Abstract
Influenza A viruses from animal reservoirs have the capacity to adapt to humans and cause influenza pandemics. The occurrence of an influenza pandemic requires efficient virus transmission among humans, which is associated with virus attachment to the upper respiratory tract. Pandemic severity depends on virus ability to cause pneumonia, which is associated with virus attachment to the lower respiratory tract. Recently, a novel avian-origin H7N9 influenza A virus with unknown pandemic potential emerged in humans. We determined the pattern of attachment of two genetically engineered viruses containing the hemagglutinin of either influenza virus A/Shanghai/1/13 or A/Anhui/1/13 to formalin-fixed human respiratory tract tissues using histochemical analysis. Our results show that the emerging H7N9 virus attached moderately or abundantly to both upper and lower respiratory tract, a pattern not seen before for avian influenza A viruses. With the caveat that virus attachment is only the first step in the virus replication cycle, these results suggest that the emerging H7N9 virus has the potential both to transmit efficiently among humans and to cause severe pneumonia.
Influenza A viruses from animal reservoirs have the capacity to adapt to humans with the potential to cause human influenza pandemics. In the past 100 years, such influenza pandemics have occurred four times (subtype H1N1 in 1918, subtype H2N2 in 1957, subtype H3N2 in 1968, and subtype H1N1 in 2009) causing estimated excess mortality ranging from several hundred thousand to 50 million people.1 Recently, a novel avian-origin influenza A virus of the subtype H7N9 has emerged in humans.2 Little is known about this virus including its potential to cause an influenza pandemic.
The properties and epidemiological circumstances of a virus capable of causing an influenza pandemic include the opportunity for a novel virus to cross the species barrier from its non-human host species to humans, the ability of this virus to productively infect humans, and the ability of this virus to transmit efficiently among humans.3 The high mutation rate of the influenza virus, coupled with the segmented nature of its genome (which allows the generation of progeny viruses that have gene segments from two or more parent viruses) provides the antigenic changes necessary to cause a pandemic.4 The opportunity for such events to occur is greatest in regions where high densities of people co-exist with high densities of poultry, domestic pigs, and other species that act as influenza virus reservoirs.5 The severity of the subsequent pandemic depends largely on the ability of the novel virus to cause pneumonia. This, in turn, is dependent both on viral and host factors.6 Viral factors include specificity of the hemagglutinin (HA) for receptors on host cells, presence of a multibasic cleavage site in the HA, activity level of the neuraminidase, transcription efficiency of the polymerase complex proteins, and ability of non-structural protein 1 to antagonize the innate immune response. Host factors are predominantly the existence of homosubtypic or heterosubtypic immunity.
The ability of an influenza virus to attach to epithelial cells at different levels of the human respiratory tract—its pattern of virus attachment—is associated with both transmissibility and virulence. The transmissibility of influenza viruses correlates with the pattern of virus attachment to the human upper respiratory tract (URT). Influenza viruses that are transmitted efficiently among humans (such as human seasonal influenza viruses) attach abundantly to human URT, whereas inefficiently transmitted viruses [such as highly pathogenic avian influenza (HPAI) H5N1 virus] rarely attach to human URT.7–8 The difference in virulence of human seasonal influenza viruses and HPAI H5N1 virus correlates with the difference in the pattern of virus attachment in bronchioles and alveoli: HPAI H5N1 virus attaches more abundantly than human seasonal influenza viruses to nonciliated cuboidal epithelial cells (Clara cells) in the bronchioles and to type II pneumocytes and alveolar macrophages in the alveoli.8–10
In March 2013, the first human infections with a novel avian-origin influenza A virus of the subtype H7N9 were reported in three patients from eastern China. Based on phylogenetic analysis, this novel avian influenza A H7N9 virus was identified as a reassortant virus with the HA most closely related to an avian influenza A H7N3 isolate from a duck, the neuraminidase most closely related to an avian influenza A H7N9 isolate from an unspecified wild bird, and the internal genes most closely related to an avian influenza A H9N2 isolate from a brambling (Fringilla montifringilla; a small passerine bird in the finch family). All three patients developed severe pneumonia and acute respiratory distress syndrome, ultimately resulting in death.2 As of May 30, 2013, novel H7N9 virus infection has been confirmed in China and in 132 patients in Taiwan, of whom 37 have died [World Health Organization (WHO), http://www.who.int/influenza/human_animal_interface/influenza_h7n9/08_ReportWebH7N9Number.pdf, last accessed July 22, 2013]. The majority of patients with confirmed H7N9 virus infection had a history of exposure to live animals, with infected poultry being the suspected source of H7N9 virus.11 Some of the human isolates contained mutations in the polymerase or HA genes associated with adaptation to the mammals. Of specific interest is the Q226L amino acid substitution in HA, which is known to be associated with a switch in the receptor binding preference of HA from α2,3-linked sialic acids to α2,6-linked sialic acids.12 In two family clusters, there was a possible occurrence of limited human-to-human transmission of H7N9 virus after close, prolonged, unprotected contact.11 Unraveling the mechanism of attachment of this novel virus may help to assess its potential transmissibility and virulence.
We therefore determined the pattern of attachment of the emerging H7N9 viruses, with and without the Q226L amino acid substitution, to human respiratory tract and compared it with that of human influenza viruses that transmit efficiently among humans and have low intrinsic virulence, and HPAI viruses that transmit inefficiently among humans and have variable to high intrinsic virulence.
Materials and Methods
Ethics
Archival paraffin-embedded human tissues were obtained from the Department of Pathology (Erasmus University Medical Centre, Rotterdam, The Netherlands). Approval from the Medical Research Ethics Committee was obtained to use human archival respiratory tract tissues for virus attachment studies (MEC-2011-129).
Viruses and Tissues
Reassortant viruses consisting of seven gene segments of influenza virus A/PR/8/34 and the HA of either influenza virus A/Shanghai/1/13 (H7 Shanghai) or A/Anhui/1/13 (H7 Anhui) (emerging H7 virus group) were produced using reverse genetics techniques as described previously.13–14 We used synthetic open reading frame sequences based on sequences deposited by the WHO Chinese National Influenza Center in the Global Initiative on Sharing All Influenza Data (GISAID) EpiFlu Database. The original synthetic constructs were kindly provided by Dr. Richard Webby. The sequence of the HA of the recombinant viruses was confirmed by real-time PCR and sequencing using primers specific for the non-coding regions of HA. Contamination of the H7 virus stocks with other influenza virus subtypes was excluded by a generic real-time RT-PCR assay targeting HA of seasonal H1, and pandemic H1, H3, or H5 (Table 1). To verify these results by an independent method, HA of H7 Shanghai was amplified by PCR and subsequently cloned into a commercial vector (TOPO TA cloning kit; Invitrogen, Carlsbad, CA). Of the 27 cloned fragments sequenced, no mutations were observed at the receptor binding site, and no H1, H3, or H5 HA was detected.
Table 1.
Oligonucleotide Primers and Probes Used for Real-Time RT-PCR Assay Targeting the HA Gene of Different Influenza A Viruses
| Gene | Sequence | |
|---|---|---|
| H3 | Forward | 5′-GGGAAAAGCTCAATAATGAGATCAG-3′ |
| H3 | Reverse | 5′-TTGGGAATGCTTCCATTTGG-3′ |
| H3-1 | Probe | 5′-TGCACCCATTGGCAAATGCAATTC-3′ |
| H3-2 | Probe | 5′-TGCACCTATTGGCAAATGCAATTC-3′ |
| Seasonal H1-1 | Forward | 5′-CCAAAGTATGTCAGGAGTGCAAAAT-3′ |
| Seasonal H1-2 | Forward | 5′-CCAAAGTATGTCAGGAGTACAAAAT-3′ |
| Seasonal H1 | Reverse | 5′-CCTTCAATGAAACCGGCAAT-3′ |
| Seasonal H1 | Probe | 5′-TGGTTACAGGACTAAGGAACATCCCATCCA-3′ |
| Pandemic H1 | Forward | 5′-GGAAAGAAATGCTGGATCTGGTA-3′ |
| Pandemic H1 | Reverse | 5′-ATGGGAGGCTGGTGTTTATAGC-3′ |
| Pandemic H1 | Probe | 5′-TGCAATACAACTTGTCAGACACCCAAGGG-3′ |
| H5 | Forward | 5′-GGAACTTACCAAATACTGTCAATTTATTCA-3′ |
| H5 | Reverse | 5′-CCATAAAGATAGACCAGCTACCATGA-3′ |
| H5 | Probe | 5′-TTGCCAGTGCTAGGGAACTCGCCAC-3′ |
For comparison of pattern of attachment, a seasonal H3N2 virus (A/Netherlands/213/03) and pandemic H1N1 virus (pH1N1; A/Netherlands/602/09) (human influenza virus group) were included, as well as HPAI H5N1 virus (A/Vietnam/1194/04) and HPAI H7N7 virus (A/Netherlands/219/03) from human fatal cases (HPAI virus group). All viruses were passaged in Madin-Darby canine kidney cells and concentrated, inactivated, and fluorescein isothiocyanate (FITC)-labeled as described previously.9–10 Briefly, viruses were concentrated on a sucrose cushion and subsequently pelleted and resuspended in a small volume of PBS. Concentrated viruses were inactivated by dialysis against 0.1% formalin for 3 days. Inactivated viruses were labeled with an equal volume of 0.1 mg/mL FITC (Sigma-Aldrich, St. Louis, MO) in 0.5 mol/L bicarbonate buffer (pH 9.5). The concentration of the different virus suspensions used for virus histochemistry was standardized at 50 hemagglutination units/50 μL using hemagglutination assay.
Included human respiratory tract tissues consisted of the nasal concha, trachea, bronchus, and lung tissues. The lung tissues consisted of bronchi, bronchioles, and alveoli. All tissues included were without histological lesions and were from individuals without evidence of respiratory tract infection at the time of death. Given the scarcity of such tissues, tissues from three individual donors were tested, except for trachea, which was available from two donors. Age of the donors (n = 11, age of one donor unknown) ranged from 41 to 73 years, except for one donor who was 19 years of age.
Virus Histochemistry
The pattern of attachment of above-mentioned viruses was determined in the same donor tissues. The pattern of attachment of the viruses to human respiratory tract tissues was determined by virus histochemistry as described previously.9–10 Briefly, formalin-fixed, paraffin-embedded tissue sections were deparaffinized in xylene and hydrated using graded alcohols. FITC-labeled influenza viruses were incubated overnight at a concentration of 50 hemagglutination units/50 μL. For visualization by light microscopy, FITC was detected with a peroxidase-labeled rabbit–anti-FITC (DAKO, Glostrup, Denmark). The signal was amplified using a tyramide amplification system (Perkin-Elmer, Boston, MA). Peroxidase was revealed with 3-amino-ethyl-carbozyle (Sigma-Aldrich) resulting in a bright red precipitate. By light microscopy, the percentage of cells to which influenza viruses attached on the apical side was estimated and ranked on an ordinal scale without knowledge of donor or virus identity: rare (attachment to the apical side of <1% of epithelial cells), occasional (< 10%), moderate (< 50%), and abundant (≥ 50%). In addition, the main cell types to which influenza viruses attached were determined based on morphological characteristics and localization.
TRBC Hemagglutination Assay
Modified turkey red blood cells (TRBC) were prepared as described previously15 but with slight modifications. Briefly, all α2,3-, α2,6-, α2,8-, and α2,9-linked sialic acids were removed from the surface of TRBCs by incubating 62.5 μL of 1% TRBCs in PBS with 50 mU Vibrio cholerae neuraminidase (VCNA; Roche, Almere, The Netherlands) in 8 mmol/L CaCl at 37°C for 1 hour. Removal of sialic acids was confirmed by observation of complete loss of hemagglutination of the TRBCs by control influenza A viruses. Subsequently, resialylation was performed using 0.25 mU of α2,3-(N)-sialyltransferase (Cosmo Bio, Bio-Connect B.V., Huissen, The Netherlands) or 12 mU of α2,6-(N)-sialyltransferase (Cosmo Bio, Bio-Connect B.V.) and 1.5 mmol/L CMP-sialic acid (Sigma-Aldrich, Zwijndrecht, The Netherlands) at 37°C in 75 μL for 2 hours to produce α2,3-TRBCs and α2,6-TRBCs, respectively. After washing, the TRBCs were resuspended in PBS containing 1% bovine serum albumin to a final concentration of 0.5% TRBC. Resialylation was confirmed by hemagglutination of viruses with known receptor specificity; recombinant viruses with six gene segments of influenza virus A/PR/8/34 and HA and neuraminidase of A/Vietnam/1194/04 H5N1 without the basic cleavage site or with seven gene segments of influenza virus A/PR/8/34 and the HA of A/Netherlands/213/03 H3N2. Recombinant viruses with seven gene segments of influenza virus A/PR/8/34 and the HA of A/Anhui/1/13 or of A/Shanghai/1/13 were inactivated by treatment with β-propiolactone (Ferak Berlin, Berlin, Germany),16 and concentrated through a 20% sucrose cushion. Next, the receptor specificity was tested by performing a standard hemagglutination assay with the modified TRBCs. In brief, serial two-fold dilutions of virus in PBS were made in 50 μL volume; 50 μL of 0.5% TRBCs were added, followed by incubation for 1 hour at 4°C before determining the hemagglutination titer.
Results
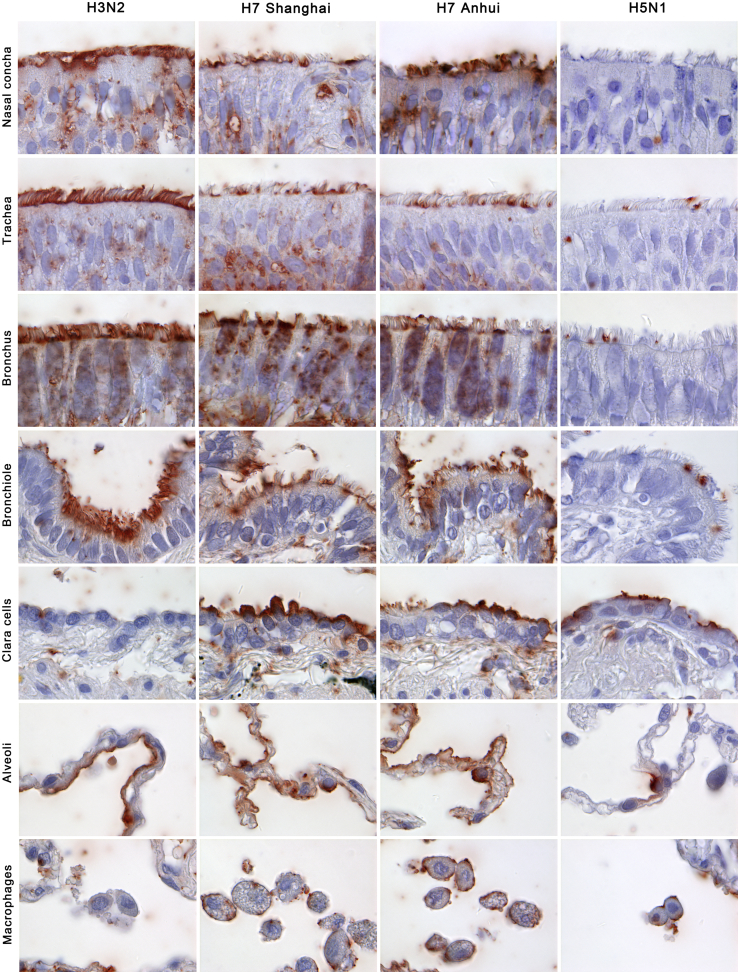
The pattern of virus attachment to human respiratory tract was similar within groups (human influenza viruses, emerging H7 viruses, and HPAI viruses) with two exceptions. In the human influenza virus group, attachment to nasal respiratory epithelium and bronchiolar epithelium was abundant for H3N2 and moderate for pH1N1. In the emerging H7 group, attachment to nasal respiratory epithelium was moderate for H7 Shanghai and abundant for H7 Anhui (Figure 1 and Table 2).
Figure 1.
Attachment of two reassortant viruses containing hemagglutinin of either influenza virus A/Shanghai/1/13 (H7 Shanghai) or A/Anhui/1/13 (H7 Anhui) to different parts of the upper and lower human respiratory tract. The attachment of a human seasonal influenza virus (H3N2) and a highly pathogenic avian influenza virus (H5N1) is shown for comparison.
Table 2.
Attachment of Human Influenza Viruses, Emerging Avian Influenza H7 Viruses, and Highly Pathogenic Avian Influenza Viruses to Different Parts of the Upper and Lower Human Respiratory Tract
| Tissue | n | Human influenza viruses |
Emerging avian influenza H7 viruses |
HPAI viruses |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| H3N2 |
pH1N1 |
H7 Shanghai |
H7 Anhui |
H7N7 |
H5N1 |
||||||||
| Score | Cell type | Score | Cell type | Score | Cell type | Score | Cell type | Score | Cell type | Score | Cell type | ||
| Nasal concha | 3 | ++ | Cil | + | Cil | + | Cil | ++ | Cil | − | ND | − | ND |
| Trachea | 2 | ++∗ | Cil | ++∗ | Cil | + | Cil | + | Cil | +/− | ND | +/− | ND |
| Bronchus | 3 | ++∗ | Cil | ++∗ | Cil | ++∗ | Cil | ++∗ | Cil | +/−∗ | ND | +/− | ND |
| Bronchioles | 3 | ++ | Cil | + | Cil | ++ | Cil & Clara | ++ | Cil & Clara | + | Clara | + | Clara |
| Alveoli | 3 | + | Type I | + | Type I | ++† | Type I & II | ++† | Type I & II | +† | Type II | +† | Type II |
Scores are median scores from individual tissues. Attachment of influenza viruses was ranked on an ordinal scale as follows: −, <1% cells positive; +/−, <10% cells positive; +, <50% cells positive; ++, ≥50% cells positive
Cil, ciliated epithelial cells; Clara, Clara cells; ND, not determined; Type I, type I pneumocytes; Type II, type II pneumocytes.
Intracellular attachment to goblet cells.
Additional virus attachment to alveolar macrophages.
Human influenza viruses (H3N2 and pH1N1) attached abundantly to the respiratory epithelium of nasal concha, trachea, bronchus, and bronchioles with a preference for ciliated cells over goblet cells. They attached moderately to alveolar epithelium with a preference for type I pneumocytes over type II pneumocytes.
Emerging H7 viruses (H7 Shanghai and H7 Anhui) attached moderately to the respiratory epithelium of nasal concha, trachea, and bronchus with a preference for ciliated cells over goblet cells. They attached abundantly to both ciliated and non-ciliated (Clara cells) cells of bronchioles and to both type I pneumocytes and type II pneumocytes of alveoli.
Highly pathogenic avian influenza viruses (H7N7 and H5N1) attached rarely to respiratory epithelium of nasal concha, trachea, and bronchus. They attached moderately to epithelium of bronchioles (with a preference for Clara cells over ciliated cells) and of alveoli (with a preference for type II pneumocytes over type I pneumocytes).
Attachment to goblet cells was not seen in the nasal concha for any viruses. Attachment to goblet cells was seen in the trachea for human influenza viruses only, and in the bronchus for all viruses except HPAI H5N1 virus. Attachment to alveolar macrophages was seen for all viruses except human influenza viruses.
The Q226L amino acid substitution in the HA has been shown to change the receptor binding preference of the HA protein from α2,3-linked sialic acids to α2,6-linked sialic acids in other influenza viruses.17 To confirm if Q226L amino acid substitution could change the receptor binding in HA of H7 Anhui,2 we tested its binding capacity to TRBCs expressing either of these sialic acids. H7 Shanghai showed predominant binding to α2,3-TRBCs with minimal binding to α2,6-TRBCs (Table 3). In contrast, H7 Anhui showed stronger binding to α2,6-TRBCs, although it retained some affinity to α2,3-TRBCs. The receptor specificity of the control viruses, A/Netherlands/213/03 and A/Vietnam/1194/04, was as expected. A/Netherlands/213/03 bound exclusively to α2,6-TRBC, whereas A/Vietnam/1194/04 bound exclusively to α2,3-TRBCs. These control viruses also showed that modified TRBCs expressed amounts of sialic acid that yielded equivalent hemagglutination titers to the titers obtained with regular TRBCs.
Table 3.
Receptor Specificity of the Emerging Avian Influenza H7 Viruses as Determined by a Modified Turkey Red Blood Cell (TRBC) Hemagglutination Assay
| Virus | Subtype | Hemagglutination titer (hemagglutination units/50 μL) |
||
|---|---|---|---|---|
| TRBC | α2,3-TRBC | α2,6-TRBC | ||
| A/Shanghai/1/13 | H7N9 | 64 | 16 | 2 |
| A/Anhui/1/13 | H7N9 | 32 | 10 | 16 |
| A/Netherlands/213/03 | H3N2 | 32 | 0 | 32 |
| A/Vietnam/1194/04 | H5N1 | 32 | 32 | 0 |
Control viruses were A/Netherlands/213/03, with a known receptor specificity for α2,6-linked sialic acids, and A/Vietnam/1194/04, with a known receptor specificity for α2,3-linked sialic acids
Discussion
H7 Shanghai and H7 Anhui viruses show a pattern of attachment not described before for any avian influenza virus, namely abundant attachment to epithelial cells of both upper and lower human respiratory tract. Like other avian influenza viruses,7,9 H7 Shanghai and H7 Anhui viruses have stronger attachment to lower parts of the human respiratory tract than to upper parts. However, the pattern of attachment of these emerging H7 viruses has three characteristics that are different from other avian influenza viruses, such as HPAI H5N1 and H7N7 viruses. First, the attachment to epithelial cells in bronchioles and alveoli is more abundant. Second, there is attachment to a broader range of cell types in bronchioles and alveoli. Third, the attachment to ciliated cells of nasal concha, trachea, and bronchi is more abundant.
The first two characteristics (more abundant attachment and broader range of cell types in bronchioles and alveoli) fit with increased virulence compared to that of human influenza viruses. The attachment of HPAI H5N1 and H7N7 viruses to epithelial cells in bronchioles and alveoli has been linked to the development of viral pneumonia and acute respiratory distress syndrome as primary disease from infection with these viruses in humans.8–10 However, virus attachment to target cells, although important, is not the only characteristic for causing disease. Low pathogenic avian influenza H5 and H6 viruses have the same pattern of attachment in the human lower respiratory tract as H5N1 but are not known to cause disease in humans.9 Other disease-causing characteristics that are important include the ability to replicate in and be released from host cells, to efficiently counteract the innate immune response, and to induce pro-inflammatory cytokine production by infected cells.18
The third characteristic (more abundant attachment to respiratory epithelium of upper parts of respiratory tract) suggests the potential for efficient transmission among humans.7 For H7 Anhui, a possible explanation for this characteristic is the Q226L amino acid substitution in the HA.2 As predicted from studies in other avian influenza viruses,17 this amino acid substitution changed the receptor binding preference of the HA protein from α2,3-linked sialic acids to α2,6-linked sialic acids (Table 3). α2,6-linked sialic acids are more abundant on the human tracheal epithelium and might increase the ability of the virus to be transmitted by air.19–20 However, this amino acid substitution was absent in H7 Shanghai, which had the predicted specificity for α2,3-linked sialic acids (Table 3). However, H7 Shanghai bound just as well to human respiratory epithelium as H7 Anhui except for moderate rather than abundant attachment to nasal respiratory epithelium (Table 2). Therefore, there must be other intrinsic factors in this virus that confer improved attachment to ciliated epithelial cells in the upper parts of the human respiratory tract. Other variables that influence the binding specificity include glycosylation and sialylation close to the receptor binding site21 for HA and the type of sialic acid, alternative linkages,22 and sulfation and fucosylation of the saccharide residues23 for the receptor.
Besides abundant attachment to respiratory epithelium of upper respiratory tract, an influenza virus may require other properties for efficient airborne transmission. Although the exact properties required for tranmission are not known, it has been speculated that these include replication to high titers in the URT and release and aerosolization of single virus particles.24 The proteins forming the viral polymerase complex are important for replication efficiency. Amino acid substitutions in the polymerase proteins have been shown to be the major determinants of host range and transmission, and the amino acid substitution Glu627 to Lys627 in the polymerase complex protein PB2 has been associated with increased virus replication at the lower temperature of the human URT than the core body temperature of birds.24–25 This amino acid substitution was also present in the HPAI H5N1 viruses that were transmitted by air among ferrets19 as well as in the emerging H7N9 virus.12 For release and aerosolization of single virus particles, neuraminidase, which facilitates the release of newly formed virus particles budding from the host cell membrane, needs to be in balance with the HA. If not, the released particles may form virus aggregates, as is seen in HPAI H5N1 virus.24 The fact that emerging H7N9 virus can cause infection in individual cases, despite its ability to attach abundantly to the human URT and possess Glu627 to Lys627 substitution in PB2, suggests that it has not acquired all of the necessary properties for efficient transmission among humans.
In conclusion, the pattern of attachment of H7 Shanghai and H7 Anhui viruses have characteristics of both human and avian influenza viruses, which have previously not been observed in avian influenza viruses. These emerging H7 viruses have both moderate attachment to ciliated respiratory epithelium of nasal cavity and trachea—which correlates with efficient transmission among humans—and abundant attachment to both ciliated cells and Clara cells in bronchioles and both type I pneumocytes and type II pneumocytes in alveoli—which fits with high virulence in HPAI H5N1 and H7N7 viruses. These results indicate, that based just on the pattern of virus attachment, the H7N9 currently emerging in China has the potential both to cause severe pulmonary disease and to be efficiently transmitted among humans. However, it needs to be recognized that attachment is only the first step in the replication cycle of influenza virus in its host cell, and that other steps, as well as host response, need to be taken into account to fully understand the potential of these emerging H7 viruses to cause an influenza pandemic.
Acknowledgments
We thank the investigators at the WHO Chinese National Influenza Center, who determined and released the viral sequences from the GISAID EpiFlu Database on which this research is based; Frank van der Panne and Peter van Run for excellent technical assistance; Michael den Bakker and Rob Verdijk for the provision of human respiratory tract tissues; and Suzan Pas and Martin Schutten for primers and probes for the real-time RT-PCR targeting the HA of seasonal H1 and pandemic H1, H3, and H5 influenza viruses.
Footnotes
Supported by European Union FP7 ANTIGONE (contract number 278976), European Union FP7 FLUPIG (contract number 258084), NIAID-NIH (contract HHSN266200700010C), NHMRC C.J. Martin post-doctoral fellowship (1054081) (K.S.).
Disclosures: A.D.M.E.O. is partly employed by ViroClinics Biosciences B.V. and owns share certificates in ViroClinics Biosciences B.V. T.K. is a part-time consultant for ViroClinics Biosciences B.V.
References
- 1.Taubenberger J.K., Morens D.M. Influenza: the once and future pandemic. Public Health Rep. 2010;125(Suppl 3):16–26. [PMC free article] [PubMed] [Google Scholar]
- 2.Gao R., Cao B., Hu Y., Feng Z., Wang D., Hu W. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888–1897. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 3.Kuiken T., Holmes E.C., McCauley J., Rimmelzwaan G.F., Williams C.S., Grenfell B.T. Host species barriers to influenza virus infections. Science. 2006;312:394–397. doi: 10.1126/science.1122818. [DOI] [PubMed] [Google Scholar]
- 4.Steinhauer D.A., Skehel J.J. Genetics of influenza viruses. Annu Rev Genet. 2002;36:305–332. doi: 10.1146/annurev.genet.36.052402.152757. [DOI] [PubMed] [Google Scholar]
- 5.Webby R.J., Webster R.G. Emergence of influenza A viruses. Philos Trans R Soc Lond B Biol Sci. 2001;356:1817–1828. doi: 10.1098/rstb.2001.0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuiken T., Taubenberger J.K. Pathology of human influenza revisited. Vaccine. 2008;26(Suppl 4):D59–D66. doi: 10.1016/j.vaccine.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Riel D., den Bakker M.A., Leijten L.M., Chutinimitkul S., Munster V.J., de Wit E., Rimmelzwaan G.F., Fouchier R.A., Osterhaus A.D., Kuiken T. Seasonal and pandemic human influenza viruses attach better to human upper respiratory tract epithelium than avian influenza viruses. Am J Pathol. 2010;176:1614–1618. doi: 10.2353/ajpath.2010.090949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shinya K., Ebina M., Yamada S., Ono M., Kasai N., Kawaoka Y. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 9.van Riel D., Munster V.J., de Wit E., Rimmelzwaan G.F., Fouchier R.A., Osterhaus A.D., Kuiken T. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. Am J Pathol. 2007;171:1215–1223. doi: 10.2353/ajpath.2007.070248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Riel D., Munster V.J., de Wit E., Rimmelzwaan G.F., Fouchier R.A., Osterhaus A.D., Kuiken T. H5N1 virus attachment to lower respiratory tract. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 11.Li Q., Zhou L., Zhou M., Chen Z., Li F., Wu H. Preliminary report: epidemiology of the avian influenza A (H7N9) outbreak in China. N Engl J Med. 2013 http://dx.doi.org/10.1056/NEJMoa1304617 [Epub] [Google Scholar]
- 12.Liu Q., Lu L., Sun Z., Chen G.W., Wen Y., Jiang S. Genomic signature and protein sequence analysis of a novel influenza A (H7N9) virus that causes an outbreak in humans in China. Microbes Infect. 2013;15:432–439. doi: 10.1016/j.micinf.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 13.de Wit E., Spronken M.I., Bestebroer T.M., Rimmelzwaan G.F., Osterhaus A.D., Fouchier R.A. Efficient generation and growth of influenza virus A/PR/8/34 from eight cDNA fragments. Virus Res. 2004;103:155–161. doi: 10.1016/j.virusres.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 14.de Wit E., Munster V.J., van Riel D., Beyer W.E., Rimmelzwaan G.F., Kuiken T., Osterhaus A.D., Fouchier R.A. Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. J Virol. 2010;84:1597–1606. doi: 10.1128/JVI.01783-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nobusawa E., Ishihara H., Morishita T., Sato K., Nakajima K. Change in receptor-binding specificity of recent human influenza A viruses (H3N2): a single amino acid change in hemagglutinin altered its recognition of sialyloligosaccharides. Virology. 2000;278:587–596. doi: 10.1006/viro.2000.0679. [DOI] [PubMed] [Google Scholar]
- 16.Matrosovich M., Zhou N., Kawaoka Y., Webster R. The surface glycoproteins of H5 influenza viruses isolated from humans, chickens, and wild aquatic birds have distinguishable properties. J Virol. 1999;73:1146–1155. doi: 10.1128/jvi.73.2.1146-1155.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chutinimitkul S., van Riel D., Munster V.J., van den Brand J.M., Rimmelzwaan G.F., Kuiken T., Osterhaus A.D., Fouchier R.A., de Wit E. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J Virol. 2010;84:6825–6833. doi: 10.1128/JVI.02737-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuiken T., Riteau B., Fouchier R.A., Rimmelzwaan G.F. Pathogenesis of influenza virus infections: the good, the bad and the ugly. Curr Opin Virol. 2012;2:276–286. doi: 10.1016/j.coviro.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Herfst S., Schrauwen E.J., Linster M., Chutinimitkul S., de Wit E., Munster V.J., Sorrell E.M., Bestebroer T.M., Burke D.F., Smith D.J., Rimmelzwaan G.F., Osterhaus A.D., Fouchier R.A. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imai M., Watanabe T., Hatta M., Das S.C., Ozawa M., Shinya K., Zhong G., Hanson A., Katsura H., Watanabe S., Li C., Kawakami E., Yamada S., Kiso M., Suzuki Y., Maher E.A., Neumann G., Kawaoka Y. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki Y. Sialobiology of influenza: molecular mechanism of host range variation of influenza viruses. Biol Pharm Bull. 2005;28:399–408. doi: 10.1248/bpb.28.399. [DOI] [PubMed] [Google Scholar]
- 22.Wu W., Air G.M. Binding of influenza viruses to sialic acids: reassortant viruses with A/NWS/33 hemagglutinin bind to alpha2,8-linked sialic acid. Virology. 2004;325:340–350. doi: 10.1016/j.virol.2004.05.013. Erratum in: Virology 2004, 329:213–214. [DOI] [PubMed] [Google Scholar]
- 23.Gambaryan A., Tuzikov A., Pazynina G., Bovin N., Balish A., Klimov A. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology. 2006;344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 24.Sorrell E.M., Schrauwen E.J., Linster M., De Graaf M., Herfst S., Fouchier R.A. Predicting ‘airborne’ influenza viruses: (trans-) mission impossible? Curr Opin Virol. 2011;1:635–642. doi: 10.1016/j.coviro.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Wit E., Fouchier R.A. Emerging influenza. J Clin Virol. 2008;41:1–6. doi: 10.1016/j.jcv.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]