.4% of the time).
Overall, POPFs occurred 22.6% of the time and, when they were the highest Accordion grade, they contributed 22.4% of the burden to the PMI (severity weight: 48.06 out of 214.98 total). While the frequency and burden of POPFs were almost identical, it is evident that CR-POPFs contribute disproportionately to that overall severity burden of 22.4%. Grade A POPFs accounted for 46% of POPFs by frequency but provided only 7% of the POPF burden. Analogously, the 54% of POPFs that were clinically relevant provided 93% of the burden contributed by POPF (Fig. 3). A focused analysis of the serious Accordion Grades 4, 5 and 6 complications shows that for the overall series these occurred in 125 patients (12.2%). The contribution of POPFs to these serious complications only comes through ISGPF Grade C patients (N = 24) as there are no Grade 4 or higher complications in patients with ISGPF A and B POPFs. Therefore this 2.3% of patients in the overall series contributed 19.2% of all the serious complications encountered.
Figure 3.
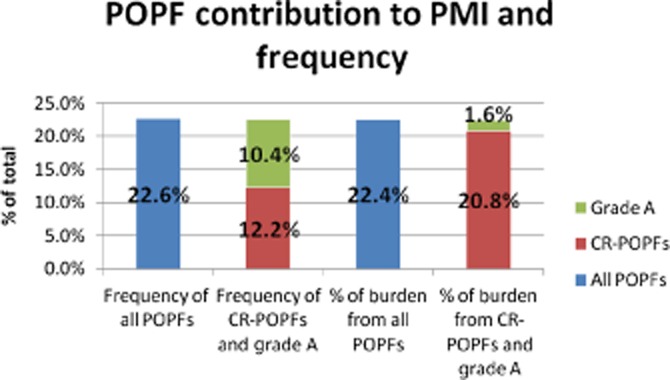
Post-operative pancreatic fistula (POPF) contribution to the Post-operative Morbidity Index (PMI) and frequency
There were 135 (13.2%) patients in the Negligible Risk group, 301 (29.5%) in the Low Risk group, 512 (50.1%) in the Moderate Risk group and 73 (7.2%) in the High Risk group of the FRS. Figure 4 shows that the FRS correlated well with the overall PMI reflecting all complications encountered (R2 = 0.81, P < 0.001), as well as the PMI only attributed to a fistula (R2 = 0.77, P < 0.001). On the other hand, the FRS did not associate with the PMI of non-fistulous complications (R2 = 0.4354, P = 0.045).
Figure 4.
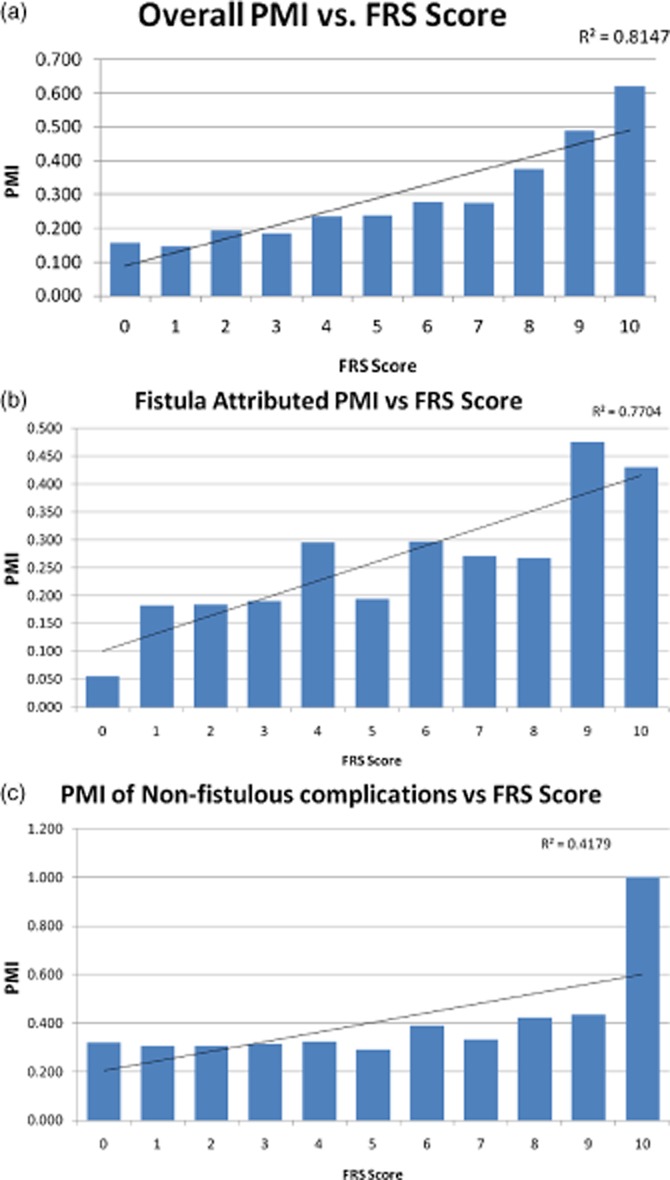
(a) Overall Post-operative Morbidity Index (PMI) compared with the Fistula Risk Score FRS score. (b) Fistula attributed PMI compared with the FRS score. (c) PMI of non-fistulous complications compared with the FRS score
Discussion
Classification and management of post-operative complications remains a challenge even with today's more sophisticated outcome reporting metrics. A clear advancement in complication analysis occurred with the advent of qualitative severity grading systems predicated on assessing the resources used to treat any given adverse event.8–10,16,17 The concept of ‘burden’ has its basis in the realization that a complication can manifest as a full spectrum of clinical effects.11 Any particular occurrence of a given complication may not register the same effect on different patients. Even in the face of a globally accepted, comprehensive, stratification system such as the ISGPF guidelines, it is difficult to quantitatively discern the difference in POPFs. This study attempts to address this dilemma using the PMI, and is the first to apply such an analysis to a specific surgical complication.
The PMI is a natural extension of the T92, Clavien–Dindo and Accordion progression of complication severity grading.8–12 Although these scales accurately categorize complications into severity strata, they fail to highlight the true impact imposed by severe complications on the collective study population. The original description of the PMI, based on data acquired from ACS-NSQIP, was the first process to take these severity grades and normalize them to accurately represent clinical burden of various complications.11,12 A pancreatic fistula and its sequelae, however, are not currently accrued by ACS-NSQIP. For this reason, the PMI presented herein uses the previous work as a conceptual foundation. Instead this study stems from comprehensive practice databases accrued by pancreatic surgical specialists with familiarity with severity grading.
This study demonstrates the capability to compare different groups (in this case, grades of POPF) using severity weighted utility scores. Severity weighting is important because it more appropriately accounts for high grade complications that, while they may be infrequent, add considerably to the overall clinical burden (PMI). The use of the PMI as an index is also important. No single patient has their own PMI rather they are assigned an individual severity weight that reflects the complication with the highest impact on them. The aggregate of each weighted Accordion score across the particular population studied creates an index much in the way the Dow-Jones Index is comprised of many different stocks. This collective indexing allows comparison not between individual patients, but between whole cohorts, or subsets, of patients. This study embodies the power of such an index by better discerning the different grades of POPF defined by the ISGPF.
The statistically significant difference between the PMIs of the various ISGPF grades establishes quantitative levels for the clinical burden of these fistulae. This serves to reinforce the grades that were originally developed qualitatively around the concept of clinical severity.4 To date, the ISGPF guidelines have been independently validated by comparing them to outcome metrics such as length of stay, readmission rates and costs.5,6 While the additive burden of POPF may be intuitive, as in the original qualitative segregation, this is the first time that it has been scrutinized by quantitative assessment. ISGPF grades can be difficult to tease apart; even the original classification document includes nuances when appointing these grades.4 Furthermore, no study has been able to accurately identify predictors which would discriminate between the occurrence of Grade B compared with Grade C CR-POPFs.13–15 If the ISGPF guidelines are to continue to be the standard for fistula description, the discrimination between these two groups of CR-POPF becomes increasingly relevant.
These data highlight how Accordion grades may be used to assist a data abstractor in distinguishing between the various types of this morbid problem. According to the ISGPF framework, each grade of POPF appears to be associated with a characteristic and finite set of Accordion grades. This means that even if an abstractor is unclear about the ISGPF grade of a fistula based on its clinical description, a distinction can easily be made based on the Accordion grade associated with the fistulous aspects of the complication. When the overall spectrum of Accordion grades are assessed, grades for biochemical POPF look very similar to those for patients who experienced only non-fistulous complications (Fig. 2a,d). This reinforces what is intuitively known; biochemical fistulae are often superseded by other, more morbid, complications.
However, this study also shows that although easily dismissed, these ‘biochemical only’ Grade A POPFs are not as innocuous as many surgeons believe, but actually do incur an element of burden on patients. By definition an Accordion 0 is simply known as no complication; however 42.9% of the grade A POPFs are graded as Accordion level 0. In the case of fistulae this can actually occur because of their ‘threshold’ definition as a biochemical increase in drain amylase activity of at least 3× normal serum amylase levels. Even if the labs indicate that a leak has developed, if the drain is removed prior to discharge it has no clinical impact on the patient and as such is graded as though no complication occurred at all (Accordion 0). However, over half of the grade A POPFs were graded as Accordion level 1, indicating the continuation of operatively-placed drains upon discharge for elevated amylase values in the post-operative period. These patients otherwise did not demonstrate prolonged drainage (>3 weeks) that would raise them into the Grade B category.4 This form of clinical management increases the POPF-specific PMI for this group to 0.032, and while very low, it is not zero. This indicates that biochemical fistulae do sustain a certain clinical impact on the patient, as well as a potential added cost with commonplace utilization of visiting nurses in these scenarios.
The array of complications changes when looking at grade B and C POPFs, which reside further up the Accordion scale both when looking at fistulous complications only, and when other complications are taken into account (Fig. 2b,c). This indicates that when they develop, CR-POPFs are often the greatest contributor to post-operative complication severity. In this series, this is particularly true of grade C POPFs which are equally distributed between reoperation, organ failure and death. Although only 12.2% of patients developed a CR-POPF, these complications contributed 20.8% to the overall burden used to calculate the PMI. This means that in terms of frequency, CR-POPFs cause almost twice the impact as would be thought simply by looking at their occurrence. It is for this reason that prediction and management of this particular entity is especially important in pancreatic resection surgery.
Figure 4 shows that the strong correlation between the Fistula Risk Score and the overall PMI (as well as the fistula-specific PMI) continues to substantiate this novel prediction tool. This indicates that the four risk factors for CR-POPF that comprise the FRS greatly contribute to overall burden of morbidity in PD. In contrast, they do not seem to influence non-fistulous complications. The FRS was originally designed to predict the development of CR-POPF.13 However, it is these particular fistulae that drive the overall severity of a patient's post-surgical recovery course more than other complications, including biochemical fistulae. In this way the FRS appropriately predicts not only CR-POPF occurrence but, through it, overall morbidity in PD. These variables can be recognized intra-operatively and, as such, the FRS can help decision making at that important point of impact and beyond.
This analysis is limited by the fact that the data were accrued from individual practice databases that, although completed by surgeons with proficiency in complication grading, lack the rigor of the ACS-NSQIP methodology, as used in the original PMI description.12 The advantages of ACS-NSQIP are that complications are gathered by trained reviewers and that each complication is rigorously defined. This reduces variances among observers and improves the quality of data going into an analysis. However, not all practices or institutions, especially outside the United States, partake in the ACS-NSQIP system. Furthermore, pancreas-specific complications (e.g. POPF, delayed gastric emptying and a post-pancreatectomy haemorrhage) are not currently accrued by ACS-NSQIP, that is anticipated to change with the expected implementation of HPB-NSQIP.18 It is very important to emphasize that the methods used to obtain any given PMI need to be explicitly described, so that comparisons between studies are made on an equal footing. In other words, in order to compare PMI amongst studies, it is necessary that complications are identified by similar processes so that the definitions of post-operative complications are the same.
Conclusion
Quantification of complications allows for measurement of the severity of the post-operative course, and furthermore facilitates the ability to perform comparative studies in surgical outcomes. In the present study, PMI is used to reinforce the ISGPF scheme and quantitatively establish a clear clinical impact for each grade of fistula. The study also shows that POPF can result in every Accordion severity level from 0–6 and that ISGPF grades segregate into discrete Accordion profiles. Clinically relevant fistulae usually reflect the patient's highest Accordion score, whereas biochemical POPFs are often superseded by more severe complications. The frequent occurrence of highest-burden CR-POPFs highlights this morbid complication, and begs for a reliable predictive tool to help alleviate their post-operative severity. The FRS provides such a tool, which can not only forecast CR-POPF development, but also the utility burden attributed to this difficult problem.
Conflicts of interest
None declared.
References
- 1.van Berge Henegouwen MI, De Wit LT, Van Gulik TM, Obertop H, Gouma DJ. Incidence, risk factors, and treatment of pancreatic leakage after pancreaticoduodenectomy: drainage versus resection of the pancreatic remnant. J Am Coll Surg. 1997;185:18–24. doi: 10.1016/s1072-7515(97)00007-0. [DOI] [PubMed] [Google Scholar]
- 2.Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000;232:786–795. doi: 10.1097/00000658-200012000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, et al. Pancreatic fistula rate after pancreatic resection: the importance of definitions. Dig Surg. 2004;21:54–59. doi: 10.1159/000075943. [DOI] [PubMed] [Google Scholar]
- 4.Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Pratt WB, Maithel SK, Vanounou T, Huang ZS, Vollmer CM., Jr Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg. 2007;245:443–451. doi: 10.1097/01.sla.0000251708.70219.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang TB, Bai XL, Zheng SS. Pancreatic fistula after pancreaticoduodenectomy: diagnosed according to International Study Group Pancreatic Fistula (ISGPF) definition. Pancreatology. 2007;7:325–331. doi: 10.1159/000105498. [DOI] [PubMed] [Google Scholar]
- 7.Pratt WB, Maithel SK, Vanounou T, Callery MP, Vollmer CM. Postoperative pancreatic fistulas are not equivalent after proximal, distal, and central pancreatectomy. J Gastrointest Surg. 2006;10:1264–1278. doi: 10.1016/j.gassur.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 9.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250:177–186. doi: 10.1097/SLA.0b013e3181afde41. [DOI] [PubMed] [Google Scholar]
- 11.Porembka MR, Hall BL, Hirbe M, Strasberg SM. Quantitative weighting of postoperative complications based on the accordion severity grading system: demonstration of potential impact using the American college of surgeons national surgical quality improvement program. J Am Coll Surg. 2010;210:286–298. doi: 10.1016/j.jamcollsurg.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Strasberg SM, Hall BL. Postoperative morbidity index: a quantitative measure of severity of postoperative complications. J Am Coll Surg. 2011;213:616–626. doi: 10.1016/j.jamcollsurg.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM. A prospectively validated risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013;216:1–14. doi: 10.1016/j.jamcollsurg.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Pratt WB, Callery MP, Vollmer CM. Risk prediction for development of pancreatic fistula using the ISGPF classification scheme. World J Surg. 2008;32:419–428. doi: 10.1007/s00268-007-9388-5. [DOI] [PubMed] [Google Scholar]
- 15.Callery MP, Pratt WB, Vollmer CM. Prevention and management of pancreatic fistula. J Gastrointest Surg. 2009;13:163–173. doi: 10.1007/s11605-008-0534-7. [DOI] [PubMed] [Google Scholar]
- 16.Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–813. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg. 2007;204:356–364. doi: 10.1016/j.jamcollsurg.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Pitt HA, Kilbane M, Strasberg SM, Pawlik TM, Dixon E, Zyromski NJ, et al. ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB. 2009;11:405–413. doi: 10.1111/j.1477-2574.2009.00074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


