Abstract
Background
Acquired cholesteatomas are commonly seen in patients less than 30 years. There is a typical history of recurrent middle ear infections with tympanic membrane perforation. The diagnosis of cholesteatoma is usually made on otologic examination.
Objective
The aim of the work was to study the role of high resolution computed tomography (HRCT) in detecting, evaluating, and diagnosing middle ear cholesteatoma.
Patients and methods
This was a prospective study that included 56 consecutive patients with chronic suppurative otitis media, unsafe type cholesteatomas. Each patient was subjected to full clinical evaluation, and HRCT examination. Intravenous contrast media was used in some patients with suspected intracranial complication. Preoperative radiological data were correlated with data related to surgical findings.
Results
The study showed that a high incidence of cholesteatoma in the third decade of life. The scutum and lateral attic wall were the most common bony erosions in the middle ear bony wall (64.3%), and the incus was the most eroded ossicle in the middle ear (88.2%). Sclerosing of mastoid air cells were encountered in 60.7% of patients and the lateral semicircular canal was affected in 9%, while facial canal erosion was found in 21.4%. Temporal bone complications are more common than intracranial complications.
HRCT findings were compared with operative features; the comparative study included the accuracy and sensitivity of HRCT in detecting cholesteatoma (92.8%), its location and extension (96.4%), ossicular chain erosion (98%), labyrinthine fistula and intracranial complications (100%).
Conclusion
The important role of HRCT scannig lies on the early detection of cholesteatoma, and more conservative surgical procedures can be used to eradicate the disease.
Keywords: cholesteatoma, high resolution computed tomography
Introduction
Otitis media remains a significant international health problem in terms of prevalence, economics, and sequelae. Chronic suppurative otitis media is divided into two main clinical types: chronic suppurative otitis media without cholesteatoma that is recognized clinically as safe type, and chronic suppurative otitis media with cholesteatoma, or unsafe type.1
Cholesteatoma is a cystic lesion composed of epithelium and stroma surrounded by inflammatory reaction.2
The ability of high resolution computed tomoghraphy (HRCT) to predict accurately the status of the structures of the temporal bone represents a major advance in delineating pathology prior to surgical exploration of ears with cholesteatoma.3
A variety of standard surgical approaches is currently used to remove cholesteatomas. All of these procedures can be categorized as either intact canal wall or canal wall down approaches.4
The aim of this work is to study the role, value, and impact of HRCT in detection, evaluation, and diagnosis of middle ear cholesteatoma.
Patients and Methods
The study was approved by the research ethics committee of the Faculty of Medicine, Minia University. All patients gave their written, informed consent to participate in the study.
The study includes 56 consecutive patients who presented to the department of ear nose and throat (ENT) at Minia University Hospital from Septemper, 15th, 2009 through February, 28th, 2010. Twenty six patients were male and 30 were female; their ages ranged from 9 to 65 years old with mean age of 25.6. All patients were diagnosed clinically as chronic suppurative otitis media with acquired cholesteatoma and presented with chronic scanty ear discharge, which is offensive, marginal tympanic membrane perforation, and conductive hearing loss. Some patients presented with signs of cranial and/or intracranial complications.
Clinical history was taken for every patient, and all were given a full ear, nose, and throat (ENT) examination with careful otoscopic and micoscopic ear examination. In addition, a full audiological evaluation was done in the form of pure tone audiometry, tymanometry, speech discrimination score, and stapedial reflex.
Exclusion criteria were previous ear surgery, previous head trauma, and known history of sensory neural hearing loss.
Radiological evaluation was done using HRCT for all patients using GE CT/PROSPEED plus Ver 0.04 scanner with 512 elements. Zooming and magnification were done for the petrous bone on each side. Contrast enhancement was done for patients with suspected intracranial complications. The hallmarks of the cholesteatoma on CT scan are based on the presence of one or more of the following: (1) nondependent soft tissue density mass associated with attic, mesotympanum or antrum, (2) typical location, and (3) bony erosion of the middle ear bony walls (ie, scutum, attic wall, tympanic spine, tegmen, sigmoid sinus plate, Korner’s septum, posterior and superior metal wall) erosion of the ossicles, scalloping of the mastoid, or erosion of the semicircular canal and facial nerve canal.5
All patients were carefully prepared. Operative procedures performed were intact canal wall (ICD), canal wall down (CWD), or atticotomy. The type of surgical procedure depended on the site and extent of the lesion. Correlation between operative data and imaging studies was done.
Results
The results of our study showed that the highest incidence of cholesteatoma was in third decade while the lowest incidence was in the sixth decade. A higher proportion of patients were female (53.6%) than male (46.4%). Chronic ear discharge with hearing loss was the main clinical presentation (60.7%).
Type of cholesteatoma is presented in Table 1. Combined pars flaccida and pars tensa cholesteatoma were the most commonly encountered type, detected in 35.7% of patients. Also commonly detected was pars flaccida type.
Table 1.
Type of cholesteatomas.
| Type of cholesteatoma | No. of patients | % |
|---|---|---|
| Pars flaccida cholesteatoma | 20 | 35.71 |
| Pars tens cholesteatoma | 16 | 28.57 |
| Combined cholesteatoma | 20 | 35.71 |
Location and extent of cholesteatoma
Extensive holotympanic acquired cholesteatoma was the most common, found in 32.14% of patients, followed by attic cholesteatoma, found in 28.6% of patients. Table 2 shows the location of cholesteatoma.
Table 2.
Location and extant of cholesteatoma.
| Location and extension | No. of patients | % |
|---|---|---|
| Attic | 16 | 28.57 |
| Attico-antral | 12 | 21.42 |
| Mesotympanum | 10 | 17.85 |
| Extensive (holotympanic) extended to mastoid antrum | 18 | 32.14 |
| Total | 56 | 100 |
Bony erosion of the middle ear bony walls
The scutum and lateral attic wall erosion was the most common finding, encountered in 64.3% of patients, followed by eroded Korner’s septum, found in 64.2%. Table 3 shows the erosion in the middle ear cavity.
Table 3.
Middle ear bony wall erosion.
| Bony wall erosion | No. of patients | % |
|---|---|---|
| Blunted scutum | 10 | 17.85 |
| Eroded scutum and lateralattic wall | 36 | 64.28 |
| Eroded tegmen | 10 | 17.85 |
| Thinning of the tegmen | 20 | 35.71 |
| Eroded sigmoid sinus plate | 8 | 14.28 |
| Eroded superior and posterior meatal wall | 10 | 17.85 |
| Eroded Korner’s septum | 36 | 64.28 |
Integrity of the ossicular chain
The incus was the most commonly eroded, found in 88.2% of patients, followed by malleus, found in 67.9%. Table 4 reveals the integrity of ossicular chain.
Table 4.
Integrity of the ossicular chain.
| Integrity of the ossicles | No. of patients | % |
|---|---|---|
| Completely eroded (no ossicles) | 32 | 57.14 |
| Eroded malleus only | 6 | 10.71 |
| Eroded incus only | 16 | 28.57 |
| Displaced intact ossicles | 2 | 3.57 |
| Total | 56 | 100.0 |
Involvement of hidden area
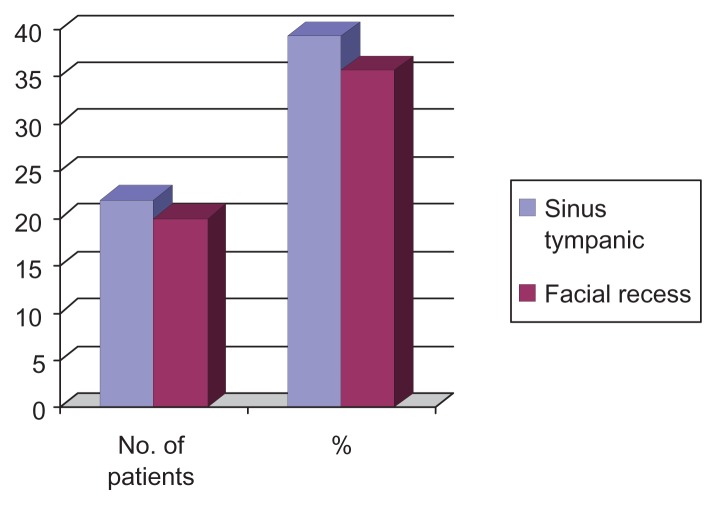
The hidden areas are sinus tympani and facial recess. Figure 1 shows the involvement of hidden areas.
Figure 1.
The involvement of hidden areas (sinus tympanic and facial recess).
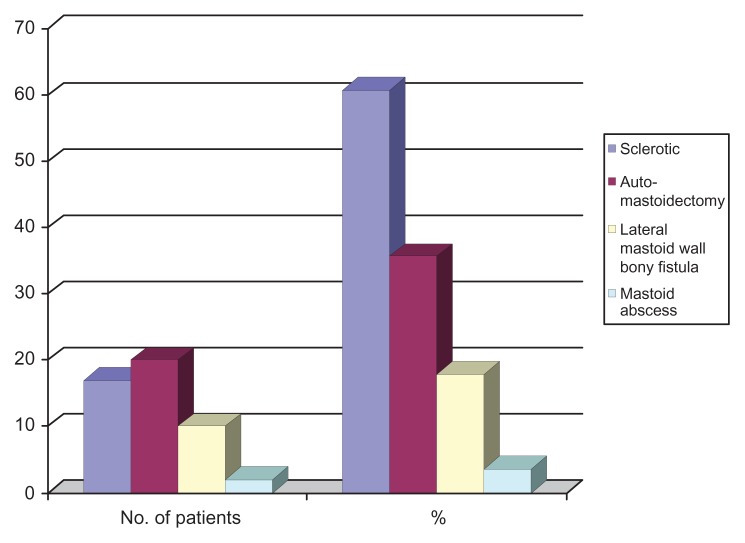
The state of mastoid air cells
Sclerotic mastoid was the most common finding encountered in 60.7%. Figure 2 shows the state of mastoid air cell.
Figure 2.
Integrity of mastoid air cell system.
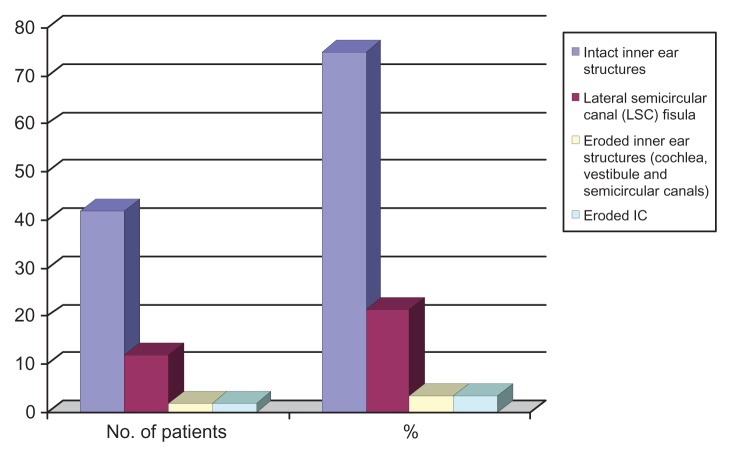
The labyrinth
The lateral semicircular canal fistula was the most common finding, encountered in 17.8% of patients. The condition of inner ear structures are presented in Figure 3.
Figure 3.
Integrity of the inner ear.
Integrity of facial nerve canal
Intact facial nerve canal was encountered in 71.4% of patients, and eroded in 21.4%. Table 5 shows the condition of facial nerve canal.
Table 5.
Integrity of the facial nerve canal.
| Facial nerve canal state | No. of patients | % |
|---|---|---|
| Intact | 40 | 71.42 |
| Dehiscent DNC | 4 | 7.14 |
| Eroded ENC | 12 | 21.42 |
| Proximal tympanic segment | 2 | 3.57 |
| Distal tympanic segment | 4 | 7.14 |
| All tympanic segment | 4 | 7.14 |
| Vertical segment | 2 | 3.57 |
| Total | 56 | 100.0 |
Condition of the other ear
The incidence of bilateral cholesteatoma was 3.57% in the studied sample. Table 6 shows the condition of the other ear.
Table 6.
The condition of the other ear.
| Other ear | No. of patients | % |
|---|---|---|
| Normal other ear | 40 | 71.42 |
| Diseased | 16 | 28.57 |
| Chronic suppurative otitis media | 14 | 25.0 |
| Cholesteatoma | 2 | 3.57 |
Complications of cholesteatoma
Cranial complications were more common than intracranial complications. Table 7 shows the percentage of each complication.
Table 7.
Temporal bone and intracranial complications of 56 patients with cholesteatoma.
| Complication | No. of patients | % |
|---|---|---|
| Temporal bone complications | ||
| Complete ssicular destruction | 32 | 57.14 |
| Automastoidectomy | 20 | 35.71 |
| Mastoid wall fistula | 10 | 17.85 |
| Conductive hearing loss | 30 | 53.75 |
| Total hearing loss | 2 | 3.57 |
| LSC fistula | 6 | 21.42 |
| Mastoid abscess | 2 | 3.57 |
| Post auricular and zygomatic abscess | 10 | 17.85 |
| Eroded sigmoid sinsus plate | 8 | 14.28 |
| Intracranial complications | ||
| Cerebellar abscess | 2 | 3.57 |
| Cerebral abscess | 2 | 3.57 |
| Extradural abscess | 2 | 3.57 |
| Otitic hydrocephalus | 2 | 3.57 |
The correlation between HRCT and operative features in the studied patients revealed that most radiological pathology correlated with the operative findings. Table 8 shows the correlation between CT findings and operative features. Figures 4–8 show the HRCT cholesteatoma in different parts of the middle ear cleft.
Table 8.
Correlation between CT findings and operative features of 56 patients with cholesteatoma.
| Features | Finding in CT | Operative features | False negative | False positive | Accuracy | Sensitivity | % |
|---|---|---|---|---|---|---|---|
| Tissue mass | 52 | 52 | 0 | 0 | 100 | 100 | 92.8 |
| Typical location | 54 | 54 | 0 | 0 | 100 | 100 | 96.4 |
| Bony erosions | 56 | 56 | 0 | 0 | 100 | 100 | 100 |
| Incus erosion | 48 | 50 | 2 | 0 | 96 | 96 | 85.71 |
| Malleus erosion | 38 | 38 | 0 | 0 | 100 | 100 | 67.86 |
| LSC fistula | 12 | 12 | 0 | 0 | 100 | 100 | 21.42 |
| Tegmen erosion | 10 | 8 | 0 | 2 | 94.4 | 100 | 17.85 |
| Facial canal | |||||||
| Intact | 42 | 42 | 0 | 0 | 100 | 100 | 75 |
| Eroded | 10 | 12 | 2 | 0 | 96.4 | 83.3 | 17.8 |
| Dehiscent | 4 | 4 | 0 | 0 | 100 | 100 | 7.14 |
| Eroded SSP | 8 | 8 | 0 | 0 | 100 | 100 | 14.28 |
| Eroded Ks | 36 | 36 | 0 | 0 | 100 | 100 | 64.28 |
| Intracranial complications | 8 | 8 | 0 | 0 | 100 | 100 | 14.28 |
Abbreviations: SSP, Sigmoid sinus plate; KS, Korner’s septum.
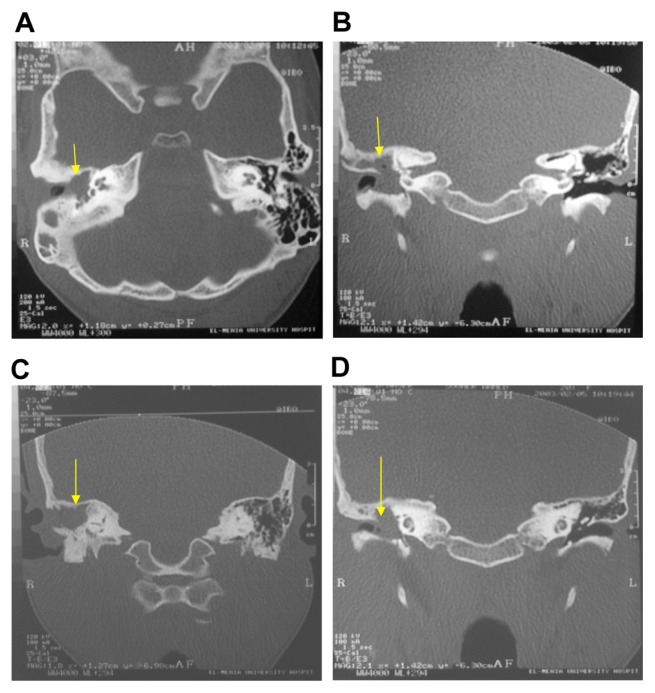
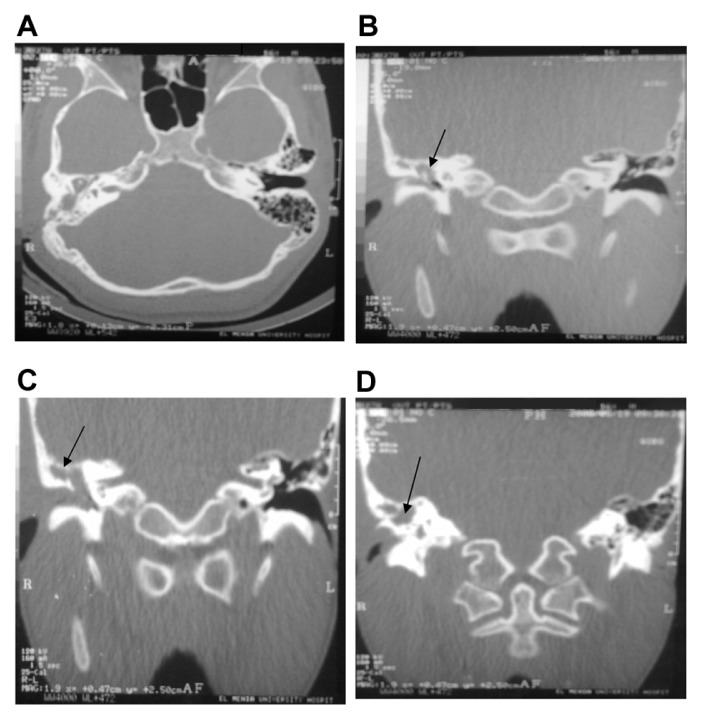
Figure 4.
High Resolution CT examination of the petrous bone. (A) Axial and (B–D) Coronal reveled evidence of abnormal soft tissue density completely opacified the right tympanic cavity.
Notes: It erodes the scutum, and lateral epitympanic wall, destruct the ossicular chain. The lesion is connected with the mastoid antrum. The tympanic segment of the facial nerve canal is eroded. (right epitympanic and antrum cholesteatoma).
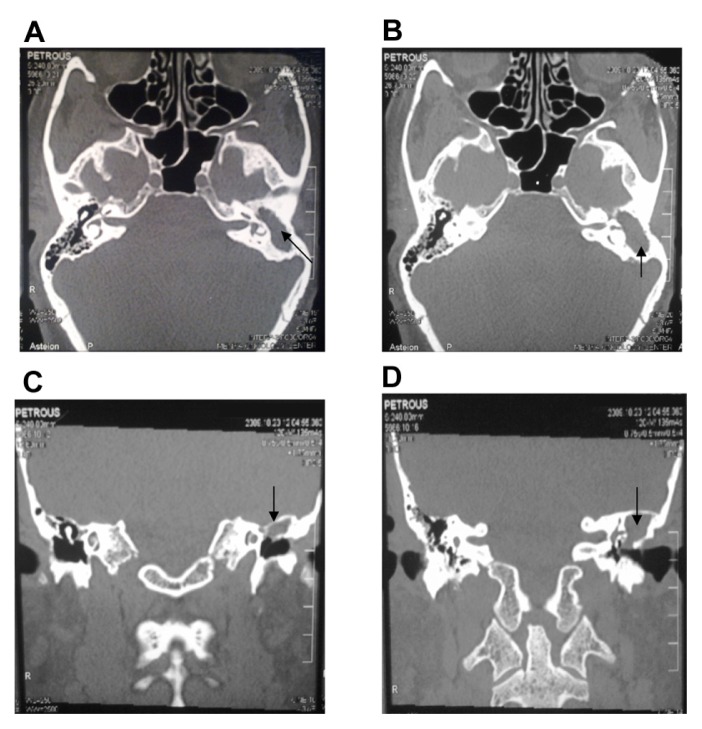
Figure 8.
Left extensive cholesteatoma. High resolution CT. (A and B) Axial and (C and D) Coronal cuts showing a well defined radical cavity involving the left mastoid, connected with the antrum with marked expansion of the aditus ad antrum, mastoid antrum and epitympanic cavity.
Notes: This is associated with complete destruction of the left middle ear cavity including the ossicular chain, thinning out of tegmen tympani with bony defect through the postero-lateral mastoid wall. The anterior limb of the left lateral semicircular canal is eroded.
Discussion
HRCT is most valuable for detection of early erosive changes in the ossicles, particularly in the smaller parts, as well as in the detection of non-dependent soft tissue opacification suggestive of cholesteatoma, is usually made on otologic examination.6
Our prospective study was composed of 26 males and 30 females, diagnosed as acquired cholesteatoma with ages ranging from 9 years to 65 years. The highest incidence of cholesteatoma was in the third decade while the lowest incidence was in sixth decade.
It is stated that acquired cholesteatoma is inflammatory lesion that may occur at any age but are more commonly seen in patients less than 30 years of age. There is typically a history of recurrent middle ear infections, with tympanic membrane perforation.7 A study done by Kemppainen et al, showed that the incidence of cholesteatoma was higher among males under the age of 50 years.8 In this study, recurrent attacks of otitis media were present in 72.4% of cholesteatoma patients.
Our study showed that conductive hearing loss was present in 34 patients (60.71%); otorrhea was a constant in 10 patients (17.85%); other clinical features such as signs of increased intracranial tension were present in 8 patients (14.28%); facial paresis, in 2 patients (3.57%); vertigo; and sensory neural hearing loss, in 2 patients (3.57%) each these clinical features are coincident with the presentation described in the literature by Seiden et al and Balleneger who reported that ear discharge and hearing loss are the main symptoms of patients with cholesteatoma; hearing loss varies from trivial to severe.1,9
Cholesteatoma can be accurately diagnosed by HRCT scan. Mafee et al reported in his series of 48 patients with cholesteatoma that 46 of them (96%) were diagnosed correctly using preoperative HRCT scans.10
One of the important advantages of the HRCT scan is the detection of early cholesteatoma with subtle bony erosion or ossicular displacement. This early detection by HRCT scan with the use of a simple noninvasive surgical technique (atticotomy) will solve the problem and preserve hearing.
In the current study, small attic and mesotympanic cholesteatoma was detected in 12 patients. Early Prussak’s space cholesteatoma was detected in 4 patients as a localized small soft tissue density mass slightly eroding the scutum and displacing the ossicles medially.
Mafee et al10 and David et al11 described the criteria indicating cholesteatoma as “blunting of the scutum’s normally sharp tip is often the earliest sign of attic cholesteatoma.”10,11
Joselitol et al stated that signs indicating cholesteatoma in the attic include erosion or destruction of scutum and widening of the aditus and antrum with loss of the “Figure 8” appearance.12
In the present study, HRCT scans demonstrate the involvement of posterior tympanic recesses (sinus tympani and facial recess) by cholesteatoma masses. In 22 patients of 56 patients (39.3%). The anterior tympanum was involved in 12 patients (21.4%). This is consistent with Hasso et al and Mafee et al, who mentioned that HRCT could demonstrate cholesteatoma in hidden areas such as post tympanic recesses, which could not be detected by the otologic examination.10,13
Ossicular chain erosion occurred in 57% of patients. The literature presents similar results, with sensitivity ranging from 80% to 100%.14
Our study showed that that 17.8% of patients had labrynthine fistula, which agrees with the results of Palva, who concluded that the labyrinthine fistula may occur in 10% of patients with chronic ear infection due to cholesteatoma.15
Our study showed that the incidence of intracranial complication is 14.3%. In the present study, complications were encountered in 8 patients in the form of cerebeller abscess, cerebral abscess, extradural abscess, and otitic hydrocephalus.
The patients presented with the general ill conditions headache and fever. A neurosurgeon was consulted for operative interference. Graziela et al concluded in their study that brain abscess is the most common intracranial complication and mostly affects the temporal lobe and cerebellum.16 El-Essawy et al17 in a series of 32 cases concluded that temporal bone complications including bone erosion and cavity formation were seen in all patients with cholesteatoma (100%) and sclerosis of the mastoid and ossicular destruction were seen in 93.81% of patients. Intracranial complications presented in 21.7%.17
Our study showed that all patients with cholesteatoma had at least one of the HRCT criteria indicating cholesteatoma, and 54 (92.8%) patients showed all 3 features of radiological findings of cholesteatoma. Fifty-four patients were accurately diagnosed with HRCT scans that correlated with surgical findings. This coincides with Mafee et al who repoted in their series of 48 patients with cholesteatoma that 46 of them (96%) had been diagnosed correctly with preoperative HRCT.10
Chee et al concluded in their series of 36 patients that 34 patients (94.4%) had been correctly diagnosed by HRCT.4
Joselito et al reported in their series of 64 patients that the analysis of the preoperative HRCT scan correlated with the surgical findings and histopathologic reports with a high degree of accuracy (96.8%).12
Hassman et al in a series of 60 patients reported that there is good correlation between HRCT findings and operative features in cholesteatoma for most middle ear structures.18
In a study done by Joselito et al in a series of 64 patients there were 4 cases (6.3%) that had labyrinthin fistula found on HRCT, but only 3 (4.7%) were in agreement with surgical findings.12
Anelise et al stated that the lateral semicircular canal erosion was present in 2 cases and was correctly identified by preoperative HRCT.19 Chee et al in their series concluded that 5 cases out of 6 lateral semicircular canal fistula were detected by preoperative HRCT.4
Stephenson et al stated that preoperative HRCT scanning is very precise in diagnosing labyrinthine fistula (100% sensitivity), and its radiologic size helps to predict the type of the fistula.20
Our results are in agreement with Joselito et al,12 Anelise et al,19 Chee et al,3 and Stephenson et al,20 in that the sensitivity of HRCT to detected labrynthine fistula was 100%.
The present study revealed that of 12 patients with surgically confirmed facial canal erosion, only 10 patients were detected by HRCT with accuracy (96.4%) and sensitivity (83.3%).
Joselito et al stated that preoperative demonstration of facial nerve canal involvement was often difficult not only because of the small size of the facial nerve canal but also due to its oblique orientation and the presence of developmental dehiscence, particularly when abutted by the soft tissue.12 Our results are supported by the findings of Sethom et al, who stated that HRCT scan analysis of middle ear bone structures shows satisfaction with 83% of sensibility and concluded that preoperative computed tomography is necessary for the diagnosis and the evaluation of chronic middle ear cholesteatoma in order to show extending lesions and to detect complications. This HRCT analysis and surgical correlation have showed that sensibility, specificity, and predictive value of HRCT scans depend on the anatomic structure implicated in cholesteatoma damages.21
Conclusions
From the study results we conclude that:
Patients with cholesteatoma should be scanned in both axial and coronal planes as many relevant structures are best seen in only one of these planes. The use of single plane may lead to mistakes because the structures parallel to the plane of section are not visualized.
HRCT scanning is a unique method of detection of early cholesteatoma as well as detection of cholesteatoma in hidden areas. In addition, HRCT scanning serves as a road map to assist the surgeon during cholesteatoma surgery.
With the more prevalent use of HRCT scanning, considerable morbidity may be avoided. Because of the ability to see middle ear structures with great clarity, more limited and more directed procedures can be done to eradicate disease while preserving function.
Recommendation
We recommend that the study should be done on large number of patients as well as at multiple centers.
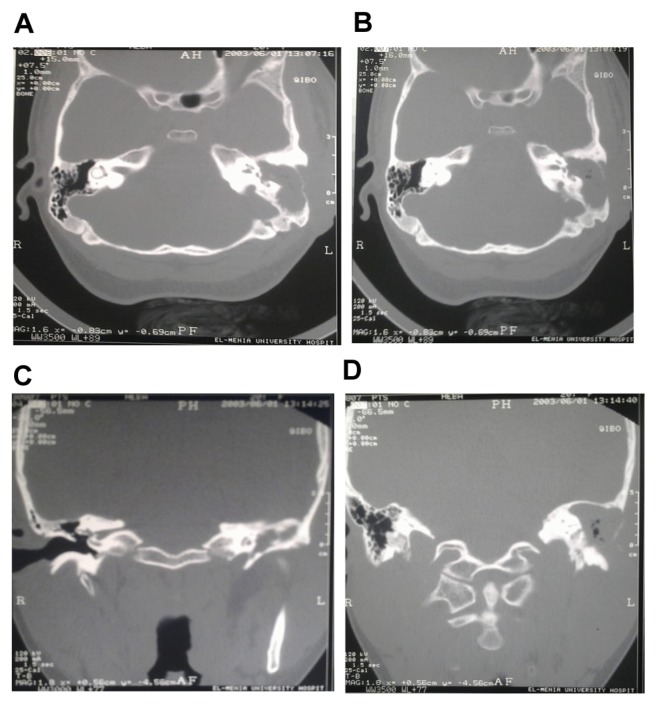
Figure 5.
Left attico-antral cholesteatoma. High resolution CT examination of the petrous bone. (A–C) Coronal section anterior tympanic level. (B) Axial midtympanic level reveled evidence of abnormal soft tissue density involve the left middle ear cavity.
Notes: The lesion involve the attic and extend to the mesotympanum. The bony ossicles show erosion of incus body. Near complete sclerosis of left mastoid air cells. No intracranial extension.
Figure 6.
Left attico antral cholesteatoma. High Resolution CT examination of the petrous bone. (A and B) Axial sections. (C and D) Coronal sections reveled evidence of abnormal soft tissue density involve the left middle ear cavity.
Notes: The lesion extend through the attic with widening of its opening and thinning of the roof of the left middle ear cavity. The bony ossicles are not visualized. near complete sclerosis of the left mastoid air cells.
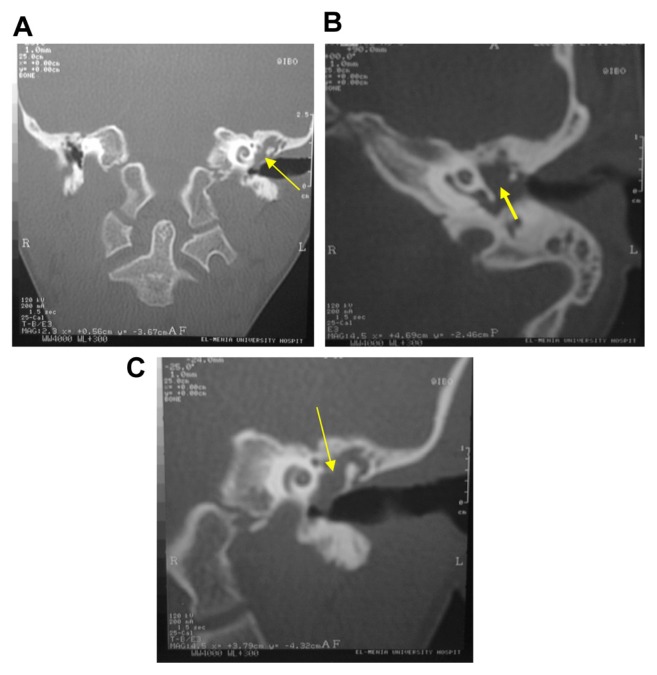
Figure 7.
High resolution CT examination of petrous bone. (A) Axial and (B–D) Coronal cuts reveled completely opacified right middle ear cavity and right mastoid antrum with bony erosion of antero-lateral wall of antrum as well as the incus, intact malleus head and neck.
Note: Associated with opacified right mastoid air cells with variable sized pockets (cavities) the largest seen at the mastoid tip …. abscess.
Footnotes
Author Contributions
Clinically diagnosed the cases: MAG. Radiologically evaluated the patients: HSAG. Conceived and designed the experiments and analyzed the data: AAS. Designed the experiments and operative interference: ARK. Jointly developed the structure and arguments for the paper: AAE. Contributed to the writing and editing of the manuscript: MAG. All authors reviewed and approved of the final manuscript.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
Funding
Author(s) disclose no funding sources.
References
- 1.Seiden AM, Tami TA, Penssak ML, Cotton RT, Gluckman JL. Otorhinolaryngology, The Essentials. New York, NY: Thieme; 2002. pp. 44–58. [Google Scholar]
- 2.Semaan MT, Megerian CA. The pathophysiology of cholesteatoma. Otolaryngol Clinic North Am. 2006;39(6):1143–59. doi: 10.1016/j.otc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Chee NC, Tan TY. The value of preoperative high resolution CT scans in cholesteatoma surgery. Singapore Med J. 2001;2/2(4):155–9. [PubMed] [Google Scholar]
- 4.Oiszewska E, Wagner M, Bernal-Sprekelsen M, et al. Etiopathogenisis of cholesteatoma. Eur Arch Otorhino Laryngol. 2004;261(1):6–24. doi: 10.1007/s00405-003-0623-x. [DOI] [PubMed] [Google Scholar]
- 5.Yates PD, Flood LM, Banerjee A, et al. CT scanning of middle ear cholesteatoma. What does the surgeon want to know? Br J Radiol. 2002;75:847–52. doi: 10.1259/bjr.75.898.750847. [DOI] [PubMed] [Google Scholar]
- 6.Mafee M, Kumar A, Yanniss D, et al. Computed tomography of the middle ear in the evaluation of cholesteatoma and other soft tissue mass; comparison with pleuri-direction tomography. Radiology. 1983;148:465–72. doi: 10.1148/radiology.148.2.6867344. [DOI] [PubMed] [Google Scholar]
- 7.White D. Aquired middle ear cholesteatoma complicated by ossicular erosion and SSC fistula. Presentation at: Wilford Hall medical center resources; 4/9/1997; brighamrad.harvard.edu/cases/mcr/hcache/259/full.html. [Google Scholar]
- 8.Kemppainen H, Puhakka J, Laippala J. Epidemiology and etiology of middle ear cholesteatoma. Acta Otolaryngol. 1999;119:568–72. doi: 10.1080/00016489950180801. [DOI] [PubMed] [Google Scholar]
- 9.Balleneger J. Diseases of the Nose, Throat, Ear, Head and Neck. 13th ed. Philadelphia, PA: Lea & Febiger; 1985. p. 1135. [Google Scholar]
- 10.Maffe M, Levin C, Appleboum I, Campos F. Cholesteatoma of the middle ear and mastoid. Otolaryngol Clin North Am. 1988;21:265–8. [PubMed] [Google Scholar]
- 11.David C, Lia D, Thomas R, Bergeron M. Contemporary radiologic imaging in the evaluation of middle ear-attic-antral complex cholesteatoma. Otolaryngol Clinic North Am. 1989;22:897–909. [PubMed] [Google Scholar]
- 12.Gurano JL, Joharjy IA. Middle ear cholesteatoma: characteristic CT findings in 64 patients. Ann Saudi Med. 2004;24(6):442–7. doi: 10.5144/0256-4947.2004.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hassco N, Bird R. Pathology of the temporal bone and mastoid. Chap. 5. Rave press; New York: 1988. pp. 1–45. [Google Scholar]
- 14.Banerjee A, Flood LM, Yates P, Clifford K. Computed tomography in suppurative ear disease: Dose it influence management. J Laryngol Otol. 2003;117(6):454–8. doi: 10.1258/002221503321892280. [DOI] [PubMed] [Google Scholar]
- 15.Palva T. The pathogenesis and treatment of cholesteatoma. Acta Otolaryngol. 1990;109:323–30. doi: 10.3109/00016489009125151. [DOI] [PubMed] [Google Scholar]
- 16.Martins G, Hausen-Pinna M, Tsuji RK, Neto R, Bento RF. Description of 34 patients with complicated cholesteatomatous chronic otitis media. Intl Arch Otorhinolaryngol, São Paulo. 2008;12(3):370–6. [Google Scholar]
- 17.El-Essawy S, El-Nahas M, El-Shewahy H, Ghoniem MR. Complicated middle ear cholesteatoma, a CT study. Egyptian Journal of Radiology and Nuclear Medicine. 1992;23(1):161–70. [Google Scholar]
- 18.Hassman-Poznanska E, Goscik E, Olenski J, Shotnika B. Computrized tomography in pre-oprative imaging of the middle ear cholesteatoma. Otorhinolaryngol Pol. 2003;57:243–9. [PubMed] [Google Scholar]
- 19.Prata A, Atunes ML, de Abreu EC, Carlos C, Frazatto R, Lima BT. Comparative study between radiological and surgical finding of chronic otitis media. Inter Arch Otorhinolaryngol. 2011;15:72–8. [Google Scholar]
- 20.Stephenson MF, Saliba I. Prognostic indicators of hearing after complete resection of cholesteatoma causing a labyrinthine fistula. Eur Arch Otorhinolaryngol. 2011;268(12):1705–11. doi: 10.1007/s00405-011-1545-7. [DOI] [PubMed] [Google Scholar]
- 21.Sethom A, Akkari K, Dridi I, et al. Preoperative CT Scan in middle ear cholesteatoma. Tunis Med. 2011;89(3):248–53. [PubMed] [Google Scholar]