Abstract
Acupuncture treatment is generally regarded as a relatively safe procedure. However, most procedures have some complications and acupuncture treatment is no exception. Reported complications of acupuncture treatment were mostly mild or temporary symptoms, but certain severe adverse effects were also observed. We report here for the first time a case of liver abscess following acupuncture and moxibustion treatment.
Keywords: Acupuncture, Streptococcus intermedius, Liver Abscess, Moxibustion
INTRODUCTION
Since the sixth century when Chinese oriental medicine including acupuncture and herbs was introduced in Korea, acupuncture has been the most widely used procedure in the Korean society over the centuries as alternative or complementary medicine.1) Acupuncture is generally regarded as a less invasive, more natural, and less liable treatment by the general population.2) The National Institutes of Health Acupuncture Consensus Development Panel already concluded that acupuncture is either effective (2 conditions) or may be useful (12 conditions) in 1998.3) Acupuncture is effective in postoperative nausea, vomiting and dental pain, and also may be useful as an adjunct treatment for stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoarthritis, low back pain, carpal tunnel syndrome, and asthma.
However, most procedures have some complications and acupuncture treatment is no exception. Reported complications of acupuncture treatment were mostly mild or temporary symptoms. Minor adverse effects included bruising, tingling, tenderness on acupoints, and fainting, and more severe adverse effects included retroperitoneal abscess, tissue trauma, pneumothorax, cardiac tamponade, and peripheral nerve or spinal cord injuries.4-6) The use of non-sterile needles may cause infections as well, such as human immunodeficiency virus, hepatitis, and endocarditis.7) Here, we present a 69 year old man with pyogenic liver abscess (PLA) following acupuncture and moxibustion treatment.
CASE REPORT
A 69-year old male presented to the family medicine clinic in Pusan National University Hospital with a 1-month history of weight loss of 9 kg, fever, and nausea. He had been in stable health except for a recent onset of hypertension. However, his blood pressure was well-controlled with a calcium channel blocker. There was no significant additional history of dental procedure, dental disease, respiratory disease, gastrointestinal disease, liver disease, or other injury/trauma. His family members were all healthy.
Two months prior to presentation, he visited a Korean Oriental Medicine Clinic for insomnia. Since then, he had received acupuncture on his arms and moxibustion on his abdomen three times per week by using 'Jang-chim' which was about 9 cm long and 4 mm thick. About one month after the treatments, he started feeling nauseous and feverish. He also began to slowly lose body weight and experience reduced appetite. However, he continued to receive the treatment until he visited our family medicine clinic, because his Korean oriental medicinal doctor assured him that the symptoms were acupuncture-related side effects and would resolve spontaneously without additional treatment within a few days. Nevertheless, his symptoms remained and became even worse.
His mental status was alert. His vital signs were as follows: body temperature, 38.0℃; blood pressure, 120/80 mm Hg; pulse rate, 90/min; and respiration rate, 23/min. On physical examination, he showed mild icteric sclera and anemic conjunctiva. Inspection of the oral cavity revealed grossly normal floor of mouth without mild dehydrated tongue. He denied any respiratory difficulties, but soon showed tachypnea. His abdomen was mildly distended and tender without lymphadenopathy and hepatosplenomegaly. There were no abdominal skin defects. Laboratory findings were as follows: while blood cell count, 14,600/mm3, with 70% neutrophils; hemoglobin, 10.8 g/dL; aspartate transaminase, 47 IU/L; alanine transaminase, 54 IU/L; alkaline phosphatase, 1,113 IU/L; lactate dehydrogenase, 348 IU/L, total bilirubin, 1.68 mg/dL; and direct bilirubin, 0.49 mg/dL. Hepatitis A, B, and C serology was negative except for reactive anti-HBs and immunoglobulin G anti-HBc antibody. Other laboratory findings including thyroid function test, blood glucose, and tumor markers were within reference ranges.
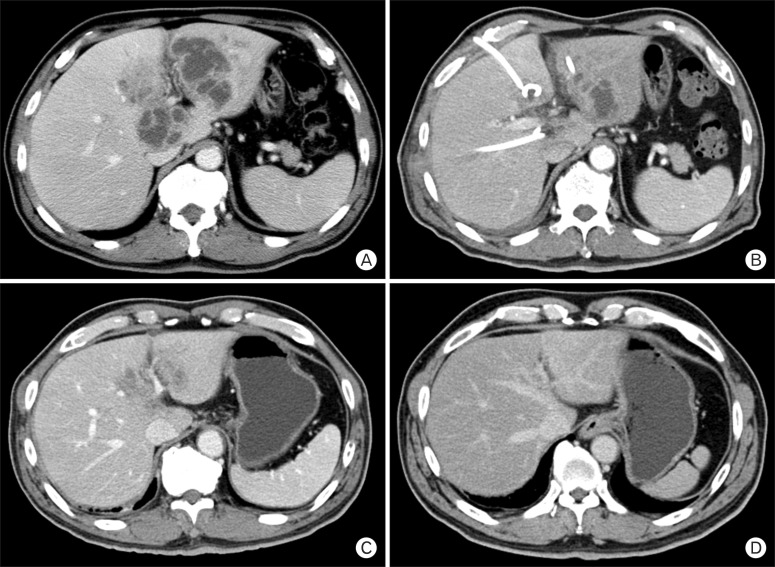
An abdominal computed tomography (CT) scan with contrast revealed multiseptated cystic lesions in the right and left lobes, the largest measuring about 10.0 cm in the left lobe (Figure 1). Pyogenic abscess was confirmed by ultrasound-guided percutaneous needle aspiration with Gram stain and culture of the aspirate. A culture of the drained pus grew Streptococcus intermedius, a member of the "Streptococcus milleri" group, which was susceptible to clindamycin, chloramphenicol, erythromycin, penicillin, and vancomycin. Anaerobic cultures were negative. He denied upper respiratory symptoms. No primary focus was identified in the upper respiratory tract, oral cavity, or skin.
Figure 1.
Computed tomography scan findings of liver abscess. (A) A 10 mm-sized, multi-septated abscess of the right and left hepatic lobe: day 1 of hospitalization. (B) Marked decrease in size of liver abscess after percutaneous drainage and antimicrobial therapy: 11th day of hospitalization. (C) Resolution of the abscess on the right lobe and a decrease in the size of the abscess on the left lobe: 6 weeks after initial antibiotic therapy and drainage procedure. (D) Complete resolution of the liver abscess: 5 months after discharge.
The patient was empirically started on intravenous cefotaxime and metronidazole before the culture and sensitivity results were available. The empiric antibiotics were changed to cefotaxime monotherapy according to the sensitivity results. After the drainage procedure and antibiotic medication, the patient's vital signs stabilized rapidly. On 18th day of his hospitalization, all laboratory findings on blood samples were normalized. Twenty-two days after admission, the patient was discharged on oral cefpodoxime to complete 4 weeks of therapy. Follow-up abdominal CT scan 6 weeks after initial antibiotic therapy and drainage procedure showed resolution of the abscess on the right lobe and a decrease in the size of the abscess on the left lobe. Another follow-up abdominal CT scan 5 months later showed complete resolution of the liver abscess. There was no sign of relapse or other side effects. Three years later, the patient is now under follow-up care without any specific problems. In this case, no primary source of infection from Streptococcus intermedius was found, except for acupuncture and moxibustion treatment history during the two months.
DISCUSSION
Liver abscess is a critical liver disease which can be classified into mainly two categories by its cause: PLA and amebic abscess.8) PLA is a potentially life-threatening infection but can be treated appropriately upon early detection due to the recent development of imaging modalities and selection of prompt antibiotic medication. In recent reports, the death rate from PLA mortality rate was about 10%.9-11) Klebsiella pneumoniae is the major pathogen of primary PLA in Asians.12) Streptococcus milleri was the major organism found in Australians.13) PLA can result from ascending infection in the biliary tract such as ascending cholangitis, vascular seeding secondary to bacteremia, direct invasion from a nearby source such as the gallbladder, or traumatic implantation such as perforation of the intestines.9) Identification of pathogens from positive blood cultures might suggest the pathway of infection. If pathogens like Streptococcus or Staphylococcus are cultured, hematogenous infection might be considered.9) This case of PLA was caused by Streptococcus intermedius, a member of the Streptococcus anginosus group (SAG). Streptococcus intermedius has an apparent tropism for the brain and liver.14,15) Pyogenic liver abscesses are an uncommon, but potentially life-threatening infection. The first cases of SAG hepatic abscesses were reported in 1975.16) Later, a study in 1981 found SAG to be the most common cause of hepatic abscesses.17) Streptococcus intermedius was the most frequent species found in a prospective study comparing the incidence and clinical features of SAG liver abscess to liver abscesses caused by other organisms.18) Several studies report no association with oral infection.19,20) To find out the cause, history taking and physical examination were conducted thoroughly. The patient had no presented risk factors such as history of drug abuse or biliary tract diseases, dental diseases, or skin disease, etc. In this case, we assume that the patient had Streptococcus intermedius bacteremia after being treated with contaminated acupuncture needles and Streptococcus intermedius was maybe seeded in the liver. The results of abdominal CT-scan led to liver abscess as a conclusive diagnosis, and Streptococcus intermedius was cultured, allowing for hematogenous dissemination. Korean Oriental Medicine has basically three types of therapeutic modalities including acupuncture, moxibustion, and herbal medicine. Acupuncture and moxibustion are increasingly being recognized as safe and useful therapeutic modalities which are used globally beyond East Asia.3,21) The abdomen is a common site for acupuncture. However, there are only a few case reports of potentially serious adverse events related to acupuncture and moxibustion,1-5,21) while most side effects are mild and transient.
Under these circumstances, we could reach the conclusion that the patient likely had a transient bacteremia from his acupuncture or moxibustion sites that seeded the liver. The timing between the onset of his symptoms and the acupuncture with moxibustion treatments suggest a causal relationship, although causation is sometimes difficult to determine beyond doubt. Recently, there was a case of an 80-year-old woman who presented with multiple epidural abscesses after acupuncture. This case also had no direct evidence but it was accepted because the acupuncture site and abscess region corresponded exactly.22) Our case was treated successfully by percutaneous drainage and antibiotic medication. To our knowledge, liver abscess has not previously been related to acupuncture or moxibustion in the literature. To prevent serious adverse effects of acupuncture and moxibustion, a few practices should be closely observed. These include maintaining clean needle techniques, receiving better training in anatomy, and lastly, paying greater attention to a patient's complaints. Adhering to these practices might spare a patient from many side effects and complications.
ACKNOWLEDGMENTS
This work was supported by a 2-Year Research Grant of Pusan National University.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ernst E. Acupuncture: a critical analysis. J Intern Med. 2006;259:125–137. doi: 10.1111/j.1365-2796.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- 2.Yin C, Park HJ, Chae Y, Ha E, Park HK, Lee HS, et al. Korean acupuncture: the individualized and practical acupuncture. Neurol Res. 2007;29(Suppl 1):S10–S15. doi: 10.1179/016164107X172301. [DOI] [PubMed] [Google Scholar]
- 3.Mayer DJ. Acupuncture: an evidence-based review of the clinical literature. Annu Rev Med. 2000;51:49–63. doi: 10.1146/annurev.med.51.1.49. [DOI] [PubMed] [Google Scholar]
- 4.Lao L. Safety issues in acupuncture. J Altern Complement Med. 1996;2:27–31. doi: 10.1089/acm.1996.2.27. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita H, Tsukayama H, Hori N, Kimura T, Tanno Y. Incidence of adverse reactions associated with acupuncture. J Altern Complement Med. 2000;6:345–350. doi: 10.1089/10755530050120718. [DOI] [PubMed] [Google Scholar]
- 6.Norheim AJ. Adverse effects of acupuncture: a study of the literature for the years 1981-1994. J Altern Complement Med. 1996;2:291–297. doi: 10.1089/acm.1996.2.291. [DOI] [PubMed] [Google Scholar]
- 7.White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122–133. doi: 10.1136/aim.22.3.122. [DOI] [PubMed] [Google Scholar]
- 8.Johannsen EC, Sifri CD, Madoff LC. Pyogenic liver abscesses. Infect Dis Clin North Am. 2000;14:547–563. vii. doi: 10.1016/s0891-5520(05)70120-3. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan GG, Gregson DB, Laupland KB. Population-based study of the epidemiology of and the risk factors for pyogenic liver abscess. Clin Gastroenterol Hepatol. 2004;2:1032–1038. doi: 10.1016/s1542-3565(04)00459-8. [DOI] [PubMed] [Google Scholar]
- 10.Jepsen P, Vilstrup H, Schønheyder HC, Sørensen HT. A nationwide study of the incidence and 30-day mortality rate of pyogenic liver abscess in Denmark, 1977-2002. Aliment Pharmacol Ther. 2005;21:1185–1188. doi: 10.1111/j.1365-2036.2005.02487.x. [DOI] [PubMed] [Google Scholar]
- 11.Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39:1654–1659. doi: 10.1086/425616. [DOI] [PubMed] [Google Scholar]
- 12.Lee TH, Park JH, Kim ST, Jung JH, Kim YS, Kim SM, et al. Clinical features of pyogenic liver abscess according to age group. Korean J Gastroenterol. 2010;56:90–96. [PubMed] [Google Scholar]
- 13.Pang TC, Fung T, Samra J, Hugh TJ, Smith RC. Pyogenic liver abscess: an audit of 10 years' experience. World J Gastroenterol. 2011;17:1622–1630. doi: 10.3748/wjg.v17.i12.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whiley RA, Beighton D, Winstanley TG, Fraser HY, Hardie JM. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol. 1992;30:243–244. doi: 10.1128/jcm.30.1.243-244.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whiley RA, Fraser H, Hardie JM, Beighton D. Phenotypic differentiation of Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus strains within the "Streptococcus milleri group". J Clin Microbiol. 1990;28:1497–1501. doi: 10.1128/jcm.28.7.1497-1501.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bateman NT, Eykyn SJ, Phillips I. Pyogenic liver abscess caused by Streptococcus milleri. Lancet. 1975;1:657–659. doi: 10.1016/s0140-6736(75)91760-2. [DOI] [PubMed] [Google Scholar]
- 17.Moore-Gillon JC, Eykyn SJ, Phillips I. Microbiology of pyogenic liver abscess. Br Med J (Clin Res Ed) 1981;283:819–821. doi: 10.1136/bmj.283.6295.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corredoira J, Casariego E, Moreno C, Villanueva L, López, Varela J, et al. Prospective study of Streptococcus milleri hepatic abscess. Eur J Clin Microbiol Infect Dis. 1998;17:556–560. doi: 10.1007/BF01708618. [DOI] [PubMed] [Google Scholar]
- 19.Tran MP, Caldwell-McMillan M, Khalife W, Young VB. Streptococcus intermedius causing infective endocarditis and abscesses: a report of three cases and review of the literature. BMC Infect Dis. 2008;8:154. doi: 10.1186/1471-2334-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Millichap JJ, McKendrick AI, Drelichman VS. Streptococcus intermedius liver abscesses and colon cancer: a case report. West Indian Med J. 2005;54:341–342. doi: 10.1590/s0043-31442005000500014. [DOI] [PubMed] [Google Scholar]
- 21.Park JE, Lee SS, Lee MS, Choi SM, Ernst E. Adverse events of moxibustion: a systematic review. Complement Ther Med. 2010;18:215–223. doi: 10.1016/j.ctim.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Yu HJ, Lee KE, Kang HS, Roh SY. Teaching NeuroImages: multiple epidural abscesses after acupuncture. Neurology. 2013;80:e169. doi: 10.1212/WNL.0b013e31828c2f1d. [DOI] [PMC free article] [PubMed] [Google Scholar]