Abstract
Background
Youth with alcohol or marijuana dependence or disorders (substance use disorders [SUDs]) are at increased risk of acquiring sexually transmitted diseases (STDs). Sexual partner characteristics may explain the relationship between SUD and STD.
Methods
Clinical criteria for SUD, clinical STD diagnosis, and sexual partner characteristics were assessed among 15- to 24-year-old STD clinic attendees between 1999 and 2002 (n = 412). We used exact logistic regression and path analysis to examine the mediation effect of sexual partner characteristics (age discordance, incarceration, STD diagnosis, other partners, perceived alcohol problem, perceived marijuana problem, and a calculated composite measure) on the relationship between SUD and STD, adjusting for important demographics and condom use.
Results
We found evidence of mediation by partner characteristics on the relationship between SUD and STD. For the logistic regression analysis, adding the partner characteristic composite reduced the strength of the association between SUD and STD from a statistically significant odds ratio of 1.7 (95% confidence interval = 1.0–2.7) to a statistically nonsignificant odds ratio of 1.5 (95% confidence interval = 0.9–2.5). In the path analysis, adding the partner characteristic composite reduced the significant direct effect of SUD on STD (β = 0.5, P = 0.04) to statistically nonsignificant effect (β = 0.1, P = 0.2). We estimated that 31% of the total effect of SUD on STD was attributable to the indirect path through the composite partner characteristic measure.
Conclusions
Even when controlling for demographics and condom use, partner characteristics partially explained the association between SUD and STD.
Approximately 9 million sexually transmitted diseases (STDs) are acquired each year by 15 to 24 year olds in the United States.1 STDs are more common among youth who use alcohol or marijuana compared to nonusers.2–4 It follows logically that youth meeting clinical criteria for alcohol or marijuana dependence or disorders, hereafter referred to as substance use disorders (SUDs), are also at increased risk of STDs. The few studies considering youth with SUDs found that STDs are 2 to 8 times more common among youth with SUDs than youth without SUDs.5–7 Yet, the biobehavioral pathways between SUD and STD are unclear.
Sexual partner characteristics (e.g., age discordance, use of alcohol and marijuana, casual) may be an important link between SUD and STD acquisition. To be considered a mediator in the pathway between SUD and STD, partner characteristics must meet 3 criteria. First, partner characteristics must be associated with STD acquisition. Sexual partner characteristics are strongly associated with STD acquisition.3,8–10 Second, partner characteristics must be associated with SUD. Having a partner who is new, casual, or uses alcohol or marijuana is more common among youth with an SUD than youth without an SUD.11,12 Third, the direct relationship between SUD and STD must be reduced when partner characteristics are considered. There is surprisingly little consideration of the potential mediation effect of partner selection on the relation of SUD and STD.
Among 15- to 24-year-old youth attending an urban STD clinic, we assessed whether there was evidence that the association between SUD and STD was mediated by select sexual partner characteristics (i.e., STD in past year, ≥5 years age difference, previously in jail, other partners in past year, perceived alcohol problem, perceived marijuana problem, and a composite variable). Understanding the relationship between SUDs, STDs, and sexual partner characteristics will help clarity whether partner characteristics are a potentially important target for STD preventive interventions.
Materials and Methods
Design and Sample
The current study is a secondary analysis of data from The Relationship of Alcohol, Youth and Sexually Transmitted Disease Project, an interview and clinical assessment conducted among men and women aged 15 to 24 years old (n = 448) attending an urban STD clinic in Pittsburgh, PA.5 For this analysis, we excluded the youth who reported a race other than Black or White (n = 15) or reported exclusively the same sex relationships in the past year (n = 21), because the sample sizes in these groups were too small to maintain model stability. No exclusions were made on the basis of drug or substance use. Institutional Review Board approval was obtained for the study procedures from the University of Pittsburgh and for this analysis, from the University of Florida.
Sexually Transmitted Disease
Among all participants, clinical assessment was performed for chlamydia and gonorrhea (ProbeTec ET system, Becton Dickinson), syphilis (serologic test), genital herpes (viral culture for suspicious lesions), genital warts (clinical observation), and Trichomonas (wet-mount microscopy among women only). An individual diagnosed with any of the above diseases was defined as having a confirmed STD.
Substance Use Disorder
Participants who reported any alcohol or marijuana use in the past 12 months were asked the questions from a youth-specific version of the Structured Clinical Interview for Diagnostic and Statistical Manual-IV regarding current (past year) DSM-IV diagnosis of alcohol abuse, alcohol dependence, marijuana abuse, or marijuana dependence.13 Abuse of and dependence on other substances were not collected, but less than 5% of participants reported using other drugs in the previous month.5 For analysis, participants with alcohol or marijuana abuse or dependence were classified as having an SUD.
Sexual Partner Characteristics
On the basis of the literature about partners and sexual risk,3,8–10,14–17 we included the following 6 measures of partner characteristics: (1) ≥5 years age discordance, (2) previously incarcerated, (3) STD diagnosis in the past year, (4) other sexual partners in the past year, (5) perceived alcohol problem, and (6) perceived marijuana problem. Participants reported each characteristic for both their main partner and their most recent, not main partner. Responses for each partner were considered equally.
A partner was defined as having a perceived alcohol problem if the participant reported that their partner “needs to cut down his or her drinking,” “has been annoyed by people criticizing his or her drinking,” “has felt bad or guilty about his or her drinking,” or “has had to take a drink first thing in the morning to steady his or her nerves or get rid of a hangover.” A partner was defined as having a perceived marijuana problem if the participant reported that the partner smokes marijuana daily; approximately half of daily users are clinically dependent, and daily use is associated with increased sexual risk taking.18,19 Participants were not asked to report their partners' use of substances other than alcohol and marijuana. Despite unknown validity as a measure of the partner's actual drug use, participant's perception of partner drug use is likely a strong predictor of the participant's behavior.20,21
We calculated a simple composite partner characteristic variable that could be incorporated into clinical practice. For each of the 6 partner characteristics described above, we assigned a value of 0 to the referent category and 1 to the risk category. For each participant, we calculated the proportion of the responses in the risk category. This yielded a proportion ranging from 0 to 1 for each participant; 0 indicated all characteristics that were in the referent category, and 1 indicated all characteristics that were in the high-risk category. We divided this proportion into the following 3 broad groups: low (≤0.33), intermediate (>0.33 and ≤0.66), and high (>0.66). Details on assessing the validity of this composite measure can be found in our previous study.9
Covariates
On the basis of the role of condom use in STD acquisition and variation of condom use by partner type,9,22–24 we included condom use during last sex as a covariate. We also selected the following 4 demographic covariates: race, sex, age, and type of medical insurance.25,26 Type of medical insurance was categorized for analysis as any medical insurance (Medicaid or private insurance) or no insurance. Marital status was not included because 83% of participants were single.
Statistical Methods
We used logistic regression and path analysis to examine direct and indirect effects between sexual partner characteristics, SUD, and STD. For unadjusted exact logistic regression, we used SAS software, version 9.2 (SAS Institute, Inc, Cary, NC). For multivariable (all covariates) exact logistic regression, we used LogXact software, version 8.0 (Cytel Software Corporation, Cambridge, MA). Common to models with several covariates,27,28 we found that the exact permutation distribution for the sufficient statistic was computationally infeasible to calculate for our multivariable models; therefore, for multivariable models, we used the LogXact network-based Monte Carlo sampling approach for conditional logistic regression to estimate unbiased exact confidence intervals (CIs).27,28
We conducted path analyses in Mplus, version 5.2 (Muthén & Muthén, Los Angeles, CA), as a secondary approach of assessing the direct and indirect associations.29 The model was built in steps, with each step estimated while controlling for all covariates. First, bivariate relations were modeled between (1) SUD and STD, (2) partner characteristics and STD, and (3) partner characteristics and SUD. Second, the bivariate regression paths were modeled simultaneously. We estimated parameters with minimum variance-weighted least squares and indirect effects by calculating the product of the regression coefficients for SUD on partner characteristics and partner characteristics on STD. We used Sobel's method to estimate the standard error of the indirect effect.30
Results
Study Population Characteristics
The mean age of the 412 study participants was 20.4 years (2.2 standard deviation), ranging from 15 to 24 years. Among participants, 48% were male and 59% were Black. The median number of lifetime sex partners was 10 (range, 1–200) and the median number of partners in the past year was 3 (range, 1–50). Women were more likely than men to report partners with risk characteristics including discordant ages (odds ratio [OR] = 2.9, 95% CI = 1.7–4.9), previously in jail (OR = 5.3, 95% CI = 3.1–9.2), perceived alcohol problem (OR = 1.5, 95% CI = 1.0–2.3), and perceived marijuana problem (OR = 2.0, 95% CI = 1.3–3.1).
STDs were diagnosed among 27% (113/412) of youth with women and men equally likely to have an STD (OR =1.1, 95% CI = 0.7–1.7). SUDs were found among 43.2% (178/412) of the youth: 60 had a marijuana disorder, 56 had an alcohol disorder, and 62 had both marijuana and alcohol use disorders. SUDs were diagnosed among 34.0% of the women and 53.3% of the men (OR = 0.5, 95% CI = 0.3–0.7).
Association Between SUD and STD
STDs were more common among youth with SUDs (31.5%) than youth who did not have an SUD (24.4%). Even when adjusting for demographics, individuals with an SUD were 1.8 times (95% CI = 1.2–2.9) as likely as individuals without an SUD to have an STD. Path analysis also showed a direct effect between SUD and STD (β = 0.5, P = 0.04).
Association Between Partner Characteristics and STD
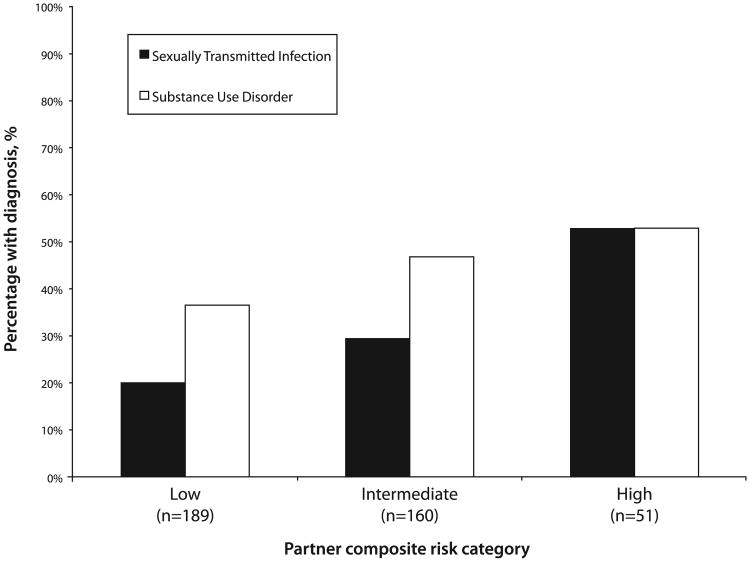
Youth who reported partners who had an STD in the past year or were ≥5 years different in age were around 3 times more likely than youth who did not report partners with these characteristics to be diagnosed with an STD (Table 1). Additionally, we found a linear relationship between increasing partner composite risk category and the percent of youth with an STD (Fig. 1). This relationship held when adjusting for demographics and condom use; compared to youth with low-risk sexual partners, youth with high-risk sexual partners were 3 times more likely to have an STD diagnosis (OR = 3.4, 95% CI = 1.6–7.0). Similarly, with path analysis, we found a direct effect between the composite partner characteristic measure and STD (β = 0.6, P < 0.0001).
Table 1. Associations Between Sexual Partner Characteristics and Sexually Transmitted Disease Diagnosis.
| Diagnosis of Sexually Transmitted Disease | ||||
|---|---|---|---|---|
|
|
||||
| With to Without Characteristic Adjusted* Odds Ratio | ||||
|
|
||||
| In Those With Characteristic % (n) | In Those Without Characteristic % (n) | OR | 95% CI | |
| Partner characteristics | ||||
| STD in past year | 46.2% (119) | 19.1% (204) | 3.4 | 2.0–5.7 |
| ≥5-yr age difference | 44.9% (98) | 23.3% (296) | 2.6 | 1.6–4.5 |
| Previously in jail | 35.8% (123) | 23.2% (233) | 1.6 | 0.9–2.5 |
| Had other partners in past year | 26.9% (234) | 22.3% (94) | 1.2 | 0.8–2.6 |
| Perceived alcohol problem | 29.4% (194) | 26.7% (206) | 1.2 | 0.8–1.9 |
| Perceived marijuana problem | 31.5% (143) | 26.1% (257) | 1.0 | 0.7–1.7 |
Adjusted for race, age, sex, and medical insurance.
indicates percent with STD with given characteristic; n, total number of adolescents in each group; OR, odds ratio; CI, confidence interval; STD, sexually transmitted disease.
Figure 1.
Proportion of youth with sexually transmitted diseases or substance use disorders for each partner composite risk category. n indicates the number of youth in each partner composite risk category.
Association Between Partner Characteristics and SUD
Youth who reported partners who were previously in jail or had a marijuana problem were more likely than youth who did not report partners with these characteristics to have an SUD (Table 2). The largest effect was found for the association between having a partner with a marijuana problem and having a current SUD (OR = 3.0, 95% CI = 1.9–5.0). When considering the partner characteristics together as the composite variable, we found a linear relationship between increasing risk category of the partner characteristic composite and SUD diagnosis (Fig. 1). Even when adjusting for demographics and condom use, compared to youth with low-risk sexual partners, youth with high-risk sexual partners were 3 times more likely to have a current SUD (OR = 3.4, 95% CI = 1.7–6.6). Path analysis also showed a direct effect between SUD and composite partner characteristics (β = 0.8, P < 0.0001).
Table 2. Associations Between Sexual Partner Characteristics and Substance Use Disorder.
| Substance Use Disorder | ||||
|---|---|---|---|---|
|
|
||||
| With to Without Characteristic Adjusted* Odds Ratio | ||||
|
|
||||
| In Those With Characteristic % (n) | In Those Without Characteristic % (n) | OR | 95% CI | |
| Partner characteristics | ||||
| STD in past year | 43.7% (119) | 38.7% (204) | 1.4 | 0.8–2.3 |
| ≥5-yr age difference | 46.9% (98) | 42.2% (296) | 1.6 | 0.9–2.7 |
| Previously in jail | 42.3% (123) | 40.8% (233) | 1.8 | 1.0–3.0 |
| Had other partners in past year | 46.2% (234) | 43.6% (94) | 1.1 | 0.7–2.0 |
| Perceived alcohol problem | 46.3% (201) | 40.3% (211) | 1.4 | 0.9–2.2 |
| Perceived marijuana problem | 55.2% (145) | 36.7% (267) | 3.0 | 1.9–5.0 |
Adjusted for race, age, sex, and medical insurance.
indicates percent with substance use disorder with given characteristic; n, total number of adolescents in each group; OR, odds ratio; CI, confidence interval; STD, sexually transmitted disease.
Relation Between STD and SUD Mediated by Partner Characteristics
In both logistic and path analyses, the association between SUD and STD was reduced in strength and became statistically nonsignificant when adding the composite partner characteristic measure. In the logistic regression analysis, adding the partner characteristic composite reduced the strength of the association between SUD and STD from a statistically significant OR of 1.7 (95% CI = 1.0–2.7) to a statistically nonsignificant OR of 1.5 (95% CI = 0.9–2.5) (Table 3).
Table 3. Mediation of Association Between Substance Use Disorder and Sexually Transmitted Disease Diagnosis by Each Partner Characteristic.
| Adjusted* Odds Between SUD and STD Diagnosis | ||
|---|---|---|
|
|
||
| Model Adjusted For | OR | 95% CI |
| Demographics and condom use only | 1.7 | 1.0–2.7 |
| Partner characteristic composite | 1.5 | 0.9–2.5 |
| Each partner characteristic separately | ||
| Partner had an STD in past year | 1.7 | 0.9–3.0 |
| ≥5-yr age difference between partners | 1.6 | 1.0–2.8 |
| Partner previously in jail | 1.3 | 0.8–2.2 |
| Partner had other partners in past year | 1.8 | 1.0–3.1 |
| Perceived partner alcohol problem | 1.6 | 1.0–2.7 |
| Perceived partner marijuana problem | 1.7 | 1.0–2.8 |
Adjusted for race, sex, medical insurance, age, and condom use last sex.
Each partner characteristic was entered into the model of SUD and STD separately.
OR indicates odds ratio; CI, confidence interval; STD, sexually transmitted disease; SUD, substance use disorder.
In the path analysis of SUD and STD, adding the partner characteristic composite measure reduced the significant direct effect of SUD on STD (β = 0.5, P = 0.04) to statistically nonsignificant effect (β = 0.1, P = 0.2). The indirect effect suggests that 31.2% of the total effect of SUD on STD is attributable to the indirect path through composite partner characteristics (indirect effect = 0.040, P = 0.012).
Some of the separate partner characteristics also mediated the association between SUD and STI (Table 3). We found the largest reduction in the OR between SUD and STD when adding having a partner previously in jail separately to the model (OR = 1.3, 95% CI = 0.8, 2.2) (Table 3). In path analysis, we did not find evidence of an indirect effect between SUD and STD when considering any of the partner characteristics separately.
Discussion
Even when controlling for demographics and condom use, we found that partner characteristics mediated the association between SUD and STD. This finding emphasizes the need to consider characteristics of both sexual partners in evaluation of STDs, especially among youth with SUDs. STD prevention among youth with SUDs is a substantial public health problem because among 18 to 25 year olds in the United States, 17.2% are abusing or dependent on alcohol and 5.6% are abusing or dependent on marijuana.31 The current study shows that selection of riskier partners by youth with SUDs is one explanation of why youth with SUDs are at increased risk of STD acquisition.
Our finding of a significant mediation of the association of SUD and STD by partner characteristics expands previous studies that have reported either direct effects of SUD and partner selection or partner selection and STD.9,12,16,32–37 SUDs may cause riskier partner selection because youth with SUDs are more likely than youth without SUDs to be using alcohol or marijuana before sex.12 Substance use before sex increases the probability of having sex with a new or casual partner, and may increase the probability of having unprotected sex with that partner.32–37
The composite measure of partner characteristics may be superior to considering each measure alone because it provided a comprehensive view of overall sexual risk of the partner, may present a more realistic representation of partner risk, and was consistently important for each direct and indirect effect. Furthermore, the composite partner characteristic accounted for one-third of the variance in the association between SUD and STD.
This study has 4 important limitations. First, because the current study is cross-sectional, we could not assess the temporal sequence. Second, because our study was a secondary analysis, we were restricted to available data. Specifically, we could not assess substances other than alcohol or marijuana, or consider participants reporting exclusively same sex partnerships. Third, partner characteristics might not be accurate because they represent the participant's perception.38,39 Fourth, participants might have come to the STD clinic because their partner was diagnosed with an STD. This potential selection bias could not account for the entire mediation effect observed because the report of partner's STD did not significantly mediate the association between SUD and STD.
This study has 4 important strengths. First, STDs among adolescents were diagnosed clinically as opposed to relying on self-report that may underestimate STDs because of social desirability bias in reporting and undiagnosed diseases.40 Second, the formal clinical assessment of SUDs limits diagnosis bias because all participants are evaluated uniformly. Third, we considered several partner characteristics, including a previously validated composite.9 Fourth, we found similar conclusions with 2 statistical methods (logistic regression and path analysis).
This study highlights the need for physicians and public health professionals to consider partner characteristics for STD detection and prevention, particularly among youth with SUDs. Partner characteristics can be routinely evaluated in physician offices with the composite measure used in this study. Moreover, substance use treatment centers should consider incorporating messages explaining partner risk markers into their STD prevention programs.
Acknowledgments
Supported by the National Institute of Health K01 AA018255; and the data collection was supported in part by the National Institute of Health K23 AA00303 and K02 AA00291.
References
- 1.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: Incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 2.Sen B. Does alcohol-use increase the risk of sexual intercourse among adolescents? Evidence from the NLSY97. J Health Econ. 2002;21:1085–1093. doi: 10.1016/s0167-6296(02)00079-6. [DOI] [PubMed] [Google Scholar]
- 3.Boyer CB, Sebro NS, Wibbelsman C, et al. Acquisition of sexually transmitted infections in adolescents attending an urban, general HMO teen clinic. J Adolesc Health. 2006;39:287–290. doi: 10.1016/j.jadohealth.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Hutton HE, McCaul ME, Santora PB, et al. The relationship between recent alcohol use and sexual behaviors: Gender differences among sexually transmitted disease clinic patients. Alcohol Clin Exp Res. 2008;32:2008–2015. doi: 10.1111/j.1530-0277.2008.00788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cook RL, Comer DM, Wiesenfeld HC, et al. Alcohol and drug use and related disorders: An underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33:565–570. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- 6.Tapert SF, Aarons GA, Sedlar GR, et al. Adolescent substance use and sexual risk-taking behavior. J Adolesc Health. 2001;28:181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- 7.Cook RL, Pollock NK, Rao AK, et al. Increased prevalence of herpes simplex virus type 2 among adolescent women with alcohol use disorders. J Adolesc Health. 2002;30:169–174. doi: 10.1016/s1054-139x(01)00339-1. [DOI] [PubMed] [Google Scholar]
- 8.Crosby RA, Diclemente RJ, Wingood GM, et al. Co-occurrence of intoxication during sex and sexually transmissible infections among young African American women: Does partner intoxication matter? Sex Health. 2008;5:285–289. doi: 10.1071/sh07098. [DOI] [PubMed] [Google Scholar]
- 9.Staras SA, Cook RL, Clark DB. Sexual partner characteristics and sexually transmitted diseases among adolescents and young adults. Sex Transm Dis. 2009;36:232–238. doi: 10.1097/OLQ.0b013e3181901e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doherty IA, Adimora AA, Schoenbach VJ, et al. Correlates of gonorrhoea among African Americans in North Carolina. Int J STD AIDS. 2007;18:114–117. doi: 10.1258/095646207779949691. [DOI] [PubMed] [Google Scholar]
- 11.Bailey SL, Gao W, Clark DB. Diary study of substance use and unsafe sex among adolescents with substance use disorders. J Adolesc Health. 2006;38:297.e213–297.e220. doi: 10.1016/j.jadohealth.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Levy S, Sherritt L, Gabrielli J, et al. Screening adolescents for substance use-related high-risk sexual behaviors. J Adolesc Health. 2009;45:473–477. doi: 10.1016/j.jadohealth.2009.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Am Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 14.Begley E, Crosby RA, DiClemente RJ, et al. Older partners and STD prevalence among pregnant African American teens. Sex Transm Dis. 2003;30:211–213. doi: 10.1097/00007435-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Ellen JM, Brown BA, Chung SE, et al. Impact of sexual networks on risk for gonorrhea and chlamydia among low-income urban African American adolescents. J Pediatr. 2005;146:518–522. doi: 10.1016/j.jpeds.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 16.Auerswald CL, Muth SQ, Brown B, et al. Does partner selection contribute to sex differences in sexually transmitted infection rates among African American adolescents in San Francisco? Sex Transm Dis. 2006;33:480–484. doi: 10.1097/01.olq.0000204549.79603.d6. [DOI] [PubMed] [Google Scholar]
- 17.Barry PM, Kent CK, Klausner JD. Risk factors for gonorrhea among heterosexuals—San Francisco, 2006. Sex Transm Dis. 2009;36(suppl 2):S62–S66. doi: 10.1097/OLQ.0b013e31815faab8. [DOI] [PubMed] [Google Scholar]
- 18.Valera P, Epperson M, Daniels J, et al. Substance use and HIV-risk behaviors among young men involved in the criminal justice system. Am J Drug Alcohol Abuse. 2009;35:43–47. doi: 10.1080/00952990802342923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Looby A, Earleywine M. Negative consequences associated with dependence in daily cannabis users. Subst Abuse Treat Prev Policy. 2007;2:3. doi: 10.1186/1747-597X-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rice RE, Donohew L, Clayton R. Peer network, sensation seeking, and drug use among junior high and senior high students. Connections. 2003;25:5–19. [Google Scholar]
- 21.Iannotti RJ, Bush PJ. Perceived vs actual friends use of alcohol, cigarettes, marijuana, and cocaine - which has the most influence. J Youth Adolesc. 1992;21:375–389. doi: 10.1007/BF01537024. [DOI] [PubMed] [Google Scholar]
- 22.Mercer CH, Copas AJ, Sonnenberg P, et al. Who has sex with whom? Characteristics of heterosexual partnerships reported in a national probability survey and implications for STI risk. Int J Epidemiol. 2009;38:206–214. doi: 10.1093/ije/dyn216. [DOI] [PubMed] [Google Scholar]
- 23.Mercer CH, Wellings K, Macdowall W, et al. First sexual partnerships—age differences and their significance: Empirical evidence from the 2000 British National Survey of Sexual Attitudes and Lifestyles (‘Natsal 2000’) J Adolesc Health. 2006;39:87–95. doi: 10.1016/j.jadohealth.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Ford K, Sohn W, Lepkowski J. Characteristics of adolescents' sexual partners and their association with use of condoms and other contraceptive methods. Fam Plann Perspect. 2001;33:100–105. 132. [PubMed] [Google Scholar]
- 25.Hallfors DD, Iritani BJ, Miller WC, et al. Sexual and drug behavior patterns and HIV and STD racial disparities: The need for new directions. Am J Public Health. 2007;97:125–132. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaestle CE, Halpern CT, Miller WC, et al. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. Am J Epidemiol. 2005;161:774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- 27.Corcoran C, Mehta C, Patel N, et al. Computational tools for exact conditional logistic regression. Stat Med. 2001;20:2723–2739. doi: 10.1002/sim.739. [DOI] [PubMed] [Google Scholar]
- 28.Mehta CR, Patel NR, Senchaudhuri P. Efficient Monte Carlo methods for conditional logistic regression. J Am Statistical Assoc. 2000;95:99–108. [Google Scholar]
- 29.Ditlevsen S, Christensen U, Lynch J, et al. The mediation proportion: A structural equation approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology. 2005;16:114–120. doi: 10.1097/01.ede.0000147107.76079.07. [DOI] [PubMed] [Google Scholar]
- 30.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1982. [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use & Health: National findings. Rockville, MD: US Department of Health and Human Services; 2009. [Google Scholar]
- 32.Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addict Behav. 2007;32:2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldstein AL, Barnett NP, Pedlow CT, et al. Drinking in conjunction with sexual experiences among at-risk college student drinkers. J Stud Alcohol Drugs. 2007;68:697–705. doi: 10.15288/jsad.2007.68.697. [DOI] [PubMed] [Google Scholar]
- 34.Lee JK, Jennings JM, Ellen JM. Discordant sexual partnering: A study of high-risk adolescents in San Francisco. Sex Transm Dis. 2003;30:234–240. doi: 10.1097/00007435-200303000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Barta WD, Portnoy DB, Kiene SM, et al. A daily process investigation of alcohol-involved sexual risk behavior among economically disadvantaged problem drinkers living with HIV/AIDS. AIDS Behav. 2008;12:729–740. doi: 10.1007/s10461-007-9342-4. [DOI] [PubMed] [Google Scholar]
- 36.Kiene SM, Barta WD, Tennen H, et al. Alcohol, helping young adults to have unprotected sex with casual partners: Findings from a daily diary study of alcohol use and sexual behavior. J Adolesc Health. 2009;44:73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anderson BJ, Stein MD. A behavioral decision model testing the association of marijuana use and sexual risk in young adult women. [Accessed September 30, 2010];AIDS Behav. 2010 doi: 10.1007/s10461-010-9694-z. In press. Available at: http://www.springerlink.com/content/988m24p5180k82km/fulltext.pdf. [DOI] [PMC free article] [PubMed]
- 38.Stoner BP, Whittington WL, Aral SO, et al. Avoiding risky sex partners: Perception of partners' risks v partners' self reported risks. Sex Transm Infect. 2003;79:197–201. doi: 10.1136/sti.79.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lenoir CD, Adler NE, Borzekowski DL, et al. What you don't know can hurt you: Perceptions of sex-partner concurrency and partner-reported behavior. J Adolesc Health. 2006;38:179–185. doi: 10.1016/j.jadohealth.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 40.Iritani BJ, Ford CA, Miller WC, et al. Comparison of self-reported and test-identified chlamydial infections among young adults in the United States of America. Sex Health. 2006;3:245–251. doi: 10.1071/sh06040. [DOI] [PubMed] [Google Scholar]