Abstract
Objective
To describe how maternal obesity prevalence varies by established international and South Asian specific BMI cut-offs in women of Pakistani origin and investigate whether different BMI thresholds can help to identify women at risk of adverse pregnancy and birth outcomes.
Design
Prospective bi-ethnic birth cohort study (The Born in Bradford Cohort).
Setting
Bradford, a deprived city in the North of the UK.
Participants
8,478 South Asian and White British pregnant women participating in the Born in Bradford cohort study
Main outcome measures
Maternal obesity prevalence; prevalence of known obesity related adverse pregnancy outcomes: mode of birth, hypertensive disorders of pregnancy (HDP), gestational diabetes, macrosomia, pre-term births.
Results
Application of South Asian BMI cut-offs increased prevalence of obesity in Pakistani women from 18.8% (95% CI 17.6 to 19.9) to 30.9% (95% CI 29.5 to 32.2). With the exception of pre-term births, there was a positive linear relationship between BMI and prevalence of adverse pregnancy and birth outcomes, across almost the whole BMI distribution. Risk of gestational diabetes and HDP increased more sharply in Pakistani women after a BMI threshold of at least 30kg/m2, but there was no evidence of a sharp increase in any risk factors at the new, lower thresholds suggested for use in South Asian women. BMI was a good single predictor of outcomes (Area Under the Receiver Operating Curve: 0.596 to 0.685 for different outcomes); prediction was more discriminatory and accurate with BMI as a continuous variable than as a binary variable for any possible cut-point.
Conclusion
Applying the new South Asian threshold to pregnant women would markedly increase those referred for monitoring and lifestyle advice. However, our results suggest that lowering the BMI threshold in South Asian women would not improve the predictive ability for identifying those at risk of adverse pregnancy outcomes.
Keywords: Pregnancy, BMI, criteria, cut-off, adverse birth outcomes, obesity
Introduction
In the field of adult cardiovascular and metabolic diseases (including diabetes) there is a growing consensus that standard cut-off points for obesity are not equally valid across different ethnic groups, and in particular that these should be lowered for South Asians from the Indian subcontinent. (1-5) This viewpoint is being incorporated into disease prevention and control guidelines, both on the Indian subcontinent (Body Mass Index (BMI, kg/m2) of 25 for obesity) (5) and in the UK (BMI cut-off of 27.5 for obesity). (6) The repercussions are likely to be widespread and not merely confined to cardiovascular and metabolic diseases. Increasingly, researchers are reporting the prevalence of obesity and overweight using both standard World Health Organisation (WHO) and revised and provisionally recommended cut-offs for some Asian populations.
The WHO has suggested using lower thresholds to define overweight and obesity in South Asians. (7) These recommendations are based on the observation that at any given BMI level, South Asians tend to have higher body fat than White Europeans and are supported by expert consensus. However, at the time of their publication, there was little evidence regarding the impact of using these thresholds in clinical and public health practice. Since then, a number of studies have explored their impact focusing largely on cardio-metabolic outcomes or all-cause mortality. One study of 4688 White European and 1333 South Asian adults found that the magnitudes of differences in adverse cardiovascular outcomes (glycaemic, lipid and blood pressure outcomes) and type II diabetes, comparing those with a BMI over 30 kg/m2 to those below this threshold, were present at much lower BMI thresholds (23-28kg/m2) in South Asians than in White Europeans. (1) However, there is increasing evidence from very large collaborative projects that for major cardiovascular events and all-cause mortality, BMI has linear or ‘J’-shaped association across most of its distribution in all populations. (8, 9) That is to say, there is no clear threshold at which BMI results in a marked increase in adverse outcomes. There is a counterpoint that this lower cut-off is not appropriate for some outcomes, including general mortality (at least on the Indian subcontinent). (9-11) There are few studies of any other important health outcomes, and yet, increasingly, the findings in relation to diabetes and metabolism are being applied generally. It is important, therefore, to study the potential consequences of this growing movement to reduce the BMI cut-off, in relation to other health outcomes, and of particular importance and relevance is the cut-off for obesity in pregnant women in multi-ethnic populations.
Greater adiposity in pregnancy is associated with increased risk of gestational diabetes, hypertensive disorders of pregnancy, large for gestational age, birth weight, birth injury and caesarean section for most of these the association is continuous across most of the BMI distribution .(12) Consequently, many national and international antenatal guidelines require overweight and obese women to be identified early in pregnancy and advice and closer monitoring provided for these women. (13, 14) As with cardio-metabolic outcomes, the association of BMI with these outcomes is largely continuous across the whole distribution, but cut-points are necessary in clinical practice for easily identifying those at the top of the distribution who are most at risk. Currently, the cut-point most frequently recommended to identify pregnant women at risk is the WHO international definition of obesity 30kg/m2. To our knowledge, no current national antenatal guidelines recommend using a lower threshold of BMI to identify South Asian women at risk of adverse pregnancy or perinatal outcomes. Given that the relationship of BMI to adverse outcomes is likely to be largely driven by the effect of fat, (12) and that the newly recommended lower thresholds for South Asians are linked to evidence suggesting that fat mass (or percent fat) is greater in South Asians than other ethnic groups at any given BMI level, it is relevant to explore whether a lower threshold in these women would more effectively identify those at greatest risk.
The application of the lower WHO recommended South Asian specific cut-off for obesity of 27.5 kg/m2 would result in a greater number of referrals of South Asian women compared with using the same threshold of 30kg/m2 for all ethnic groups. In areas with large South Asian populations this could have a significant impact on health care resources; however, if these thresholds are better at identifying women at risk, who can then be effectively managed to reduce later adverse pregnancy outcomes, there could be net benefit. To our knowledge, no previous study has examined the extent to which the new South Asian thresholds increase the prevalence of maternal pregnancy obesity or better predict adverse pregnancy and birth outcomes compared with using the existing threshold of 30kg/m2 between ethnic groups. The aim of this study is to explore whether there is evidence that use of different thresholds of BMI in women of South Asian origin compared to White British women better identifies those at risk of adverse pregnancy and perinatal outcomes.
Method
A description of the full methodology for Born in Bradford is published separately elsewhere. (15, 16) Here, we provide details of the methods related to this study.
Setting
The study is set in Bradford, a city in the North of England with a population of nearly 500 000 and high levels of deprivation. Approximately 20% of the general population, and 50% of the women receiving antenatal care in the city are of South Asian origin.
Study cohort
Born in Bradford (BiB) is a longitudinal multi-ethnic birth cohort study aiming to examine environmental, psychological and genetic factors that impact on health and development perinatally, during childhood and subsequent adult life, and those that influence their parents’ health and wellbeing. All mothers intending to give birth at the Bradford Royal Infirmary from March 2007 to December 2010 were invited to take part in the research during their routine 26-28 week glucose tolerance test (GTT). Those not attending this appointment were approached elsewhere during routine hospital attendances whenever possible. A total of 12 453 women comprising 13 776 pregnancies were recruited to the study. Analysis in this paper includes only women of Pakistani (n=4547) and White British (n=3931) origin. Restriction to these two ethnic groups is because of the focus on comparing South Asian to white European women, the fact that they form the largest ethnic groups in BiB (and are relatively homogeneous), and that other ethnic groups were too small for separate analysis to be reliable. Additionally, participants were excluded from these analyses if they had not completed a baseline questionnaire in which information on ethnicity was collected (n=1 057), were carrying multiple births (n=142) or had missing data for delivery and pregnancy outcome details, ethnicity or pregnancy BMI (n=1 269). Following these exclusions, 8 478 mothers carrying a singleton pregnancy were included in the analyses.
Exposure data
Maternal BMI was calculated using height measured at baseline (26-28 weeks gestation) and weight measured at first antenatal clinic visit (approximately 12 weeks gestation) using Seca 2in1 scales (Harlow Healthcare Ltd, London, UK). Ethnicity was self-assigned by the mother at the baseline questionnaire using the same ethnic group classification of the 2001 UK census (17) and categorised into White British, Pakistani, Other South Asian (Indian, Bangladeshi and Other South Asian) and Other ethnicities (White other, Black, mixed race, other unspecified).
Outcome data
Outcomes included in the analysis were: mode of birth (caesarean section operative versus vaginal delivery (including babies delivered with forceps/ventouse); hypertensive disorders of pregnancy (gestational hypertension systolic BP ≥140mmHg or at least 30mmHg above 1st trimester BP or diastolic BP ≥90mmHg or at least 15mmHg above 1st trimester BP (at least 2 readings, one hour apart), with our without 1+ of proteinuria on dipstick); gestational diabetes (fasting plasma glucose ≥6.1mmol/l and/or 2-hr post challenge (with 75g Polycol glucose load) glucose ≥ 7.8mmol/l at 26-28 weeks); macrosomia (infant birth weight >4kg) and pre-term births (delivered <37 weeks gestation). These data were obtained from the obstetric medical records and in the case of gestational diabetes verified by the fasting and post load glucose measurements which are in the BiB database.
Ethics statement
Ethical approval for the study was obtained from the Bradford Research Ethics Committee (Ref 07/H1302/112) and all participants provided written informed consent prior to inclusion in the research.
Statistical analysis
All analyses were conducted using Stata statistical software, version 11.2 IC (StataCorp, TX). Maternal obesity was defined using WHO classification (BMI≥30kg/m2) and South Asian specific criteria (BMI ≥27.5kg/m2). Prevalence of obesity with 95% confidence intervals (95% CI) was calculated overall and by ethnicity. All possible thresholds were defined for BMIs between 19 and 40kg/m2 in one unit increments. This allowed us to test the predictive ability of the WHO international and South Asian specific cut-points in both ethnic groups, but also all other possible thresholds in order to determine which might be the best threshold for these pregnancy outcomes. Prevalence, sensitivity, specificity and positive and negative predictive values were calculated at each threshold for each pregnancy and perinatal outcome, Receiver Operating Characteristic (ROC) curves were constructed and the Area Under the ROC (AUROC) calculated to assess the overall accuracy of BMI (as a continuous variable in 1 unit increments) to predict the outcomes. All measurements are presented with 95% confidence intervals and are stratified by ethnicity. To examine whether associations were linear across the BMI distribution in both ethnic groups, we split BMI into fifths and used a likelihood ratio test to examine deviation from linearity (comparing a model in which the fifths were included as four indicators, to one in which they were included as an ordinal linear score). We examined the odds of each outcome per 5kg/m2 greater BMI in each ethnic group using multivariable logistic regression and determined whether this linear association differed between the two ethnic groups by including an interaction term between ethnic group and BMI in these thresholds.
Results
Obesity prevalence
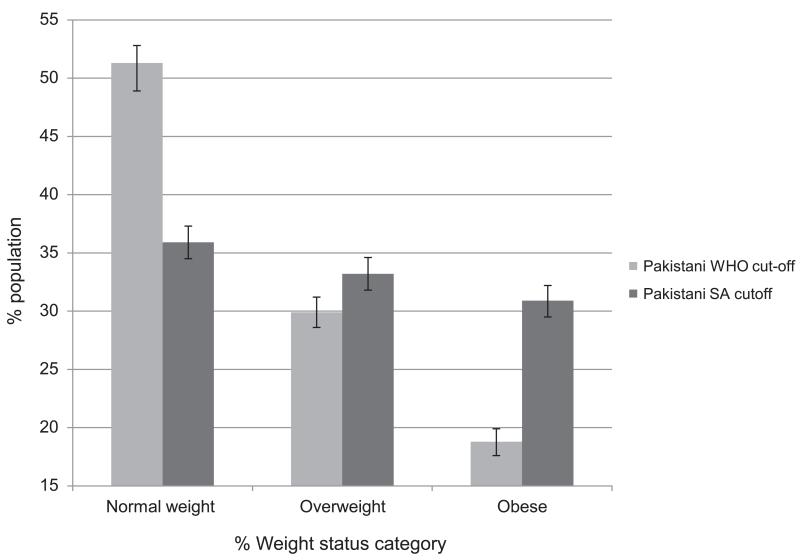
Table 1 shows the prevalence of pregnancy and birth outcomes by ethnicity. According to WHO criteria, approximately half of the sample were of normal BMI. Prevalence of obesity using these criteria (BMI ≥30) was 25.4% (n=999) in White British women, compared to 18.8% (n=853) in Pakistani women. Application of South Asian specific BMI criteria resulted in fewer Pakistani women being categorised as normal weight from 51.3% (95% CI; 49.9, 52.8) to 35.9% (95%CI; 34.5, 37.3) and an increase in obesity prevalence from 18.8% (95% CI; 17.6, 19.9) to 30.9% (95% CI; 29.5, 32.2), p < 0.001 for difference in BMI categories with the different criteria (Figure 1). If standard WHO criteria were applied to both groups the whole cohort prevalence of obesity would be 21.3%; this would increase to 28.3% (95%CI 27.4, 29.3) if the South Asian specific threshold were used to define obesity in the Pakistani women (with the White British women still defined using WHO thresholds), p<0.001, for difference in BMI categories for the whole cohort comparing use of standard WHO criteria for all to South Asian specific criteria in the Pakistani women.
Table 1.
Sample pregnancy and birth outcomes by maternal ethnicity (N (%) unless otherwise stated
| White British (n=3931) |
Pakistani (n=4547) |
All (n=8478) |
||
|---|---|---|---|---|
| Maternal BMI | Mean (SD) | 26.8 (6.0) | 25.6 (5.4) | 26.2 (5.7) |
| Normal weight (BMI<25.0) | 1816 (46.2) | 2335 (51.3) | 4151 (49.0) | |
| Overweight (BMI 25.0-29.9) | 1116 (28.4) | 1359 (29.9) | 2475 (29.2) | |
| Obese (BMI≥30) | 999 (25.4) | 853 (18.8) | 1852 (18.8) | |
| Maternal age | Mean (SD) | 26.9 (6.1) | 27.9 (5.2) | 27.4 (5.6) |
| Maternal education | <5 GCSEs | 771 (19.6) | 1170 (25.7) | 1941 (22.9) |
| 5+ GCSEs | 1350 (34.3) | 1425 (31.3) | 2775 (32.7) | |
| A level equivalent | 661 (16.8) | 576 (12.7) | 1237 (14.6) | |
| Degree level equivalent | 770 (19.6) | 1167 (25.7) | 1937 (22.9) | |
| Other | 335 (8.5) | 145 (3.2) | 480 (5.7) | |
| Don’t know/Missing | 44 (1.1) | 64 (1.4) | 108 (1.3) | |
| Gestational age (weeks) | Mean (SD) | 39.3 (1.9) | 39.1 (1.8) | 39.2 (1.8) |
| Preterm infants | (<37 weeks) | 227 (5.8) | 232 (5.1) | 459 (5.4) |
| Mode of birth | Vaginal birth | 3028 (77.0) | 3618 (79.6) | 6646 (78.4) |
| Caesarean Section | 903 (23.0) | 929 (20.4) | 1832 (21.6) | |
| Stillbirth | Yes | 18 (0.5) | 32 (0.7) | 50 (0.6) |
| HDP | Yes | 263 (6.7) | 244 (5.4) | 507 (6.0) |
| Gestational diabetes | Yes | 179 (4.5) | 426 (9.4) | 605 (7.1) |
| Infant birth weight (grams) | Mean (SD) | 3362 (562) | 3134 (534) | 3239 (559) |
| Macrosomia | >4kg | 467 (11.9) | 188 (4.1) | 655 (7.7) |
Figure 1. Weight status prevalence (95% CI) defined by WHO1 and South Asian2 specific BMI cut-offs.
1 BMI, (kg/m2) 20-24.9 = normal weight, 25-29.9 =overweight, ≥30 =obese
2 BMI, (kg/m2) 18.5-22.9 = normal weight, 23-27.5 =overweight, ≥27.5 =obese
Prevalence of adverse pregnancy and birth outcomes by BMI threshold
Figure 2 shows the prevalence of each outcome by cumulative increments of BMI, and Supplementary Web-Tables S1-S5 give prevalence, sensitivity, specificity and positive (PPV) and negative predictive values (NPV) together with 95% confidence intervals for each of these measurements. For all outcomes, except pre-term birth, there was a positive monotonic association between BMI and prevalence of outcomes. White British women had slightly higher prevalence of Caesarean section and hypertensive disorder of pregnancy, and more than double the prevalence of macrosomia compared to Pakistani women across the BMI distribution, but rates of increase in these outcomes with increasing BMI threshold were broadly similar in the two ethnic groups. In both groups the prevalence of Caesarean section increased more sharply after a BMI threshold of 36 Kg/m2. At all BMI threshold levels the prevalence of gestational diabetes was greater in Pakistani women compared to White British women and the rate of increase was greater in Pakistani women after a BMI of 33kg/m2. The prevalence of preterm birth was low in both groups compared with other outcomes and was not notably related to BMI threshold below 28kg/m2. The prevalence appeared to increase sharply between 28kg/m2 and 35kg/m2 and then returned to the earlier consistent value in Pakistani women. None of these analyses supported a marked increase in adverse pregnancy outcomes at a BMI threshold of 27.5kg/m2 in Pakistani women or at 30.0kg/m2 in either ethnic group.
Figure 2. Prevalence of adverse pregnancy and birth outcomes by cumulative BMI.
Table 2 further illustrates the generally linear association of BMI with outcomes in both ethnic groups, by highlighting the association of BMI as a linear exposure (per 5 kg/m2) with each outcome in each ethnic group. This table also shows p-values for deviation from linearity for each of these associations and also p-values for interaction between BMI and ethnicity (i.e. testing the null hypothesis that the linear association of BMI with each outcome is the same in each ethnic group). These results showed significantly increased odds between BMI (per 5kg/m2) and caesarean section, hypertensive disorder of pregnancy, macrosomia and gestational diabetes in both ethnic groups, and of pre-term birth in White British women. There was also a linear association across fifths of BMI for all outcomes in both ethnic groups with the exception of pre-term birth in Pakistani women. Thus, data confirms that (except for preterm births in Pakistani women; where no association was found), there is no strong statistical support for deviation from linearity in the association of BMI with each outcome for either group. Magnitudes of association of BMI, as a linear exposure, with caesarean births and hypertensive disorders of pregnancy were similar in the two ethnic groups. However, the magnitude of association of BMI with macrosomia and gestational diabetes was significantly higher in Pakistani women. This is further highlighted in Figure 2, in which the strength of the association is shown to be greater in White British women for macrosomia and greater for Pakistani women for gestational diabetes.
Table 2.
Associations of BMI with perinatal outcomes in Pakistani and White British women.
| Outcome | Pakistani women (N = 4547) | White British women (N = 3931) | p-interactiona | ||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Odds ratio (95%CI) per 5kg/m2 |
p-linearb | p-deviation from linearc |
Odds ratio (95%CI) per 5kg/m2 |
p-linearb | p-deviation from linearc |
||
| Caesarean section | 1.36 (1.27, 1.45) | <0.001 | 0.05 | 1.34 (1.26, 1.42) | <0.001 | 0.37 | 0.78 |
| Hypertensive disorder of pregnancy |
1.54 (1.39, 1.71) | <0.001 | 0.35 | 1.60 (1.46, 1.76) | <0.001 | 0.95 | 0.60 |
| Macrosomia | 1.57 (1.41, 1.75) | <0.001 | 0.48 | 1.36 (1.27, 1.47) | <0.001 | 0.89 | 0.04 |
| Gestational Diabetes | 1.55 (1.43, 1.69) | <0.001 | 0.44 | 1.25 (1.12, 1.40) | <0.001 | 0.29 | 0.003 |
| Pre-term birth | 0.98 (0.87, 1.11) | 0.216 | 0.41 | 0.87 (0.77, 0.98) | 0.03 | 0.41 | 0.17 |
Testing the null hypothesis that associations of BMI with outcome do not differ between Pakistani and White British women
Testing the null hypothesis that there is no linear association across fifths of BMI (i.e. p-value associated with linear increase across fifths)
Testing the null hypothesis that the association of BMI with outcomes does not deviate from linearity (tested by comparing a model in which fifths for BMI are entered as four indicator variables to one in which the fifths of BMI distribution are entered as one ordinal (linear score) variable, using a likelihood ratio test to compare the two) s four indicator variables to one in which the fifths of BMI distribution are entered as one ordinal (linear score) variable, using a likelihood ratio test to compare the two)
Diagnostic accuracy of BMI to predict adverse outcomes
There was no clear BMI threshold at which outcomes were more accurately identified (Supplementary Web Tables S1-S5) and no strong statistical evidence for deviation from linearity in either ethnic group for any outcomes (Table 2). Given the pattern of association of outcome prevalence with BMI thresholds shown in Figure 2, as expected, for all outcomes in both ethnic groups sensitivity and negative NPV decreased with increasing BMI threshold and specificity and positive predictive value PPV increased with increasing BMI thresholds. At all levels of BMI threshold, specificity and PPV were greater in women of Pakistani origin than of White British women, with sensitivity being correspondingly greater in White British women. For macrosomia PPV was lower and NPV higher in Pakistani women at all BMI thresholds. Receiver Operator Characteristic Area Under the Curve (ROC AUC) are shown in Figure 3. With the exception of pre-term births, results suggest that BMI alone, across the whole distribution (i.e. as a continuous variable), is an acceptable single predictor of adverse outcomes, (18-20) with AUROC ranging from 0.60 to 0.68. AUROC values were similar for White British and Pakistani women.
Figure 3. ROC Area Under the Curve for adverse outcomes with cumulative BMI increments.
Discussion
We have shown that, if the newly proposed South Asian specific BMI threshold of 27.5kg/m2 were applied to the BIB population, the prevalence of obesity in the whole cohort would increase from 21.3% to 28.3%. In clinical terms, for this one maternity unit with approximately 6000 deliveries per year (approximately 50% of whom are of Pakistani origin) this would result in an increase in the number of women referred for specialist obesity related antenatal care from 1 278 to 1 698 each year. Across the whole of the UK, it is estimated that there are 96 908 births to women of South Asian origin annually. If our results were generalisable to all South Asian women in the UK, the application of South Asian obesity cut-offs would increase the number of referrals of South Asian women by 11 726, from 18 219 to 29 945 each year. This increase in referrals would have a considerable impact on health care resources, and yet our results suggest that there is no increase in risk of adverse perinatal outcomes at a BMI threshold of 27.5kg/m2 (the South Asian threshold) or indeed at the established international threshold of 30.0Kg/m2, with most outcomes examined showing a positive linear association across most of the BMI distribution. Thus, for these outcomes, our findings do not support use of a South Asian specific BMI threshold.
BIB is a large birth cohort with high proportion of Pakistani women in which there is longitudinal outcome data. (16) We have only compared White British with Pakistani women, because there were too few numbers in other ethnic groups (including amongst those of ‘other’ South Asian ethnicity). It is possible that results may differ in other South Asian (or other Asian) groups. We did not examine how maternal BMI predicted still births in each ethnic group at different thresholds because of the low prevalence of this outcome (0.6% in the whole cohort). Since the relationship of BMI with the outcomes examined here is likely to be driven by body fat, and there is evidence that at a given BMI this is greater in South Asians, it would have been valuable to have had a more direct measure of body fat such as fat mass from DXA scans, or a marker of percent fat mass, from bioimpedance or skinfold thickness. Such measurements are not available in BiB. However, our study is relevant to clinical practice and exploring the suggestion that lower BMI thresholds should be used to identify individuals at risk if they are of South Asian origin. BMI is the most commonly used measure in clinical practice and screening all pregnant women with more complex measures, such as skinfold thicknesses that are influenced by practitioners skills or DXA scans which might be unacceptable due to the small radiation dose, is unlikely to be feasible.
Our findings of continuous linear associations of BMI across most of its distribution with adverse pregnancy outcomes in both White British and South Asian women is consistent with other studies showing the same across a number of different ethnic groups. (12) The directions were the same in both ethnicities and the magnitudes of the associations were broadly similar, with the exception of gestational diabetes prevalence, which was higher in women of Pakistani origin, and macrosomia which was lower in Pakistani compared to White British women at all BMI levels. Again, these findings are consistent with previous studies comparing prevalence rates for of gestational diabetes and macrosomia in women of South Asian and European origin. (21) Whilst our aim was not to develop a prediction tool for adverse pregnancy outcomes, it is notable that the discrimination properties of BMI alone when used as a continuous variable for predicting adverse pregnancy outcomes are reasonable. The AUROC of ~ 0.6 is comparable to that found for the Framingham prediction tool, which combines several risk factors to predict the risk of coronary heart disease and has been used in several populations. (18-20) It is possible that the addition of other risk factors such as family history and past obstetric history within a prediction tool would increase the accuracy for identifying women at risk of adverse pregnancy outcomes.
To our knowledge, this is the first study to examine the impact of applying the new South Asian BMI thresholds to a pregnant population. Other studies have examined this in more general (non-pregnant) populations. For example, Gray et al. (2011) concluded that a BMI of 21.5kg/m2 in South Asian women was equivalent to a BMI of 30 kg/m2 in terms of identifying those at risk of glycaemia. (1) However, that study was cross-sectional and tested correlations between BMI and risk factors rather than exploring the accuracy of individual BMI thresholds at predicting actual outcomes. Chui and colleagues (2011) investigated diabetes risk at differing BMI thresholds in White, South Asian, Chinese and Black adults. (2) This study used a longitudinal design to predict incidence rates of diabetes at a BMI of 30kg/m2 in White adults. Corresponding BMI values for other ethnic groups were then ascertained at this incidence rate; indicating that, in South Asian adults, the equivalent BMI threshold was 24 kg/m2. The effects of implementing differing BMI thresholds for specific groups is unclear, (3, 10). Even so, the evidence that South Asian populations incur a higher risk of many cardiovascular outcomes at lower WHO BMI thresholds, (7) has led to the NHS Health Checks programme in the UK using a BMI of 27.5 kg/m2 as the trigger for preventive action among people of South Asian origin. Public health guidance to support such decision making processes is currently being investigated by the National Institute for Health and Clinical Excellence; but this investigation does not include children or pregnant women from black and minority ethnic groups.
Our findings show that if the new South Asian BMI threshold of 27.5 kg/m2 were used to identify early pregnancy obesity, it would result in substantial increases in the referral of women for intensive monitoring and advice across the UK. We were unable to demonstrate that a lower BMI threshold would be more effective in identifying Pakistani women at increased risk of adverse perinatal outcomes. Indeed across most of the BMI range, associations were linear, with some evidence that risk of Caesarean section increased more steeply at a threshold of 36 kg/m2, but this was the same for both groups. Gestational diabetes increased more steeply at a threshold of 33 kg/m2 in women of Pakistani origin. Given the linear relationship up to this point, it may be more appropriate to suggest that policy makers should select a threshold that is appropriate in terms of funding and service provision, and consider the acceptability of labelling many women who are at low risk of certain adverse outcomes as ‘high risk’ (or conversely, not identifying all those who are truly high risk). Further research is therefore required to examine the cost-effectiveness of using different thresholds of BMI to identify women at risk of adverse perinatal outcomes. Importantly, this work provides further argument towards the need to revisit BMI standard cut-offs, at least in the context of child and maternal health, given that current threshold of 30kg/m2 is not fully evidence based. It is therefore recommended that the WHO sets up an expert consultation to address the question of the relationship between BMI and other measures of adiposity and a wide range of health outcomes, including pregnancy outcomes, as a matter of urgency. While cardiovascular diseases and diabetes are important, findings from this field do not necessarily apply to other fields. This paper highlights that a more critical stance is required than hitherto.
Supplementary Material
Acknowledgements
We are grateful to all the families who took part in this study, to the midwives for their help in recruiting them, the paediatricians and health visitors and to the Born in Bradford team which included interviewers, data managers, laboratory staff, clerical workers, research scientists, volunteers and managers.
Financial disclosure
This work was funded by an NIHR CLAHRC implementation grant and an NIHR applied programme grant (RP-PG-0407-10044). This paper presents independent research commissioned by the National Institute for Health Research (NIHR) under the CLAHRC programme. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
Footnotes
Conflicts of interest
The authors declare no conflict of interest. All authors had some financial support from an NIHR CLAHRC implementation grant and/or an NIHR applied programme grant (RP-PG-0407-10044) for the submitted work, but have had no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Supplementary information is available at the journal's website
References
- 1.Gray LJ, Yates T, Davies MJ, Brady E, Webb DR, Sattar N, et al. Defining Obesity Cut-Off Points for Migrant South Asians. PLoS ONE. 2011;6(10):e26464. doi: 10.1371/journal.pone.0026464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV. Deriving Ethnic-Specific BMI Cutoff Points for Assessing Diabetes Risk. Diabetes Care. 2011 Aug 1;34(8):1741–8. doi: 10.2337/dc10-2300. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Misra A. Revisions of cutoffs of body mass index to define overweight and obesity are needed for the Asian-ethnic groups. International Journal of Obesity and Related Metabolic Disorders. 2003;27(11):1294–6. doi: 10.1038/sj.ijo.0802412. [DOI] [PubMed] [Google Scholar]
- 4.Razak F, Anand SS, Shannon H, Vuksan V, Davi sB, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115(16):2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 5.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus Statement for Diagnosis of Obesity, Abdominal Obesity and the Metabolic Syndrome for Asian Indians and Recommendations for Physical Activity, Medical and Surgical Management. Journal of the Association of Physicians of India. 2009;57:163–70. [PubMed] [Google Scholar]
- 6.National Institute for Health and Clinical Excellence (NICE) Preventing type 2 diabetes: population and community level interventions in high risk groups and the general population. London: 2011. [Google Scholar]
- 7.WHO expert consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 8.Prospective Studies C Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. The Lancet. 373(9669):1083–96. //28. [Google Scholar]
- 9.Pierce BL, Kalra T, Argos M, Parvez F, Chen Y, Islam T, et al. A prospective study of body mass index and mortality in Bangladesh. International Journal of Epidemiology. 2010 Aug 1;39(4):1037–45. doi: 10.1093/ije/dyp364. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stevens J. Ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes Relat Metab Disord. 2003;27(11):1297–9. doi: 10.1038/sj.ijo.0802417. [DOI] [PubMed] [Google Scholar]
- 11.Pednekar MS, Hakama M, Hebert JR, Gupta PC. Association of body mass index with all-cause and cause-specific mortality: findings from a prospective cohort study in Mumbai (Bombay), India. International Journal of Epidemiology. 2008 Jun 1;37(3):524–35. doi: 10.1093/ije/dyn001. 2008. [DOI] [PubMed] [Google Scholar]
- 12.Lawlor DA, Relton C, Sattar N, Nelson SM. Maternal adiposity-a determinant of perinatal and offspring outcomes? Nat Rev Endocrinol. 2012 doi: 10.1038/nrendo.2012.176. advance online publication. [DOI] [PubMed] [Google Scholar]
- 13.(CMACE) CfMaCE . Maternal obesity in the UK: Findings from a national project. London: 2010. [Google Scholar]
- 14.National Institute of health and Clinical Excellence (NICE) Weight management before, during and after pregnancy. 2010. Contract No.: PH27. [Google Scholar]
- 15.Raynor P, Born in Bradford Bradford Collaborative Group Born in Bradford, a cohort study of babies born in Bradford, and their parents: Protocol for the recruitment phase. BMC Public Health. 2008;8:327. doi: 10.1186/1471-2458-8-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wright J, Small N, Raynor P, Tuffnell D, Bhopal R, Cameron N, et al. Cohort profile: The Born in Bradford multi-ethnic family cohort study. International Journal of Epidemiology. 2012 Oct 12; doi: 10.1093/ije/dys112. 2012. [DOI] [PubMed] [Google Scholar]
- 17.Office for National Statistics . Ethnic group statistics: A guide for the collection and classification of ethnicity data. The Stationary Office; HMSO Licensing Division; London: 2003. [Google Scholar]
- 18.Brindle P, Jonathan E, Lampe F, Walker M, Whincup P, Fahey T, et al. Predictive accuracy of the Framingham coronary risk score in British men:prospective cohort study. BMJ. 2003;327(7426):1267. doi: 10.1136/bmj.327.7426.1267. 2003-11-27 00:00:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Empana JP, Ducimetière P, Arveiler D, Ferrières J, Evans A, Ruidavets JB, et al. Are the Framingham and PROCAM coronary heart disease risk functions applicable to different European populations?: The PRIME Study. European Heart Journal. 2003 Nov 1;24(21):1903–11. doi: 10.1016/j.ehj.2003.09.002. 2003. [DOI] [PubMed] [Google Scholar]
- 20.May M, Lawlor DA, Brindle P, Patel R, Ebrahim S. Cardiovascular disease risk assessment in older women: can we improve on Framingham? British Women’s Heart and Health prospective cohort study. Heart. 2006 Oct 1;92(10):1396–401. doi: 10.1136/hrt.2005.085381. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vangen S, Stoltenberg C, Holan S, Moe N, Magnus P, Harris JR, et al. Outcome of Pregnancy Among Immigrant Women With Diabetes. Diabetes Care. 2003 Feb 1;26(2):327–32. doi: 10.2337/diacare.26.2.327. 2003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.