Abstract
Insomnia has been established as a risk factor for depression and mental illness for decades, but a growing body of evidence has recently exposed insomnia to be an independent risk factor for suicide that encompasses all age ranges. This discovery has invigorated investigation to elucidate the relationship between insomnia and suicide, and over 20 studies reinforcing this association in adults have been published since 2010 alone. This article analyzes relevant research and emphasizes studies published within the last three years with the intent of proposing theoretical mechanisms explaining the link between suicide and insomnia. These mechanisms may then be used as targets for future investigation of treatment.
Keywords: Sleep, Depression, Suicide, Risk factors, Insomnia, Hopelessness, Nightmares, Mechanisms, Dysfunctional belief about sleep, Decision making, Serotonin, Hyperarousal, Circadian rhythm of suicide, Psychiatry
Introduction
Millions of Americans suffer from sleep related disorders such as obstructive sleep apnea, insomnia, and parasomnias, yet the study of sleep disorders and their long-term consequences is still relatively in its infancy. The recognition of Sleep Medicine as a legitimate subspecialty of medicine came upon the wings of a series of developments that include the establishment of a defined body of specialty-based knowledge, recognition by the American Medical Association, the creation of fellowship training programs approved by the Accreditation Council for Graduate Medical Education (ACGME), and the creation of board exams sponsored by the American Board of Medical Specialties (ABMS). In the course of these developments, the discovery that one sleep disorder, obstructive sleep apnea (OSA), is associated with excess mortality [1] elevated sleep problems from the status of trivial to urgent. In contrast to OSA, the realization that insomnia is a risk factor for suicide has come only recently.
Solid evidence has shown that insomnia is a risk factor for the development of mental illness, with the strongest risk ratios for depressive illness [2]. The causal mechanism of this association is not clear. For example, it is unknown whether insomnia is an independent phenomenon that if interrupted could forestall the emergence of a mental disorder, or whether insomnia is simply the leading edge of an illness that is already on the way. Investigators are already examining the former possibility, by way of focusing on preventing recurrent depressive illness. Success in this line of investigation would be of immense importance as there are presently limited numbers of means to prevent or minimize the recurrence of mental disorders of any type.
The importance of these findings has been paralleled by an accumulating body of evidence that insomnia is a risk factor for suicidal ideation, suicidal behavior, and suicide death (which we will collectively refer to here as “suicide”). Suicidal ideation is defined as a desire to die, or at least an indifference towards living, that may be accompanied by specific plans to kill oneself [3, 4]. By extension, suicidal behavior is a self-harm behavior, or a behavior that is preparatory to self-harm, and it is intended to lead to the possibility of death or increase the risk of death. Death by intentional self-harm would seem to be straightforward, yet sometimes death is the result of a self-harm act that was originally intended only to generate a response from others in the environment. This example would hence not be considered as suicidal. Suicidal behavior may be attended by simultaneous rescue behaviors, i.e., a person cuts their wrists with the idea of dying yet then goes to lie down in a public place to see if someone will rescue him/her. This example, however, would be coded as suicidal behavior [4]. Suicide is complex and is driven by different motivations in different individuals; several competing and potentially conflicting motivations may operate simultaneously in a given individual.
The evidence base linking insomnia and suicide is both wide and deep. There are more than 60 separate research reports that encompass children, adolescents, young adults, and older persons, and these reports come from the Americas, Europe, and Asia. A summary of the studies in adults can be found in Table 1. The reports include population studies, clinical samples, chart reviews, prospective case-control cohorts, and clinical trials. The methods of assessing insomnia vary widely across these studies, with some studies using validated and standardized measures of insomnia and other studies only using one-off indicators of insomnia. Furthermore, some studies reported insomnia as either present versus absent while other studies used dimensional measures of insomnia intensity. The measurement of suicide was similarly varied across these studies. Despite the variability in assessment, the basic findings remain remarkably consistent with relative risks in the range of 2.0 (Table 1).
Table 1. The Relationship between Sleep and Suicide in Adults, by Year of Publication.
| Author/year | Source of sample | Design, N= | Sleep disturbance | Specified outcome |
|---|---|---|---|---|
| Barraclough 1975 [64] | Suicidal/depressed outpatients | Cross-sectional, N=192 | Insomnia | Suicide death |
| Fawcett 1990 [65] | Depressed patients | Prospective, N=954 | Insomnia | Suicide death |
| Agargun 1997 [66] | Depressed patients | Cross-sectional, N=41 | Insomnia | Suicidal thoughts |
| Agargun 1997 [67] | Depressed patients | Cross-sectional, N=113 | Insomnia | Suicidal thoughts |
| Agargun 1998 [68] | Depressed patients | Cross-sectional, N=63 | Nightmares | Suicidal thoughts |
| Krakow 2000 [69] | Female sexual assault survivors | Cross-sectional, N=153 | Sleep breathing & sleep movement disorders | Suicidal thoughts |
| Tanskanen 2001 [70] | Population survey | Prospective, N=36,211 | Nightmares | Suicide death |
| Turvey 2002 [71] | Population survey | Prospective, N=14,456 | Insomnia | Suicide death |
| Agargun 2003 [72] | Depressed patients | Cross-sectional, N=26 | REM disturbances | Suicidal thoughts |
| Smith 2004 [73] | Chronic pain patients | Cross-sectional, N=51 | Insomnia | Suicidal thoughts |
| Bernert 2005 [74] | Psychiatric outpatients | Cross-sectional, N=176 | Insomnia & nightmares | Suicidal thoughts |
| Fujino 2005 [75] | Population survey | Prospective, N=15,597 | Insomnia | Suicide death |
| Agargun 2007 [76] | Depressed inpatients | Cross-sectional, N=149 | Insomnia & nightmares | Prior suicide attempt |
| Chellappa 2007 [77] | Depressed outpatients | Cross-sectional, N=70 | Insomnia | Suicidal thoughts |
| Sjostrom 2007 [78] | Suicide attempters | Cross-sectional, N=165 | Insomnia & nightmares | Prior suicide attempt |
| Goodwin 2008 [79] | Population survey | Cross-sectional, N=8,098 | Short sleep | Suicidal thoughts & attempts |
| Bernert 2009 [80] | Depressed outpatients | Cross-sectional, N=82 | Insomnia & nightmares | Suicidal thoughts |
| Sjostrom 2009 [6] | Suicide attempters | Prospective, N=165 | Insomnia & nightmares | Repeat suicide attempt |
| Lee 2010 [81] | Population survey | Cross-sectional, N=2,054 | Insomnia | Suicidal thoughts |
| Li 2010 [82] | Outpatient psychiatric clinic | Prospective, N=1,231 | Insomnia & nightmares | Suicide attempts |
| McCall 2010 [83] | Depressed insomniacs | Longitudinal, N=60 | Insomnia | Suicidal thoughts |
| Nadorff 2010 [84] | College survey | Cross-sectional, N=583 | Insomnia & nightmares | Suicidal thoughts |
| Selvi 2010 [76] | Depressed patients | Cross-sectional, N=160 | Sleep quality, chronotype | Suicidal thoughts |
| Benute 2011 [85] | High-risk pregnancy patients | Cross-sectional, N=268 | Insomnia | Suicidal thoughts |
| Bjerkeset 2011 [86] | Population survey | Prospective, N=74,977 | Sleep problems | Suicide death |
| Brower 2011 [87] | Population survey | Cross-sectional, N=5,692 | Insomnia | Suicidal thoughts |
| Carli 2011 [88] | Prisoners | Cross-sectional, N=1,420 | Insomnia | Suicidal thoughts |
| Krakow 2011 [89] | Sleep patients | Cross-sectional, N=1,584 | Insomnia & nightmares | Suicidal thoughts |
| Susanszky 2011 [7] | Community survey | Cross-sectional, N=4,642 | Insomnia & nightmares | Gender differences & suicidal thoughts & attempts |
| Klimkiewicz 2012 [90] | Substance abusers | Cross-sectional, N=304 | Insomnia | Suicidal thoughts |
| Li 2012 [5] | Depressed outpatients | Prospective, N=371 | Insomnia & nightmares | Suicidal thoughts |
| Pigeon 2012 [15] | Veteran suicides | Chart review, N=381 | Insomnia | Latency to suicide death |
| Ribeiro 2012 [12] | Suicidal active duty military | Cross-sectional and longitudinal, N=311 | Insomnia | Suicidal thoughts & attempts |
| Suh 2012 [13] | Non-depressed population survey | Longitudinal, N=1,282 | Insomnia | Depression & suicide thoughts or attempts |
| Bae 2013 [91] | General population | Cross-sectional, N=1,000 | Insomnia | Suicidal thoughts |
| Gunnell 2013 [92] | Outpatients | Prospective, N=393,983 | Insomnia | Suicide death |
| McCall 2013 [9] | Depressed insomniacs | Cross-sectional, N=50 | Insomnia, nightmares, & dysfunctional beliefs and attitudes about sleep | Suicidal thoughts |
| Nadorff 2013 [10] | Elderly population | Cross-sectional, N=81 | Insomnia, nightmares | Suicidal thoughts |
| Nadorff 2013 [14] | Population survey | Cross-sectional, N=972 | Insomnia, nightmares | Suicidal thoughts & attempts |
| Suh 2013 [13] | Non-depressed population survey | Longitudinal, N=1,282 | Insomnia | Suicidal thoughts & attempts |
Multiple investigations have simultaneously assessed both “insomnia” and “nightmares”, and these studies typically found that the presence of nightmares was as potent, or more potent, than insomnia in predicting suicide [5•, 6]. The term “nightmares” connotes the experience of a dysphoric dream during rapid eye movement (REM) sleep, characterized by a narrative (albeit a disjointed narrative), high visual impact, and good recall upon awakening. Indeed, frequent nightmares are reported to increase the risk of suicidal thoughts by a factor of 1.5 – 3 and increase the risk for suicide attempts by a factor of 3 – 4 [7•]. Nightmares are a common feature of post-traumatic stress disorder (PTSD), and perhaps play a role in explaining the rising rates of suicide in US servicemen returning from the Global War on Terror [8]. When nightmares as well as dysfunctional beliefs and attitudes about sleep (DBAS) are simultaneously considered as mediators between insomnia and suicide, then the association between insomnia and suicide disappears [9••]. It is of note, however, that the correlation between nightmares and suicide may not hold true in older adults [10], and this may possibly be due in part because of the sleep changes that occur with increased age such as altered REM sleep patterns and decreased number of reported nightmares [10].
Recent Reports on the Sleep-Suicide Link
The sheer variety of the sources of data and the convergence of the findings make a compelling case that the association between insomnia and suicide is real. Healthy skepticism, nonetheless, would note that insomnia is a frequent symptom of depression, and depression is a known risk for suicide. It could therefore be argued that it is the depression syndrome rather than the insomnia symptom itself that conveys the risk. However, meta-analysis shows that the association between insomnia and suicide still holds even after controlling for the presence or absence of depressive disorder [11•] and after controlling for the intensity of specific symptoms such as depressed mood and hopelessness [12]. In fact, persistent insomnia among individuals who lacked depression at baseline increases the risk of both depression and suicidal thoughts prospectively across the span of six years [13•].
Nightmares are an additional independent predictor of suicide [7•]. Nightmares, especially when persistent over time, can foreshadow suicidal behavior in the form of repeated suicide attempts among those who had attempted suicide within the preceding two years [6]. The temporal duration of insomnia and nightmares, like the intensity of insomnia and nightmares, is also predictive of suicide. Indeed, unresolved insomnia and nightmare symptoms were significantly correlated with suicidal ideation among depressed patients who remitted across a span of four years. Residual nightmares, in particular, were associated with suicidal ideation with a large odds ratio of 8.4 [5]. Furthermore, the overall duration of insomnia and nightmares increased suicide risk independently of the current severity of sleep disturbance and depression [14]. Not only is the duration of the insomnia complaint relevant as a predictor of suicide, but insomnia is also often temporally proximal to suicide. In one sample of veteran suicide deaths, insomnia was documented in nearly half of the last doctor's visits preceding suicide death [15].
The associations among insomnia and nightmares and suicide may or may not be uniform across all ages of patients. For example, the mechanism explaining the linkage in children might be different from the linkage in adults. For this reason, the remainder of this paper will focus on these relationships in adults.
Insomnia, Hopelessness, and Nightmares—Modifiable Risk Factors for Suicide
Insomnia, hopelessness, and nightmares can be viewed as part of the collection of modifiable risk factors for suicide. Some of the strongest risk factors for suicide cannot be (easily) modified, and these include age, gender, and race/ethnicity. On the other hand, there are a larger number of risk factors that are potentially modifiable which include active symptoms of depression, active alcohol or substance abuse, social isolation, and some chronic diseases in addition to the aforementioned processes of hopelessness, insomnia, and nightmares [16].
Hopelessness is among the strongest psychological risk factors for suicide, and specific psychological treatments have been devised in order to address hopeless ideation [17]. It has been shown to an independent factor that distinguishes depressed individuals with suicidal ideation from depressed individuals without suicidal ideation [18•], and it has recently been implicated as a unique contributor in the contemplative phase of impulsive suicide attempts [19]. There are also cognitive aspects of chronic insomnia that have a hopeless “flavor”, such as “I have little ability to manage the negative consequences of disturbed sleep” or “When I sleep poorly on one night, I know it will disturb my sleep schedule for the whole week”. These sorts of pessimistic cognitions are captured in the Dysfunctional Beliefs and Attitudes about Sleep (DBAS) scale [20, 21]. Of note, the word “hopeless” never appears in any item of the scale, although the feeling of hopelessness is certainly reflected by some of the items.
Psychological Mechanisms
Hopelessness versus Dysfunctional Beliefs and Attitudes about Sleep
Based upon the well-described association between hopelessness and suicide, it might be expected that some of the relationship between insomnia and suicide was mediated via hopelessness. To this end, we examined whether hopelessness was correlated with dysfunctional beliefs and attitudes about sleep and with the intensity of suicidal ideation in a sample of 50 persons with depressive disorders of various types, degrees of severity, and treatment settings. We found that the DBAS was related to the intensity of suicidal ideation, and insomnia and hopelessness were correlated with suicide as expected. To our surprise, however, we found that hopelessness as measured in the Beck Hopelessness Scale (BHS) was unrelated to the DBAS [9]. In other words, the pessimistic cognitions measured by the DBAS represent a separate cognitive process from the conventional understanding of hopelessness. Moreover, both the DBAS score and the BHS score separately and independently predicted suicidal ideation. Consistent with cross-sectional evidence, neither depression nor hopelessness were found to mediate the link between insomnia and prospective suicidal ideation and behavior in a study of young adults in the military [12]. These discoveries potentially offer a new target for mitigating suicide: dysfunctional beliefs and attitudes about sleep.
Sleep, Executive Decision Making, and Suicide
Apart from self-defeating cognitions, insomnia may also adversely impact cognitive function through impaired decision making. The role of sleep in memory consolidation has been well described, as sleep loss is associated with decrements in verbal and visual memory [22]. We recognize that insomnia and sleep deprivation are different problems. Insomnia and sleep deprivation, nonetheless, share the common feature of reduced total sleep time, and reduced sleep time has been associated with impaired decision making [22]. In particular, insomnia is associated with deficient problem-solving capacity, especially when involving complex tasks [23•].
Suicide attempters demonstrate problem-solving abnormalities that parallel those described in insomniacs. Multiple studies have shown past suicide attempters exhibit reduced attention and working memory performance as compared with depressed non-attempters and non-depressed controls [24•, 25, 26]. Prior attempters of suicide produced a fewer number of solutions when faced with an experimental problem, and those solutions were more passive and less effective than those created by controls [27]. Moreover, suicide attempters may perceive their problem solving skills as inadequate, even without any actual problem-solving impairment upon testing [28]. Deficits in problem solving are seen regardless of the current severity of suicidal thoughts or the severity of prior suicide attempt [24•, 27], suggesting that this is a stable trait. Together these findings raise the possibility that insomnia leads to perceived or documentable deficiencies in decision making that may lead psychiatrically ill patients to consider a poorer quality and diminished number of solutions to their problems. Suicide may perhaps be left as the only remaining possibility. Under this scenario, treatment of insomnia might lead to improvements in decision-making and hence reduced risk of suicide.
Possible Biological and Physiological Mechanisms between Insomnia, Nightmares, and Suicide
Serotonin
The insomnia-suicide link may be mediated by serotonergic mechanisms. The first collection of evidence stems from the knowledge that serotonin (5-HT) has an important and complex role in the induction and maintenance of sleep [29•], and the complexity of the 5-HT/sleep relationship is exemplified by a wide variety of 5-HT receptors with different regional brain distributions [29•]. For this reason, it is impossible to distill the 5-HT/sleep relationship down to a simple statement such as “5-HT helps you sleep”. For example, administration of the 5-HT precursor, L-tryptophan, is helpful for sleep [30], and yet facilitation of 5-HT with a serotonin re-uptake inhibitor can lead to deterioration of sleep [31]. The possibility that manipulation of sleep could alter the dynamics of 5-HT has been recently reported. In humans, one in vivo study of cerebral serotonin receptors showed a 9.6% increase in receptor binding potential after as little as 24 hours of total sleep deprivation [32•]. Furthermore, sleep deprivation of rodents led to a loss of sensitivity of post-synaptic 5-HT receptors [33, 34], and this serotonin desensitization was paralleled by a blunted hypothalamic-pituitary-adrenal (HPA) axis stress reaction in the form of decreased pituitary cortisol response [33].
Abnormalities in 5-HT function are also seen in suicide attempters. One of the most replicable biological findings in suicide is reduced CNS serotonergic (5-HT) function, as reflected by low levels of serotonin's main metabolite, 5-Hydroxyindoleacetic acid (5-HIAA), in the cerebrospinal fluid (CSF) of suicide victims and perpetrators of violence upon others [35••]. In addition, pre-synaptic serotonin midbrain transporters were diminished in binding potential distinctively among those who attempted suicide and/or suffered suicide death as contrasted to individuals with major depression who lacked a past history of suicide [36, 37]. These findings are consistent with evidence that chronic alterations of pre-synaptic serotonin availability is intercorrelated with changes in the sensitivity and density of both pre-synaptic transporters and post-synaptic receptors [38, 39]. Under this scenario, insomnia, and the associated reduction in total sleep time, could lead to a loss of 5-HT function, and in turn, increased risk of suicide.
The prefrontal cortex and its control over executive function are under the influence of the serotonergic system as well. Inadequate serotonin input to the prefrontal cortex is known to foster impoverished decision making [40•] and its ensuing array of aforementioned consequences. Together these raise the possibility that low 5-HT function is not just a marker of suicide, but is more so a marker of violent impulsivity and diminished decision-making skills that lower the threshold to suicide.
Hyperarousal
Converging lines of evidence have led to the view that primary insomnia is a condition of hyperarousal, and its 24-hour span of symptoms is paralleled by a variety of biological and physiological abnormalities [41]. HPA dysfunction was previously mentioned to be a consequence of sleep deprivation [33], and cortisol is also a potent biological marker of suicide risk, particularly in the setting of stress-related suicide. Stress activates the HPA system and thus releases a cascade of hormones including but not limited to corticotrophin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and cortisol; these hormones then augment susceptibility to hyperarousal, REM alterations, and subsequently suicidal behavior [42••]. Hyperarousal is typified by inhibition of night time sleep, elevated core body temperature (especially at night), accelerated electroencephalogram (EEG) rhythms both awake and asleep, and elevated brain metabolism both awake and asleep [43]. The view of insomnia as a disorder of physiologic hyperarousal parallels the view that nightmare symptoms in PTSD are related to adrenergic overdrive [44]. Thus the link between insomnia and suicide as well as the link between nightmares and suicide may share a common feature in hyperarousal and HPA dysfunction.
Unpleasant mental experiences, however, can presumably occur outside of REM sleep. These dysphoric non-REM sleep experiences may be characterized by depressive cognitions occurring during sleep, but without the complex narratives and high visual impact of a nightmare. Persons with depression are more likely to report depressive mental content during sleep [45]. Prior reports linking nightmares to suicide have not clarified whether the link exists for classic REM sleep-nightmares, or for non-REM sleep depressive cognition, or both. Clarity is needed as there are treatments available for PTSD-REM sleep-nightmares that may or may not have effect in non-REM sleep dysphoric sleep experiences. Specific treatments for PTSD-nightmares include blocking adrenergic receptors with prazosin [46], suggesting that adrenergic overdrive is a mechanism behind nightmares and perhaps other PTSD symptoms such as hypervigilence [47].
Circadian Rhythm of Suicide
The preceding discussion on insomnia, nightmares, and suicide raises the question of whether a preponderance of suicides occurs at night. To the contrary, suicide between midnight and 8 AM is relatively uncommon, but rises abruptly between 8 AM and noon [48 – 51]. How then might sleep problems contribute to excess suicide during the morning hours? Much may revolve around what time of the day an individual naturally feels better. In colloquial terms, some individuals are naturally “larks” or morning chronotypes, and others are better described as “night owls” or evening chronotypes. Neural imaging has even reinforced these concepts by showing diurnal variations in positive-affect related structures that are in accordance with an individual's reported chronotype [52]. Chronotype has not been found to be casual of suicide, per se. However, morningness is associated with less aggression, is protective against the incidence of major depression, and provides relief of symptoms among those who already suffer from major depression regardless of subjective sleep quality [53••, 54•]. Eveningness, on the other hand, raises the likelihood of experiencing nightmares, difficulty falling asleep, poor sleep quality, fewer hours spent asleep, feeling worse in the morning, and has a well-established correlation with depression [54•, 55, 56]. The eveningness chronotype even correlated with a higher degree of impulsivity and lethality of suicide method in contrast to morning-type individuals [57]. It is also of interest to note that new research indicates eveningness to be associated with a higher cardiovascular disease rate [58, 59], and one does indeed find that other serious medical crises, such as myocardial infarction [60] and stroke [61], tend to peak during the same 8am – 12pm time frame.
The Way Forward
The understanding of the insomnia-suicide link is in the earliest stages of development, and therefore most of what has been presented in this paper is conjectural and intended only to provide ideas for hypothesis testing. Still, we have presented a broad array of targets for attack on suicide risk ranging from distorted cognitions about sleep, to deficient decision making, to under-performing 5-HT systems, to hyperarousal. A visual schematic of proposed mechanisms is presented in Figure 1. Potential interventions could include medications, brain stimulation, or psychotherapy depending upon the model being tested.
Figure 1. The Link between Insomnia and Suicide: Theoretical Mechanisms Schematic.
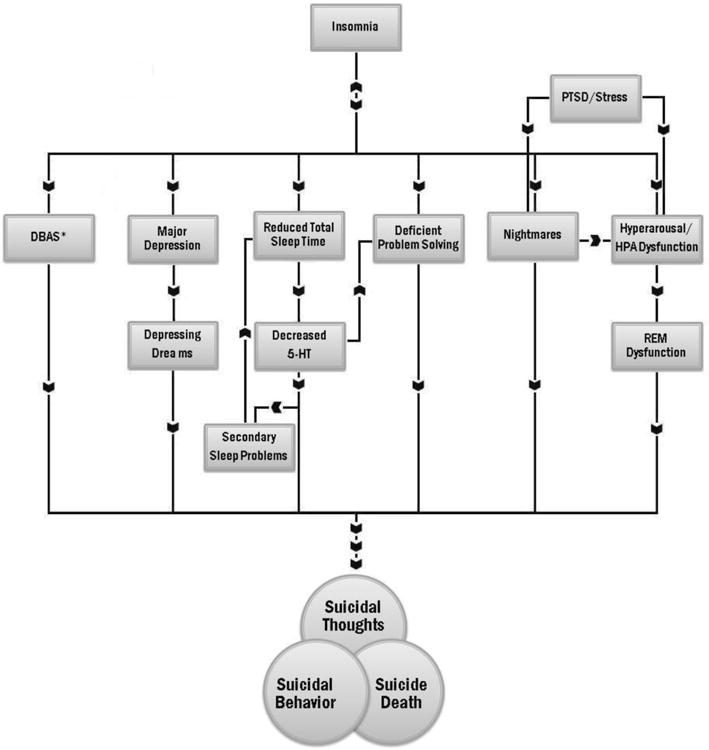
*Dysfunctional Beliefs and Attitudes about Sleep
There are a series of intermediate steps that could precede clinical trials of these targets in depressed, suicidal insomniacs. In the case of dysfunctional beliefs and attitudes about sleep (DBAS), it would be useful to establish whether DBAS can be modified by pharmacology or only through cognitive behavior therapy for insomnia. The finding of deficient decision-making begs the question as to whether any form of insomnia treatment, either pharmacologic or psychotherapeutic, leads to improvements in decision-making. Finally, the possibility of a link between hyperarousal-insomnia or hypervigilence-nightmares and suicide suggests that treatments that dampen hyperarousal may lower suicide risk. To this end there is preliminary evidence that standard benzodiazepine agonist hypnotics reduce hypermetabolism in relevant brain regions of non-depressed insomniacs [62]. It is not known whether a similar effect can be reproduced in depressed insomniacs or with cognitive behavior therapy for insomnia, and it remains unknown whether these effects would lead to diminished suicidality.
Conclusion
Global death rates from dysentery and tuberculosis have fallen in the last 20 years as medicine continues to advance in the fight against infectious causes of illness, yet suicide is rising in its importance as a global killer, increasing from 14th to 13th place of all causes of mortality [63]. As once was the case for infection, strategies are lacking for the prevention of suicide. Recent research has raised the possibility that the treatment of insomnia and nightmares, or addressing the mechanisms that drive insomnia and nightmares, may be an avenue for prevention tactics against the rising threat of suicide.
Acknowledgments
This research was supported by National Institutes of Health grant MH095776-01A1.
Footnotes
Compliance with Ethics Guidelines: W. Vaughn McCall has received compensation from Luitpold Pharmaceuticals for serving as a consultant, has received royalties from Lippincott Williams & Wilkins for serving as editor for The Journal of ECT, and has received compensation from CME for development of educational presentations.
Conflict of Interest: Carmen G. Black declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
W. Vaughn McCall, Email: wmccall@gru.edu, Department of Psychiatry and Health Behavior, Medical College of Georgia, Georgia Regents University, 1120 15th Street, Augusta, GA 30912, Phone: 706–721–6719, Fax: 706–721–1793.
Carmen G. Black, Email: carblack@gru.edu, Class of 2014, Medical College of Georgia, Georgia Regents University, 1120 15th Street, Augusta, GA 30912, Phone: 706–721–7309, Fax: 706–721–1793.
References
Recently published papers of particular interest have been highlighted as:
• Of importance
•• Of major importance
- 1.He J, Kryger MH, Zorick F, et al. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988;94:9–14. [PubMed] [Google Scholar]
- 2.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 3.Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior: utility and limitations of research instruments. In: First MB, editor. Standardized Evaluation in Clinical Practice. Washington, DC: APPI Press; 2003. pp. 103–130. [Google Scholar]
- 4.Posner K, Oquendo M, Gould M, et al. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. American Journal of Psychiatry. 2007;164:1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5•.Li S, Lam S, Chan J, et al. Residual sleep disturbances in patients remitted from major depressive disorder: a 4-year naturalistic follow-up study. Sleep. 2012;35:1153–1161. doi: 10.5665/sleep.2008. Both nightmares and insomnia significantly correlate with remitted major depression and suicidal ideation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sjostrom N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170:208–211. doi: 10.1016/j.psychres.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 7•.Susansky E, Hajnal A, Kopp M. Sleep disturbances and nightmares as risk factors for suicidal behavior among men and women. Psychiatr Hung. 2011;26:250–257. Frequent nightmares increase the risk for suicidal thoughts and attempts. [PubMed] [Google Scholar]
- 8.Surveillance of suicidal behavior January-December 2011. Army Institute of Public Health; 2012. Behavioral and Social Health Outcomes Program. [Google Scholar]
- 9••.McCall W, Batson N, Webster M, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. Journal of Clinical Sleep Medicine. 2013;9:135–140. doi: 10.5664/jcsm.2408. Nightmares and dysfunctional beliefs and attitudes about sleep mediate the relationship between insomnia and suicide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadorff M, Fiske A, Sperry J, et al. Insomnia symptoms, nightmares, and suicidal ideation in older adults. J Gerontol B Psychol Sci Soc Sci. 2013;68:145–152. doi: 10.1093/geronb/gbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11•.Pigeon W, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. Journal Clinical Psychiatry. 2012;73:1160–1167. doi: 10.4088/JCP.11r07586. Depressive disorder does not mediate the link between insomnia and suicide. [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro J, Pease J, Gutierrez P, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disorder. 2012;136:743–750. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 13•.Suh S, Kim H, Yang H, et al. Longitudinal course of depression scores with and without insomnia in non-depressed individuals: a 6-year follow-up longitudinal study in a Korean cohort. Sleep. 2013;36:369–376. doi: 10.5665/sleep.2452. Persistent insomnia prospectively increases the likelihood of developing both major depression and suicidal ideation among insomniacs who lack depression at baseline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadorff R, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43:139–149. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pigeon W, Britton P, Ilgen M, et al. Sleep disturbance preceding suicide among veterans. Am J Public Health. 2012;102:S93–S97. doi: 10.2105/AJPH.2011.300470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- 17.Simpson G, Tate R, Whiting D, et al. Suicide prevention after traumatic brain injury: a randomized controlled trial of a program for the psychological treatment of hopelessness. J Head Trauma Rehabil. 2011;26:290–300. doi: 10.1097/HTR.0b013e3182225250. [DOI] [PubMed] [Google Scholar]
- 18•.Nyer M, Holt D, Pedrelli P, et al. Factors that distinguish college students with depressive symptoms with and without suididal thoughts. Ann Clin Psychiatry. 2013;25:41–49. The presence of hopelessness is an independent risk factor for suicidal ideation among depressed individuals. [PMC free article] [PubMed] [Google Scholar]
- 19.Bagge C, Littlefield A, Lee H. Correlates of proximal premeditation among recently hospitalized suicide attempters. Journal of Affective Disorders. 2013 doi: 10.1016/j.jad.2013.02.004. 10.1016/j.jad.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Morin C, Stone J, Trinkle D, et al. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993;8:463–467. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- 21.Morin C, Vallieres A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16) Sleep. 2007;30:1547–1554. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noh H, Joo E, Kim S, et al. The relationship between hippocampal volume and cognition in patients with chronic primary insomnia. J Clin Neurol. 2012;8:130–138. doi: 10.3988/jcn.2012.8.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23•.Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, et al. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Rev Med. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. Insomnia reduces problem solving capacity. [DOI] [PubMed] [Google Scholar]
- 24•.Keilp J, Gorlyn M, Russell M, et al. Neuropsychological function and suicidal behavior:attention control, memory and executive dysfunction in suicide attempt. Psychol Med. 2013;43:539–551. doi: 10.1017/S0033291712001419. Past suicide attempters exhibit reduced attention and working memory performance as compared with depressed non-attempters and non-depressed controls regardless of current severity of suicidal thoughts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keilp J, Gorlyn M, Oquendo M, et al. Attention deficit in depressed suicide attempters. Psychiatry Res. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keilp J, Sackeim H, Brodsky B, et al. Neuropsychological dysfunction in depressed suicide attempters. Am J Psychiatry. 2001;158:735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- 27.Pollock L, Williams J. Problem-solving in suicide attempters. Psychol Med. 2004;34:163–167. doi: 10.1017/s0033291703008092. [DOI] [PubMed] [Google Scholar]
- 28.Gibbs L, Dombrovski A, Morse J, et al. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009;24:1396–1404. doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29•.Monti J. Serotonin control of sleep-wake behavior. Sleep Med Rev. 2011;15:269–281. doi: 10.1016/j.smrv.2010.11.003. Serotonin helps regulate the induction and maintenance of sleep. [DOI] [PubMed] [Google Scholar]
- 30.Silber B, Schmitt J. Effects of tryptophan loading on human cognition, mood, and sleep. Neurosci Biobehav Rev. 2010;34:387–407. doi: 10.1016/j.neubiorev.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 31.Aszalos Z. Effects of antidepressants on sleep. Orv Hetil. 2006;147:773–783. [PubMed] [Google Scholar]
- 32•.Elmenhorst D, Kroll T, Matusch A, et al. Sleep deprivation increases cerebral serotonin 2A receptor binding in humans. Sleep. 2012;35:1615–1623. doi: 10.5665/sleep.2230. Sleep deprivation induces serotonergic dysfunction in the form of increased cerebral serotonin receptor binding potential. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Novati A, Roman V, Cetin T, et al. Chronically restricted sleep leads to depression-like changes in neurotransmitter receptor sensitivity and neuroendocrine stress reactivity in rats. Sleep. 2008;31:1579–1585. doi: 10.1093/sleep/31.11.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roman V, Luiten PG, Meerlo P. Too little sleep gradually desensitizes the serotonin 1A receptor system. Sleep. 2005;28:1505–1510. [PubMed] [Google Scholar]
- 35••.Chatzittofis A, Nordström P, Hellström C, et al. CSF 5-HIAA, cortisol and DHEAS levels in suicide attempters. Eur Neuropsychopharmacol. 2013 doi: 10.1016/j.euroneuro.2013.02.002. Serotonergic dysfunction is a common finding among suicide victims and perpetrators of violence upon others. [DOI] [PubMed] [Google Scholar]
- 36.Miller J, Hesselgrave N, Ogden R, et al. Positron Emission Tomography Quantification of Serotonin Transporter in Suicide Attempters with Major Depressive Disorder. Biol Psychiatry. 2013 doi: 10.1016/j.biopsych.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nye J, Purselle D, Plisson C, et al. Decreased brainstem and putamen SERT binding potential in depressed suicide attempters using [11-C]-ZIENT PET imaging. Depress Anxiety. 2013 doi: 10.1002/da.22049. [DOI] [PubMed] [Google Scholar]
- 38.Bose S, Mehta M, Selvaraj S, et al. Presynaptic 5-HT1A is related to 5-HTT receptor density in the human brain. Neuropsychopharmacology. 2011;36:2258–2265. doi: 10.1038/npp.2011.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Erritzoe D, Holst K, Frokjaer V, et al. A nonlinear relationship between cerebral serotonin transporter and 5-HT(2A) receptor binding: an in vivo molecular imaging study in humans. J Neurosci. 2010;30:3391–3397. doi: 10.1523/JNEUROSCI.2852-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40•.Mann J. The serotonergic system in mood disorders and suicidal behaviour. Philos Trans R Soc Lond B Biol Sci. 2013;368 doi: 10.1098/rstb.2012.0537. Serotonergic dysfunction in the prefrontal cortex is associated with poor decision-making and executive function. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bonnet MH, Arand DL. 24-Hour metabolic rate in insomniacs and matched normal sleepers. Sleep. 1995;18:581–588. doi: 10.1093/sleep/18.7.581. [DOI] [PubMed] [Google Scholar]
- 42••.Han K, Kim L, Shim I. Stress and sleep disorder. Exp Neurobiol. 2012;21:141–150. doi: 10.5607/en.2012.21.4.141. Stress induces HPA dysfunction which in turn increases susceptibility to hyperarousal, REM alterations, and suicidal behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Medicine Reviews. 2010;14:9–15. doi: 10.1016/j.smrv.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 44.Krystal J, Neumeister A. Noradrenergic and serotonergic mechanisms in the Neurobiology of posttraumatic stress disorder and resilience. Brain Res. 2009;1293:13–23. doi: 10.1016/j.brainres.2009.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cartwright R. Dreams and adaptation to divorce. In: Barrett D, editor. Trauma and Dreams. Cambridge, Mass: Harvard University Press; 1996. pp. 179–185. [Google Scholar]
- 46.Aurora RN, Zak RS, Auerbach SH, et al. Best practice guide for the treatment of nightmare disorders in adults. Journal of Clinical Sleep Medicine. 2010;6:389–401. [PMC free article] [PubMed] [Google Scholar]
- 47.Hudson S, Whiteside T, Lorenz R, et al. Prazosin for the treatment of nightmares related to posttraumatic stress disorder: a review of literature. Prim Care Companion CNS Disord. 2012;14 doi: 10.4088/PCC.11r01222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Houwelingen C, Beersma D. Seasonal changes in 24-h patterns of suicide rates: a study on train suicides in The Netherlands. J Affect Disord. 2001;66:215–223. doi: 10.1016/s0165-0327(00)00308-6. [DOI] [PubMed] [Google Scholar]
- 49.Altamura C, VanGastel A, Pioli R, et al. Seasonal and circadian rhythms in suicide in Cagliari, Italy. J Affect Disord. 1999;53:77–85. doi: 10.1016/s0165-0327(98)00099-8. [DOI] [PubMed] [Google Scholar]
- 50.Preti A, Miotto P. Diurnal variations in suicide by age and gender in Italy. J Affect Disord. 2001;65:253–261. doi: 10.1016/s0165-0327(00)00232-9. [DOI] [PubMed] [Google Scholar]
- 51.Erazo N, Baumert J, Ladwig K. Sex-specific time patterns of suicidal acts on the German railway system. An analysis of 4003 cases. J Affect Disord. 2004;83:1–9. doi: 10.1016/j.jad.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 52.Hasler B, Germain A, Nofzinger E, et al. Chronotype and diurnal patterns of positive affect and affective neural circuitry in primary insomnia. J Sleep Res. 2012;21:515–526. doi: 10.1111/j.1365-2869.2012.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53••.Selvi Y, Aydin A, Boysan M, et al. Associations between chronotype, sleep quality, suicidality, and depressive symptoms in patients with major depression and healthy controls. Chronobiol Int. 2010;27:1813–1828. doi: 10.3109/07420528.2010.516380. Morning preference is protective against the incidence of major depression and provides relief of symptoms among those who already suffer from major depression regardless of subjective sleep quality. [DOI] [PubMed] [Google Scholar]
- 54•.Kitamura S, Hida A, Watanabe M, et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol Int. 2010;27:1797–1812. doi: 10.3109/07420528.2010.516705. Evening preference is associated with multiple insomnia symptoms and the incidence of depression. [DOI] [PubMed] [Google Scholar]
- 55.Hirata F, Lima M, de Bruin V, et al. Depression in medical school: the influence of morningness-eveningness. Chronobiol Int. 2007;24:939–946. doi: 10.1080/07420520701657730. [DOI] [PubMed] [Google Scholar]
- 56.Merikanto I, Kronholm E, Peltonen M, et al. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol Int. 2012;29:311–317. doi: 10.3109/07420528.2012.655870. [DOI] [PubMed] [Google Scholar]
- 57.Selvi Y, Aydin A, Atli A, et al. Chronotype differences in suicidal behavior and impulsivity among suicide attempters. Chronobiol Int. 2011;28:170–175. doi: 10.3109/07420528.2010.535938. [DOI] [PubMed] [Google Scholar]
- 58.Merikanto I, Lahti T, Puolijoki H, et al. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol Int. 2013;30:470–477. doi: 10.3109/07420528.2012.741171. [DOI] [PubMed] [Google Scholar]
- 59.Lucassen E, Zhao X, Rother K, et al. Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One. 2013;8:e56519. doi: 10.1371/journal.pone.0056519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mogabgab O, Wiviott S, Antman E, et al. Relation Between Time of Symptom Onset of ST-Segment Elevation Myocardial Infarction and Patient Baseline Characteristics: From the National Cardiovascular Data Registry. Clin Cardiol. 2013;36:222–227. doi: 10.1002/clc.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kelly-Hayes M, Wolf P, Kase C, et al. Temporal patterns of stroke onset. The Framingham Study. Stroke. 1995;26:1343–1347. doi: 10.1161/01.str.26.8.1343. [DOI] [PubMed] [Google Scholar]
- 62.Nofzinger E, et al. Eszopiclone reverses brain hyperarousal in insomnia: Evidence from [18]-FDG PET. Sleep. 2008;31:A232. [Google Scholar]
- 63.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barraclough B, Pallis DJ. Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychological Medicine. 1975;5:61. doi: 10.1017/s0033291700007212. [DOI] [PubMed] [Google Scholar]
- 65.Fawcett J, Scheftner WA, Fogg L, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 66.Agargun M, Kara H, Solmaz M. Subjective Sleep Quality and Suicidality in Patients with Major Depression. J Psychiat Res. 1997;31:377–381. doi: 10.1016/s0022-3956(96)00037-4. [DOI] [PubMed] [Google Scholar]
- 67.Agargun MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–251. doi: 10.4088/jcp.v58n0602. [DOI] [PubMed] [Google Scholar]
- 68.Agargun M, Cilli A, Kara H, et al. Repetitive and Frightening Dreams and Suicidal Behavior in Patients with Major Depression. Comprehensive Psychiatry. 1998;39:198–202. doi: 10.1016/s0010-440x(98)90060-8. [DOI] [PubMed] [Google Scholar]
- 69.Krakow B, Artar A, Warner T, et al. Sleep disorder, depression, and suicidality in female sexual assault survivors. Crisis. 2000;21:163–170. doi: 10.1027//0227-5910.21.4.163. [DOI] [PubMed] [Google Scholar]
- 70.Tanskanen A, Tuomilehto J, Vinamaki H, et al. Nightmares as Predictors of Suicide. Sleep. 2001;24:844–847. [PubMed] [Google Scholar]
- 71.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- 72.Agargun MY, Cartwright R. REM Sleep, Dream Variables and Suicidality in Depressed Patients. Psychiatry Res. 2003;119:33–39. doi: 10.1016/s0165-1781(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 73.Smith M, Perlis M, Haythornthwaite J. Suicidal Ideation in Outpatients with Chronic Musculoskeletal Pain. Clin J Pain. 2004;20:111–118. doi: 10.1097/00002508-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 74.Bernert R, Joiner T, Cukrowicz K, et al. Suicidality and Sleep Disturbances. Sleep. 2005;28:1135–1141. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 75.Fujino Y, Mizoue T, Tokui N, et al. Prospective Cohort Study of Stress, Life Satisfaction, Self-Rated Health, Insomnia, and Suicide Death in Japan. Suicide Life Threat Behav. 2005;35:227–237. doi: 10.1521/suli.35.2.227.62876. [DOI] [PubMed] [Google Scholar]
- 76.Agargun M, Besiroglu L, Cilli A, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007;98:267–270. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 77.Chellappa S, Araujo J. Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res. 2007;153:131–136. doi: 10.1016/j.psychres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 78.Sjostrom N, Waern M, Hetta J. Nightmares and Sleep Disturbances in Relation to Suicidality in Suicide Attempters. Sleep. 2007;30:91–95. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 79.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 80.Bernert R, Reeve J, Perlis M, et al. Insomnia and nightmares as predictors of elevated suicide risk among patients seeking admission to emergency mental health facility. Sleep. 2009;32:A365–A366. [Google Scholar]
- 81.Lee J, Lee M, Liao S, et al. Prevalence of suicidal ideation and associated risk factors in the general population. J Formos Med Assoc. 2010;109:138–147. doi: 10.1016/S0929-6646(10)60034-4. [DOI] [PubMed] [Google Scholar]
- 82.Li SX, Lam SP, Yu MW, et al. Nocturnal sleep disturbance as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. Journal of Clinical Psychiatry. 2010;71:1140–1146. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 83.McCall WV, Blocker JN, D'Agostino R, Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Medicine. 2010;11:822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–98. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Benute G, Nomura R, Jorge V, et al. Risk of suicide in high risk pregnancy: an exploratory study. Rev Assoc Med Bras. 2011;57:583–587. doi: 10.1590/s0104-42302011000500019. [DOI] [PubMed] [Google Scholar]
- 86.Bjerkeset O, Romundstad P, Gunnell D. Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. Sleep. 2011;34:1155–1159. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Brower K, McCammon R, Wojnar M, et al. Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. Journal of Clinical Psychiatry. 2011;72:515–521. doi: 10.4088/JCP.09m05484gry. [DOI] [PubMed] [Google Scholar]
- 88.Carli V, Roy A, Bevilacqua L, et al. Insomnia and suicidal behavior in prisoners. Psychiatry Res. 2011;185:141–144. doi: 10.1016/j.psychres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 89.Krakow B, Ribeiro J, Ulibarri V, et al. Sleep disturbance and suicidal ideation in sleep medical center patients. Journal of Affective Disorder. 2011;131:422–427. doi: 10.1016/j.jad.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 90.Klimkiewicz A, Bohnert A, Jakubczyk A, et al. The association between insomnia and suicidal thoughts in adults treated for alcohol dependence in Poland. Drug Alcohol Depend. 2012;122:163. doi: 10.1016/j.drugalcdep.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bae S, Lee YCI, Kim S, et al. Risk factors for suicidal ideation of the general population. J Korean Med Sci. 2013;28:602–607. doi: 10.3346/jkms.2013.28.4.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gunnell D, Chang S, Tsai M, et al. Sleep and suicide: an analysis of a cohort of 394,000 Taiwanese adults. Soc Psychiatry Psychiatric Edpidemiol. 2013 doi: 10.1007/s00127-013-0675-1. org/10.1016/j.jad.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 93.Norra C, Richter N, Juckel G. Sleep disturbances and suicidality: A common association to look for in clinical practice and preventive care. EPMA J. 2011;2:295–307. doi: 10.1007/s13167-011-0101-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


