Abstract
Employment-contingent health insurance may create incentives for ill workers to remain employed at a sufficient level (usually full-time) to maintain access to health insurance coverage. We study employed married women, comparing the labor supply responses to new breast cancer diagnoses of women dependent on their own employment for health insurance with the responses of women who are less dependent on their own employment for health insurance, because of actual or potential access to health insurance through their spouse’s employer. We find evidence that women who depend on their own job for health insurance reduce their labor supply by less after a diagnosis of breast cancer. In the estimates that best control for unobservables associated with health insurance status, the hours reduction for women who continue to work is 8 to 11 percent smaller. Women’s subjective responses to questions about working more to maintain health insurance are consistent with the conclusions from observed behavior.
1. Introduction
When workers are faced with serious health conditions that require expensive treatment and long periods of recovery, provision of health insurance through an employer can complicate their decisions. Although workers may want to invest in their health by taking time away from work for treatment and recovery, their demand for health insurance rises because of the increased risk of health care expenses. Employer-provided health insurance is often only offered to or taken up by full-time employees, in which case ill workers must also work enough hours to keep their health insurance benefits. The potential loss of insurance coverage (or an increased cost of health insurance if workers reduce hours and purchase coverage) therefore raises the cost of forgoing work for treatment (or recovery) (Bradley et al., 2006). The need to maintain labor supply at a level sufficient to keep health insurance could have adverse health consequences; work could conflict with recovery, or it could influence treatment decisions or adherence with a treatment plan.
Workers who become ill and lose their employer-provided health insurance have limited alternative options to obtain insurance. One possibility is continuing coverage through the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA). However, former employees pay the full cost of group coverage, and the policy is usually limited to 18 to 36 months – making continuation of coverage via COBRA a prohibitively expensive option for many and only a temporary measure even for those who can afford it.1 Alternatively, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) allows employees to add to their insurance policy a spouse or other dependent who loses job-related coverage, without waiting until next open enrollment cycle. However, HIPAA offers no protection to many ill workers, including those whose spouses are not employed and those with employed spouses whose employer does not offer health insurance coverage for family members.2 The Family Medical Leave Act (FMLA) entitles eligible employees of covered employers to take unpaid, job-protected leave for specified family and medical reasons with continuation of group health insurance coverage (U.S. Department of Labor, 2012). However, not all workers are covered by FMLA and some workers may fear that using FMLA will result in adverse consequences at work. Nonetheless, FMLA seems likely to mute the extent to which people with health shocks are constrained to remain at work and not reduce their hours.
This paper studies labor supply changes following health shocks, comparing married women newly diagnosed with breast cancer and dependent on their own job for health insurance to similar women who are insured through a spouse’s policy or with access to insurance through a spouse. We survey these women three times to cover three distinct periods: just prior to diagnosis (retrospectively) and two and nine months after initiation of treatment. By focusing on the time period immediately following treatment initiation, we observe labor supply behavior when treatment demands are greatest and therefore entail decisions about labor supply (including whether to remaining employed).
We include a core set of analyses that replicate Bradley et al. (2006), but we use a sample specifically constructed to address the relationship between labor supply and dependence on one’s job for health insurance in a breast cancer context. Moreover, we present a number of new analyses based on comparisons of women who depend on their jobs for health insurance to subsets of women who are less dependent on their own employment for health insurance but who are more likely to be similar in terms of unobservables such as job characteristics and commitment to work. The alternative comparisons are intended to better account for unobserved heterogeneity associated with the prior choice of health insurance source that could affect labor supply changes over time, perhaps also including labor supply in responses to a new diagnosis of breast cancer. When we simply compare women offered health insurance through their employer (which we term ECHI, for “employment-contingent health insurance”) to those without ECHI, differences in labor supply behavior may be driven by the other differences between women who do or do not have ECHI, or differences in their jobs. In contrast, for example, one new comparison we introduce restricts attention to women offered ECHI, and distinguishes between those who enrolled in ECHI and those who declined (and instead took insurance through their spouses’ employers). Women offered ECHI are likely to have more similar types of jobs and careers, so among those offered ECHI, the difference between those women who do and do not enroll should better isolate differences in labor supply responses attributable solely to how dependent they are on their own job for insurance. A second comparison is again only among the more homogeneous group of women with ECHI, but contrasting those who have the option to switch to a spouse’s policy with those who do not.
Finally, as an alternative method of accounting for unobserved heterogeneity associated with labor supply changes and the prior determination of the source of health insurance, we constructed a sample of demographically-similar women from the Current Population Survey (CPS) (U.S. Department of Labor, 2002), who we assume were healthy and did not get a cancer diagnosis. When we combine the two samples, we add another level of differencing that removes the potential influence of differences in how labor supply evolves over time for women with and without ECHI.
2. Research on Labor Market Incentives and Employer-Based Health Insurance
The studies most relevant to our investigation directly examine changes in labor supply following a health shock, although only a handful of studies fit this description, implying a substantial gap in the literature that the current study can help to fill. There are also studies of “job lock” – the hypothesis that workers remain in their current job to retain health insurance. These studies are related because they link the need for health insurance to being “locked” into a job. The literature on job lock is larger, but because it does not pertain to health shocks per se, we focus in this brief literature review on studies that incorporate health status of the employee (or their dependents) into their analysis.
Labor supply and health conditions
We are aware of three studies of labor supply that report evidence on how workers with employer-provided health insurance respond to illness. In a study using primary data collected from a sample of married women in Detroit newly diagnosed with breast cancer, women with ECHI were significantly more likely to remain employed than were women with insurance provided by another source; similarly, ECHI moderated the negative impact of cancer on weekly hours worked (Bradley et al., 2006). Specifically, women with ECHI were 10 percentage points more likely to remain employed six months after diagnosis than women with insurance through another source, rising to 17 percentage points 18 months after diagnosis.
Paralleling these findings, Tunceli et al. (2009), using data from cancer survivors two to six years following diagnosis, and a non-cancer sample drawn from the Health and Retirement Study (HRS), reported higher employment rates after a cancer diagnosis for those with ECHI compared to those who had an alternative source of health insurance or who were uninsured. Relative to changes for those with and without ECHI in the non-cancer sample, they found positive influences of ECHI on remaining employed (or remaining employed full-time) and on staying in the same job.
Finally, using the HRS to identify respondents with a broad range of health shocks, and a comparison group without health shocks to control for differences in change in labor supply associated with insurance source, Bradley et al. (2012) found that for some specifications of health shocks ECHI encourages continued employment of men, although not of women. In particular, this was true for health shocks mainly associated with higher future costs of health care rather than current morbidity that could itself directly reduce employment. Thus this literature, although sparse, generally suggests that ECHI dampens the negative labor supply response to illness, presumably because employees with ECHI work at higher levels following illness to maintain their insurance.
One likely reason for the small quantity of research on how labor supply responses to illness are affected by employer-provided health insurance is that in national databases such as the HRS, the prevalence of illness and/or poor health status – especially among employed individuals – is too low to provide adequate sample sizes for study. Furthermore, illnesses are heterogeneous in type, severity, and treatment, and few studies collect sufficient detail on illness and treatment to adequately control for these differences. Thus, researchers seeking to study this topic are limited by the secondary data sources available. This motivates efforts to collect primary data from a sample of individuals with a similar disease followed by similar treatments, as we have done for the research in this paper.
Job lock
The first published paper on the topic of job lock induced by ECHI, Cooper and Monheit (1993), suggested that the phenomenon was important. Studying a sample of workers aged 25 to 55, they estimated that ECHI reduced the likelihood that a worker changed jobs by 25% among married males, the group with the strongest labor force attachment, and up to 38% for married females, the group with the weakest attachment. However, a major criticism of Cooper and Monheit’s research was that it suffered from biases owing to endogeneity of health insurance that can lead to correlations of health insurance status with job characteristics such as pensions, life insurance, sick leave, and paid vacations, as well as wages and working conditions. These other factors may attract less mobile or more committed workers, leading to estimated effects on job mobility that are wrongly attributed to ECHI. Madrian (1994) attempted to address these issues using difference-in-differences estimators to isolate job lock by comparing groups with differences in their demand for health insurance. She used three different proxies for the demand for ECHI, including the availability of insurance coverage from other sources, family size, and the occurrence of a pregnancy (with the second and third proxies indicating higher expected future health expenses). Madrian found evidence that job lock reduced voluntary job changes by 25% (or 4 percentage points, from 16% to 12%).
Kapur (1998) re-analyzed Madrian’s data and specification, and in part due to data issues and in part due to specification issues found much smaller and statistically insignificant estimates for some specifications. Kapur also used a refined version of Madrian’s approach, relying on the interaction of double insurance coverage (by one’s own employer, and access through a spouse) and measures of health status to estimate job lock. She also incorporated additional measures of health status including medical conditions, nights in a hospital, emergency department visits, medical visits, prescribed medications, and medical expenses. Using her framework and data, Kapur found small, precise, and insignificant estimates of job lock, in sharp contrast to Madrian’s results.
Gilleskie and Lutz (2002) made a significant departure from the rest of the job lock literature in using a structural modeling approach to estimate the influence of health insurance on job mobility. Unlike previous work that identified effects by narrowing down comparison groups to be as similar as possible, Gilleskie and Lutz relied on a dynamic optimization model of employment transitions, the offer of ECHI, and the acceptance of ECHI to explicitly account for unobserved individual characteristics that are correlated with the choice of insurance source, incorporating new data (from the 1979 National Longitudinal Survey of Youth) on the offer of ECHI by employers. Gilleskie and Lutz found no evidence of job lock for married men and only a modest effect for unmarried men.
Like the more convincing evidence on job lock, in the current paper we also pay close attention to unobserved (as well as observed) individual and job characteristics correlated with the offer or take-up of ECHI that can independently influence labor supply changes over time and, in particular, labor supply responses to a health shock.
3. Application to Breast Cancer
Female breast cancer survivors comprise the largest percentage of all cancer survivors, approximately 23%, and the largest percentage (41%) of all female cancer survivors (National Cancer Institute, 2011a). Five-year survival rates exceed 83% for women diagnosed with regional stage disease and 96% for women with local stage disease (National Cancer Institute, 2011b). There are numerous studies of breast cancer’s impact on employment, motivated by the fact that with screening and earlier detection, working age women have become more likely to be diagnosed with and treated for the disease. One study found that women with breast cancer were 17 percentage points less likely to be employed than women in a non-cancer control group six months following diagnosis, but by 12 and 18 months following diagnosis, their likelihood of employment was not statistically different (Bradley et al., 2007). Recent studies of breast cancer and employment also find modest declines in employment; examining over 1,000 initially-employed women diagnosed with breast cancer, Mujahid et al. (2011) report that approximately 90% were employed nine months following diagnosis, although employment fell more for Latina women than for white women.
Although the evidence points to high rates of return to work on average, women with more extensive disease that requires several months of chemotherapy and/or radiation may experience greater work interruption than women treated with surgery alone (Stephan, 2010). In addition to the time away from work required for treatment, women who receive chemotherapy experience considerable morbidity, which can negatively affect their ability to return to work. For example, Hassett et al. (2009) reported return to work rates of 93% among over 3,200 employed and insured women, but those who received chemotherapy were more likely to go on disability, stop working, or retire relative to women who did not receive chemotherapy. The effects of chemotherapy can continue for several months or even years following the completion of treatment (Bradley et al., 2007; Johnsson et al., 2011; Hassett et al., 2009).
Despite the morbidities imposed by breast cancer treatments, women have a strong incentive to continue working if they are dependent on their jobs for health insurance. The cost of breast cancer treatment for insured women in 2007 was estimated to be $66,489, and out-of-pocket expenses for women with employer-provided coverage were estimated to be $6,250 (Gabel et al., 2009). Given high survival rates, once women are successfully treated, their worries may turn away from survival and toward the future costs of care for cancer surveillance, second primary cancers, and reoccurrence of the first primary cancer.
Capitalizing on our knowledge of breast cancer’s impact on employment, and our past experience recruiting, enrolling, and studying breast cancer patients, we designed a study to address the intersection of breast cancer, employment, and employer-provided health insurance. The earlier research on employment and hours responses (Bradley et al., 2006) used a sample limited to a single metropolitan area (Detroit, MI) and collected limited information on cancer treatment. Our current study of ECHI and breast cancer was designed to overcome these limitations. Most importantly, it targeted women who received chemotherapy or radiation (or both), for whom the tensions between not working to recover and working to maintain insurance are sharp; these treatments are the most costly, and they are more likely to entail both considerable morbidity and severe disease (making the chances of reoccurrence higher). We study women with breast cancer because we can determine disease severity and the uniformity of treatment by disease stage. These conditions allow us to isolate ECHI’s incentives without introducing noise due to differences in diseases and treatments. The new data we collected provide a more complete picture of how employer-provided health insurance affects labor supply responses to illness than has been available to date.
4. Data
Cancer sample
Our study uses a quasi-experimental design to examine how women’s dependence on their job for health insurance influences their labor supply responses following a new diagnosis of breast cancer. We enrolled 496 employed, married women within two months following surgery or initiation of chemotherapy or radiation. The women had to have ECHI, or be covered by their spouse’s employer-provided health insurance.3 We aimed to enroll women with chemotherapy and/or radiation, although a small number of women in our sample did not pursue these options and others were recommended against chemotherapy and/or radiation following results from surgery.4 The study was powered to detect statistically significant differences (p<.05) in the proportion subsequently employed six months following diagnosis between those with and without ECHI, based on estimated effect sizes from prior work. In that prior work, 85% of women with ECHI and 70% of women without ECHI remained employed following diagnosis and treatment (Bradley et al., 2006). To detect this effect size, we required a minimum of 134 women in each group, but ultimately aimed to enroll 500 women with 250 in each group, anticipating that we would retain 220 in each group throughout the study period.5 Enrolling women with health insurance through their spouse proved to be more difficult than anticipated because a greater share of eligible women was covered through their own employer than in our previous study (Bradley et al., 2006). As a result, when enrollment ended, we had 278 subjects with ECHI and 218 with insurance through their spouse’s employer-provided policy.
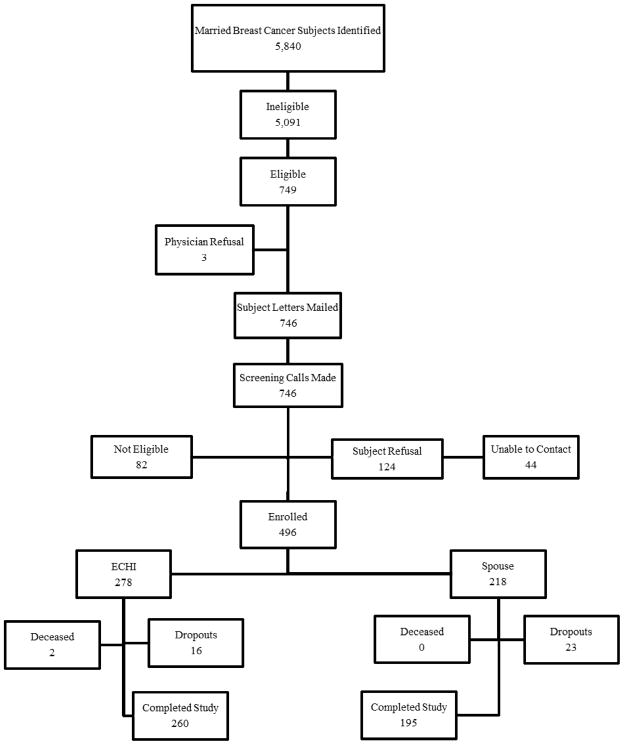
To obtain this sample, we collaborated with two academic and one private non-profit hospital-based treatment centers and five private oncology centers from urban and rural areas in Virginia. Figure 1 traces out how we got from the initial subjects identified to our analysis sample. We reviewed the records of 5,840 breast cancer patients to identify prospective study subjects. Inclusion criteria were: married, between ages 21 and 64 years at the time of diagnosis, employed at diagnosis, and insured either through their own employer or through a spouse’s employer (and not explicitly enrolled in insurance from both sources).6 Subjects had to be without metastatic disease7 and within two months of initiating chemotherapy and/or radiation (or for the few cases of women who did not receive these treatments, within two months following surgery).
Figure 1.
Subject identification, enrollment, and retention for cancer sample
Letters were mailed to eligible subjects’ physicians (N=749). Physicians of three subjects refused to allow us to contact their patients. We mailed letters and consent forms to 746 women. Interviewers then telephoned the women to screen for eligibility. Only 124 (20%) of eligible women refused to participate; 82 (11.1%) were ineligible for the study because they had multiple insurance sources or were uninsured; and we were unable to contact 44 women (6%). If we include subjects who we were unable to contact in the refusal rate (possibly passive refusals), the refusal rate rises slightly (to 25.3%). Women who refused were approximately two years older than retained subjects, and more likely to be white.
We retained 92% of the sample over the nine-month study period. Women who dropped out of the study were comparable to those retained in terms of age and insurance source, but were more likely to be white. Among those who dropped out of the study and for whom we have cancer stage information, fewer had ductal carcinoma in situ relative to those who completed the study (8% versus 16%), and more of the dropouts had Stage III cancer – 20%, versus 9% in the retained sample. Abbreviated surveys were completed by 18 of the dropouts (47.4%), of whom 10 had ECHI and 8 had insurance through their spouse. Only one of these women reported that they were no longer working. Given the small number of dropouts overall, we suspect their impact on the analysis is minimal.8 Lastly, two women died before completing all interviews and were removed from the sample.
Starting in the fall of 2007, we interviewed women covering three periods: at enrollment (a retrospective interview that referred to the employment situation at diagnosis), during chemotherapy or radiation treatment (approximately two months following the initiation of treatment – in many cases coupled with the same interview that collected the retrospective information), and approximately nine months following treatment initiation. The majority of women (85%) completed treatment by the last interview.
The questionnaire asked about subject and spouse demographic characteristics, job characteristics, job involvement, job satisfaction, insurance characteristics, and mental and physical health status. In addition to the telephone interview, we conducted audits of subjects’ medical records. These audits extracted detailed information about cancer stage, surgery, chemotherapy regimen, and radiation. All interviews were audio recorded; quality control checks of the audio recordings against data entry revealed a data entry error rate below 1%.9 The last interview was completed in September 2011.10
CPS control samples
The selection of ECHI is potentially endogenous, and could be correlated with other sources of changes in labor supply that occur over time independently of health shocks. To implement one of our approaches to this problem, we constructed control samples of Virginia residents who are assumed healthy using the CPS. Because we use the CPS control sample to control for labor supply changes over time, we matched the spans between interviews in our cancer sample to the extent possible while maximizing the size of the sample extracted from the CPS. The cancer sample interviews were conducted on average two and nine months from treatment initiation, which led to an average span of three months between diagnosis and the first post-treatment interview and 12 months between diagnosis and the second post-treatment interview. To match the baseline and post-diagnosis interviews in the cancer sample, we chose CPS respondents with a similar time span between interviews. We used the March supplement as the baseline interview for all CPS respondents because it contains health insurance information. To mimic the two-month interview, we matched CPS respondents to the March supplement with the same individuals’ responses to the basic monthly survey for the month of May.11 This implies that CPS respondents who were in month-in-sample (MIS) 1 during March were matched to the same individuals’ records for MIS 3. Likewise, MIS 2 records were matched to MIS 4 records, MIS 5 to MIS 7, and MIS 6 to MIS 8.12 To match the span between the cancer interviewees’ baseline and second interview, we allowed a slightly wider range for CPS respondents, selecting those with intervals from 9 to 12 months apart. Therefore, March supplement respondents in MIS 1 through MIS 4 were matched to their basic monthly records for MIS 5 (which occurred the following December of the same year through March of the next).13 Specific questions regarding diseases such as cancer were not part of the CPS, and so a few respondents in the control population may have had cancer or other diseases.
From the CPS sample, we selected married, employed women between the ages of 26 and 64 years who were covered by insurance provided by their own employers or their husbands’ employers. Respondents with double insurance coverage were excluded, to mimic this feature of the cancer sample. The combination of these exclusions, CPS survey attrition, and the matching process left us with 372 individuals from the CPS to use as controls to match to the baseline and first interview, and 386 controls to match to the baseline and second interview.14 Among the control subjects selected for the two-month interview sample, 194 had ECHI and 178 were insured by their husbands’ employers. For the nine-month interview control sample, 209 had ECHI and the remaining 177 had insurance through their husbands’ employers.
5. Empirical Approach
Statistical models
The transition from employment to non-employment and the percentage change in weekly hours worked are modeled as functions of the source of health insurance prior to diagnosis (either ECHI or spouse insurance in our baseline specification, with INS an indicator of having one form of insurance or the other), breast cancer stage (BCS),15 other exogenous variables (the vector of these other variables and BCS is denoted X), and unobserved influences (ε). Breast cancer stage is categorized as ductal carcinoma in situ (DCIS or Stage 0), Stage I (tumor <2 cm and no lymph node involvement), Stage II (tumor <2 cm and lymph node involvement or tumor <5 cm without lymph node involvement), and Stage III (cancer present in the axillary lymph nodes and chest wall). Stage IV is metastatic cancer. Although we excluded patients with Stage IV disease from initial study enrollment, three such patients were included in the sample who were thought to have earlier stage disease but were later found to have distant metastases.
We estimate the employment equation for post-diagnosis periods:
| (1) |
We define employment status as a binary variable (Eit) that equals one if a woman reports that she worked for pay one or more hours per week (Eit * is an unobserved latent variable).16 We estimate separate linear probability models for employment at the two- and nine-month interviews. The subscript i refers to the ith individual and the subscript t refers to the interview period (t=1 for the baseline interview period, t=2 for the two-month interview, and t=3 for the nine-month interview), and αE, βE, and γE (a vector) are parameters.
In our estimation of the effect of ECHI on weekly hours worked (H), we assume that the same variables that affect employment also potentially affect hours worked, and estimate models for the percent change in hours worked relative to the period just prior to the breast cancer diagnosis, for those working. For the two-month interview, for example, we estimate:
| (2) |
We also report results from similar models of the percent change in weekly hours worked that do not condition on employment after diagnosis. These unconditional models also capture the effect of non-employment for women no longer working, with weekly hours worked post-diagnosis set to zero for non-employed women. The conditional and unconditional hours equations are estimated separately for the two- and nine-month interviews. All models are estimated using Ordinary Least Squares (OLS) with reported standard errors clustered at the physician level.
Note that these models estimate the relationship between ECHI and changes in employment or hours relative to labor supply prior to the breast cancer diagnosis. Variation in pre-diagnosis labor supply associated with ECHI, which we would expect, is differenced out in these specifications. Thus, the “first-order” effects of endogeneity in the selection of ECHI are removed. Nonetheless, unobserved differences across women with and without ECHI can still be associated with changes in labor supply, and this is a confounding factor in trying to draw causal inferences regarding how ECHI affects labor supply following a health shock, even when we condition on labor supply prior to the shock. To further address these concerns, we estimate three alternative specifications that compare women based on their offer of health insurance and on the offer and take up of their spouse’s health insurance.
Control variables
The most direct approach to trying to account for differences between women with and without ECHI that could affect labor supply changes over time (whether or not a health shock occurs) is to include detailed controls, and our data set was designed to include a very rich set of such controls. We control for worker, family, and job characteristics, as well as physical and mental health and cancer treatment.
The control variables describing the respondents and their job characteristics are measured for the pre-diagnosis period. We control for weekly hours worked at baseline, individual characteristics including age, race (non-Hispanic white, non-Hispanic African American, and other), education (high school diploma or less, some college or Associate’s degree, Bachelor’s degree, advanced degree), whether the subject has children under age 18, occupation type (white collar or blue collar), pre-diagnosis annual household income (< $40,000, between $40,000 and $74,999, between $75,000 and $150,000, > $150,000), and share of household income that was contributed by the subject (≤ 25%, 26% to 50%, 51% to 75%, and >75%). Age is specified as a continuous variable. All estimations include dummy variables for the year of the interview (2007–2011).
Job characteristics (in addition to blue- and white-collar designations) include firm size (<25, 25 to 49, 50 to 99, 100 or more employees), employer type (government, private for-profit, non-profit, and self-employed17), generosity of sick leave benefits (full pay less than one month, one to three months full pay, four to six months full pay, seven or more months full pay, full pay, but length unknown, partial pay for less than one month, partial pay for one to three months, partial pay for four to six months, partial pay for seven or more months, partial pay of length unknown, and not offered paid sick leave18), availability of retirement plan (retirement plan offered and the subject participates, retirement plan offered but subject does not participate, retirement plan not offered), health insurance generosity (employee pays all of premium, employee pays part of premium, employee pays none of premium, and a separate variable indicating whether the employee has co-pays), and health insurance flexibility (employee can choose any physician, employee has only a limited set of physicians).
We then include variables for whether the subject holds more than one job, has worked for 49 or more weeks in the past year, and held the current job for more than one year, and whether she engaged in job search activities prior to diagnosis (including looking for a job, completing applications, contacting a potential employer, or interviewing for another position).19 As a further measure of job satisfaction, we included subjects’ scores on the Minnesota Job Satisfaction questionnaire that referenced the pre-diagnosis period (Weiss et al., 1967). Responses were summed across the 20 items to create a summary measure of overall job satisfaction.
We also included responses to job task questions that parallel those in the HRS. These questions asked if the woman agreed with statements such as “My job involves a lot of physical effort.” The response categories were all/almost all of the time, most of the time, some of the time, or none/almost none of the time, for the following tasks: physical effort, lifting heavy loads, stooping, kneeling, crouching, intense concentration/attention, data analysis, keeping up with the pace set by others, learning new things, and whether the job requires good eyesight. We dichotomized responses into all/almost all of the time and most of the time versus some of the time or none/almost none of the time. We also asked subjects to report the number of hours they spent sitting per day and created a dummy variable indicating if the respondent spent less than 2.5 hours, 2.5 to five, five to seven, or more than seven hours a day sitting.
Last, we assessed women’s degree of job involvement using Likert-type questions (Lodahl and Kejner, 1965). Women were asked if they strongly agreed, agreed, disagreed, or strongly disagreed with five statements regarding their attitudes toward their jobs that reflect both commitment and the quality of the job. The statements were “the major satisfaction in my life comes from my job,” “the most important things that happen to me involve my work,” “I’m really a perfectionist about my work,” “I live, eat, and breathe my job,” and “I am very much involved personally in my work.” We dichotomized the responses into strongly agree/agree versus strongly disagree/disagree.
We also add controls that are more specific as to the timing and type of treatment, with separate indicators for whether chemotherapy and/or radiation were received at the time of the two-month and/or nine-month interviews. To control for health status we include scores on the SF-36v2 Health Survey (Ware et al., 1993), including separately the mental and physical component scores (MCS and PCS). We also the 10-item Center for Epidemiologic Studies Depression scale (CESD-10) (Anderson et al., 1994). Last, we ask subjects to report whether they had been diagnosed with any of the Charlson comorbid conditions (Charlson et al., 1987) and categorized their responses as having no comorbid conditions, one condition, or two or more conditions.
To give an idea of how the inclusion of our extensive set of controls affects the estimates, in some of the tables we report estimates of parsimonious baseline models and then expanded models; in others we report only the expanded models.20
Alternative comparisons
Our baseline analysis compares the labor supply responses to health shocks for women with and without ECHI. Although we have very rich controls in our data, there still may be unobserved differences between women with ECHI and women without ECHI, and likewise there may be differences between jobs that offer ECHI and jobs that do not. These individual or job differences may affect how labor supply changes over time, possibly leading to spurious attributions of response differences to dependence on employment for health insurance. For example, women with ECHI could be more persistent or committed workers who are less likely to reduce labor supply. Alternatively, they could be in jobs that are more accommodating to health shocks allowing for greater labor supply reductions. As this discussion indicates, biases from unobserved differences between women with or without ECHI could in principle bias the estimated differences in labor supply responses depending on ECHI in either direction.
To address these concerns, we estimated three additional specifications. First, we include a dummy variable for whether the woman was offered ECHI (denoted OFFER), and an interaction between ECHI and OFFER. We then focus on the interaction between ECHI and OFFER. In this case, equation (1) becomes:
| (3) |
The idea is that those who took up the ECHI offer are dependent on their own employment for insurance, while those who did not take it up are not. Women who were offered ECHI but did not accept it should have jobs with similar unobserved characteristics to those jobs held by women who took up ECHI. The inclusion of the OFFER variable can be interpreted as adding a control for employer and job characteristics. The difference – among those offered ECHI – between those who take up the offer and those who do not – captured in the parameter βE’ – provides a comparison among more homogeneous women than we get from the simple comparison between women with ECHI and without ECHI.21 Notice that because everyone with ECHI must have been offered ECHI, the three variables ECHI, OFFER, and ECHI × OFFER cannot vary independently. It is not possible to observe the combination ECHI = 1 and OFFER = 0, which is why an ECHI main effect does not appear in the equation (as it would in a difference-in-differences specification). Rather, there are only three conditional expectations that can be observed that identify the effects of ECHI: E(Eit|OFFERi1=1,ECHIi1 = 1,Xi1), E(Eit|OFFERi1=1,ECHIi1 = 0,Xi1), and E(Eit|OFFERi1=0,ECHIi1 = 0,Xi1). βE’ identifies the difference between the first two of these, which is the effect of ECHI for those offered ECHI and excludes the influence on the estimated effect of ECHI of those not offered ECHI. However, there still could be differences between women who declined an offer of ECHI and those who accepted it, stemming from individual-level differences such as career orientation, insurance generosity relative to a spouse’s policy, and degree of dependence on a spouse. The comparisons we discuss below try to account for these differences as well.
Note that the identification strategy is the same if we simply study only observations with OFFERi1 = 1, and estimate the model:
| (4) |
In this model βE” captures the same effect as βE’ in equation (3). The advantage of estimating equation (3) on the full sample is that we have a very large number of controls in X, and excluding the observations with OFFERi1 ≠ 1 discards information on the coefficients of these controls. With 116 control variables in X, this is a serious concern. Nonetheless, we estimated the simpler equation (4), and the corresponding versions for the other comparisons discussed below. The results (not shown) were qualitatively similar.22
As a second comparison, aimed at better controlling for unobserved individual-level differences, we estimate models that retain the ECHI indicator, and add an interaction term between ECHI and an indicator for whether or not the woman’s spouse is insured through his own employer-provided policy. We define a dummy variable NOSECHI, equal to one when the spouse does not have employer-provided coverage. A similar point to the above discussion applies here. In this case, it is not possible to observe ECHI = 0 and NOSECHI = 1 in our sample, since women recruited into our sample either have ECHI or insurance through their spouse. In this specification, the variable ECHI serves as a control for unobservables associated with ECHI, and instead we focus on the difference – among women with ECHI – between those who can switch to an insured spouse’s policy and those who cannot, as the former group is less dependent on their own employment for health insurance.23 The coefficient of interest, therefore, is that on the ECHI × NOSECHI interaction, which we would expect to be positive, indicating that those with ECHI but without an option for coverage through their spouse are more likely to remain employed or to work longer hours after diagnosis.24
We note an important point regarding the nature of our sample of women with breast cancer and the validity of this second alternative comparison. Women with explicit double coverage were excluded from our cancer sample during the recruitment stage. This implies that the women for whom ECHI equals one and NOSECHI equals zero did not explicitly hold double coverage in insurance; the wives in the sample held insurance through their employers to cover themselves and the husbands held separate coverage of their own through their own (the husbands’) employers. This does not mean, though, that the women would be unable to access the coverage from their husbands’ employers or that they would have to wait until an open enrollment period. Under HIPAA, if a woman lost access to her ECHI (as she would if she decided not to work to focus on treatment), she would be given the opportunity to enroll in her husbands’ employer-provided insurance, even with a pre-existing condition.25 Thus, NOSECHI captures the women in our sample who have the option to switch to their husbands’ insurance, even though they were not actually enrolled at the time.
There is an important drawback, however, in using NOSECHI to proxy for the ability to switch insurance: the rules in HIPAA that allow a wife to switch to her husbands’ employer-provided insurance when she loses her coverage also apply when even when her husband is not actually enrolled in his employer’s insurance. As long as his employer offers family insurance coverage to its employees, the wife and her husband would both have the option to enroll in his employer’s plan upon losing their other coverage, even if it is not an open enrollment period. Thus, when we use NOSECHI to capture the option to switch insurance sources, we improperly categorize some individuals – those who have NOSECHI equal to one, but whose spouse’s employer offers health insurance.
To address this issue, we take advantage of the unique level of detail in our survey of cancer patients and create the indicator variable NOSOFFER, another proxy for the option to switch. NOSOFFER equals one when the husband’s employer does not offer a health insurance plan. We then estimate a similar specification to the second (NOSECHI) comparison, again effectively conditioning on ECHI but using an interaction of NOSOFFER with ECHI to indicate the option to switch to the husband’s employer-provided insurance.
Adding the CPS data
The addition of the CPS samples to the cancer sample provides another means of controlling for unobserved heterogeneity that can be correlated both with the source of health insurance and labor supply changes, as explained earlier. When we also use the CPS control samples, we add to equations (1) and (2) a dummy variable that indicates if the woman was a subject from the breast cancer sample (and hence had cancer, denoted BCA), and an interaction between this dummy variable and the ECHI dummy variable, such as in the following equation for employment:
| (5) |
In this model, with these data, the ECHI dummy variable captures changes in employment associated with ECHI, while βE’ is now the parameter that captures how ECHI affects the labor supply response of the breast cancer diagnosis.
The CPS contains a much more limited set of controls than what we have in our primary data. We therefore estimate more parsimonious models when we include the CPS data, including only the controls common to both datasets. Demographic controls include subject and spouse age, race, and education, household income, the wife’s share of household income, and an indicator for children under 18. Employment controls include firm size, firm type, and baseline hours worked for both subject and spouse (unemployed spouses were included via a separate indicator variable), and an indicator for occupation type (blue vs. white collar) for the wife. Dummies for year of interview are also included.26 These more parsimonious specifications are unlikely to pose a problem for this analysis, because identification comes from differences associated with breast cancer only among women with ECHI, so that the underlying differences between women with and without ECHI are differenced out.
6. Results
Descriptive statistics
Table 1 reports descriptive statistics for the cancer sample. Columns 1 and 2 compare women with and without ECHI. Women with ECHI were more likely to be diagnosed at later stages and were more likely to have had chemotherapy by the second interview. Women with ECHI were more likely to be African American, to earn a larger share of household income, and more likely to work for a large firm (100 or more employees) or be employed by a government agency. They were more likely to have jobs that offered more generous sick leave benefits and were more likely to be included in a retirement plan at work. Women with ECHI were also more likely to have jobs that required the analysis of data or other information, keeping the pace set by others, and sitting for the majority of the day, but less likely to have jobs that require stooping, kneeling, or crouching. These women were also less likely to have engaged in job search activities in the prior year and had longer job tenure prior to the diagnosis of breast cancer. They also appear to have slightly more generous health insurance plans in terms employer paid premiums and visits to specialists. Their spouses are more likely to self-employed or not working and if working, to be employed in smaller firms. Fewer of their spouses report excellent or very good health status. Their spouses work fewer hours per week (38.46 versus 43.95) than the spouses of women who are covered by their husband’s insurance.
Table 1.
Descriptive statistics for cancer sample at baseline interview
| Observations | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) |
|---|---|---|---|---|---|---|---|---|
| Base comparison | Alternative 1 | Alternative 2 | Alternative 3 | |||||
|
| ||||||||
| OFFER=1 | OFFER=1 | ECHI=1 | ECHI = 1 | ECHI=1 | ECHI=1 | |||
| ECHI=0 | ECHI=1 | ECHI=0 | ECHI=1 | NOSECHI=0 | NOSECHI=1 | NOSOFFER=0 | NOSOFFER=1 | |
| 195 | 260 | 110 | 260 | 109 | 151 | 164 | 96 | |
| Labor supply | ||||||||
| Employed 2 months (SD) | 83.08 (37.59) | 83.08 (37.57) | 81.82 (38.75) | 83.08 (37.57) | 85.32 (35.55) | 81.46 (38.99) | 84.76 (36.05) | 80.21 (40.05) |
| Employed 9 months (SD) | 87.69 (32.94) | 91.92 (27.30) | 86.36 (34.47) | 91.92 (27.30)* | 90.83 (29.00) | 92.72 (26.08) | 91.46 (28.03) | 92.71 (26.14) |
| Mean weekly hours worked (SD), Baseline | 37.26 (13.34) | 43.97 (8.30)*** | 40.59 (10.40) | 43.97 (8.30)*** | 43.36 (7.58) | 44.42 (8.78) | 43.65 (7.97) | 44.52 (8.85) |
| Mean weekly hours worked (SD), 2 months | 25.96 (16.68) | 30.89 (16.92)*** | 28.57 (16.90) | 30.89 (16.92) | 30.42 (15.95) | 31.23 (17.62) | 31.12 (16.39) | 30.50 (17.85) |
| Mean weekly hours worked (SD), 9 months | 29.79 (16.35) | 38.11 (14.27)*** | 32.63 (15.86) | 38.11 (14.27)*** | 36.74 (14.33) | 39.10 (14.19) | 37.22 (14.11) | 39.64 (14.48) |
| Demographics | ||||||||
| Age (SD) | 48.92 (7.09) | 49.38 (7.77) | 48.34 (7.07) | 49.38 (7.77) | 48.73 (8.36) | 49.84 (7.32) | 48.27 (8.06) | 51.26 (6.89)*** |
| Race/ethnicity | *** | ** | ||||||
| White, non-Hispanic | 84.62 | 73.85 | 81.82 | 73.85 | 72.48 | 74.83 | 70.12 | 80.21 |
| African-American, non-Hispanic | 9.23 | 23.46 | 11.82 | 23.46 | 23.85 | 23.18 | 26.22 | 18.75 |
| Other | 6.15 | 2.69 | 6.36 | 2.69 | 3.67 | 1.99 | 3.66 | 1.04 |
| Education | ||||||||
| High school diploma or less | 13.85 | 14.62 | 10.91 | 14.62 | 19.27 | 11.26 | 14.63 | 14.58 |
| Some college or Associate’s degree | 27.18 | 29.62 | 27.27 | 29.62 | 27.52 | 31.13 | 30.49 | 28.12 |
| Bachelor’s degree | 30.77 | 32.31 | 32.73 | 32.31 | 34.86 | 30.46 | 35.37 | 27.08 |
| Advanced degree | 28.21 | 23.46 | 29.09 | 23.46 | 18.35 | 27.15 | 19.51 | 30.21 |
| Has children < 18 | 46.67 | 39.23 | 51.82 | 39.23** | 40.37 | 38.41 | 42.68 | 33.33 |
| Household income | ||||||||
| <$40,000 | 3.59 | 5.00 | 4.55 | 5.00 | 5.50 | 4.64 | 3.66 | 7.29 |
| $40,000 – $74,999 | 17.95 | 21.54 | 15.45 | 21.54 | 21.1 | 21.85 | 18.29 | 27.08 |
| $75,000 – $150,000 | 48.72 | 48.46 | 50.91 | 48.46 | 46.79 | 49.67 | 48.78 | 47.92 |
| >$150,000 | 27.18 | 22.31 | 28.18 | 22.31 | 23.85 | 21.19 | 26.22 | 15.62 |
| Respondent’s share of household | ||||||||
| income | *** | *** | ** | *** | ||||
| <25% | 36.41 | 6.92 | 25.45 | 6.92 | 11.01 | 3.97 | 8.54 | 4.17 |
| 26% – 50% | 45.64 | 44.23 | 53.64 | 44.23 | 49.54 | 40.4 | 51.22 | 32.29 |
| 51% – 75% | 14.87 | 35.00 | 18.18 | 35.00 | 31.19 | 37.75 | 32.32 | 39.58 |
| >75% | 1.03 | 11.54 | 1.82 | 11.54 | 5.50 | 15.89 | 4.88 | 22.92 |
| Cancer and Treatment | ||||||||
| Breast cancer stage | *** | ** | ||||||
| Stage 0 | 9.74 | 11.92 | 10.91 | 11.92 | 13.76 | 10.6 | 13.41 | 9.38 |
| Stage I | 39.49 | 29.62 | 40 | 29.62 | 27.52 | 31.13 | 28.05 | 32.29 |
| Stage II | 43.59 | 41.92 | 43.64 | 41.92 | 41.28 | 42.38 | 39.63 | 45.83 |
| Stage III or IV | 7.18 | 16.54 | 5.45 | 16.54 | 17.43 | 15.89 | 18.9 | 12.5 |
| Had chemotherapy and/or radiation (SD) | 92.31 (26.72) | 93.46 (24.77) | 94.55 (22.81) | 93.46 (24.77) | 95.41 (21.02) | 92.05 (27.14) | 95.12 (21.61) | 90.63 (29.30) |
| Radiation at 2 months post-diagnosis (SD) | 16.06 (36.81) | 14.17 (34.95) | 18.52 (39.03) | 14.17 (34.95) | 15.60 (36.45) | 13.10 (33.86) | 14.91 (35.73) | 12.90 (33.71) |
| Radiation at 9 months post-diagnosis (SD) | 6.19 (24.15) | 5.47 (22.78) | 8.26 (27.65) | 5.47 (22.78) | 6.42 (24.63) | 4.76 (21.37) | 6.13 (24.07) | 4.30 (20.40) |
| Chemotherapy at 2 months post-diagnosis (SD) | 55.15 (49.86) | 66.27 (47.37)** | 57.27 (49.69) | 66.27 (47.37) | 64.15 (48.18) | 67.79 (46.89) | 67.08 (47.14) | 64.89 (47.99) |
| Chemotherapy at 9 months post-diagnosis (SD) | 8.95 (28.62) | 9.49 (29.36) | 10.19 (30.39) | 9.49 (29.36) | 10.58 (30.90) | 8.72 (28.32) | 12.58 (33.7) | 4.26 (20.29)** |
| Health measures | ||||||||
| CES-D10 score (%’s) (SD) | 11.67 (14.42) | 13.44 (15.82) | 11.57 (15.70) | 13.44 (15.82) | 13.28 (15.89) | 13.55 (15.83) | 12.75 (14.42) | 14.62 (17.99) |
| Count of comorbidities (max of 2) (SD) | 1.12 (0.85) | 1.11 (0.84) | 1.10 (0.88) | 1.11 (0.84) | 1.11 (0.84) | 1.11 (0.84) | 1.08 (0.85) | 1.17 (0.83) |
| SF-36 physical health score (SD) | 56.43 (5.26) | 56.00 (5.95) | 56.00 (5.56) | 56.00 (5.95) | 56.43 (5.41) | 55.69 (6.31) | 56.24 (5.39) | 55.58 (6.80) |
| SF-36 mental health score (SD) | 53.91 (7.98) | 53.33 (7.59) | 53.98 (8.42) | 53.33 (7.59) | 53.58 (7.16) | 53.14 (7.90) | 54.07 (6.61) | 52.06 (8.93)** |
| Job characteristics | ||||||||
| Occupation type | ||||||||
| White collar | 92.82 | 93.08 | 95.45 | 93.08 | 89.91 | 95.36 | 91.46 | 95.83 |
| Blue collar | 7.18 | 6.54 | 4.55 | 6.54 | 9.17 | 4.64 | 7.93 | 4.17 |
| Firm size | *** | ** | * | |||||
| <25 employees | 37.44 | 7.31 | 16.36 | 7.31 | 9.17 | 5.96 | 7.32 | 7.29 |
| 25 – 49 employees | 6.15 | 5.00 | 4.55 | 5.00 | 8.26 | 2.65 | 6.10 | 3.12 |
| 50 – 99 employees | 6.67 | 5.00 | 10.00 | 5.00 | 2.75 | 6.62 | 3.05 | 8.33 |
| 100+ employees | 49.74 | 82.31 | 69.09 | 82.31 | 78.9 | 84.77 | 82.93 | 81.25 |
| Firm type | *** | |||||||
| Government | 21.03 | 39.23 | 30.00 | 39.23 | 35.78 | 41.72 | 37.80 | 41.67 |
| Private, for-profit | 53.85 | 48.08 | 53.64 | 48.08 | 51.38 | 45.70 | 49.39 | 45.83 |
| Non-profit | 13.33 | 10.00 | 13.64 | 10.00 | 8.26 | 11.26 | 9.76 | 10.42 |
| Self-employed | 11.79 | 2.31 | 2.73 | 2.31 | 3.67 | 1.32 | 2.44 | 2.08 |
| Offered full sick pay | *** | ** | * | |||||
| Not Offered | 42.05 | 8.85 | 16.36 | 8.85 | 9.17 | 8.61 | 7.32 | 11.46 |
| < 1 month | 30.77 | 35.00 | 46.36 | 35.00 | 30.28 | 38.41 | 32.93 | 38.54 |
| 1–3 months | 16.92 | 30.77 | 25.45 | 30.77 | 36.70 | 26.49 | 37.20 | 19.79 |
| 4–6 months | 3.59 | 13.85 | 4.55 | 13.85 | 16.51 | 11.92 | 12.20 | 16.67 |
| 7 or more months | 3.59 | 7.69 | 5.45 | 7.69 | 4.59 | 9.93 | 6.10 | 10.42 |
| Offered but length not known | 3.08 | 3.08 | 1.82 | 3.08 | 1.83 | 3.97 | 3.66 | 2.08 |
| Offered partial sick pay | *** | |||||||
| Not offered | 83.08 | 60.77 | 73.64 | 60.77 | 62.39 | 59.60 | 60.37 | 61.46 |
| <1 month | 2.56 | 1.92 | 3.64 | 1.92 | 0.92 | 2.65 | 1.22 | 3.12 |
| 1–3 months | 2.56 | 8.46 | 4.55 | 8.46 | 5.50 | 10.60 | 7.32 | 10.42 |
| 4–6 months | 2.05 | 9.62 | 3.64 | 9.62 | 10.09 | 9.27 | 9.15 | 10.42 |
| 7 or more months | 2.56 | 6.54 | 3.64 | 6.54 | 4.59 | 7.95 | 6.10 | 7.29 |
| Offered but length not known | 5.13 | 9.62 | 8.18 | 9.62 | 14.68 | 5.96 | 13.41 | 3.12 |
| Retirement plan | *** | *** | ||||||
| Not offered | 35.38 | 3.85 | 13.64 | 3.85 | 5.50 | 2.65 | 3.66 | 4.17 |
| In plan | 51.28 | 92.69 | 73.64 | 92.69 | 90.83 | 94.04 | 92.68 | 92.71 |
| Offered, not in plan | 11.28 | 3.46 | 11.82 | 3.46 | 3.67 | 3.31 | 3.66 | 3.12 |
| Job requires most of the time or more often | ||||||||
| Lots of physical effort (SD) | 28.72 (45.36) | 25.38 (43.60) | 26.36 (44.26) | 25.38 (43.60) | 23.85 (42.82) | 26.49 (44.27) | 25.00 (43.43) | 26.04 (44.12) |
| Intense concentration or attention (SD) | 80.00 (40.10) | 82.69 (37.90) | 78.18 (41.49) | 82.69 (37.90) | 77.98 (41.63) | 86.09 (34.72)* | 79.88 (40.21) | 87.50 (33.25) |
| Lifting heavy loads (SD) | 7.69 (26.72) | 8.85 (28.45) | 6.36 (24.52) | 8.85 (28.45) | 8.26 (27.65) | 9.27 (29.10) | 9.15 (28.91) | 8.33 (27.78) |
| Stooping, kneeling, or crouching (SD) | 23.59 (42.57) | 17.31 (37.90)* | 21.82 (41.49) | 17.31 (37.90) | 11.01 (31.44) | 21.85 (41.46)** | 14.63 (35.45) | 21.88 (41.56) |
| Analysis of data or information (SD) | 63.08 (48.38) | 72.69 (44.64)** | 68.18 (46.79) | 72.69 (44.64) | 71.56 (45.32) | 73.51 (44.27) | 72.56 (44.76) | 72.92 (44.67) |
| Learning new things (SD) | 54.36 (49.94) | 58.46 (49.37) | 51.82 (50.20) | 58.46 (49.37) | 58.72 (49.46) | 58.28 (49.47) | 57.32 (49.61) | 60.42 (49.16) |
| Good eyesight (SD) | 88.72 (31.72) | 88.85 (31.54) | 88.18 (32.43) | 88.85 (31.54) | 88.07 (32.56) | 89.40 (30.88) | 86.59 (34.19) | 92.71 (26.14) |
| Job requires keeping up with pace set by others | ** | * | * | |||||
| Most of the time or more often | 45.13 | 36.92 | 47.27 | 36.92 | 43.12 | 32.45 | 39.63 | 32.29 |
| Some of the time or less often | 53.85 | 63.08 | 52.73 | 63.08 | 56.88 | 67.55 | 60.37 | 67.71 |
| Number of hours sitting per day at job | ** | |||||||
| <2.5 hours | 30.77 | 23.08 | 29.09 | 23.08 | 24.77 | 21.85 | 22.56 | 23.96 |
| 2.5 to 4.5 hours | 31.28 | 25.00 | 25.45 | 25.00 | 23.85 | 25.83 | 25.61 | 23.96 |
| 5 to 7 | 26.15 | 31.92 | 29.09 | 31.92 | 30.28 | 33.11 | 29.27 | 36.46 |
| >7 hours | 11.79 | 20.00 | 16.36 | 20.00 | 21.10 | 19.21 | 22.56 | 15.62 |
| Recent job search (SD) | 0.34 (0.89) | 0.18 (0.66)** | 0.31 (0.83) | 0.18 (0.66) | 0.19 (0.70) | 0.17 (0.64) | 0.21 (0.73) | 0.13 (0.53) |
| Job tenure of less than a year (SD) | 10.77 (31.08) | 4.23(20.17)*** | 10.00 (30.14) | 4.23 (20.17)** | 2.75 (16.44) | 5.30 (22.47) | 4.88 (21.61) | 3.13 (17.49) |
| Held one or more other jobs (SD) | 12.31 (32.94) | 11.92 (32.47) | 8.18 (27.53) | 11.92 (32.47) | 14.68 (35.55) | 9.93 (30.01) | 12.20 (32.82) | 11.46 (32.02) |
| Worked 49 or more weeks last year (SD) | 81.03 (39.31) | 92.31 (26.70)*** | 84.55 (36.31) | 92.31 (26.70)** | 93.58 (24.63) | 91.39 (28.14) | 93.29 (25.09) | 90.63 (29.30) |
| Job satisfaction score (%’s) (SD) | 68.45 (12.04) | 67.83 (11.46) | 67.22 (12.08) | 67.83 (11.46) | 67.76 (11.98) | 67.88 (11.10) | 68.13 (11.65) | 67.31 (11.16) |
| Job involvement score (%’s) (SD) | 56.71 (8.23) | 57.37 (7.34) | 56.00 (7.40) | 57.37 (7.34) | 58.24 (7.83) | 56.74 (6.93) | 57.65 (7.40) | 56.90 (7.27) |
| Health insurance features | ||||||||
| Employer pays premium | * | |||||||
| All | 15.03 | 12.69 | 11.82 | 12.69 | 15.6 | 10.6 | 12.8 | 12.5 |
| Part | 78.24 | 84.62 | 85.45 | 84.62 | 80.73 | 87.42 | 84.15 | 85.42 |
| None | 2.59 | 1.92 | 0.91 | 1.92 | 2.75 | 1.32 | 1.83 | 2.08 |
| Can visit any doctor | ||||||||
| Yes | 68.91 | 66.15 | 73.64 | 66.15 | 62.39 | 68.87 | 65.85 | 66.67 |
| No | 30.57 | 32.69 | 26.36 | 32.69 | 37.61 | 29.14 | 33.54 | 31.25 |
| Policy limits visits to non-cancer specialists | ** | ** | ||||||
| Yes | 19.69 | 26.92 | 14.55 | 26.92 | 27.52 | 26.49 | 23.78 | 32.29 |
| No | 49.22 | 52.31 | 54.55 | 52.31 | 50.46 | 53.64 | 56.10 | 45.83 |
| Co-pay for office visit | ** | |||||||
| Yes | 92.33 | 92.69 | 92.73 | 92.69 | 96.33 | 90.07 | 95.73 | 87.50 |
| No | 7.77 | 6.92 | 7.27 | 6.92 | 3.67 | 9.27 | 4.27 | 11.46 |
| Co-pay for outpatient services | *** | |||||||
| Yes | 73.06 | 71.15 | 73.64 | 71.15 | 77.98 | 66.23 | 78.05 | 59.38 |
| No | 25.39 | 24.62 | 24.55 | 24.62 | 18.35 | 29.14 | 19.51 | 33.33 |
| Co-pay for hospitals | ||||||||
| Yes | 84.46 | 82.69 | 88.18 | 82.69 | 83.49 | 82.12 | 83.54 | 81.25 |
| No | 10.88 | 12.31 | 10.00 | 12.31 | 11.01 | 13.25 | 12.20 | 12.50 |
| Spouse characteristics | ||||||||
| Spouse firm type | *** | ** | *** | *** | ||||
| Government | 24.62 | 18.46 | 24.55 | 18.46 | 27.52 | 11.92 | 24.39 | 8.33 |
| Private, for-profit | 59.49 | 48.85 | 57.27 | 48.85 | 55.05 | 44.37 | 59.76 | 30.21 |
| Non-profit | 3.08 | 2.31 | 1.82 | 2.31 | 2.75 | 1.99 | 2.44 | 2.08 |
| Self-employed | 5.13 | 13.08 | 4.55 | 13.08 | 3.67 | 19.87 | 4.88 | 27.08 |
| Spouse not working | 7.18 | 17.31 | 10.91 | 17.31 | 11.01 | 21.85 | 8.54 | 32.29 |
| Spouse firm size | *** | *** | *** | *** | ||||
| <25 employees | 8.72 | 21.92 | 6.36 | 21.92 | 11.01 | 29.80 | 10.98 | 40.62 |
| 25 – 49 employees | 3.08 | 5.77 | 1.82 | 5.77 | 6.42 | 5.30 | 6.71 | 4.17 |
| 50 – 99 employees | 4.10 | 5.38 | 2.73 | 5.38 | 3.67 | 6.62 | 6.71 | 3.12 |
| 100+ employees | 47.87 | 48.08 | 77.27 | 48.08 | 64.22 | 36.42 | 64.63 | 19.79 |
| Spouse not working | 7.18 | 17.31 | 10.91 | 17.31 | 11.01 | 21.85 | 8.54 | 32.29 |
| Spouse age (SD) | 50.68 (7.60) | 51.77 (8.86) | 50.11 (7.89) | 51.77 (8.86)* | 51.20 (8.89) | 52.18 (8.86) | 50.30 (8.73) | 54.26 (8.56)*** |
| Spouse health excellent or very good (SD) | 69.23 (46.27) | 57.69 (49.50)** | 67.27 (47.14) | 57.69 (49.50)* | 61.47 (48.89) | 54.97 (49.92) | 61.59 (48.79) | 51.04 (50.25)* |
| Spouse worked more than one job (SD) | 9.74 (29.73) | 14.23 (35.00) | 8.18 (27.53) | 14.23 (35.00) | 16.51 (37.30) | 12.58 (33.28) | 14.02 (34.83) | 14.58 (35.48) |
| Spouse job tenure of less than a year (SD) | 5.64 (23.13) | 6.54 (24.77) | 3.64 (18.81) | 6.54 (24.77) | 0.00 (0.00) | 11.26 (31.71)*** | 4.88 (21.61) | 9.38 (29.30) |
| Spouse hours worked per week (SD) | 43.95 (16.07) | 38.46 (20.54)*** | 41.01 (17.09) | 38.46 (20.54) | 42.35 (17.57) | 35.64 (22.07)*** | 42.88 (16.07) | 30.91 (24.81)*** |
| Spouse education level | *** | ** | * | |||||
| High school diploma or less | 21.03 | 32.31 | 24.55 | 32.31 | 31.19 | 33.11 | 31.71 | 33.33 |
| Some college or Associates degree | 20.51 | 26.15 | 18.18 | 26.15 | 30.28 | 23.18 | 27.44 | 23.96 |
| Bachelor’s degree | 32.82 | 21.92 | 33.64 | 21.92 | 15.6 | 26.49 | 18.29 | 28.12 |
| Advanced degree | 25.64 | 18.85 | 23.64 | 18.85 | 21.1 | 17.22 | 21.34 | 14.58 |
| Spouse race/ethnicity | *** | *** | ||||||
| Non-Hispanic white | 85.13 | 72.31 | 80.00 | 72.31 | 71.56 | 72.85 | 69.51 | 77.08 |
| Non-Hispanic black | 9.74 | 25.00 | 12.73 | 25.00 | 25.69 | 24.50 | 28.66 | 18.75 |
| Other | 5.13 | 2.69 | 7.27 | 2.69 | 2.75 | 2.65 | 1.83 | 4.17 |
Notes: Values in Table 1 are column percentages in the case of multi-category variables and means for continuous and binomial variables. ECHI=employment-contingent health insurance for the respondent, OFFER=respondent was offered ECHI, NOSECHI=respondent’s spouse is not covered by employment-contingent or military health insurance, and NOSOFFER=spouse was not offered (from his employer) employment-contingent health insurance and did not have military health insurance. A few variables are denoted as %’s in the table, to indicate that they have been converted to percentages, instead of their usual standardized scales, to account for instances where some questions that are needed to create the score were not answered by the respondent. Columns within each pair are compared using the χ2 test for multi-category variables and the two-sample t-test for continuous or binomial variables. Missing data: radiation at 2 months (n=17); radiation at 9 months (n=11); chemotherapy at 2 months (n=7); chemotherapy at 9 months (n=7). For these variables, we excluded the missing values when calculating means and performing t-tests, though the missing value observations were included in the following regressions by use of a dummy variable. For some categorical variables (including some binomial variables), there are a few respondents in “don’t know/refused” categories. In these cases, χ2 tests are performed that include these responses in a separate category (though these categories are not reported in the table), and these cases are captured with dummy variables in the regressions that follow. Three respondents refused to give or did not know their husbands’ ages. These observations are excluded from the spouse age means and tests above, though they are included in the following regressions via use of a dummy variable. Percentages calculated and tests performed for health insurance characteristic variables exclude observations for two respondents who were not asked questions about their health insurance due to a survey error. These individuals were included in the regressions, again via the use of a dummy variable. Statistically significant differences are indicated above estimates for variables with multiple categories reported and next to estimates otherwise. Conventional levels of statistical significance are noted as follows:
p<.10,
p<.05,
p<.01.
At the two- and nine-month interviews, the percentages of women employed exceeded 80% and were comparable for women with and without ECHI. At all interviews, women with ECHI worked more weekly hours than women with insurance through a spouse, working an average of 44 hours in the pre-diagnosis period, versus 37 hours for women without ECHI. At the two-month interview, women with ECHI worked an average of 31 hours per week and women without ECHI worked 26 hours per week. And at the final interview, women with ECHI returned to nearly full-time work (on average, 38 hours per week), while women without ECHI worked about 30 hours per week. The difference-in-differences in hours worked between women with ECHI and women with insurance through a spouse, at the two-month and nine-month interviews relative to baseline, were 1.8 and 1.7 hours, respectively, which are relatively small.
In columns 3–8 we present descriptive statistics for the other comparisons we use to estimate the effects of dependence on employment for insurance. As previously explained, these alternative comparisons are intended to use more homogeneous groups of women who are still differentiated by this dependence, to reduce unobservable differences between those who do and do not depend on their job for their health insurance. The statistics in Table 1 speak to differences in observables, but if these differences are smaller it is likely that differences in unobservables follow suit.
Columns 3 and 4 focus on those offered ECHI, distinguishing between those who do and do not take it up. For this comparison, many of the differences that were statistically significant between columns 1 and 2 (for women with and without ECHI) remain statistically significant or large. This is not surprising, because this comparison still focuses on differences between women with and without ECHI, although in more similar jobs where insurance is offered. We therefore might expect job characteristics to be more similar, but not necessarily individual characteristics. That appears to be the case. For example, the firm size distribution is more similar, as are the self-employment rates and job requirements, but the education distribution is more different.
The other two alternative comparisons, in columns 5 through 8, would be expected to yield groups more similar on both job and individual characteristics, and that is true to some extent. For example, the racial distributions are no longer significantly different, nor are the firm size categories in columns 7 and 8. Moreover, for the comparisons in columns 5 through 8 the differences in baseline hours worked are much more similar. Overall, the comparisons in the last two columns (“Alternative 3”) appear most similar, and the comparisons in the last four columns are more similar than the others, suggesting that these alternative comparisons may give us the most reliable estimates of how dependence on one’s job for health insurance affects the labor supply response to a health shock. The key difference we observe in these columns is between spouse characteristics. Women with ECHI and a spouse without the offer of ECHI are more likely to have a spouse that is not working and if working, to work fewer hours, reinforcing the hypothesis that these women have no other alternative for health insurance.
Probability of employment
Table 2 reports estimates of our models explaining the probability of continuing to be employed at the two- and nine-month interviews. In all estimations, the coefficient for ECHI is positive, consistent with women with ECHI being more likely to remain employed, but is statistically significant only in one estimation (column 3), where the estimate implies that women with ECHI were 5.30 percentage points more likely to be employed than women with health insurance through a spouse at the nine-month interview. This specification most closely matches estimations from Bradley et al. (2006).27 In the expanded specification that includes all controls reported in Table 1 (column 4), the ECHI coefficient falls from 5.30 to 2.20 percentage points and is no longer statistically significant.28
Table 2.
Linear probability models of employment at two-month and nine-month interviews, cancer sample
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Two-month interview
|
Nine-month interview
|
|||
| Baseline model | Expanded model | Baseline model | Expanded model | |
| ECHI | 0.013 (0.039) | 0.018 (0.059) | 0.053* (0.030) | 0.022 (0.040) |
| Breast cancer stage: | ||||
| Stage 0 | 0.024 (0.044) | -0.033 (0.058) | −0.077 (0.057) | −0.047 (0.063) |
| Stage II | −0.140*** (0.033) | −0.077 (0.048) | −0.082*** (0.030) | −0.036 (0.031) |
| Stage III or IV | −0.131* (0.067) | −0.100 (0.085) | −0.103 (0.064) | −0.038 (0.045) |
| All control variables from Table 1 included | No | Yes | No | Yes |
Notes: There are 455 observations. Standard errors in parentheses:
p < .1,
p < .05,
p < .01 (two-tailed tests).
ECHI=employment-contingent health insurance. OLS regressions with robust standard errors clustered by physician. Stage I is the omitted cancer stage. Controls in baseline model include age in years, indicator of chemotherapy or radiation observed at any point, pre-diagnosis weekly hours worked, and sets of dummy indicators for race, education level, having children under age 18, household income, whether the respondent’s job is a blue collar job, and year of interview (2007 to 2011). Controls for expanded models include controls used in the baseline model in addition to all other non-labor supply variables reported in Table 1.
Change in weekly hours worked
Table 3 reports estimates for our models explaining the percent change in weekly hours worked from the baseline interview to the two- and nine-month interviews. In the conditional (on employment) estimations of the baseline models for both the two- and nine-month interviews, there is statistically significant evidence that women with ECHI reduced their weekly hours by less than women with health insurance through a spouse (columns 1 and 3), although the magnitudes are not large (about 5 percent). The coefficient estimates remain positive, but are smaller and statistically insignificant in the specifications when other controls are added. The unconditional estimations in columns 5 through 8 mirror these findings, although all of the coefficients become larger because they reflect the combined employment and hours effects.
Table 3.
Percentage change in hours worked, conditional and unconditional on working post-diagnosis, cancer sample
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| Conditional on working | Not conditional on working | |||||||
| N=378
|
N=410
|
N=455
|
||||||
| Two-month interview
|
Nine-month interview
|
Two-month interview
|
Nine-month interview
|
|||||
| Baseline model | Expanded model | Baseline model | Expanded model | Baseline model | Expanded model | Baseline model | Expanded model | |
| ECHI | 0.048** (0.022) | 0.046 (0.029) | 0.059* (0.033) | 0.040 (0.028) | 0.061* (0.036) | 0.053 (0.054) | 0.102** (0.039) | 0.053 (0.049) |
| Breast cancer stage: | ||||||||
| Stage 0 | 0.049* (0.026) | −0.004 (0.041) | 0.048 (0.028) | 0.026 (0.033) | 0.058 (0.051) | −0.039 (0.060) | −0.028 (0.066) | −0.021 (0.073) |
| Stage II | −0.070** (0.030) | −0.048 (0.035) | 0.027 (0.035) | −0.003 (0.039) | −0.184*** (0.035) | −0.104** (0.040) | −0.055 (0.036) | −0.040 (0.041) |
| Stage III or IV | −0.102** (0.046) | −0.010 (0.054) | 0.010 (0.037) | −0.014 (0.036) | −0.201*** (0.064) | −0.102 (0.073) | −0.104 (0.068) | −0.072 (0.052) |
| All control variables from Table 1 included | No | Yes | No | Yes | No | Yes | No | Yes |
Notes: Standard errors in parentheses:
p < .1,
p < .05,
p < .01 (two-tailed tests).
ECHI=employment-contingent health insurance. All regressions estimated using OLS with robust standard errors clustered by physician. Stage I is the omitted cancer stage. Controls are the same as noted in Table 2.
Alternative comparisons
In Table 4, we provide what we regard as more compelling tests of the dependence of labor supply on the need to maintain health insurance, using the alternative comparisons discussed earlier. All models include the full set of controls as reported in Table 1 (the same controls as the “expanded” models in Tables 2 and 3). The first set of regressions (Alternative 1) focuses on those offered ECHI, distinguishing between those who take up ECHI and those who do not. The interaction term OFFER × ECHI is positive in every specification, but is never statistically significant. The positive estimates are consistent with women who are more dependent on their employment for health insurance remaining employed or working more hours following a breast cancer diagnosis.
Table 4.
Labor supply outcomes, alternative specifications of expanded model, cancer sample
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Two-month interview
|
Nine-month interview
|
|||||
| Employment | Percent change in hours, conditional on working | Percent change in hours, unconditional | Employment | Percent change in hours, conditional on working | Percent change in hours, unconditional | |
| Alternative 1 | ||||||
| OFFER | −0.078 (0.099) | 0.023 (0.061) | −0.017 (0.087) | −0.112 (0.068) | 0.086 (0.124) | −0.002 (0.155) |
| OFFER × ECHI | 0.034 (0.059) | 0.040 (0.033) | 0.056 (0.056) | 0.040 (0.038) | 0.022 (0.038) | 0.049 (0.049) |
| Alternative2 | ||||||
| ECHI | −0.022 (0.065) | 0.005 (0.032) | 0.015 (0.063) | 0.018 (0.056) | 0.021 (0.038) | 0.025 (0.065) |
| ECHI × NOSECHI | −0.007 (0.045) | 0.080* (0.042) | 0.073 (0.051) | 0.008 (0.047) | 0.037 (0.043) | 0.056 (0.058) |
| Alternative 3 | ||||||
| ECHI | 0.028 (0.057) | 0.024 (0.028) | 0.040 (0.054) | 0.013 (0.044) | 0.009 (0.027) | 0.012 (0.050) |
| ECHI × NOSOFFER | −0.035 (0.051) | 0.078* (0.043) | 0.048 (0.055) | 0.034 (0.036) | 0.113*** (0.040) | 0.153*** (0.056) |
Notes: Standard errors in parentheses:
p < .1,
p < .05,
p < .01 (two-tailed tests).
ECHI=employment-contingent health insurance for the respondent, OFFER=respondent was offered ECHI, NOSECHI=respondent’s spouse is not covered by employment-contingent or military health insurance, and NOSOFFER=spouse was not offered (from his employer) employment-contingent health insurance and did not have military health insurance. All regressions run using OLS with standard errors clustered by physician, and all include the same set of control variables as what was included in the “expanded” models in Tables 2 and 3. Sample sizes are the same as in Tables 2 and 3, but are reduced by two spouse insurance respondents in regressions that include the variable OFFER because those respondents were not asked if they were offered insurance from their employer due to interviewer error.
The second specification (Alternative 2) focuses on those with ECHI, distinguishing between women whose husbands have employer-provided health insurance. In this specification, a positive coefficient on the ECHI × NOSECHI interaction implies that women with a health shock who are more dependent on their own employment for insurance maintain higher labor supply. The hours estimates are all positive, and in column 2 the estimated coefficient on this interaction – for the change in hours conditional on working at the two-month interview – is statistically significant, indicating that conditional on being employed, women with ECHI but without the option to switch to a spouse’s policy reduce their hours less than women with ECHI whose spouse also has ECHI to which they can likely switch. This evidence is consistent with the hypothesis that dependence on employment for one’s health insurance mutes the labor supply response to breast cancer, although the evidence is not strong and emerges only for some analyses.
In the final set of estimations (Alternative 3), we focus on whether the spouse is offered ECHI rather than whether the spouse has ECHI. We suggested that, on a priori grounds, this comparison might be the most compelling because NOSOFFER better reflects the lack of an option to switch to a spouse’s insurance than NOSECHI, and whether or not the spouse takes up his ECHI may be more of a choice variable; the descriptive statistics in Table 1 support this, as the women we compare in this specification are the most similar on observables. The results in the last two rows of Table 4 provide the strongest evidence consistent with the labor supply hypothesis. For three of the hours specifications there is statistically significant evidence that women more dependent on their own job for health insurance have higher labor supply following a health shock. We find this evidence for hours at both the two- and nine-month interviews, with estimated magnitudes in the 7.8 to 11 percent range (conditional on employment).
Table 5 reports estimates for changes in labor supply from the baseline interview to the two- and nine-month interviews for the sample comprising our study and CPS respondents. The top panel of the table first reports estimates using the cancer sample only, but with the control variables that are common to the CPS and cancer sample (for comparison purposes, since the coefficients estimated in Tables 2 and 3 are based on models with more extensive controls). Relative to the expanded models reported in Tables 2 and 3, the coefficients remained about the same for employment outcomes and became smaller for change in hours worked outcomes.
Table 5.
Labor supply outcomes, cancer and CPS sample
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Two-month interview
|
Nine-month interview
|
|||||
| Employment | Percent change in hours, conditional on working | Percent change in hours, unconditional | Employment | Percent change in hours, conditional on working | Percent change in hours, unconditional | |
| Estimates using CPS controls – cancer sample only | ||||||
| ECHI | 0.011 (0.045) | 0.008 (0.034) | 0.013 (0.047) | 0.041 (0.037) | −0.010 (0.031) | 0.028 (0.043) |
| CPS and cancer samples | ||||||
| ECHI | 0.012 (0.035) | −0.071** (0.031) | −0.052 (0.045) | 0.027 (0.031) | −0.075 (0.047) | −0.042 (0.054) |
| Cancer (BCA) | −0.096** (0.039) | −0.164*** (0.034) | −0.234*** (0.047) | −0.025 (0.034) | −0.065 (0.056) | −0.077 (0.060) |
| Cancer × ECHI | −0.017 (0.047) | 0.082** (0.039) | 0.053 (0.056) | 0.0059 (0.041) | 0.107 (0.073) | 0.103 (0.079) |
Notes: Heteroskedasticity-robust standard errors in parentheses:
p < .1,
p < .05,
p < .01 (two-tailed tests).
CPS=Current Population Survey, BCA=breast cancer and ECHI=employment-contingent health insurance. All regressions run using OLS. The control variables include subject and spouse age, race, and education, household income, the wife’s share of household income, indicator for children under 18, firm size, type, and baseline hours worked for both subject and spouse (with unemployed spouses included using a separate indicator variable), indicator for blue collar occupation for the wife, year of interview dummies, and an indicator for observations where baseline hours worked was based on actual, not usual, hours worked (discussed in the text). The construction of the CPS samples is discussed in the text. See notes to Table 4 for other details on the cancer sample. For employment and unconditional hours regressions, the combined CPS and cancer sample size is 827 and 841 for 2-month and 9-month interviews, respectively (455 come from the cancer sample). For the conditional hours regressions, the 2-month interview sample size is 719 (378 cancer sample); the 9-month sample size is 766 (410 cancer sample).
The second panel adds the CPS sample to the cancer sample and includes an interaction term between cancer and ECHI (equation (5)). As noted above, this is a different way to control for unobserved heterogeneity than the alternative comparisons in Table 4. In this panel, the coefficients on the interaction term BCA × ECHI are positive, with one exception – employment at the two-month interview – and in the case of the percent change in hours worked at the two-month interview is statistically significant, implying that women newly diagnosed with cancer who have ECHI increased their weekly hours relative to women in the control sample with ECHI but without cancer. Moreover, the point estimates are quite similar to those in the bottom row of Table 4, which we argued are the preferred estimates among the alternative comparisons used in that table. Thus, the evidence from the inclusion of the CPS sample supports our findings from the cancer sample alone.
Perceptions of the need to work to keep health insurance
Thus far we focused on observed labor supply responses to ECHI. We also examined responses to questions that ask women directly if they are working to preserve health insurance coverage (Table 6). This information on the perceived link between ECHI and labor supply can provide complementary evidence to what we learn from observed behavior. We present these responses for the same comparisons we used in the regression analysis of labor supply responses.
Table 6.
Reasons for continued employment and hours worked (%), cancer sample
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| Base specification | Alternative 1 | Alternative 2 | Alternative 3 | |||||
|
|
||||||||
| OFFER=1 | OFFER=1 | ECHI=1 | ECHI = 1 | ECHI=1 | ECHI=1 | |||
| Survey question | ECHI=0 | ECHI=1 | ECHI=0 | ECHI=1 | NOSECHI=0 | NOSECHI=1 | NOSOFFER=0 | NOSOFFER=1 |
| Two-month interview | ||||||||
|
| ||||||||
| Are you currently working to maintain health insurance benefits? | 3.70 (N=162) | 62.96*** (N=216) | 3.33 (N=90) | 62.96*** (N=216) | 58.06 (N=93) | 66.67 (N=123) | 57.55 (N=139) | 72.73** (N=77) |
|
| ||||||||
| If you could have the same health insurance without additional cost to you, would you reduce the number of hours you work each week? | 29.33 (N=150) | 48.15*** (N=216) | 27.91 (N=86) | 48.15*** (N=216) | 48.39 (N=93) | 47.97 (N=123) | 48.92 (N=139) | 46.75 (N=77) |
|
| ||||||||
| Nine-month interview | ||||||||
|
| ||||||||
| Are you currently working to maintain health insurance benefits? | 7.02 (N=171) | 66.95*** (N=239) | 11.58 (N=95) | 66.95*** (N=239) | 66.67 (N=99) | 67.14 (N=140) | 64.00 (N=150) | 71.91 (N=89) |
|
| ||||||||
| If you could have the same health insurance without additional cost to you, would you reduce the number of hours you work each week? | 27.04 (N=159) | 49.79*** (N=239) | 30.00 (N=90) | 49.79*** (N=239) | 41.41 (N=99) | 55.71** (N=140) | 45.33 (N=150) | 57.30* (N=89) |
Notes: ECHI=employment-contingent health insurance for the respondent, OFFER=respondent was offered ECHI, NOSECHI=respondent’s spouse is not covered by employment-contingent or military health insurance, and NOSOFFER=spouse was not offered (from his employer) employment-contingent health insurance and did not have military health insurance. For the first question, we report the percentage responding “strongly agree” or “agree.” The second question is a simple yes/no response; the percentage reporting yes is reported. Asterisks indicate statistically significant differences using two- tailed t-tests
p<.10,
p<.05,
p<.01.
Individuals who were not employed and those who refused to answer or responded as ‘don’t know’ are excluded from calculations.
As shown in columns 1 and 2, women with ECHI overwhelmingly perceive that they are working to maintain health. Naturally, women with ECHI almost never report this. For example, at the two-month interview, nearly two-thirds of women (63%) with ECHI report that they strongly agree or agree with the statement that they are working to maintain health insurance, relative to a tiny percentage among those without ECHI. The numbers are virtually the same in columns 3 and 4.
The interesting differences in responses are the comparisons based only on women with ECHI or offered ECHI, where we infer dependence on one’s employment for health insurance based on what might be available through the spouse. In columns 7 and 8, where the comparison is based on whether or not the spouse is offered employer-provided health insurance, among women with ECHI, at the two-month interview women whose spouses are not offered health insurance are about 15 percentage points more likely to report they are currently working to maintain insurance, a statistically significant difference.
When we look at responses about whether women would reduce hours worked if they could have the same insurance without additional cost, we find even more consistent evidence that the need to maintain health insurance constrains labor supply choices of women with breast cancer. For the more reliable and meaningful comparisons – in columns 5 through 8 – which focus on differences among women with ECHI or offered ECHI, there are significant differences at the nine-month interview, with about 13 to 14 percentage points more women whose husbands do not have or are not offered ECHI indicating that are maintaining higher hours than they want to maintain their health insurance.
7. Discussion
The evidence supports the hypothesis that ECHI incentivizes women newly diagnosed with breast cancer to maintain higher labor supply than they would otherwise. The estimated difference in labor supply responses to the health shock is modest – about 8 to 11 percent – and the evidence is somewhat sensitive to the choice of comparison groups. However, the evidence is strongest statistically when we compare women who differ in their dependency on their jobs for continued insurance, but are otherwise most similar in terms of personal and job characteristics, which in our view strengthens the conclusion. In particular, the strongest evidence emerges from comparing women with ECHI, but differentiated only by whether their spouses are offered employer-provided health insurance that would cover the woman if she lost coverage through her employer. The evidence from the inclusion of the CPS sample supports our findings, producing very similar coefficients on the effects of ECHI for women diagnosed with breast cancer. In addition, subjective responses of women diagnosed with breast cancer to questions about whether they are working more to maintain health insurance are consistent with the conclusions from observed behavior.
Our study advances what is known about the relationship between ECHI and labor supply, and has two advantages over prior studies. First, we collected data on a rich set of control variables, including disease and treatment characteristics, job characteristics, and respondent and spouse characteristics, which were used to help rule out competing explanations of the observed effects. Second, we improved upon prior assessments of ECHI’s effect on labor supply (our own included) by using alternative, more homogeneous comparison groups that better identify the effects of dependence on one’s job for health insurance. In general, these alternative comparisons led to stronger evidence that dependence on one’s employment for health insurance moderates labor supply reductions in response to breast cancer.
Our evidence consistently points to smaller labor supply reductions in response to breast cancer for women who depend on their own employment for health insurance, although the magnitudes are modest and in many cases not statistically significant. Our results can be viewed as consistent with the job lock literature, which has generally found modest estimates of the effect of employment-contingent health insurance in reducing job mobility, despite a few early papers that suggested large effects. Our research differs in providing evidence on a different channel by which employer-provided health insurance may constrain worker’s labor market decisions – which we might think of as “hours lock” that constrains labor supply, rather than job lock that constrains job mobility.
In addition to drawing inferences from observed labor supply behavior, we questioned the women in our sample – all of whom had a breast cancer diagnosis – about their motivation to continue employment. Although the responses to these questions may reflect unobserved preferences for both employment and health insurance, women dependent on their own employment for health insurance report that they are working – or are working more – in order to maintain health insurance, which may explain worries related to insurance expressed by participants in qualitative studies of cancer survivorship (Schwartz et al., 2009). Although few women stopped working during the study period, concerns regarding health insurance insecurity are probably well founded given the strong correlation between job loss and loss of health insurance coverage (Cawley et al., 2011).
There are limitations to the study, although there are some justifications for these limitations. First, the study is confined to a single state, which may limit whether it can be generalized to other settings. To mitigate this possibility, we enrolled subjects from academic and private practices and from rural and urban settings. An advantage of focusing on a single state is that women in the sample were most likely subject to similar economic conditions that may affect employment.
Second, we study a single disease where treatment is largely provided on an outpatient basis and is reasonably uniform across practices. Again, this limits generalizability, but it avoids problems from heterogeneity of disease, morbidity, and treatment. These conditions strengthen the internal validity, but at the expense of external validity. Therefore, it would be valuable to gain more knowledge about how health insurance that is tied to one’s job influences labor supply responses to different types of health shocks, particularly those that require long absences from work, although collecting the requisite data, as in our study, is expensive.
Third, we study married women, so the findings may not generalize to single women (or men) who do not have the option to switch to a spouse’s policy, nor to married men who are less likely to have the option to switch to a wife’s policy. Prior work suggests that men will be more constrained by ECHI following the diagnosis of a serious illness because they are likely to have fewer options than women to switch to their spouse’s employer-provided health insurance (Bradley et al., 2011).
Fourth, in spite of our attempts to enroll and study similar groups of women, in the absence of randomization of employees to equivalent ECHI policies and spouse ECHI policies, dissimilarities between the treatment and control groups are inevitable. Dissimilarities can occur between study subjects, comparability of insurance policies, and jobs. We therefore cannot completely rule out bias from selection into different health insurance statuses. Absent an experimental design, we tried to overcome or assess this limitation by studying more similar groups of women. The overall consistency of our findings, and the fact that they are stronger when we use comparisons among more homogeneous groups of women who are still differentiated by how dependent they are on their own employment for health insurance, should bolster confidence in the findings. Nonetheless, we cannot definitively rule out a role for unobserved characteristics that are associated with the offer and acceptance of health insurance through one’s job and subsequent labor supply changes.
The evidence that dependence on employment for health insurance creates an incentive to maintain higher labor supply when faced with a health shock, and that women strongly perceive this incentive, suggests that employer-provided health insurance may lead to anxiety or stress among people who experience a health shock and are dependent on employment for their health insurance. Moreover, the resulting constraint on reducing labor supply may influence treatment decisions and adherence behavior to avoid reducing labor supply as much as might be optimal for recovery. Future research will explore the effects on treatment, adherence, and health consequences of the dependence on employment for health insurance. From a public policy perspective, having better and cheaper options for health insurance outside of the employer may benefit some workers. At the same time, the relatively modest differences we find in labor supply responses to health shocks suggest that providing these options outside the employerbased system are unlikely to trigger substantial reductions in labor supply.
Acknowledgments
Bradley, Neumark, and Barkowski’s research was supported by NCI grant number R01-CA122145, “Health, Health Insurance, and Labor Supply.” The authors are grateful to Myra Owens, Ph.D. and Mirna Hernandez for project coordination, Meryl Motika for programming support, the interviewers and medical record auditors who collected the data, and the many subjects who generously donated their time to the project.
Footnotes
The American Recovery and Reinvestment Act (ARRA) of 2009 provided a premium reduction (to 35% of premiums) for continuation coverage for eligible individuals who were terminated involuntarily from employment through May 31, 2010. Individuals who qualified paid reduced premiums for up to 15 months, as long as they were not eligible for another group health plan or Medicare (U.S. Department of Labor, 2011).
Although not relevant to our study period, the Patient Protection and Affordable Care Act (ACA) will expand Medicaid coverage to very low-income workers who lose employer-provided coverage and allow others without employer-provided coverage to purchase health insurance on exchange markets (Kaiser Family Foundation, 2011).
The spouse insurance group includes a handful of women covered by their spouse’s military insurance (5 of the 195 women in the final sample coded as spouse insurance).
There were 28 women in the sample who did not receive chemotherapy or radiation.
This sample size was larger than what we needed to detect the effect size for changes in hours of work based on the prior evidence.
The factor most responsible for exclusion from the sample was age greater than or equal to 65.
Treatment for metastatic disease is generally palliative without clear rules for when to stop chemotherapy.
The higher incidence of stage III cancer among dropouts may lead to more muted labor supply reductions overall in the study sample, but should not affect differences associated with ECHI.
The error rate was defined as the number of incorrectly-entered responses out of all questions. The total number of questions varied, depending on the skip patterns for a particular subject.
The questionnaire is available upon request.
The CPS follows households over time, not individuals; therefore, the matching of records for individuals over time occurs with some error. Our matching algorithm is nearly the same as that proposed by Madrian and Lefgren (2000). Subjects were matched across surveys by comparing individual roster numbers that are retained from one survey month to the next. We matched sex, race, and age (allowing a difference of minus one to plus three years) from one roster number to the next to ensure that the correct individual answered each survey.
CPS respondents are interviewed for four months (MIS 1–4), not interviewed for eight months, and then interviewed for another four months (MIS 5–8). Thus, respondents who were MIS 3, 4, 7, or 8 in March were excluded from our two-month CPS sample because they were out of the CPS sample during the follow-up observation period for our sample.
More specifically, MIS 4 March records were matched to MIS 5 records from December. These records construct the sample of individuals with a nine-month gap. Records with 10-month gaps result from matching March MIS 3 with January MIS 5. Likewise, MIS 2-MIS 5 and MIS 1-MIS 5 pairs result in the 11- and 12-month gap records. We did not allow individuals to appear more than once in the sample, which is why we did not match, for example, March MIS 4 records with their MIS 5, MIS 6, MIS 7, and MIS 8 records. This would have resulted in the same individual having four records – each with varying gaps – but which would have been highly dependent on each other.
One subject was dropped from the two-month sample because there was a 4,400% increase in hours worked reported.
Breast cancer stage was determined using the American Joint Commission on Cancer staging criteria, which incorporates Tumor, Node, and Metastases. Cancer stage is used to decide treatment course and is the best indicator of prognosis.
We also modeled whether women worked more than a particular hours threshold, using four different specifications (weekly hours ≥ 20, ≥ 30, ≥ 35, and ≥ 40). In all cases except one, the estimates were positive, but statistically insignificant (results not shown).
The cancer sample contained 29 self-employed women, among whom only six had ECHI. The employment and weekly hours worked models were estimated without these women and the results were qualitatively unchanged (results not shown).
Many women reported having full or partial sick leave for four or more months, which most likely reflects the availability of short-term disability leave. The inclusion of these variables in the models did not alter the conclusions.
This is coded as a linear term from zero to three (1 = looking; 2 = applied; 3 = contacted employer or interviewed).
The notes to Table 2 explain the differences in control variables between these specifications.
Our use of data on the offer of ECHI parallels the concerns that motivate the approach taken in Gilleskie and Lutz (2002), although they explicitly model potentially endogenous variables as outcomes that are chosen jointly and influenced by common fixed and time-varying unobserved heterogeneity.
Results discussed in the paper but not shown in the included tables are available from the authors upon request.
This assumes that the husbands’ employer-provided insurance policy offers coverage for wives. We do not know this for everyone in the sample. But combining those women who get insurance through their spouse with those that do not but who were explicitly asked about family coverage, 97% of those whose husbands were offered insurance through their employer could cover their spouses.
This parallels the approach taken by Madrian (1994), and has been used by several other authors in the job lock literature. It might seem more straightforward to include an interaction between ECHI and a dummy variable indicating spousal coverage (labeled SECHI – the opposite of NOSECHI). In that case, though, we would be testing for a negative effect. We find it simpler to use specifications that uniformly predict a positive coefficient on the variable indicating that a woman is reliant on her own employment for insurance, in part to parallel our other specifications. Note also that the same discussion surrounding equation (4) applies here; in this case we could condition on ECHIi1 = 1 and estimate the effect of NOSECHI for this subsample.
The ability to switch immediately given a pre-existing condition assumes that a woman had been enrolled in her own employer’s insurance long enough to amass 12 months of “creditable coverage.” Even if the woman did not have a full 12 months of creditable coverage, her waiting period to enroll in her husband’s insurance would be reduced by the amount of creditable coverage that she had. Our survey did not collect information on how long women held their ECHI. We do know, though, that among the 260 women in our cancer sample who held ECHI, only 11 had job tenure of less than a year as of the time of their diagnosis. Thus, it seems likely that a very high percentage would not have face any waiting period to switch to their husbands’ insurance.
There is one other control included in the hours specifications. Most hours responses are based on the question “how many hours did you usually work last week?” In a small number of cases people reported “varies.” For these cases, we used their response to the question “how many hours did you actually work last week?” We include a dummy variable indicating when the actual hours worked question was used.
In Bradley et al. (2006), women with ECHI were 10 percentage points more likely to be employed at six months following diagnosis, but this estimate was not statistically significant. At 12 months following diagnosis, women with ECHI were 13 percentage points more likely to be employed than women without ECHI (p < .05).
We tested specifications in which we included interaction terms between cancer stage and ECHI. Coefficients on these estimates were not statistically significant (results not shown). The full estimates including the coefficients of all the control variables are available upon request.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Cathy J. Bradley, Email: cjbradley@vcu.edu, Professor, Department of Healthcare Policy and Research and the Massey Cancer Center, Virginia Commonwealth University, Richmond, VA
David Neumark, Email: dneumark@uci.edu, Chancellor’s Professor, Department of Economics, and Director, Center for Economics & Public Policy, University of California, Irvine, CA; Research Associate, National Bureau of Economic Research; and Research Fellow, IZA
Scott Barkowski, Email: scott.barkowski@uci.edu, Ph.D. candidate, Department of Economics, University of California, Irvine, CA.
References
- Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Bradley CJ, Neumark D, Luo Z, Bednarek H. Employment-based health insurance, illness, and labor supply of women: evidence from married women with breast cancer. Health Economics. 2006;16(7):719–734. doi: 10.1002/hec.1191. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Neumark D, Luo Z, Schenk M. Employment and cancer: findings from a longitudinal study of breast and prostate cancer survivors. Cancer Investigation. 2007;25(1):47–54. doi: 10.1080/07357900601130664. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Neumark D, Motika M. The effects of health shocks on employment and health insurance: the role of employer-provided health insurance. International Journal of Health Care Finance and Economics. 2012;12(4):253–267. doi: 10.1007/s10754-012-9113-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Moriya AS, Simon KI. The impact of the macroeconomy on health insurance coverage: evidence from the great recession. [Accessed April 26, 2012];National Bureau of Economic Research Working Paper 17600. 2011 http://www.nber.org/papers/w17600.pdf.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Disease. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cooper PF, Monheit AC. Does employment-related health insurance inhibit job mobility? Inquiry. 1993;30(4):400–416. [PubMed] [Google Scholar]
- Gabel JR, McDevitt R, Lore R, Pickreign J, Whitmore H, Ding T. Trends in underinsurance and the affordability of employer coverage, 2004–2007. Health Affairs. 2009;28(4):w595–606. doi: 10.1377/hlthaff.28.4.w595. [DOI] [PubMed] [Google Scholar]
- Gilleskie DB, Lutz BF. The impact of employer-provided health insurance on dynamic employment transitions. The Journal of Human Resources. 2002;37(1):129–162. [Google Scholar]
- Hassett MJ, O’Malley AJ, Keating NL. Factors influencing changes in employment among women with newly diagnosed breast cancer. Cancer. 2009;115(12):2775–2782. doi: 10.1002/cncr.24301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J. Kaiser Family Foundation. [Accessed January 26, 2012];Focus on health reform: summary of coverage provisions in the Patient Protection and Affordable Care Act. 2011 http://www.kff.org/healthreform/upload/8023-R.pdf.
- Johnsson A, Fornander T, Rutgvist LE. Olsson M. Work status and life changes in the first year after breast cancer diagnosis. Work. 2011;38(4):337–346. doi: 10.3233/WOR-2011-1137. [DOI] [PubMed] [Google Scholar]
- Kapur K. The impact of health on job mobility: a measure of job lock. Industrial and Labor Relations Review. 1998;51(2):282–298. [Google Scholar]
- Madrian B. Employment-based health insurance and job mobility: Is there evidence of job lock? The Quarterly Journal of Economics. 1994;109(1):27–54. [Google Scholar]
- Madrian B, Lefgren L. An approach to longitudinally matching Current Population Survey (CPS) respondents. Journal of Economic and Social Measurement. 2000;26(1):31–62. [Google Scholar]
- Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Graff J, Katz SJ. Racial/ethnic differences in job loss for women with breast cancer. Journal of Cancer Survivorship. 2011;5(1):102–111. doi: 10.1007/s11764-010-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute (a) [Accessed November 10, 2011];Estimated US cancer prevalence. 2011 http://cancercontrol.cancer.gov/ocs/prevalence/prevalence.html#allsites.
- National Cancer Institute (b) [Accessed November 22, 2011];SEER Stat Fact Sheets: Breast. 2011 http://seer.cancer.gov/statfacts/html/breast.html#incidence-mortality.
- Schwartz K, Claxton G, Martin K, Schmidt C. [Accessed April 26, 2012];Spending to survive: cancer patients confront holes in the health insurance system. 2009 http://www.kff.org/insurance/upload/7851.pdf.
- Stephan P. [Accessed November 10, 2011];Breast cancer treatment and recovery times: treatment schedule and time management during breast cancer. 2010 http://breastcancer.about.com/od/whattoexpect/a/Breast-Cancer-Treatment-Recovery-Times.htm.
- Tunceli K, Short PF, Moran JR, Tunceli O. Cancer survivorship, health insurance, and employment transitions among older workers. Inquiry. 2009;46(1):17–32. doi: 10.5034/inquiryjrnl_46.01.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Labor, Bureau of Labor Statistics. [Accessed 9 Nov 2012];Technical Paper 63RV Design and Methodology. 2002 http://www.census.gov/prod/2002pubs/tp63rv.pdf.
- United States Department of Labor Employee Benefits Security Administration. [Accessed January 26 2012];COBRA continuation coverage assistance under ARRA. 2011 http://www.dol.gov/ebsa/COBRA.html.
- United States Department of Labor Wage and Hour Division. [Accessed April 26, 2012];Family and Medical Leave Act. 2012 http://www.dol.gov/whd/fmla.
- Ware JE, Snow KK, Kosinski M, editors. SF-36 Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- Weiss DJ, Dawis RV, England GW. Manual studies in vocational rehabilitation. Manual for the Minnesota Satisfaction Questionnaire. 1967;22:1–120. [Google Scholar]