Abstract
Pancreatic cancer is a deadly disease killing 37,000 Americans each year. Despite two decades of research on treatment options, the chances of survival are still <5% upon diagnosis. Recently, chemopreventive strategies have gained considerable attention as an alternative to treatment. We have previously shown significant in vitro chemopreventive effects with low dose combinations of aspirin (ASP), curcumin (CUR) and sulforaphane (SFN) (ACS) on pancreatic cancer cell lines. Here, we report the results of 24-week chemopreventive study with the oral administration of ACS combinations on the N-nitrosobis (2-oxopropyl) amine (BOP)-treated Syrian golden hamster model to suppress the progression of pancreatic intraepithelial neoplasms (PanINs) using (1) unmodified (free drug) combinations of ACS, and (2) nanoencapsulated (solid-lipid nanoparticles; SLN) combinations of ASP, CUR and free SFN. The use of three different doses (low, medium and high) of unmodified ACS combinations exhibited reduction in tumor incidence by 18%, 50% and 68.7% respectively; whereas the modified nano-encapsulated ACS regimens reduced tumor incidence by 33%, 67% and 75%, respectively, at 10X lower dose compared to the free drug combinations. Similarly, while the unmodified free ACS demonstrated a notable reduction in cell proliferation, the SLN encapsulated ACS regimens, showed significant reduction in cell proliferation at 6.3%, 58.6 % and 72.8 % as evidenced by PCNA expression. Cell apoptotic indices were also up regulated by 1.5X, 2.8X and 3.2X respectively, compared to BOP control. These studies provide a proof-of-concept for the use of an oral, low dose, nanotechnology-based combinatorial regimen for the long term chemoprevention of pancreatic cancer.
Keywords: Chemoprevention, Pancreatic cancer, Syrian golden hamster, Solid lipid nanoparticles
Introduction
Pancreatic cancer is a lethal malignancy with an overall 5-year survival rate of <5% making it the fourth major cause of cancer deaths in United States. In 2012, it was estimated that more than 43,920 Americans would be diagnosed with pancreatic cancer, of which 37,390 were expected to succumb to this disease (1). Early detection is difficult and by the time the disease is recognized, it is often too late to help the patient clinically. The dismal prognosis attributed to its aggressive local invasion, early metastases, and low responsiveness to conventional chemotherapies, indicate that efforts should be directed at developing novel strategies such as chemoprevention to reverse, suppress, prevent or delay the progression of pancreatic cancer (2, 3).
Recently, there has also been an increasing interest to use a combination of low doses of several chemopreventive agents that differ in their mode of action and targeting multiple pathways to increase their efficacy with less toxicity. We recently successfully demonstrated combinations of aspirin (ASP), folic acid (FA) and calcium (C) (AFAC) to be effective in the prevention of colon cancer in vitro as well as in vivo in azoxymethane-treated rats when encapsulated in poly-lactide-co-glycolide (PLGA) nanoparticles (4, 5). Subsequently, a new in vitro study conducted in our lab on multiple pancreatic cancer cell lines demonstrated that well known chemopreventive agents aspirin (ASP), curcumin (CUR) and sulforaphane (SFN) when combined and encapsulated in solid lipid nanoparticles (SLNs) were able to reduce the cancer cell proliferation more effectively compared to the free forms of the drugs (6, 7).
Epidemiologic evidence from both in vitro and in vivo studies has demonstrated that inflammation represents an important role in the carcinogenesis of many cancers including pancreatic cancer (8). The transcription factor nuclear factor-κB (NF-κB) has been linked with suppression of cell proliferation, invasion, angiogenesis, and metastases in pancreatic cancer (9). Non-steroidal anti-inflammatory drugs (NSAIDs) such as ASP, nimesulide, sulindac and indomethacin can significantly affect the development of pancreatic cancer in animal models by targeting inflammatory pathways (10–13). This makes it an important target for pancreatic cancer chemoprevention. The mechanisms of action of ASP have shown to inhibit proliferation, induce G1 cell cycle arrest in human pancreatic cancer cell lines and thereby induce apoptosis. However, the recent epidemiologic studies of ASP in pancreatic cancer reached conflicting findings suggesting the need for further studies on this drug (14–16).
Curcumin (diferuloylmethane) is a bioactive component of the spice turmeric extracted from the rhizomes of the plant curcuma longa. CUR has been extensively studied for the numerous biological activities over the last few decades (17). Many pharmacological and clinical studies support the fact that CUR has chemopreventive and anti-proliferative activity against a variety of human cancers including pancreatic cancer (18–20). Inhibition of COX-2, cell growth and induction of apoptosis are the common mechanisms by which CUR shows its anticancer effects (21). Recent phase II clinical trials of CUR (8g daily dose) in patients with advanced pancreatic cancer showed that oral CUR is well tolerated and, despite its limited absorption, has biological activity in some patients with pancreatic cancer (22).
Sulforaphane, a sulfur-containing isothiocyanate is a major compound found in cruciferous vegetables like broccoli to possess chemopreventive activity (23). Previous studies suggest that SFN modulates multiple targets, which regulate many cellular activities including oxidative stress, apoptosis induction, cell cycle arrest, angiogenesis and metastasis suppression, and detoxification of carcinogens (24). A recent study highlighted the effectiveness of SFN in eradication of pancreatic tumor initiation cells and its ability to potentiate the antitumor effects of the human tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) by repression of NF-κB activity (25).
Nanoparticles are increasingly being used as drug delivery platforms. Solid-lipid nanoparticles (SLN), a novel nanotechnology-based drug delivery system has received considerable attention in the last few years as a promising method of delivering drug encapsulated nanoparticles into the body at a controlled release rate. SLNs are characterized by a solid lipid core and stabilized by surfactants. They are generally solid at physiological temperatures, stable, biocompatible and biodegradable (26). Stearic acid, a fatty acid lipid has been commonly used as a raw material for the manusfacture of SLNs. Stearic acid is an FDA approved compound with generally recognized as safe (GRAS) approval for use in food products (27, 28). Based on previous studies conducted in our lab (6), we believe that SLNs are extremely suited towards pancreatic cancer chemoprevention. This is due to better control on the release of drugs, significant decrease in renal and hepatic clearance, decreased immune recognition and increased half-lives of drugs. However, the most important feature of solid-lipid nanoparticles (SLN) especially in the pancreatic cancer chemoprevention is that they are absorbed via the lymphatic circulation thereby increasing the circulation time and bioavailability of drugs (29). This allows the administration of lower doses with less chances of toxic side effects, while maintaining their chemopreventive efficacy. Thus, for the first time, an SLN encapsulated combined chemopreventive regimen has been used to study the in vivo utility of this regimen in the chemoprevention of pancreatic cancer using the hamster animal model.
The Syrian golden hamster model exhibits many morphologic and molecular features of human pancreatic cancer progression and has commonly been used as an in vivo model in pancreatic cancer studies. Recent reports in literature have used the hamster model to study the effects of porcine pancreatic enzymes in the prevention pancreatic cancer (30). Other studies have used the hamster model design for cancer chemopreventive purposes using different drug regimens and for imaging purposes to detect early pancreatic cancer (11, 31, 32). Pancreatic intraepithelial neoplasia (PanINs) lesions such as the low grade PanIN1 and PanIN2 develop into more malignant PanIN3 and pancreatic cancer following the administration of a carcinogen BOP, one of the few carcinogens that cause pancreatic neoplasia in rodents (33, 34). Syrian golden hamsters treated with BOP show a progression from mild hyperplasic lesions (PanIN1) at 8 weeks to papillary hyperplasia (PanIN2) and carcinoma in situ (PanIN3) at 20 weeks post injection (35). Overall, the hamster model continues to be widely accepted as a viable in vivo model for pancreatic cancer research as reported in recent literature.
Thus, the objective of our research was to use a novel solid-lipid nanoparticle (SLN) nanotechnology-based oral delivery system to encapsulate a combinatorial regimen of ASP, CUR with free SFN (ACS) to evaluate the in vivo chemopreventive effects against N-nitrosobis (2-oxopropyl) amine (BOP) induced pancreatic carcinogenesis in the Syrian golden hamster model.
Materials and Methods
Animals and reagents
The chemopreventive agents ASP, CUR and SFN were obtained from LKT laboratories (St. Paul, MN). For the in vivo studies, male Syrian golden hamsters were purchased from Harlan laboratories (Indianapolis, IN). The carcinogen N-nitrosobis (2-oxopropyl) amine (BOP) was obtained from Santa Cruz Biotechnology (Santa Cruz, CA). For the preparation of nanotechnology-based chemopreventive regimens, stearic acid (lipid) and poloxamer 188 (emulsion stabilizer) was purchased from Spectrum Chemicals (Gardena, CA). Dichloromethane (DCM) was purchased from Fisher Scientific (Houston, TX). Proliferating cell nuclear antigen (PCNA) antibody was obtained from Cell Signaling Technology (Boston, MA). TUNEL apoptosis detection kit used to detect apoptotic cells was obtained from GenScript (Piscataway, NJ).
Hamster study design
The study was conducted on male Syrian golden hamsters, 4–5 weeks old with an average body weight of ~100 g. All studies were conducted as per protocol approved by the Western University of Health Sciences Institutional Animal Care and Use Committee and conformed to the “Principles of Laboratory Animal Care”. Hamsters were observed daily for any signs of illness and weighed weekly throughout the experimental period. Animal health records were maintained according to USDA guidelines. The hamsters were administered five consecutive weekly subcutaneous injections (35 mg/kg initial dose; 20 mg/kg remaining doses) of the carcinogen BOP to initiate PanIN lesions in the pancreas. All animals were divided into two sets as follows:
Set 1: As indicated in Table 1, this set consisted of five groups (T1–T5) of hamsters. The treatment groups T3–T5 received three different doses (low, medium and high) of ACS chemopreventive combination regimen daily via oral gavage. Therapy was started on the day of the initial BOP injection and continued every 24 h for 24 weeks. Two groups of control animals, saline (T1) and BOP-treated (T2), serving as (−) and (+) controls respectively, were also included. The highest dose selected for ASP, CUR and SFN regimen was 200, 450 and 16 mg/kg respectively which was determined based on current evidence in literature (3, 19, 22, 36, 37). The medium and low doses were calculated as 1/3 and 1/10 of the high dose of chemopreventive agents.
Set 2: Based on results obtained from Set 1 studies, a study of drugs encapsulated in nanoparticles was conducted (Set 2, Table 1). This set had a total of six groups, three groups (n=6) served as saline (T6), blank SLN (T7) control groups and BOP carcinogen group (T8). The other three groups T9–T11 received three different doses (low, medium and high) of the SLN combination regimens. Based on previous studies on cell lines in our lab, the dose for this set was determined to be 10 times (10X) lower compared to the unmodified drug regimens in Set 1.
Table 1.
Treatment plan showing group of hamsters treated with unmodified (Set 1) and SLN modified nanoparticle (Set 2) forms of chemopreventive agents ASP, CUR and SFN at various doses.
| Set 1 | |||
|---|---|---|---|
| Group | Treatment plan | Dose, mg/kg | |
| T1 | Saline control | Saline (control) | 0 |
| T2 | BOP control | BOP | 35 (1st week) / 20 (next 4 weeks) |
| T3 | Low dose ACS | ASP+CUR+SFN | 20 + 45 + 1.6 |
| T4 | Medium dose ACS | ASP+CUR+SFN | 70 + 150 + 5 |
| T5 | High dose ACS | ASP+CUR+SFN | 200 + 450 + 16 |
| Set 2 | |||
| T6 | Saline control | Saline (Control) | 0 |
| T7 | Blank SLN control | Blank SLN (Vehicle control) | 0 |
| T8 | BOP control | BOP | 35(1st week) / 20(next 4 weeks) |
| T9 | Low dose SLN ACS | ASP+CUR+SFN | 2 + 4.5 + 0.16 |
| T10 | Medium dose SLN ACS | ASP+CUR+SFN | 7 + 15 + 0.5 |
| T11 | High dose SLN ACS | ASP+CUR+SFN | 20 + 45 + 1.6 |
Abbreviations: ASP, aspirin; CUR, curcumin; SFN, sulforaphane; BOP, N-nitrosobis (2-oxopropyl) amine; SLN, solid lipid nanoparticles.
Preparation of solid lipid nanoparticles (SLNs)
SLNs were prepared using a hot melt oil-in-water (o/w) emulsion technique (38). Stearic acid was used as the lipid to make the nanoparticle formulation. At first, 1g of stearic acid was melted by heating in a water bath at 70–80° C. The drug (100 mg) was suspended in 3 ml of dichloromethane (DCM). The suspended drug solution was then added to the melted stearic acid and heated until all the DCM was evaporated. The water phase consisted of 1.0% poloxamer solution which was heated to the same temperature as that of the oil phase. The oil phase was then added to the poloxamer solution and the mixture was further sonicated for 5 min using an ultra-sonicator (Branson, Los Angeles, CA) to create an o/w emulsion. The emulsion formed was then cooled and washed with water to remove any impurities. SLNs were freeze-dried (Labconco, Kansas City, MO) and subjected to particle sizing and encapsulation efficiency determination. For the current study, ASP and CUR were encapsulated within SLNs whereas SFN was used in its free, unmodified form. SFN has been demonstrated to have high absorption potential of ~75% from the jejunum and ability to reach micromolar concentrations in the blood. Thus, it was not encapsulated for this project due to its high efficacy (39, 40).
Histological examination
All organs of the thoracic and abdominal cavities were carefully examined in situ macroscopically after euthanization. Four anatomical parts of the pancreas (gastric, splenic, duodenal lobes and head portion) were fixed in 10% phosphate-buffered formalin for 24 h. The formalin-fixed pancreata were cut into small pieces at 2 cm intervals. 4-μm thick sections were processed routinely and stained with H&E. Two independent investigators blinded to sample identity evaluated the sections of pancreas and scored them according to PanIN criteria within the following categories: PanIN1, PanIN2, PanIN3 and carcinoma (41). Cancer incidence (percentage number of hamsters with pancreatic cancer) and multiplicity (number of pancreatic cancers per hamster) were calculated based on these scores.
Immunohistochemistry (IHC)
Paraffin-embedded sections of pancreatic tissue were deparaffinized, rehydrated, and heated in citrate buffer (pH 6.0) for 20 min for antigen retrieval. Subsequently, 10% normal goat serum blocking buffer was applied. The blocking buffer was removed after 1h of incubation in humidified chamber and primary antibody was added to the slides, incubated overnight at 4° C. The secondary antibody was then added and incubated for 90 min at room temperature. Proliferating cell nuclear antigen (PCNA; Cell Signaling Technology) was used as a primary antibody.
Terminal deoxyribonucleotide transferase-mediated nick-end labeling (TUNEL) staining
TUNEL staining was conducted using the TUNEL apoptosis detection kit (GenScript, Piscataway, NJ) following the manufacturer's protocol. Briefly, 4-um-thick formalin-fixed, paraffin-embedded tissue sections were deparaffinized and rehydrated. Endogenous peroxidase activity was quenched by hydrogen peroxide and tissue protein was hydrolyzed with proteinase K. Positive control sections were treated DNase I 1,000units/mL and negative control sections were incubated with label solution (without terminal deoxynucleotidyl transferase enzyme). All the other sections were incubated with TUNEL reaction mixture (fluorescein-labeled nucleotides) at 37° C for 1 hour in a humidity chamber, mounted and observed under a fluorescence microscope.
Evaluation of staining
A minimum of 10 microscopic fields per section were counted manually by two independent investigators blinded to sample identity. For PCNA staining, the nuclear staining in red was considered labeled/positive and nuclear staining in blue as unlabeled/negative staining. For TUNEL assay staining, the nuclear staining in green was considered positive/apoptotic. The proliferative and apoptotic indices were calculated as number of positive cells in lesions divided by the total cell number counted multiplied by 100.
Statistical analysis
The data were expressed as mean ± SE. Differences between treatment and BOP controls were analyzed by ANOVA followed by Dunnett's multiple comparison test. Difference between treatment and BOP controls in PanIN count was analyzed by 2-way ANOVA followed by a Bonferroni post hoc analysis using Graph pad prism software. p ≤ 0.05 was considered statistically significant.
Results
General observations
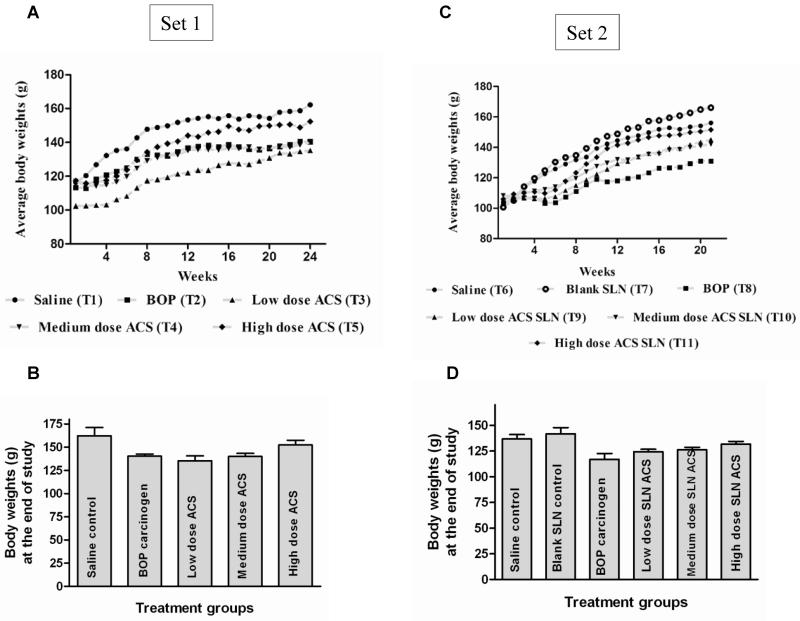
All the hamsters were weighed weekly over the 24-week study period to observe for signs of weight loss. Overall the body weight transition curves of all the hamster groups showed a steady gain from start to end of the study period. In set 1, the saline control, BOP carcinogen control, medium and high dose ACS groups had a mean body weight of ~115g while the low dose ACS group showed ~102g at the start of the study. At the end of the study, the mean body weight gain in the range of ~20–40% was observed, indicating overall good health of hamsters during the study (Figure 1A–1B). In the SLN encapsulated ACS regimen (Set 2), at the start of the study hamsters in all the groups (T6–T11) had a mean body weight of ~ 104g. At the end of the study, a body weight gain in the range of ~30–60% was observed, again indicating good health of hamsters during the study period (Figure 1C–1D). Additionally, no statistical difference was found between control group and ACS combination treated groups as determined by oneway ANOVA followed by Dunnett's multiple comparison test post hoc analysis.
Figure 1.
Body weight variations of hamsters during the ACS treatment period. (A and C) Average body weight transitions of hamsters over the 24-week treatment period. (B and D) Average body weight of hamsters at the end of the study. The statistical significance was determined by one-way ANOVA followed by Dunnett's multiple comparison test post hoc analysis.
ACS combination regimen significantly inhibits BOP-induced pancreatic carcinogenesis
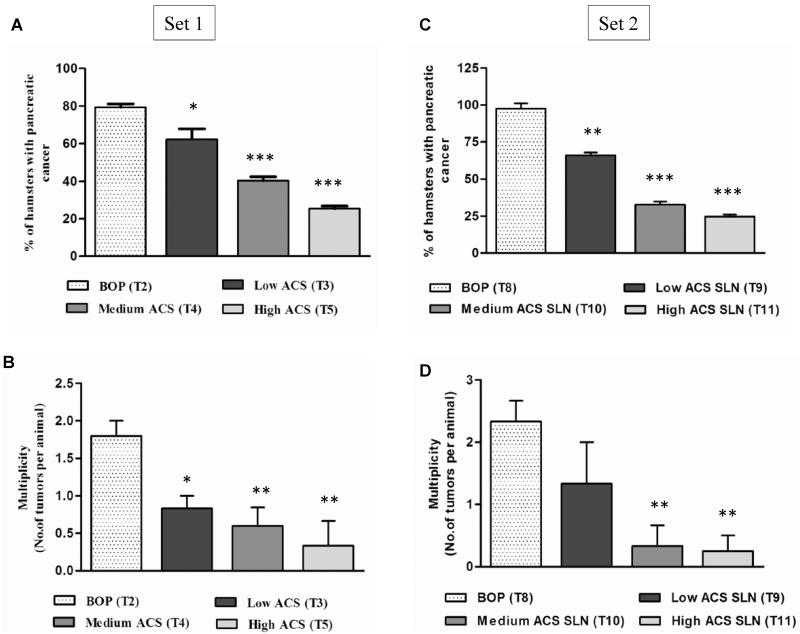
The chemopreventive efficacy of the unmodified ACS (Set 1) combination regimen was evaluated based on tumor incidence and multiplicity. As shown in Figure 2A, the BOP-treated group (T2) exhibited tumor incidence of 80% (percentage of hamsters with pancreatic cancer); whereas the low dose (T3) treatment group had an incidence of 66.6% (p>0.05; NS); the medium (T4) and high dose (T5) ACS groups showed significantly low incidence of 40% (p<0.05; 50% reduction compared to BOP group) and 25% (p<0.001; 68.7% reduction) respectively as determined by histological analysis. Whereas for tumor multiplicity (number of pancreatic cancers per hamster) (Figure 2B), the T2 group showed a tumor multiplicity of 1.8 ± 0.2 whereas T3, T4 and T5 treatment groups exhibited significantly (p<0.05) reduced multiplicity of 0.83 ± 0.17 (54% reduction), 0.6 ± 0.24 (67% reduction) and 0.33 ± 0.29 (82% reduction) compared to T2 group, respectively. These results show that the medium and high doses of ACS combination regimen were effective in reducing cancer incidence and multiplicity when compared to the BOP carcinogen treated control group of hamsters.
Figure 2.
Effect of ACS combination treatment on pancreatic tumor incidence and tumor multiplicity. (A and C) Tumor incidence is determined by percentage of animals with pancreatic cancer. (B and D) Tumor multiplicity is calculated as number of pancreatic cancers per hamster. The Statistical significance was determined by one-way ANOVA followed by Dunnett's multiple comparison test post hoc analysis. *, p<0.05; **, p<0.01; ***, p<0.001 represents statistical significance between BOP (N-nitrosobis (2-oxopropyl) amine) carcinogen control and ACS treatment groups.
In SLN encapsulated ACS regimen (Set 2) (Figure 2C), the BOP-treated hamster group (T8) exhibited tumor incidence of 100%; whereas the low dose ACS SLN group (T9) had an incidence of 66.66% (p>0.05; NS); the medium (T10) and high dose (T11) ACS SLN groups showed significantly low incidence of 33% (p<0.01; 67% reduction compared to T8 group) and 25% (p<0.01; 75% reduction) respectively as determined by histological analysis. The BOP control group (T8) showed a tumor multiplicity of 2.3 ± 0.3, whereas low dose ACS SLN group (T9) showed multiplicity of 1.33 ± 0.7 (p>0.05; NS); medium (T10) and high dose (T11) ACS SLN treatment groups exhibited significantly reduced multiplicities of 0.7 ± 0.67 (p<0.05; 69% reduction compared to BOP control) and 0.25 ± 0.2 (p<0.05; 89% reduction) respectively (Figure 2D).
ACS chemopreventive regimen delays the progression of PanINs into adenocarcinoma
The isolated pancreatic tissues were subjected to H&E staining and different grades of PanINs were counted upon histological examination based on an established classification system for pancreatic duct lesions. PanIN1s are flat epithelial lesions composed of tall columnar cells with basally located nuclei or a papillary pseudo-stratified architecture (42). Further progression of PanIN1s results in formation of PanIN2s which are flat or papillary mucinous epithelial lesions with nuclear abnormalities which may include some loss of polarity, nuclear crowding and enlarged nuclei. Finally, PanIN3s, resulting from PanIN2 lesions are identified as papillary or micro-papillary structures characterized with high grade dysplasia and loss of nuclear polarity indicating development of pancreatic cancer. Based on the above criteria and upon histological examination of H&E stained pancreatic tissues, PanINs were counted in the pancreatic tissues (Figure 3A–3E).
Figure 3.
Hematoxylin and eosin (H&E) staining of pancreatic tissues. Representative figures showing (A) Normal pancreatic ducts and epithelia in saline group (T6); (B) PanIN3 lesions in BOP (N-nitrosobis (2-oxopropyl) amine) carcinogen control group (T8); (C) PanIN2 lesions in low dose SLN ACS treated group (T9); (D) PanIN1 lesions in medium dose SLN ACS group (T10); (E) Low grade PanINs in high dose SLN ACS group (T11) was observed. All the pictures were taken at 200X magnification.
As shown in figures 3A–3E, the highest grade of PanINs in each treatment group was used as a representative image. The saline group, as expected, showed normal pancreatic epithelial cells and ducts (Figure 3A), while the BOP (Figure 3B) and three ACS SLN treatment groups (Figure 3C (low); 3D (medium) and 3E (high)) showed varying regions of normal epithelia and different grades of PanINs. BOP treated hamsters developed pancreatic cancer upon the progression of PanINs, ranging from PanIN1s (low grade) to PanINs 2 and 3 (high grade). PanIN3 is shown as a representative image in Figure 3B characterized by loss of nuclear polarity and the appearance of “budding off” of small clusters of epithelial cells into the lumen. The low dose treatment group exhibited the highest number of PanIN2 lesions (Figure 3C) characterized by enlarged nuclei and nuclear crowding, whereas medium and high dose groups was represented by PanIN1 lesions characterized by small, oval shape nuclei and oriented to basal membrane (Figures 3D and 3E).
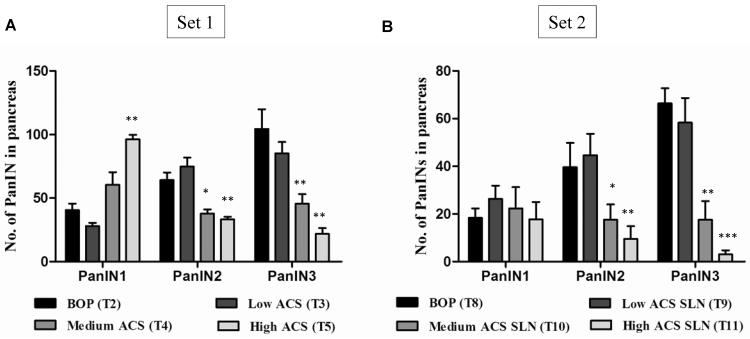
In Set 1, the BOP carcinogen group (T2) showed an average of 41 PanIN1, 65 PanIN2 and 105 PanIN3 lesions (Figure 4A). In comparison, the unmodified ACS low dose group (T3) showed an average of 28 PanIN1, 85 PanIN2 and 78 PanIN3 lesions with no statistical significance in treatment compared to the BOP control group. The unmodified ACS medium dose group (T4) showed an increase in PanIN1 lesion count to 61 but a significant decrease in PanIN2 (38; p<0.05) and PanIN3 (46; p<0.001) lesion formation compared to the T2 group. Finally, the unmodified ACS high dose group (T5) also showed an increase in PanIN1 (97; p<0.001) lesions with a significant decrease in PanIN2 (34; p<0.05) and PanIN3 (22; p<0.001) lesions compared to the T2 (Figure 4A). Thus, the efficacy of the medium and high dose treatment groups were apparent whereby the ACS combination regimens reduced the transformation, and therefore progression, of low grade PanIN lesions to a higher grade variety, hence potentially arresting the onset of pancreatic carcinogenesis.
Figure 4.
Pancreatic intraepithelial neoplasia (PanIN) count categorized into PanIN1, PanIN2 and PanIN3. (A) The PanIN count in unmodified ACS treatment (Set 1); and (B) The PanIN count in modified ACS SLN treatment (Set 2). Statistical significance was determined by two way ANOVA followed by a Bonferroni post hoc analysis. *, p<0.05; **, p<0.01; ***, p<0.001 represents statistical significance between BOP carcinogen and ACS treatment.
In SLN encapsulated ACS regimen (Set 2) (Figure 4B), the BOP control group (T8) showed an average of 19 PanIN1, 40 PanIN2 and 67 PanIN3 lesions. In comparison, the low dose ACS SLN group (T9) showed an average of 27 PanIN1, 45 PanIN2 and 59 PanIN3 lesions. The medium dose ACS SLN group (T10) had 23 PanIN1 lesions (NS; p>0.05), 18 PanIN2 (NS; p>0.05) and 17 PanIN3 (p<0.001) lesions; while the high dose ACS SLN group (T11) also showed a significant decrease in PanIN1 (18; p<0.001), PanIN2 (10; p<0.05) and PanIN3 (3; p<0.001) lesions compared to the BOP control group. Thus, the efficacy of the medium and high dose ACS SLN treatment groups was significant.
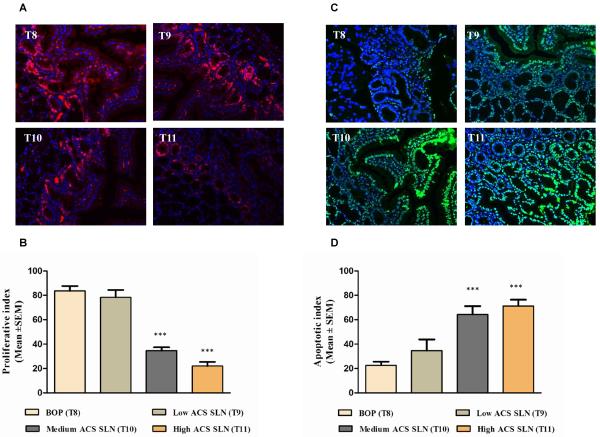
Inhibition of Proliferating Cell Nuclear Antigen (PCNA) expression by the ACS chemopreventive regimen
In order to evaluate the effect of ACS chemopreventive regimens on tumor proliferation, immunohistochemistry was performed to measure the expression of cell proliferation markers, proliferative cell nuclear antigen (PCNA) on pancreatic tissues. The PCNA expression was quantified by PCNA labeling index as described in the methods section. Result showed that the PCNA labeling index was significantly lowered by low, medium and high dose treatment of the unmodified ACS regimens. In comparison, the saline group (T1) showed little or no expression of PCNA. Quantitatively, PCNA expression in the BOP control group (T2) showed an index of 79.2 ± 3.12 (mean ± SEM) in the pancreatic lesions whereas the low (T3), medium (T4) and high dose (T5) ACS groups showed indices of 45.67 ± 1.99, 29.40 ± 2.04 and 11.25 ± 2.29, respectively, accounting for a significant decrease of around 42.3%, 62.9 % and 85.8 % respectively (p< 0.001).
In SLN encapsulated ACS study (Set 2), quantification of the IHC stains showed the PCNA labeling index to be 83.67 ± 3.04 (mean ± SEM) in the pancreatic lesions of BOP carcinogen group (T8); whereas the low (T9), medium (T10) and high dose (T11) ACS SLN groups showed proliferation indices of 78.33 ± 4.33 (p>0.05), 34.67 ± 2.11 (p< 0.001) and 21.67 ± 3.42 (p< 0.001), respectively, accounting for a decrease of around 6.3%, 58.6 % and 72.8 % respectively compared to BOP carcinogen control (Figure 5A and 5B).
Figure 5.
Effect of ACS chemopreventive regimen on tumor cell proliferation and apoptosis. Immunohistochemical analysis and TUNEL assay was performed on paraffin-embedded and micro-sectioned hamster pancreatic tissues as described in methods section. (A) Representative figures showing effect of modified ACS SLN combination on PCNA expression in pancreatic lesions. (B) A significant decrease in the PCNA expression was observed in modified ACS treatment groups (T9–T11) compared to BOP (N-nitrosobis (2-oxopropyl) amine) carcinogen control (T8) group. (C) Representative figures showing effect of modified ACS SLN combination on apoptosis in pancreatic lesions. (D) A dose-dependent increase in the apoptosis was observed in ACS SLN treated groups (T9-T11) compared to the BOP carcinogen control (T8) group. All the pictures were taken at 200X magnification. Statistical significance was determined by two-way ANOVA followed by a Bonferroni post hoc analysis. *, p<0.05; ***, p<0.001 represents statistical significance between BOP carcinogen and ACS treatment.
Induction of apoptosis by the ACS combined chemopreventive regimen
TUNEL assay was performed to determine the effect of ACS chemopreventive regimens on tumor cell apoptosis. Qualitative microscopic examination of TUNEL-stained sections showed a dose-dependent increase in TUNEL-positive cells in the pancreatic tissue of hamsters treated with unmodified ACS chemopreventive regimens compared with the BOP carcinogen control (T2). The quantification of apoptotic staining showed that the apoptotic index was 13.6 ± 2.09 (mean ± SEM) in the pancreatic lesions of BOP control group. The treatment groups of low (T3), medium (T4) and high dose (T5) ACS regimens showed significantly high apoptotic index of 25.83 ± 1.31(p<0.05), 51.4 ± 3.26 and 85.25 ± 3.71 (p<0.0001) respectively compared to BOP control group.
In the SLN encapsulated ACS study (Set 2), the quantification of apoptotic staining showed that the apoptotic index was 22.67 ± 2.29 (mean ± SEM) in the pancreatic lesions of BOP carcinogen group (T8). Among the treatment groups, the low dose (T9) ACS SLN group showed an apoptotic index of 34.67 ± 6.54 (p>0.05) while medium (T10) and high dose (T11) ACS SLN regimens showed significantly high apoptotic indices of 64.33 ± 5.24 (p<0.001; 3X increase compared to BOP control) and 71.25 ± 5.23 (p<0.0001; 3.2X increase compared to BOP control) respectively (Figure 5C and 5D).
Discussion
Pancreatic cancer has a poor prognosis and low survival rates for patients stricken by this disease. Despite improved treatment modalities during the last decade, there has been little to no substantial improvement in survival rates. This indicates the urgent need for the development of novel strategies against pancreatic cancer. Chemoprevention refers to the use of agents that have the potential to prevent, reverse, suppress or delay the development of cancer. This may prove to be valuable for individuals who are at high risk of developing pancreatic cancer including people with pre-malignant lesions and those with known risk factors for the disease.
Previously, no other research group has investigated the combined treatment effects of ASP, CUR and SFN (ACS) on the prevention of pancreatic cancer. In-vitro studies conducted in our lab indicated that ACS when combined in low doses significantly inhibited the cell viability and induced apoptosis in human pancreatic cancer cells, both in unmodified (free) and modified (nano-encapsulated) forms (6, 7). Additionally, a novel nanotechnology-based oral drug delivery system first introduced in our lab for the chemoprevention of pancreatic cancer showed initial success in suppressing cancer cell growth (6). Our present in vivo work, stemming from the results of in vitro studies provides continued strong evidence for the successful oral use of SLN-based ACS formulations on the combined chemoprevention of pancreatic cancer.
The major objective of this study was to assess the efficacy of a combined regimen of chemopreventive agents by targeting multiple pathways, thereby minimizing toxicity and other side effects. Recent results from our lab demonstrated that ACS combinations can induce apoptosis in MIA PaCa-2 and Panc-1 pancreatic cancer cells through activation of the ERK1/2 signaling system and inhibition of NF-κB pathway mechanisms (7). In the present study, unmodified ASP was used in combination with CUR and SFN at a dose range of 20 – 200 mg/kg and was demonstrated to be effective in suppressing the progression to pancreatic cancer. More importantly, SLN encapsulated ASP was used at 10X lower dose compared to unmodified ASP (2 – 20 mg/kg). A study conducted by Li et al., showed that intravenous liposomal CUR (40 mg/kg, 3 times per week for 20 days) suppressed pancreatic carcinoma growth in murine xenograft model and inhibited tumor angiogenesis (43). From an oral dosing standpoint, CUR has low bioavailability therefore high doses of CUR are usually needed to achieve significant anti-tumor effect. Kunnumakkara et al., showed that an oral dose of 1g/kg CUR was able to enhance the anti-tumor activity of gemcitabine in an orthotopic mouse model (36). For this study, we used a daily oral dose range of 45 – 450 mg/kg unmodified CUR and 4.5 – 45 mg/kg SLN encapsulated CUR which are considerably lower than doses used in previous studies.
In the case of SFN, Kuroiwa et al., have shown that SFN alone as a single agent was able to inhibit pancreatic carcinogenesis at 80 mg/kg in hamsters (37). In comparison, our studies used SFN dose at a range of 1.6 – 16mg/kg in hamsters thereby reducing the effective dose by 40 – 80%. Overall, the lower chemopreventive doses chosen for this study demonstrated significant efficacy upon being combined leading to a significant decrease in pancreatic cancer progression.
The formulation strategy for pancreatic drug delivery is challenging due to the relative inaccessibility of this organ. The overall intent of chemoprevention implies oral delivery to be the most optimal route of delivery of these agents as dosing has to occur over prolonged time periods with low to no toxicity. There is considerable evidence demonstrating that SLNs carry most of the drugs through the lymphatic system and drain into the systemic circulation near the jugular vein hence avoiding presystemic first pass metabolism (27). It is noteworthy that the ACS regimen in SLN formulations showed a greater efficacy at 1/10 of original dose when compared to its unmodified form therefore providing strong proof-of-concept for the use of SLN-based nanotechnology formulations on the chemoprevention of pancreatic cancer. The possible reasons might be attributed to the enhanced permeation and retention (EPR) effect of the lipid nanoparticles (44). Also, the lymphatic uptake of SLNs may have avoided the first pass metabolism thereby allowing more drug to reach the blood circulation making them effective at lower concentrations (45). In clinical use, this might address the possible bioavailability and dose related toxicity issues of these chemopreventive agents, for ex., gastrointestinal irritation caused by ASP. ASP can be given at low doses in combination to avoid the side effects associated with it when given individually. A recent clinical trial on curcumin usage for pancreatic cancer showed that an 8g daily dose of curcumin despite being well tolerated, was effective only in some patients with pancreatic cancer. This is possibly due to bioavailability issues associated with curcumin (22). In such cases, use of an SLN delivery system of this drug or in combination with other drugs at low doses would assist in reducing the effective daily dose in patients thereby lowering chances of toxicity. In this study, both ASP and CUR were encapsulated within SLNs using a modified oil-in-water emulsion method using stearic acid as the lipid and poloxamer 188 as the surfactant. As stated earlier, SFN was not formulated as nanoparticle preparations owing to its higher potency at low doses of unmodified forms. The encapsulation efficiency for both ASP and CUR was found to be approximately 78 and 66 %, respectively. The high encapsulation of these drugs can be attributed to the lipophilic nature of both ASP and CUR which makes it possible to be encapsulated within the lipid matrix of the stearic acid in SLNs. The particle sizing for ASP and CUR SLNs was found to be 169 ± 53 nm and 223 ± 79 nm, respectively.
PCNA is considered as a positive marker for proliferation since it is expressed in the nuclei of cells during the DNA synthesis phase of the cell cycle (46). Recent evidence suggests that PCNA is at the center of many essential cellular processes, such as DNA replication, repair of DNA damage, chromatin structure maintenance, chromosome segregation, and cell-cycle progression (47). Over-expression of PCNA or increased cell proliferation has been associated with a variety of gastric cancers including pancreatic cancer (48, 49). Our studies showed an increased expression of PCNA in the BOP treated hamsters indicating the intense cellular proliferation, while the chemopreventive ACS combination significantly decreased this expression as seen via immunohistochemistry analysis.
An imbalance in the levels of proliferation and apoptosis may result in deregulated tissue growth and cancer. Inability of a cell to undergo apoptosis in response to an apoptotic signal is a hallmark in pancreatic cancer (50). Additionally, defective apoptosis signaling is the underlying cause of failure to respond to the current treatment approaches for pancreatic cancer since cytotoxic therapeutic agents depend on induction of apoptosis in cancer cells in order to be effective (51). In our study, utilization of the TUNEL assay on the pancreatic cancer tissues showed a dose dependent increase in apoptosis when using the ACS combined regimen. Thus, both the PCNA and apoptotic indices studies provide convincing evidence of the efficacy of the novel chemopreventive regimen in delaying pancreatic carcinogenesis. Our recent publication provides new information on possible mechanisms of action for ACS regimens on pancreatic cancer cells through sustained activation of the ERK1/2 signaling system and down regulation of P-Akt kinase, an attractive target for cancer prevention and treatment (7).
In conclusion, novel strategies are warranted in the fight against pancreatic cancer as it is evident that very little progress has been made in this area during the past decade, despite newer and better treatment modalities to combat cancers. Our combinatorial treatment approach demonstrates higher efficacy at considerably lower doses potentially minimizing toxicity and other side effects, as evidenced from our results. Moreover, studies on the development of solid lipid nanoparticles (SLN) and its efficacy in the Syrian golden hamster model demonstrate the feasibility of delivering the drugs into circulation. These results provide strong proof-of-concept of the potential of chemoprevention using low dose drug therapy regimens to suppress, reverse or delay the progression of this otherwise fatal disease. Overall, the clinical relevance extends to the use of the novel ACS nanotechnology regimen for chemoprevention of pancreatic cancer in patients with high risk and those with pre-malignant lesions.
Acknowledgments
Grant Support: This work was supported by National Institutes of Health (1R03CA153812-01A1; S Prabhu). The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
Conflicts of interest: No potential conflicts of interest were disclosed.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Duffy JP, Eibl G, Reber HA, Hines OJ. Influence of hypoxia and neoangiogenesis on the growth of pancreatic cancer. Mol Cancer. 2003;2:12. doi: 10.1186/1476-4598-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ouyang N, Williams JL, Tsioulias GJ, Gao J, Iatropoulos MJ, Kopelovich L, et al. Nitric oxide-donating aspirin prevents pancreatic cancer in a hamster tumor model. Cancer Res. 2006;66:4503–11. doi: 10.1158/0008-5472.CAN-05-3118. [DOI] [PubMed] [Google Scholar]
- 4.Chaudhary A, Sutaria D, Huang Y, Wang J, Prabhu S. Chemoprevention of colon cancer in a rat carcinogenesis model using a novel nanotechnology-based combined treatment system. Cancer Prev Res (Phila) 2011;4:1655–64. doi: 10.1158/1940-6207.CAPR-11-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanthamneni N, Chaudhary A, Wang J, Prabhu S. Nanoparticulate delivery of novel drug combination regimens for the chemoprevention of colon cancer. Int J Oncol. 2010;37:177–85. doi: 10.3892/ijo_00000665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sutaria D, Grandhi BK, Thakkar A, Wang J, Prabhu S. Chemoprevention of pancreatic cancer using solid-lipid nanoparticulate delivery of a novel aspirin, curcumin and sulforaphane drug combination regimen. Int J Oncol. 2012 doi: 10.3892/ijo.2012.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thakkar A, Sutaria D, Grandhi BK, Wang J, Prabhu S. The molecular mechanism of action of aspirin, curcumin and sulforaphane combinations in the chemoprevention of pancreatic cancer. Oncol Rep. 2013 doi: 10.3892/or.2013.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uomo I, Miraglia S, Pastorello M. Inflammation and pancreatic ductal adenocarcinoma: a potential scenario for novel drug targets. JOP. 2010;11:199–202. [PubMed] [Google Scholar]
- 9.Aggarwal BB. Nuclear factor-kappaB: the enemy within. Cancer Cell. 2004;6:203–8. doi: 10.1016/j.ccr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Funahashi H, Satake M, Dawson D, Huynh NA, Reber HA, Hines OJ, et al. Delayed progression of pancreatic intraepithelial neoplasia in a conditional Kras(G12D) mouse model by a selective cyclooxygenase-2 inhibitor. Cancer Res. 2007;67:7068–71. doi: 10.1158/0008-5472.CAN-07-0970. [DOI] [PubMed] [Google Scholar]
- 11.Takahashi M, Furukawa F, Toyoda K, Sato H, Hasegawa R, Imaida K, et al. Effects of various prostaglandin synthesis inhibitors on pancreatic carcinogenesis in hamsters after initiation with N-nitrosobis(2-oxopropyl)amine. Carcinogenesis. 1990;11:393–5. doi: 10.1093/carcin/11.3.393. [DOI] [PubMed] [Google Scholar]
- 12.Molina MA, Sitja-Arnau M, Lemoine MG, Frazier ML, Sinicrope FA. Increased cyclooxygenase-2 expression in human pancreatic carcinomas and cell lines: growth inhibition by nonsteroidal anti-inflammatory drugs. Cancer Res. 1999;59:4356–62. [PubMed] [Google Scholar]
- 13.Kokawa A, Kondo H, Gotoda T, Ono H, Saito D, Nakadaira S, et al. Increased expression of cyclooxygenase-2 in human pancreatic neoplasms and potential for chemoprevention by cyclooxygenase inhibitors. Cancer. 2001;91:333–8. doi: 10.1002/1097-0142(20010115)91:2<333::aid-cncr1006>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 14.Anderson KE, Johnson TW, Lazovich D, Folsom AR. Association between nonsteroidal anti-inflammatory drug use and the incidence of pancreatic cancer. J Natl Cancer Inst. 2002;94:1168–71. doi: 10.1093/jnci/94.15.1168. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs EJ, Connell CJ, Rodriguez C, Patel AV, Calle EE, Thun MJ. Aspirin use and pancreatic cancer mortality in a large United States cohort. J Natl Cancer Inst. 2004;96:524–8. doi: 10.1093/jnci/djh084. [DOI] [PubMed] [Google Scholar]
- 16.Schernhammer ES, Kang JH, Chan AT, Michaud DS, Skinner HG, Giovannucci E, et al. A prospective study of aspirin use and the risk of pancreatic cancer in women. J Natl Cancer Inst. 2004;96:22–8. doi: 10.1093/jnci/djh001. [DOI] [PubMed] [Google Scholar]
- 17.Goel A, Kunnumakkara AB, Aggarwal BB. Curcumin as “Curecumin”: from kitchen to clinic. Biochem Pharmacol. 2008;75:787–809. doi: 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Aggarwal BB, Banerjee S, Bharadwaj U, Sung B, Shishodia S, Sethi G. Curcumin induces the degradation of cyclin E expression through ubiquitin-dependent pathway and up-regulates cyclin-dependent kinase inhibitors p21 and p27 in multiple human tumor cell lines. Biochem Pharmacol. 2007;73:1024–32. doi: 10.1016/j.bcp.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Shehzad A, Wahid F, Lee YS. Curcumin in cancer chemoprevention: molecular targets, pharmacokinetics, bioavailability, and clinical trials. Arch Pharm (Weinheim) 2010;343:489–99. doi: 10.1002/ardp.200900319. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal S, Ichikawa H, Takada Y, Sandur SK, Shishodia S, Aggarwal BB. Curcumin (diferuloylmethane) down-regulates expression of cell proliferation and antiapoptotic and metastatic gene products through suppression of IkappaBalpha kinase and Akt activation. Mol Pharmacol. 2006;69:195–206. doi: 10.1124/mol.105.017400. [DOI] [PubMed] [Google Scholar]
- 21.Goel A, Boland CR, Chauhan DP. Specific inhibition of cyclooxygenase-2 (COX-2) expression by dietary curcumin in HT-29 human colon cancer cells. Cancer Lett. 2001;172:111–8. doi: 10.1016/s0304-3835(01)00655-3. [DOI] [PubMed] [Google Scholar]
- 22.Dhillon N, Aggarwal BB, Newman RA, Wolff RA, Kunnumakkara AB, Abbruzzese JL, et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14:4491–9. doi: 10.1158/1078-0432.CCR-08-0024. [DOI] [PubMed] [Google Scholar]
- 23.Clarke JD, Dashwood RH, Ho E. Multi-targeted prevention of cancer by sulforaphane. Cancer Lett. 2008;269:291–304. doi: 10.1016/j.canlet.2008.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lampe JW. Sulforaphane: from chemoprevention to pancreatic cancer treatment? Gut. 2009;58:900–2. doi: 10.1136/gut.2008.166694. [DOI] [PubMed] [Google Scholar]
- 25.Kallifatidis G, Rausch V, Baumann B, Apel A, Beckermann BM, Groth A, et al. Sulforaphane targets pancreatic tumour-initiating cells by NF-kappaB-induced antiapoptotic signalling. Gut. 2009;58:949–63. doi: 10.1136/gut.2008.149039. [DOI] [PubMed] [Google Scholar]
- 26.Mehnert W, Mader K. Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev. 2001;47:165–96. doi: 10.1016/s0169-409x(01)00105-3. [DOI] [PubMed] [Google Scholar]
- 27.Yuan H, Chen J, Du YZ, Hu FQ, Zeng S, Zhao HL. Studies on oral absorption of stearic acid SLN by a novel fluorometric method. Colloids Surf B Biointerfaces. 2007;58:157–64. doi: 10.1016/j.colsurfb.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Zhang ZH, Zhang YL, Zhou JP, Lv HX. Solid lipid nanoparticles modified with stearic acid-octaarginine for oral administration of insulin. Int J Nanomedicine. 2012;7:3333–9. doi: 10.2147/IJN.S31711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuan H, Chen J, Du YZ, Hu FQ, Zeng S, Zhao HL. Studies on oral absorption of stearic acid SLN by a novel fluorometric method. Colloids Surf B Biointerfaces. 2007;58:157–64. doi: 10.1016/j.colsurfb.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Saruc M, Nozawa F, Yalniz M, Itami A, Pour PM. Effects of porcine pancreatic enzymes on the pancreas of hamsters. Part 1: basic studies. JOP. 2012;13:476–81. doi: 10.6092/1590-8577/522. [DOI] [PubMed] [Google Scholar]
- 31.Yoshimoto M, Hayakawa T, Mutoh M, Imai T, Tsuda K, Kimura S, et al. In vivo SPECT imaging with 111In-DOTA-c(RGDfK) to detect early pancreatic cancer in a hamster pancreatic carcinogenesis model. J Nucl Med. 2012;53:765–71. doi: 10.2967/jnumed.111.099630. [DOI] [PubMed] [Google Scholar]
- 32.Okamura T, Umemura T, Inoue T, Tasaki M, Ishii Y, Nakamura Y, et al. Chemopreventive Effects of 4-Methylthio-3-butenyl Isothiocyanate (Raphasatin) but Not Curcumin against Pancreatic Carcinogenesis in Hamsters. J Agric Food Chem. 2013 doi: 10.1021/jf3003174. [DOI] [PubMed] [Google Scholar]
- 33.Birt DF, Pour PM, Nagel DL, Barnett T, Blackwood D, Duysen E. Dietary energy restriction does not inhibit pancreatic carcinogenesis by N-nitrosobis-2-(oxopropyl)amine in the Syrian hamster. Carcinogenesis. 1997;18:2107–11. doi: 10.1093/carcin/18.11.2107. [DOI] [PubMed] [Google Scholar]
- 34.Hall PA, Lemoine NR. Models of pancreatic cancer. Cancer Surv. 1993;16:135–55. [PubMed] [Google Scholar]
- 35.Scarlett CJ, Salisbury EL, Biankin AV, Kench J. Precursor lesions in pancreatic cancer: morphological and molecular pathology. Pathology. 2011;43:183–200. doi: 10.1097/PAT.0b013e3283445e3a. [DOI] [PubMed] [Google Scholar]
- 36.Kunnumakkara AB, Guha S, Krishnan S, Diagaradjane P, Gelovani J, Aggarwal BB. Curcumin potentiates antitumor activity of gemcitabine in an orthotopic model of pancreatic cancer through suppression of proliferation, angiogenesis, and inhibition of nuclear factor-kappaB-regulated gene products. Cancer Res. 2007;67:3853–61. doi: 10.1158/0008-5472.CAN-06-4257. [DOI] [PubMed] [Google Scholar]
- 37.Kuroiwa Y, Nishikawa A, Kitamura Y, Kanki K, Ishii Y, Umemura T, et al. Protective effects of benzyl isothiocyanate and sulforaphane but not resveratrol against initiation of pancreatic carcinogenesis in hamsters. Cancer Lett. 2006;241:275–80. doi: 10.1016/j.canlet.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 38.Muchow M, Maincent P, Muller RH. Lipid nanoparticles with a solid matrix (SLN, NLC, LDC) for oral drug delivery. Drug Dev Ind Pharm. 2008;34:1394–405. doi: 10.1080/03639040802130061. [DOI] [PubMed] [Google Scholar]
- 39.Petri N, Tannergren C, Holst B, Mellon FA, Bao Y, Plumb GW, et al. Absorption/metabolism of sulforaphane and quercetin, and regulation of phase II enzymes, in human jejunum in vivo. Drug Metab Dispos. 2003;31:805–13. doi: 10.1124/dmd.31.6.805. [DOI] [PubMed] [Google Scholar]
- 40.Cornblatt BS, Ye L, Dinkova-Kostova AT, Erb M, Fahey JW, Singh NK, et al. Preclinical and clinical evaluation of sulforaphane for chemoprevention in the breast. Carcinogenesis. 2007;28:1485–90. doi: 10.1093/carcin/bgm049. [DOI] [PubMed] [Google Scholar]
- 41.Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, et al. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–86. doi: 10.1097/00000478-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Lohr M, Kloppel G, Maisonneuve P, Lowenfels AB, Luttges J. Frequency of K-ras mutations in pancreatic intraductal neoplasias associated with pancreatic ductal adenocarcinoma and chronic pancreatitis: a meta-analysis. Neoplasia. 2005;7:17–23. doi: 10.1593/neo.04445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li L, Braiteh FS, Kurzrock R. Liposome-encapsulated curcumin: in vitro and in vivo effects on proliferation, apoptosis, signaling, and angiogenesis. Cancer. 2005;104:1322–31. doi: 10.1002/cncr.21300. [DOI] [PubMed] [Google Scholar]
- 44.Maeda H. The enhanced permeability and retention (EPR) effect in tumor vasculature: the key role of tumor-selective macromolecular drug targeting. Adv Enzyme Regul. 2001;41:189–207. doi: 10.1016/s0065-2571(00)00013-3. [DOI] [PubMed] [Google Scholar]
- 45.Greish K. Enhanced permeability and retention of macromolecular drugs in solid tumors: a royal gate for targeted anticancer nanomedicines. J Drug Target. 2007;15:457–64. doi: 10.1080/10611860701539584. [DOI] [PubMed] [Google Scholar]
- 46.Johnson DG, Walker CL. Cyclins and cell cycle checkpoints. Annu Rev Pharmacol Toxicol. 1999;39:295–312. doi: 10.1146/annurev.pharmtox.39.1.295. [DOI] [PubMed] [Google Scholar]
- 47.Maga G, Hubscher U. Proliferating cell nuclear antigen (PCNA): a dancer with many partners. J Cell Sci. 2003;116:3051–60. doi: 10.1242/jcs.00653. [DOI] [PubMed] [Google Scholar]
- 48.Sato T, Konishi K, Kimura H, Maeda K, Yabushita K, Tsuji M, et al. Evaluation of PCNA, p53, K-ras and LOH in endocrine pancreas tumors. Hepatogastroenterology. 2000;47:875–9. [PubMed] [Google Scholar]
- 49.Niijima M, Yamaguchi T, Ishihara T, Hara T, Kato K, Kondo F, et al. Immunohistochemical analysis and in situ hybridization of cyclooxygenase-2 expression in intraductal papillary-mucinous tumors of the pancreas. Cancer. 2002;94:1565–73. doi: 10.1002/cncr.10358. [DOI] [PubMed] [Google Scholar]
- 50.Fulda S. Targeting apoptosis signaling pathways for anticancer therapy. Front Oncol. 2011;1:23. doi: 10.3389/fonc.2011.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fulda S, Debatin KM. Extrinsic versus intrinsic apoptosis pathways in anticancer chemotherapy. Oncogene. 2006;25:4798–811. doi: 10.1038/sj.onc.1209608. [DOI] [PubMed] [Google Scholar]