Abstract
Background and Objectives
Mismatch negativity (MMN) is an event-related potential (ERP) measure of preattentional sensory processing. While deficits in the auditory MMN are robust electrophysiological findings in schizophrenia, little is known about visual mismatch response and its association with social cognitive functions such as emotion recognition in schizophrenia. Our aim was to study the potential deficit in the visual mismatch response to unexpected facial emotions in schizophrenia and its association with emotion recognition impairments, and to localize the sources of the mismatch signals.
Experimental Design
The sample comprised 24 patients with schizophrenia and 24 healthy control subjects. Controls were matched individually to patients by gender, age, and education. ERPs were recorded using a high-density 128-channel BioSemi amplifier. Mismatch responses to happy and fearful faces were determined in 2 time windows over six regions of interest (ROIs). Emotion recognition performance and its association with the mismatch response were also investigated.
Principal Observations
Mismatch signals to both emotional conditions were significantly attenuated in patients compared to controls in central and temporal ROIs. Controls recognized emotions significantly better than patients. The association between overall emotion recognition performance and mismatch response to the happy condition was significant in the 250–360 ms time window in the central ROI. The estimated sources of the mismatch responses for both emotional conditions were localized in frontal regions, where patients showed significantly lower activity.
Conclusions
Impaired generation of mismatch signals indicate insufficient automatic processing of emotions in patients with schizophrenia, which correlates strongly with decreased emotion recognition.
Introduction
Perception of emotional facial expressions has been shown to be closely related to psychosocial functioning and quality of life in schizophrenia [1]. An extensive body of research has accumulated suggesting a robust impairment in emotion recognition in schizophrenia, especially regarding facial emotion recognition [2].
While the behavioral indices of facial emotion recognition deficits in schizophrenia are robust, the underlying neurophysiological processes are still largely unknown. Although a large number of studies have investigated the electrophysiological correlates of conscious emotional face processing (see [3] for review), only a few studies investigated the automatic processing of unattended expressions, usually with healthy subjects [4], [5].
In the present study we investigated automatic change detection in facial expressions via the visual mismatch (vMM) component of the event-related potentials. vMM response is the visual counterpart of the auditory mismatch negativity (MMN: for review see [6]). The auditory MMN has been widely studied in schizophrenia, and reports usually indicate impaired automatic auditory processing [7]. Both the auditory MMN and vMM signals are typically elicited by stimuli with an infrequent (deviant) stimulus feature embedded in a stream of frequent (standard) stimuli. vMM response is elicited by deviant color [8], orientation [9], movement [10], spatial frequency [11], contrast [12], and even abstract sequential regularities of visual stimulation [13], see [14]–[16] for reviews). Mismatch responses are considered as automatic prediction error signals [17] representing the updating of generative models of environmental regularities after the violation of the model’s prediction by a deviant stimulus [18]. Urban et al found that deviant stimulus features (motion direction) elicited reduced vMM signal in schizophrenic patients [19].
The ERP paradigm applied in our study does not require overt responses to the face stimuli, allowing us to study the automatic processing of facial emotions presented outside of the focus of visual attention. Regarding its ecological validity, in real-life situations our attention is mostly engaged by events appearing in the center of the visual field, while important events (such as emotionally relevant stimuli) may emerge at the periphery. Furthermore, behavioral priming studies confirmed that affective processing occurs outside of the focus of visual attention [20]–[22].
Several studies demonstrated that vMMN is elicited by simple deviant features (see Kimura et al. [5] for a review, and Maekawa et al. [23] for a clinically-focused review ). To date only a few studies investigated visual mismatch negativity in healthy subjects using abstract regularities [24] or complex natural visual stimuli such as emotional facial expressions [5], [25], or body parts [13]. A recent study by Kimura et al. [5] reported that occipital, temporal and frontal regions play a major role in the generation of the facial expression-related mismatch response. As Stefanics et al. [25] summarized, occipital and temporal visual areas together with frontal generators automatically represent regularities in the emotional content of unattended faces appearing outside of the focus of attention and store them as predictive memory representations. The biological significance of such representation might be orienting our attention to sudden changes in emotional expression of conspecifics in our environment, analogously to auditory MMN [26], and also maintaining a predictive model of the environment. Although the processing of unattended facial emotions is likely to play an important role in social interactions, to our knowledge no study so far investigated the neural correlates of these processes in patients with schizophrenia.
We studied the differences between patients and control subjects by comparing their vMM responses to unattended rare (deviant) facial emotions embedded in a stream of faces expressing frequent (standard) emotions. We hypothesized that the vMM signal might be a sensitive indicator of compromised automatic information processing of emotional expressions in schizophrenia. Emotion recognition performance was evaluated in a separate behavioral test. To establish an association between the automatic vMM response and emotion recognition performance, we studied the correlation between behavioral performance and mismatch signal amplitudes. Based on well-known deficits in emotion processing in schizophrenia [2] we expected lower emotion recognition performance in patients. In conjunction with this, we also expected a significantly decreased mismatch response to emotional facial stimuli in patients with schizophrenia compared to controls. Finally, we hypothesized that the neural generators of the vMM response are located in occipital-temporal and frontal-prefrontal areas [5], and that the activity of these regions is decreased in schizophrenia.
Materials and Methods
Ethics Statement
The experiments were conducted in full compliance with the Helsinki Declaration and all relevant national and international ethical guidelines. The research was approved by the review board of the Semmelweis University, Budapest, Hungary. All procedures were carried after written informed consent was obtained from the participants. All potential participants who declined to participate or otherwise did not participate were not disadvantaged in any way by not participating in the study.
Subjects
Twenty-eight patients and twenty-eight healthy controls were recruited for the study. Data of four healthy controls and four patients were excluded from the final analysis because of low trial numbers due to artifacts (<50 artifact-free trials in the deviant conditions). The final sample comprised twenty-four patients with schizophrenia and twenty-four healthy controls. Healthy control participants were matched individually to schizophrenia patients by gender, age (+/−5 years), and years of education (+/−3 years), resulting in 24 matched pairs. All participants were right-handed with the exception of three left-handed patients and two left-handed healthy controls and had normal or corrected-to-normal vision. Participants did not receive payment for their participation. Data from the control group were published in part in Stefanics et al. [25].
Patients were recruited from the Department of Psychiatry and Psychotherapy of the Semmelweis University, Budapest, Hungary, from both the inpatient and outpatient units. Patients met the criteria for schizophrenia based on the Structured Clinical Interview for DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [27]) Axis I Disorders. A trained psychiatrist or psychologist evaluated psychiatric symptoms on the Positive and Negative Syndrome Scale (PANSS) [28]. At the time of testing all patients were on antipsychotic medication ( Table 1 ). To recruit a homogenous patient sample, besides outpatients, inpatients only before discharge were recruited into the study, which is reflected in the low overall PANSS scores ( Table 2 ).
Table 1. Antipsychotic medications.
| Antipsychotic Medication | Number of Patients (n) | Mean Daily Dose (SD) in milligrams |
| Amisulpride | 5 | 700 (264) |
| Aripiprazole | 3 | 20,0 (8.7) |
| Clozapine | 6 | 198 (129) |
| Haloperidol | 1 | 3,0 (0) |
| Olanzapine | 3 | 15 (5) |
| Quetiapine | 4 | 600 (294) |
| Risperidone | 9 | 5.2 (2.5) |
| Zuclopenthixol | 1 | 67,0 (0,0)* |
Weekly dose.
Table 2. Basic demographic and descriptive characteristics of the two study groups.
| Patients with | Healthy Control | |
| Schizophrenia (n = 24) | Subjects (n = 24) | |
| Gender (Male/Female) | 13/11 | 13/11 |
| Age (years) | 34.2 (10.3) | 33.2 (9.8) |
| Education (years) | 13.9 (10.1) | 15.0 (2.6) |
| Handedness (right/left) | 21/3 | 22/2 |
| Symptom Checklist 90 (Global Severity Index) | 98.6 (66.6) | 22.9 (23.5) |
| Schizophrenia Subtypes: Paranoid/Catatonic/Disorganized/Undifferentiated | 13/2/6/3 | N/A |
| Inpatients/Outpatients | 9/15 | N/A |
| Duration of illness (years) | 9.7 (7) | N/A |
| PANSS total | 59.4 (21.6) | N/A |
| PANSS positive | 14.5 (6.0) | N/A |
| PANSS negative | 15.1 (7.5) | N/A |
| Antipsychotic medication (Atypical/Typical) | 23/1 | N/A |
| Chlorpromazine equivalent (mg) | 601.9 (445.5) | N/A |
Patients and controls were excluded if they had any other DSM-IV Axis I disorder, any central nervous system disease, mental retardation, history of head injury with loss of consciousness for more than 1 h, and alcohol or drug abuse. In case of controls, a short interview was performed by a trained physician for screening. According to the Derogatis criteria for ‘caseness’ (i.e.: high risk for a psychiatric disorder), a global severity index of >114 on the SCL-90 was an additional exclusion criteria for controls [29]. (114 was the T score of 63 on a Hungarian population sample [30]). No subjects from the Stefanics et al. 2012 investigation [25] were excluded from the control group based on these criteria.
The following clinical and emotion recognition measures were obtained from all participants before EEG recordings: the SCL-90, a 90-item Symptom Checklist assessing general dimensions of psychopathology, and the Ekman-60 Test (Facial Expressions of Emotion – Stimuli and Tests, FEEST) [31], a computerized emotion recognition test of 60 trials, where participants have to indicate what facial expression from the six basic emotions they think is displayed in the face by using the computer’s mouse to point and click on the appropriate emotion label on the screen.
Demographic information for both groups and clinical characteristics of the schizophrenia group are presented in Table 2 .
Stimuli and Procedure
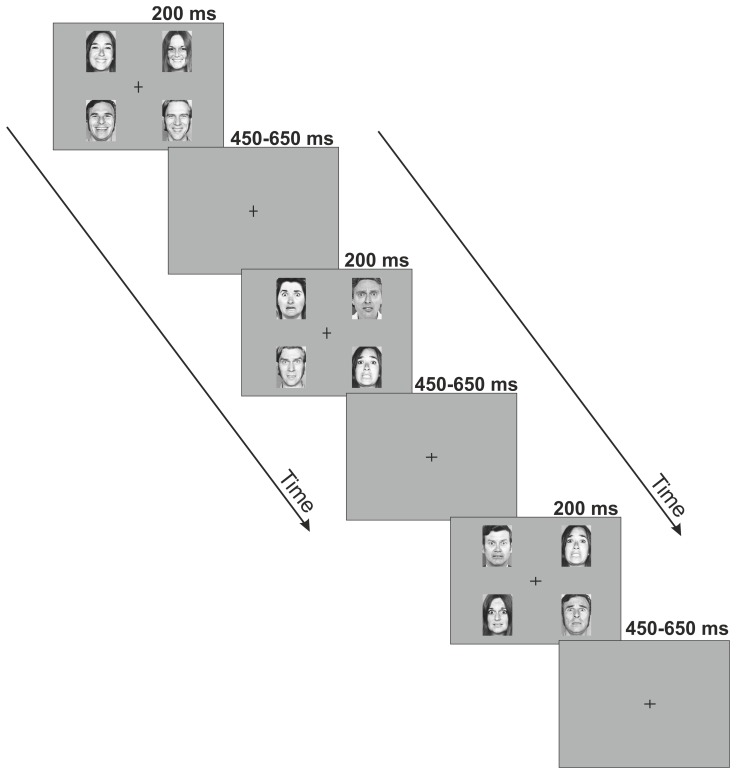
Visual stimuli were presented on a computer monitor. Stimulus presentation was designed in a manner to facilitate the forming of memory traces to emotions rather than to individual faces. To this end, black and white photographs of 5 female and 5 male faces were used as stimuli, taken from the Pictures of Facial Affect set [31] which is a standard set of stimuli in the field of facial emotion research, and has been used in many studies in the past decades. On each screen, 4 images of faces expressing the same emotion, specifically, images of 2 males and 2 females expressing the same facial emotion were presented in the upper-left, upper-right, lower-left and lower-right quadrants of the monitor. There are two advantages of this stimulus arrangement. First, faces presented outside the center of the visual field enable studying mismatch responses to deviants without attentional confounds. Second, using four different faces on each stimulus panel likely prevents local adaptation effects to contribute to possible deviance effects. In the center of the monitor a black fixation cross was presented. Pictures appeared on a dark-grey background at a viewing distance of 0.5 m. Figure 1 illustrates the stimuli used in the experiment. Each face was subtended by 5.6° visual angle horizontally and 7.7° vertically. The distance of the inner corner of the pictures from the fixation cross was 4.4 visual angle horizontally and 3.8 visual angle vertically The presentation order of the individual pictures was randomized with the restriction that a picture of the same person was not presented on subsequent stimulus displays. Stimulus duration was 200 ms. The stimulus onset asynchrony (SOA) was randomized between 650–850 ms. In two experimental blocks fearful facial emotions were presented as frequent standards and happy facial emotions were presented as rare deviants (standard P = 0.9, deviant P = 0.1). In the remaining two blocks the standard and deviant emotions were swapped. The order of the four blocks was randomized across participants. A total of 100 deviant and 900 standard stimuli were presented for each emotion. The task of the subjects was a feature detection task entirely unrelated to the change in the facial expressions: they had to respond with a speeded button-press to the unpredictable changes in the length of either the horizontal or vertical lines of a black fixation cross presented in the center of the visual field. From time to time, the cross became either wider or longer, with a mean frequency of 11 changes per minute (SD = 3).
Figure 1. Stimuli and paradigm.
Schematic illustration of the pattern of emotional stimuli used in the experiment. Four individual photographs displaying the same facial affect were presented on each screen for 200-stimulus interval randomly varying between 450–650 ms during which occasionally the vertical and horizontal lines of the fixation cross changed. The subjects’ task was a speeded button-press to the changes of the cross.
EEG Recording and Preprocessing
EEG was recorded from DC with a low-pass filter at 100 Hz using a high-density 128-channel BioSemi ActiveTwo amplifier [32]. The electrode caps had an equidistant-layout and covered the whole head. EOG electrodes to monitor eye movements were placed below the left and above the right external canthi. Data were digitized at 24 bit resolution and a sampling rate of 512 Hz. Built-in and self-developed functions as well as the freeware EEGLAB toolbox [33] in the Matlab (MathWorks, Natick, MA) development environment were used for subsequent off-line data analyses. EEG was re-referenced to the common average potential and filtered off-line between 0.1 and 30 Hz using zero-phase shiftforward and reverse IIR Butterworth filter.
600 ms activity following the onset of the stimuli were extracted from the continuous EEG. The pre-stimulus period was 100 ms, which was used as baseline for the ERP generation. For both facial emotions, epochs were averaged separately for standards and deviants. Trials occurring within an 800 ms interval after a target event (i.e., change in the fixation cross) were automatically excluded from the analysis. To avoid potential artifacts, epochs with values exceeding ±120 µV on any EEG or EOG channel were rejected from the analysis. The mean number (and SD) of accepted trials for fearful and happy deviants and fearful and happy standards were 77 (8.4), 77 (6.9), 567 (62.3) and 561 (66.8) in the control group, and 75 (9.6), 86 (11.5), 533 (70.4) and 536 (70.8) in the schizophrenia group, respectively.
Data Analysis
Generation of difference waveforms
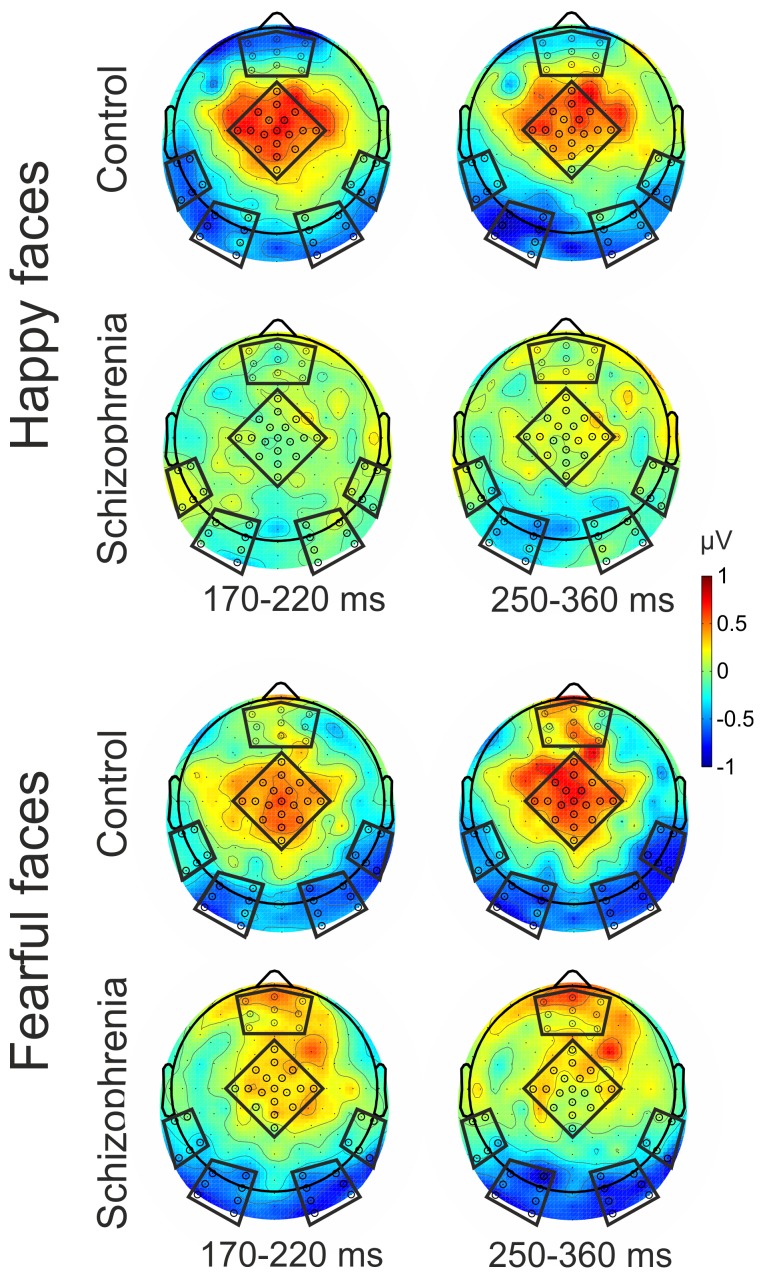
Difference waveforms (mismatch responses) were created by subtracting ERPs to standards from the ERPs to deviants, separately for the two emotions ( Figure 2 ). In half of the blocks the roles of deviants and standards were reversed, responses to standard fearful faces were subtracted from responses to deviant fearful faces, and responses to standard happy faces were subtracted from responses to deviant happy faces. The only difference between standard and deviant emotions was the frequency of presentation in the given block. Since exactly the same pictures were used as deviants and standards, responses to physically identical stimuli were subtracted to calculate mismatch responses. Six Regions of Interest (ROIs) were formed (pre-frontal, central, temporal left, temporal right, occipital left and occipital right) according to previous visual mismatch studies [25], [34] ( Figure 3 ). Mean ERP responses were calculated by averaging across electrodes within ROIs. (Electrode clusters selected for analyses are marked with black dots in black frames in Figure 3 ).
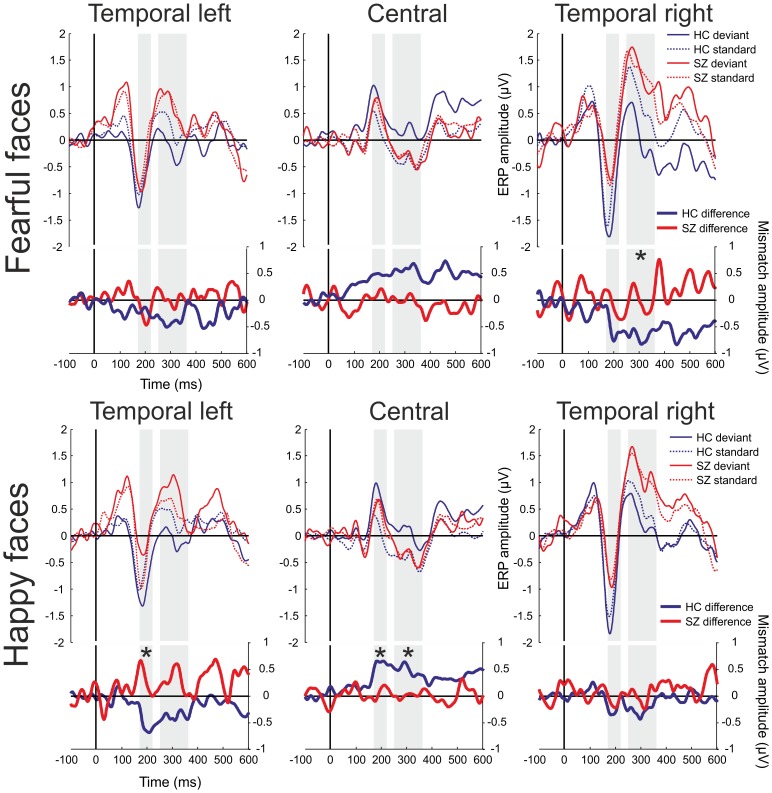
Figure 2. Event-related potentials and mismatch waveforms by region.
HC = Healthy Controls, SZ = Patients with Schizophrenia. Upper panel: ERPs for fearful faces; lower panel: ERPs for happy faces. Shaded intervals indicate time windows of amplitude measurements. Only those ROIs were used for between-group comparison where the mismatch waveform in at least one of the study groups differed significantly from zero after correction for multiple testing. Asterisks mark time windows where significantly larger mismatch responses were found in the healthy control group compared to the patients.
Figure 3. Scalp topography of the mismatch responses.
Electrode clusters selected for analyses are marked with black dots in black frames (Region of Interests: ROIs).
The pre-stimulus baseline periods were compared between study groups in all ROIs and did not differ significantly after Hochberg correction [35] for multiple comparisons (p>0.5).
Study group comparison
Time windows of 170–220 ms and 250–360 ms were selected for analyses based on results from the same control population [25]. These time windows correspond well to those used in similar paradigms [4], [5], [36]. The early (170–220 ms) time window is thought to reflect activity related to the processing of emotions by the fusiform gyrus and the superior temporal areas [36], whereas the mismatch response in the later time window (250–360 ms) is thought to correspond with frontal generators [5]. The mean of the difference waveforms were calculated within these intervals and served as dependent variables in the main analysis. Group differences were characterized by Cohen’s d. For Cohen’s d an effect size of 0.2 to 0.3 is considered as “small” effect, around 0.5 a “medium” effect and >0.8, a “large” effect [37]. Difference between study groups was investigated by ANOVA with mismatch response amplitude as dependent and study group as independent variable. Only those ROIs were used for comparison where the mismatch waveform in at least one of the study groups differed significantly (t-test, P<0.05) from zero after Hochberg correction for multiple testing [35] across all ROIs. In other words, those ROIs were selected for study group comparison where the deviant and the standard waveforms differed significantly (i.e: the difference waveform represents a statistically validated mismatch signal). The ANOVA was done separately for the two emotions and two time windows. The p-values for the between-group comparison were also corrected for multiple comparisons (Hochberg correction) in each time window separately.
The rationale of this analysis strategy was twofold. First, a between-group difference is hardly explicable if no mismatch signal was found in any of the study groups. Second, by decreasing the number of the between group comparisons we can reduce the likelihood of Type II errors which may occur due to the adjustment for multiple comparisons.
Correlation with behavioral indices
In addition to investigating group differences, we also examined whether difference waveforms in the aforespecified time windows and regions exhibited any significant association with behavioral indices. Due to the non-normal distribution of the behavioral variables, Spearman rank correlation was used for these calculations.
Source Localization
The source activations for different conditions were compared using standardized low-resolution brain electromagnetic tomography (sLORETA, [38]–[40]). This method computes the cortical three-dimensional distribution of current source density of scalp-recorded electroencephalography (EEG). It provides a standardized discrete, three-dimensional distributed, linear, minimum norm inverse solution to the inverse problem of location of cerebral sources. The method uses the MNI152 template [41], with the three-dimensional solution space restricted to cortical gray matter, as determined by the probabilistic Talairach atlas [42]. The intracerebral volume is segmented into 6239 voxels with a 5 mm spatial resolution. Accordingly, sLORETA images reflect the standardized electric activity at each voxel in neuroanatomic Montreal Neurological Institute (MNI) space as the exact magnitude of the estimated current density. It has been confirmed that this method achieves zero localization error in noise-free stimulations [38]. Brodmann areas are also reported using MNI space, with correction to Talairach space [43].
Results
Event-related potentials and difference potentials are shown in Figure 2 , while Figure 3 displays the scalp distributions of difference potentials. Deviant minus standard difference waveforms were negative in the occipital ( Figure 3 and Supporting Information: Figure S1) and temporal regions and positive in the central region ( Figures 2 – 3 ).
Behavioral Results
Reaction times and hit rates for the occasional changes in the fixation cross as well as false alarm rates were compared between study groups. A t-test of reaction times showed no significant differences between the blocks. Mean reaction times were 358 ms (SD = 117) for controls and 338 ms (SD = 160) for patients (t = 0.49, P = 0.62. Hit rate was above 94% for both study groups; nonetheless, controls (97.8% SD = 1.8) significantly outperformed patients (94.2% SD = 3.9) (Kruskal-Wallis Test: Chi2 = 8.5, P<0.005). False alarm rate was calculated as the ratio of button presses which were not preceded by a cross-flip in a 2000 ms interval before the event to the actual number of cross-flips. Mean false alarm rates were 1.1% (SD = 1.0) for controls and 2.5% (SD = 2.6) for patients respectively (Kruskal-Wallis Test: Chi2 = 4.1, P<0.05). High hit rates and low false alarm rates even in the patient group made it unlikely that patients failed to direct their attention to the task.
Mismatch Responses for Fearful Faces
In the control group a significant mismatch response was detected in the 250–360 ms time window over the left and right occipital and right temporal regions. No significant mismatch response was detected in the schizophrenia group in any of the ROIs for fear condition. Significant group difference (F(1,46) = 6.6, n = 48, P = 0.01) was found in the 250–360 ms time window over the right temporal region ( Table 3 ). This difference was 0.75 in terms of the effect size measure Cohen’s d (SD). The difference between study groups did not reach significance over the occipital regions (P>0.1).
Table 3. Between group differences in mismatch responses by region and emotion stimulus.
| Deviant vs. Standard | Between Group Difference in Mismatch Signal | ||||||
| Control Group | Schizophrenia Group | ||||||
| Condition | Time Window | Region of Interest (ROI) | LSMean(SE) | p value | LSMean(SE) | p value | Effect size (Cohen’s D) |
| 170–220 ms | Pre-Frontal | 0.10 (0.25) | – | 0.41 (0.25) | – | 0.26 | |
| Central | 0.48 (0.20) | 0.024 | 0.10 (0.20) | – | 0.38 | ||
| Temporal Left | −0.21 (0.15) | – | −0.28 (0.15) | 0.064 | 0.09 | ||
| Temporal Right | −0.54 (0.21) | 0.014 | −0.08 (0.21) | – | 0.45 | ||
| Occipital Left | −0.52 (0.24) | 0.035 | −0.54 (0.24) | 0.027 | 0.02 | ||
| Fear | Occipital Right | −0.55 (0.23) | 0.018 | −0.39 (0.23) | 0.087 | 0.15 | |
| 250–360 ms | Pre-Frontal | 0.25 (0.26) | – | 0.28 (0.26) | – | 0.02 | |
| Central | 0.57 (0.25) | 0.024 | −0.06 (0.25) | – | 0.53 | ||
| Temporal Left | −0.38 (0.20) | 0.056 | 0.01 (0.20) | – | 0.42 | ||
| Temporal Right | −0.67 (0.18) | <.001 * | −0.02 (0.18) | – | 0.75 a | ||
| Occipital Left | −0.61 (0.18) | 0.001 * | −0.41 (0.18) | 0.027 | 0.23 | ||
| Occipital Right | −0.60 (0.18) | 0.002 * | −0.43 (0.18) | 0.021 | 0.19 | ||
| 170–220 ms | Pre-Frontal | −0.31 (0.23) | – | 0.09 (0.23) | – | 0.36 | |
| Central | 0.61 (0.14) | <.001 * | 0.07 (0.14) | – | 0.81 a | ||
| Temporal Left | −0.57 (0.20) | 0.007 * | 0.32 (0.20) | – | 0.89 a | ||
| Temporal Right | −0.24 (0.20) | – | −0.12 (0.20) | – | 0.12 | ||
| Occipital Left | −0.51 (0.27) | 0.064 | −0.12 (0.27) | – | 0.30 | ||
| Happy | Occipital Right | −0.38 (0.27) | – | −0.20 (0.27) | – | 0.14 | |
| 250–360 ms | Pre-Frontal | −0.06 (0.21) | – | 0.19 (0.21) | – | 0.25 | |
| Central | 0.45 (0.13) | 0.002 * | 0.00 (0.13) | – | 0.68 a | ||
| Temporal Left | −0.38 (0.19) | 0.053 | 0.30 (0.19) | – | 0.73 | ||
| Temporal Right | −0.26 (0.19) | – | 0.01 (0.19) | – | 0.29 | ||
| Occipital Left | −0.70 (0.21) | 0.001 * | −0.18 (0.21) | – | 0.53 | ||
| Occipital Right | −0.43 (0.22) | 0.054 | −0.10 (0.22) | – | 0.31 | ||
p<0.05 significant difference in ERPs to deviant and standard stimuli (significant mismatch signal) after Hochberg correction for multiple comparisons.
p<0.05 significant difference in mismatch signal between groups.
Antipsychotic medication dose and symptom severity (PANSS total, positive and negative scores) did not correlate with the mismatch signals in these time windows over the above ROIs (P>0.5).
Mismatch Responses for Happy Faces
In the control group a significant mismatch signal was detected over the central and the left temporal region in the 170–220 ms time window, while no mismatch was detected in any of the ROIs in the schizophrenia group ( Table 3 ). A significantly larger mismatch response was observed in the control group compared to the patient group over the central (F(1;46) = 7.9, n = 48, P = 0.007) and the temporal left (F(1;46) = 9.1, n = 48, P = 0.003) regions. These difference were 0.81 and 0,89 SD respectively.
In the control group in the 250–360 ms time window a significant mismatch signal was detected over the central and occipital ROIs, and again, no significant mismatch was detected in the schizophrenia group in any of the ROIs ( Table 3 ). The difference between the groups was significant over the central region (F(1;46) = 5.5, n = 48, P = 0.02, Cohen’s D = 0.68).
Antipsychotic medication dose and symptom severity (PANSS total, positive and negative scores) did not affect the mismatch signals in these time windows over the above ROIs (P>0.1).
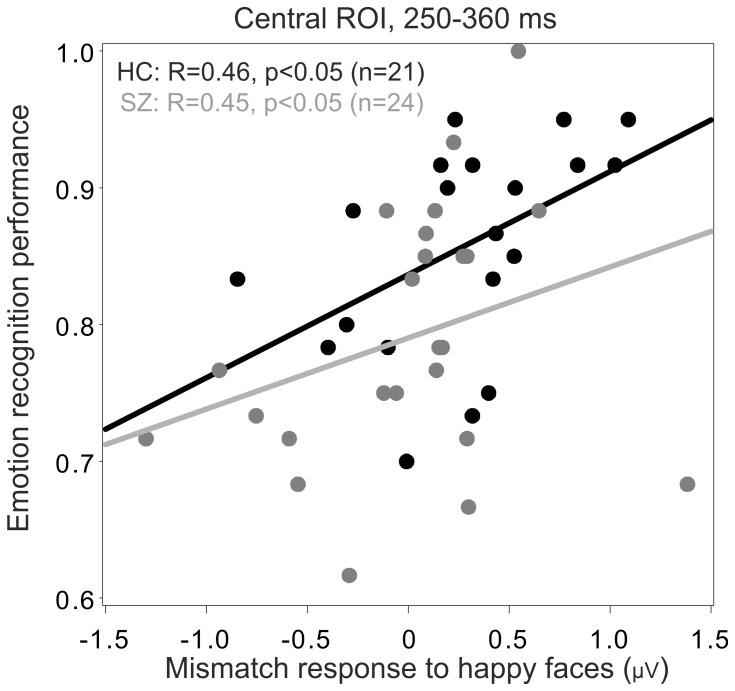
Emotion Recognition and its Association with the Mismatch Responses
Behavioral performance on the emotion recognition task as indexed by the Facial Expressions of Emotion – Stimuli and Tests (FEEST) significantly differed between the study groups (Kruskal-Wallis Test: Chi2 = 6.99, n = 45, P = 0.008). The mean correct recognition scores (Control group = 85.9%, (SD = 7.5), Schizophrenic group = 79.0%, (SD = 9.3)) indicated a deficit in emotion recognition in the patient group. The effects size was 0.82 SD. Due to technical difficulties three healthy control subjects’ emotion recognition scores were not obtained thus only n = 21 control participants’ data were entered in group comparison.
Mismatch response to happy condition in the central ROI correlated significantly with overall emotion recognition (Spearman R = 0.49, n = 45, P<0.001), after correction for multiple testing. This correlation was significant in both study groups (Controls: R = 0.46, n = 21, P<0.05; Patients: R = 0.45, n = 24, P<0.04). All correlations were controlled for age and gender. More positive mismatch signals were associated with higher recognition rates in this region ( Figure 4 ). No significant association between mismatch response and emotion recognition was found in the other ROIs.
Figure 4. Association between recognition accuracy and mismatch responses.
Subjects with Schizophrenia: Grey, Control Subjects: Black; ROI = Region of Interest. More positive mismatch signals were associated with higher recognition rates in this region.
Association between Emotion Recognition Performance, Symptom Severity, and Antipsychotic Medication Dose in the Schizophrenia Group
Symptom severity (PANSS total, positive and negative scores) and antipsychotic medication did not affect emotion recognition performance (Spearman rank correlation, P>0.4).
Source Localization of the Mismatch Responses by sLORETA
The source activations underlying the scalp ERP waveforms were calculated for each subject using a statistical nonparametric mapping method based on the sLORETA toolbox. First, voxel-by-voxel comparisons were made between standard and deviant stimuli within the groups separately for the 2 emotion conditions, and thereafter between the mismatch signals of the two study groups by independent t-test (Control Group Deviant minus Control Group Standard vs. Schizophrenia Group Deviant minus Schizophrenia Group Standard). Statistical significance was assessed with a nonparametric randomization test (n = 5000) that corrects for multiple comparisons [44]. Source locations were estimated for the 170–220 and 250–360 ms time windows.
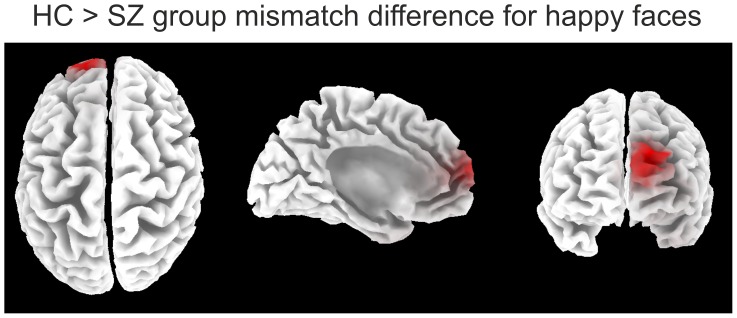
In the Schizophrenia group, no difference was observed between standard and deviant stimuli in any of the time windows for either condition. In the Control group significant differences were found between standard and deviant stimuli in the 170–220 ms time window at (P<0.1) level and in the 250–360 ms period at (P<0.05) level for both emotion conditions in frontal regions ( Table 4 ). Group comparison revealed a significantly attenuated activity in the 250–360 ms time window for both emotion conditions (P<0.05 for happy condition, and P<0.1 for fear condition) in frontal regions in the Schizophrenia group. Results are summarized in Table 4 and Figure 5 .
Table 4. Source Localization of the Mismatch Signals.
| Study Group(s) | Condition(s) | Time window | Areas1 | Brodmann | MNI coordinates at tmax | |||
| Areas | X | Y | Z | |||||
| 170–220 ms | Middle Frontal Gyrus(*) | 11 | −45 | 45 | −15 | |||
| Superior Frontal Gyrus(*) | 8 | 25 | 25 | 55 | ||||
| 250–360 ms | Middle Frontal Gyrus* | 6, 8, 10, 11, 47 | −40 | 55 | −5 | |||
| Happy Deviant | Superior Frontal Gyrus* | 6, 8, 10, 11 | 30 | 25 | 55 | |||
| Within | Control Group | vs. | Inferior Frontal Gyrus* | 10, 47 | −40 | 55 | 5 | |
| Group | Happy Standard | Sub-Gyral* | 8, 10 | −40 | 45 | 0 | ||
| Comparison | Cingulate Gyrus* | 6, 24, 32 | 20 | 5 | 50 | |||
| Medial Frontal Gyrus(*) | 6, 8, 10, 32 | 15 | 10 | 50 | ||||
| Anterior Cingulate(*) | 32 | −20 | 45 | 10 | ||||
| Schizophrenia Group | Happy Deviant vs. | 170–220 ms | No Significant Difference | – | – | – | – | |
| Happy Standard | 250–360 ms | No Significant Difference | – | – | – | – | ||
| 170–220 ms | No Significant Difference | – | – | – | – | |||
| Between | Control Group | Happy | 250–360 ms | Superior Frontal Gyrus * | 9, 10 | −15 | 60 | 25 |
| Group | vs. | Mismatch | Middle Frontal Gyrus * | 10 | −20 | 60 | 25 | |
| Comparison | Schizophrenia Group | Medial Frontal Gyrus * | 9, 10 | −5 | 55 | 20 | ||
| Anterior Cingulate * | 32 | −5 | 45 | 15 | ||||
| Fear Deviant | 170–220 ms | Superior Frontal Gyrus(*) | 8, 9 | 30 | 45 | 40 | ||
| Within | Control Group | vs. | Middle Frontal Gyrus(*) | 8, 9 | 25 | 45 | 40 | |
| Group | Fear Standard | 250–360 ms | Superior Frontal Gyrus* | 6 | −15 | 20 | 65 | |
| Comparison | Schizophrenia Group | Fear Deviant vs. | 170–220 ms | No Significant Difference | – | – | – | – |
| Fear Standard | 250–360 ms | No Significant Difference | – | – | – | – | ||
| Between | Control Group | Fear | 170–220 ms | No Significant Difference | – | – | – | – |
| Group | vs. | Mismatch | 250–360 ms | Superior Frontal Gyrus( * ) | 6 | −15 | 20 | 65 |
| Comparison | Schizophrenia Group | |||||||
p<0.05, two-tailed, (*) p<0.1, two-tailed.
Areas listed by tmax in decreasing order.
Figure 5. Results of the source localization for the happy condition.
Red color indicates significant group differences in mismatch generation to the happy condition in the 250–360 ms time window. (HC = Healthy Controls, SZ = Patients with Schizophrenia).
Discussion
To our knowledge the current study is the first to compare visual mismatch responses, an index of automatic predictive mechanisms, to unattended facial expressions between patients with schizophrenia and controls. Non-conscious expectations were induced by frequent repetitions of unattended faces (standard) expressing a particular emotion, and this expectation was violated by faces expressing another emotion (deviant). ERPs to physically identical deviant and standard stimuli were compared to control for possible effects for differences in low-level physical features. Although this method does not control for possible refractoriness effects per se as equiprobable paradigms do [45], [46], we interpret the observed mismatch activity as prediction error responses to ‘unexpected’ emotions, since in the current study pictures of several male and female models were used to avoid the possibility of low-level adaptation to features of a particular face. Thus predictive memory representations were formed for emotions, rather than to individual faces.
Diminished Visual Mismatch Responses in the Schizophrenia Group and Differences with Controls
In the schizophrenia group, a tendency for mismatch responses was detected over the occipital regions for the fear condition in the 170–220 ms and 250–360 ms time windows ( Table 3 , Supporting Information: Figure S1). However, after correction for multiple testing mismatch responses in the patient group did not reach significance for any of the emotional conditions. These findings are in line with the results of Urban et. al., who also reported decreased visual mismatch responses in a schizophrenic group in a motion-direction oddball paradigm [19].
In the control group mismatch responses were detected for fearful faces in the left and right occipital and in the right temporal regions in the 250–360 ms time window. Between study groups, the difference was significant over the right temporal region for fearful faces ( Figure 2 ). In the control group, for the happy condition, mismatch responses were detected in the 170–220 ms time window in the left temporal and central regions, and in the 250–360 ms time window in the left occipital and central regions, and again no such effects emerged in the schizophrenic group. Group differences were significant and showed large effects sizes in the 170–220 ms time window in the left temporal and central regions and in the 250–360 ms time window in the central region for happy faces ( Table 3 and Figure 2 ).
Medium-to-high effect sizes were also detected for both time windows for both conditions, but they did not reach significance due to the relatively small sample size. Furthermore, significant group differences were excluded where the difference between deviant and standard stimulus did not reach significance in any of the study groups (e.g. Left Temporal ROI late time window, happy stimulus). The largest effect sizes between study groups were in the 0.75–0.89 range ( Table 3 ), which fall well within the 95% confidence limits determined by a meta-analysis of auditory MMN studies in schizophrenia (mean effect size = 0.99, 95% CI:0.79–1.29) [7]. This indicates that the magnitude of the deficit in mismatch generation in the visual modality is comparable to that detected in auditory modality. Our results showed that the visual (emotion processing) system was capable of detecting the difference between frequent (standard) and rare (deviant) stimuli in healthy participants, while the same detection process was impaired in patients with schizophrenia. Alternatively, it is conceivable that the build-up of the expectation for a reappearing (repeating) emotion might have failed in schizophrenia patients, thereby preventing the elicitation of a mismatch response. In either case, our results demonstrate that impairment of emotion processing in schizophrenia is present already at the automatic unconscious level. The fact that the severity of psychotic symptoms did not influence the mismatch signals in the specified regions and time windows support the notion that this is rather a trait- than a state-like deficit in schizophrenia.
In the auditory modality diminished MMN in schizophrenic patients has been attributed to N-methyl-D-aspartate (NMDA) receptor-mediated glutamate dysfunction [47], [48]. NMDA antagonists have been shown to diminish MMN amplitude in animal models [49]. It is possible that a similar receptor mechanism may underlie the generation of visual MMN and that visual mismatch deficits in schizophrenia might be caused by altered modulation of NMDA receptor-related synaptic plasticity [18], [50]. However, further studies are required to evaluate this possibility.
Relationship between Mismatch Responses and Emotion Recognition
Mismatch responses with positive polarity were observed in central regions for both emotional conditions. Previous studies applying oddball paradigms have observed this positive response mainly in central and anterior regions [8], [51]. It has been proposed that responses of fusiform sources to face stimuli in scalp EEG recordings usually manifest as positivities at the vertex [52], [53]. The fusiform gyrus is a face-selective area [54], and might have contributed to the processing of facial emotions in our experiment.
One of the key findings of the present study is that mismatch responses showed an association with emotion recognition performance. Mismatch response amplitude for happy faces positively correlated with overall emotion recognition and was significantly more positive in the control group relative to the patient group in the central region (250–360 ms time window).
To our knowledge this is the first study to demonstrate a relationship between mismatch signals and emotion recognition performance. Earlier studies showed that auditory MMN impairments can be linked to cognitive [55] and everyday functioning [56]. Light and Braff [56] suggested that MMN deficits represent a core neurophysiological dysfunction, which is linked to global impairments in everyday functioning in schizophrenia patients. They found that deficits in automatic preattentive information processing, as measured by MMN, strongly correlated with global functioning in subjects with schizophrenia, although they did not find a relationship between symptom severity, laboratory-based measures of functional capacity (UPSA), and mismatch amplitudes. Social functioning is also strongly correlated with social cognition and facial affect recognition [57], [58]. These findings, taken together with our results support the notion that emotion recognition deficits might be mediators between automatic preattentive information processing deficits and everyday life functioning impairments in schizophrenia. A future study applying a visual mismatch paradigm to test facial emotion processing should also include measures of facial affect recognition and social functioning to confirm this notion.
Source Localization
The estimated sources of the mismatch responses for both emotional conditions were localized in prefrontal regions. This is in line with prior results [5] showing that sources of visual MMN to emotional faces in healthy subjects were located in frontal and temporal cortices. These regions play a key role in the formation and updating of visual predictions [16], [59]. A recent study [60] reported decreased source activity to emotional faces in frontal regions in patients with schizophrenia compared to controls. Taken together with our findings, these results also corroborate the notion that impaired functioning of frontal-prefrontal brain regions might be an underlying cause of deficits in emotion recognition in schizophrenia. The finding that sLOTERA localized the source of the MM signal in the frontal region and yielded a significant between group difference while the effect size did not reach statistical significance for this ROI on the scalp maybe due to the fact the EEG signal dampens, and undergoes spatial blurring while transmitted to broad regions of the scalp [61]. However, with the dense electrode array we used, sLORETA captures this spatially distributed information since it calculates the sources of the EEG signal by solving the inverse problem based on all electrodes.
Contrary to our expectations and previous results [5], neural generators were not identified in the temporal gyrus (e.g. in the Fusiform Face Area). A possible explanation is that simultaneously active sources can only be separated by sLORETA if their fields are distinct enough and of similar strength. In the context of a strong or superficial source, weak or deep sources remain invisible for this method, and nearby sources of similar orientation tend not to be separated but interpreted as one source located roughly in between [62]. Future studies with better resolution will be needed to clarify this issue.
Limitations and Future Directions
A main limitation of our study is that all patients had been receiving psychotropic medication at the time of testing. However, no correlation was found between antipsychotic dose and mismatch signals, which is in line with previous findings, namely that D2 or 5 HT2 antagonist antipsychotics such as Clozapine and Olanzapine do not influence MMN amplitude [63], [64]. Another limitation is that the investigation was cross-sectional and the average PANSS scores were low, indicating a chronic-stable mental state [65], which may have limited our ability to find a correlation between symptom severity and mismatch signals. Further longitudinal studies are needed to clarify this association. Since our aim was to study emotion recognition, in the present study specific visual stimuli (i.e. emotional facial expressions) were used. Accordingly, further research should investigate the correlation between MMN to simpler visual stimuli and social cognition.
Conclusions
Building up a predictive model based on the regularities of facial expressions around us and the comparison of any upcoming facial cue to this model can be the key to the unintentional recognition of others’ facial expressions in everyday life. Our findings support the notion that impaired generation of mismatch signals may indicate impairment in automatic processing of emotions in patients with schizophrenia, which leads to decreased emotion recognition and subsequently to a disability in social functioning.
Supporting Information
Event-related potentials and mismatch waveforms by region (HC = Healthy Controls, SZ = Patients with Schizophrenia). Upper panel: ERPs for fearful faces; lower panel: ERPs for happy faces. Shaded intervals indicate time windows of amplitude measurements. Crosses mark time windows where deviant and standard waveforms differ significantly (i.e. significant mismatch waveform).
(EPS)
Funding Statement
The study was partially supported by the “Ambient Assisted Living Joint Programme – Call 2” grant (Project Identifier: AAL_08-1-2011-0005 M3W). (http://www.aal-europe.eu). The additional part of the study was supported by the National Research Fund of Hungary (OTKA, 71600; http://www.otka.hu/en). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Kee KS, Green MF, Mintz J, Brekke JS (2003) Is emotion processing a predictor of functional outcome in schizophrenia? Schizophr Bull 29: 487–497. [DOI] [PubMed] [Google Scholar]
- 2. Kohler CG, Walker JB, Martin EA, Healey KM, Moberg PJ (2010) Facial emotion perception in schizophrenia: a meta-analytic review. Schizophr Bull 36: 1009–1019 sbn192 [pii]; 10.1093/schbul/sbn192 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eimer M, Holmes A (2007) Event-related brain potential correlates of emotional face processing. Neuropsychologia 45: 15–31 S0028-3932(06)00157-6 [pii]; 10.1016/j.neuropsychologia.2006.04.022 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Astikainen P, Hietanen JK (2009) Event-related potentials to task-irrelevant changes in facial expressions. Behav Brain Funct 5: 30 1744-9081-5-30 [pii]; 10.1186/1744-9081-5-30 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimura M, Kondo H, Ohira H, Schroger E (2011) Unintentional Temporal Context-Based Prediction of Emotional Faces: An Electrophysiological Study. Cereb Cortex. bhr244 [pii]; 10.1093/cercor/bhr244 [doi] [DOI] [PubMed]
- 6. Naatanen R, Paavilainen P, Rinne T, Alho K (2007) The mismatch negativity (MMN) in basic research of central auditory processing: a review. Clin Neurophysiol 118: 2544–2590 S1388-2457(07)00193-9 [pii]; 10.1016/j.clinph.2007.04.026 [doi] [DOI] [PubMed] [Google Scholar]
- 7. Umbricht D, Krljes S (2005) Mismatch negativity in schizophrenia: a meta-analysis. Schizophr Res 76: 1–23 S0920-9964(04)00459-1 [pii]; 10.1016/j.schres.2004.12.002 [doi] [DOI] [PubMed] [Google Scholar]
- 8. Czigler I, Balazs L, Winkler I (2002) Memory-based detection of task-irrelevant visual changes. Psychophysiology 39: 869–873 10.1017/S0048577202020218 [doi];S0048577202020218 [pii] [DOI] [PubMed] [Google Scholar]
- 9. Astikainen P, Ruusuvirta T, Wikgren J, Korhonen T (2004) The human brain processes visual changes that are not cued by attended auditory stimulation. Neurosci Lett 368: 231–234 10.1016/j.neulet.2004.07.025 [doi];S0304-3940(04)00889-4 [pii] [DOI] [PubMed] [Google Scholar]
- 10. Pazo-Alvarez P, Amenedo E, Lorenzo-Lopez L, Cadaveira F (2004) Effects of stimulus location on automatic detection of changes in motion direction in the human brain. Neurosci Lett 371: 111–116 S0304-3940(04)01085-7 [pii]; 10.1016/j.neulet.2004.08.073 [doi] [DOI] [PubMed] [Google Scholar]
- 11. Sulykos I, Czigler I (2011) One plus one is less than two: visual features elicit non-additive mismatch-related brain activity. Brain Res 1398: 64–71 S0006-8993(11)00868-7 [pii]; 10.1016/j.brainres.2011.05.009 [doi] [DOI] [PubMed] [Google Scholar]
- 12. Stagg C, Hindley P, Tales A, Butler S (2004) Visual mismatch negativity: The detection of stimulus change. Neuroreport 15: 659–663. [DOI] [PubMed] [Google Scholar]
- 13. Stefanics G, Czigler I (2012) Automatic prediction error responses to hands with unexpected laterality: an electrophysiological study. NeuroImage 63: 253–261 S1053-8119(12)00684-2 [pii]; 10.1016/j.neuroimage.2012.06.068 [doi] [DOI] [PubMed] [Google Scholar]
- 14. Czigler I, Weisz J, Winkler I (2007) Backward masking and visual mismatch negativity: electrophysiological evidence for memory-based detection of deviant stimuli. Psychophysiology 44: 610–619 PSYP530 [pii]; 10.1111/j.1469-8986.2007.00530.x [doi] [DOI] [PubMed] [Google Scholar]
- 15. Czigler I, Sulykos I (2010) Visual mismatch negativity to irrelevant changes is sensitive to task-relevant changes. Neuropsychologia 48: 1277–1282 S0028-3932(09)00515-6 [pii]; 10.1016/j.neuropsychologia.2009.12.029 [doi] [DOI] [PubMed] [Google Scholar]
- 16.Kimura M (2011) Visual mismatch negativity and unintentional temporal-context-based prediction in vision. Int J Psychophysiol. S0167-8760(11)00357-6 [pii]; 10.1016/j.ijpsycho.2011.11.010 [doi] [DOI] [PubMed]
- 17. Friston K (2010) The free-energy principle: a unified brain theory? Nat Rev Neurosci 11: 127–138 nrn2787 [pii]; 10.1038/nrn2787 [doi] [DOI] [PubMed] [Google Scholar]
- 18. Stephan KE, Baldeweg T, Friston KJ (2006) Synaptic plasticity and dysconnection in schizophrenia. Biol Psychiatry 59: 929–939 S0006-3223(05)01269-2 [pii]; 10.1016/j.biopsych.2005.10.005 [doi] [DOI] [PubMed] [Google Scholar]
- 19. Urban A, Kremlacek J, Masopust J, Libiger J (2008) Visual mismatch negativity among patients with schizophrenia. Schizophr Res 102: 320–328 S0920-9964(08)00153-9 [pii]; 10.1016/j.schres.2008.03.014 [doi] [DOI] [PubMed] [Google Scholar]
- 20. Calvo MG, Nummenmaa L (2007) Processing of unattended emotional visual scenes. J Exp Psychol Gen 136: 347–369 2007-11669-001 [pii]; 10.1037/0096-3445.136.3.347 [doi] [DOI] [PubMed] [Google Scholar]
- 21. Calvo MG, Avero P (2008) Affective priming of emotional pictures in parafoveal vision: left visual field advantage. Cogn Affect Behav Neurosci 8: 41–53. [DOI] [PubMed] [Google Scholar]
- 22. Calvo MG, Dolores Castillo M, Fuentes LJ (2006) Processing of “unattended” threat-related information: Role of emotional content and context. Cognition and Emotion 20: 1049–1074. [Google Scholar]
- 23. Maekawa T, Hirano S, Onitsuka T (2012) Auditory and Visual Mismatch Negativity in Psychiatric Disorders: A Review. Current Psychiatry Reviews 8: 97–105. [Google Scholar]
- 24. Stefanics G, Kimura M, Czigler I (2011) Visual mismatch negativity reveals automatic detection of sequential regularity violation. Front Hum Neurosci 5: 46 10.3389/fnhum.2011.00046 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stefanics G, Csukly G, Komlósi S, Czobor P, Czigler I (2012) Processing of unattended facial emotions: A visual mismatch negativity study. NeuroImage 59: 3042–3049 10.1016/j.neuroimage.2011.10.041 [DOI] [PubMed] [Google Scholar]
- 26. Naatanen R, Kujala T, Winkler I (2011) Auditory processing that leads to conscious perception: a unique window to central auditory processing opened by the mismatch negativity and related responses. Psychophysiology 48: 4–22 10.1111/j.1469-8986.2010.01114.x [doi] [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatry Association (1994) DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, fourth ed. Washington, DC.: American Psychiatry Association.
- 28. Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276. [DOI] [PubMed] [Google Scholar]
- 29.Derogatis LR (1994) SCL-90-R: Symptom Checklist-90-R. Administration, scoring, and procedures manual. Minneapolis, Minnesota: National Computer Sytems.
- 30. Unoka Zs, Rózsa S, Kő N, Kállai J, Fábián Á, et al. (2004) Validity and reliability of the SCL-90 in a Hungarian population sample. Psychiatria Hungarica 19: 235–243. [Google Scholar]
- 31.Ekman P, Friesen WV (1976) Pictures of facial affect. Palo Alto, CA: Consulting Psychologists Press.
- 32. Metting van Rijn AC, Peper A, Grimbergen CA (1990) High-quality recording of bioelectric events. Part 1. Interference reduction, theory and practice. Med Biol Eng Comput 28: 389–397. [DOI] [PubMed] [Google Scholar]
- 33. Delorme A, Makeig S (2004) EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods 134: 9–21 10.1016/j.jneumeth.2003.10.009 [doi];S0165027003003479 [pii] [DOI] [PubMed] [Google Scholar]
- 34. Yao J, Dewald JP (2005) Evaluation of different cortical source localization methods using simulated and experimental EEG data. Neuroimage 25: 369–382 S1053-8119(04)00721-9 [pii]; 10.1016/j.neuroimage.2004.11.036 [doi] [DOI] [PubMed] [Google Scholar]
- 35. Hochberg Y (1988) A sharper bonferroni procedure for multiple tests of significance. Biometrika 75: 800–802. [Google Scholar]
- 36. Zhao L, Li J (2006) Visual mismatch negativity elicited by facial expressions under non-attentional condition. Neurosci Lett 410: 126–131. [DOI] [PubMed] [Google Scholar]
- 37.Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates.
- 38.Pascual-Marqui RD (2002) Standardized low-resolution brain electromagnetic tomography (sLORETA): technical details. Methods Find Exp Clin Pharmacol 24 Suppl D: 5–12. 846 [pii]. [PubMed]
- 39.Fuchs M, Kastner J, Wagner M, Hawes S, Ebersole JS (2002) A standardized boundary element method volume conductor model. Clin Neurophysiol 113: 702–712. S1388245702000305 [pii]. [DOI] [PubMed]
- 40. Jurcak V, Tsuzuki D, Dan I (2007) 10/20, 10/10, and 10/5 systems revisited: their validity as relative head-surface-based positioning systems. Neuroimage 34: 1600–1611 S1053-8119(06)00972-4 [pii]; 10.1016/j.neuroimage.2006.09.024 [doi] [DOI] [PubMed] [Google Scholar]
- 41. Mazziotta J, Toga A, Evans A, Fox P, Lancaster J, et al. (2001) A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos Trans R Soc Lond B Biol Sci 356: 1293–1322 10.1098/rstb.2001.0915 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, et al. (2000) Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp 10: 120–131 10.1002/1097-0193(200007)10:3<120::AID-HBM30>3.0.CO;2-8 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brett M, Johnsrude IS, Owen AM (2002) The problem of functional localization in the human brain. Nat Rev Neurosci 3: 243–249 10.1038/nrn756 [doi];nrn756 [pii] [DOI] [PubMed] [Google Scholar]
- 44. Nichols TE, Holmes AP (2002) Nonparametric permutation tests for functional neuroimaging: a primer with examples. Hum Brain Mapp 15: 1–25 10.1002/hbm.1058 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li X, Lu Y, Sun G, Gao L, Zhao L (2012) Visual mismatch negativity elicited by facial expressions: new evidence from the equiprobable paradigm. Behav Brain Funct 8: 7 1744-9081-8-7 [pii]; 10.1186/1744-9081-8-7 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kimura M, Katayama J, Ohira H, Schroger E (2009) Visual mismatch negativity: new evidence from the equiprobable paradigm. Psychophysiology 46: 402–409 PSYP767 [pii]; 10.1111/j.1469-8986.2008.00767.x [doi] [DOI] [PubMed] [Google Scholar]
- 47. Javitt DC, Steinschneider M, Schroeder CE, Arezzo JC (1996) Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: implications for schizophrenia. Proc Natl Acad Sci U S A 93: 11962–11967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heekeren K, Daumann J, Neukirch A, Stock C, Kawohl W, et al. (2008) Mismatch negativity generation in the human 5HT2A agonist and NMDA antagonist model of psychosis. Psychopharmacology (Berl) 199: 77–88 10.1007/s00213-008-1129-4 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tikhonravov D, Neuvonen T, Pertovaara A, Savioja K, Ruusuvirta T, et al. (2008) Effects of an NMDA-receptor antagonist MK-801 on an MMN-like response recorded in anesthetized rats. Brain Res 1203: 97–102 S0006-8993(08)00348-X [pii]; 10.1016/j.brainres.2008.02.006 [doi] [DOI] [PubMed] [Google Scholar]
- 50.Schmidt A, Diaconescu AO, Kometer M, Friston KJ, Stephan KE, et al. (2012) Modeling Ketamine Effects on Synaptic Plasticity During the Mismatch Negativity. Cereb Cortex. bhs238 [pii]; 10.1093/cercor/bhs238 [doi] [DOI] [PMC free article] [PubMed]
- 51. Astikainen P, Lillstrang E, Ruusuvirta T (2008) Visual mismatch negativity for changes in orientation–a sensory memory-dependent response. Eur J Neurosci 28: 2319–2324 EJN6510 [pii]; 10.1111/j.1460-9568.2008.06510.x [doi] [DOI] [PubMed] [Google Scholar]
- 52. Jeffreys DA (1989) A face-responsive potential recorded from the human scalp. Exp Brain Res 78: 193–202. [DOI] [PubMed] [Google Scholar]
- 53. Schendan HE, Ganis G, Kutas M (1998) Neurophysiological evidence for visual perceptual categorization of words and faces within 150 ms. Psychophysiology 35: 240–251. [PubMed] [Google Scholar]
- 54. Halgren E, Raij T, Marinkovic K, Jousmaki V, Hari R (2000) Cognitive response profile of the human fusiform face area as determined by MEG. Cereb Cortex 10: 69–81. [DOI] [PubMed] [Google Scholar]
- 55. Baldeweg T, Klugman A, Gruzelier J, Hirsch SR (2004) Mismatch negativity potentials and cognitive impairment in schizophrenia. Schizophr Res 69: 203–217. [DOI] [PubMed] [Google Scholar]
- 56. Light GA, Braff DL (2005) Mismatch negativity deficits are associated with poor functioning in schizophrenia patients. Arch Gen Psychiatry 62: 127–136 62/2/127 [pii]; 10.1001/archpsyc.62.2.127 [doi] [DOI] [PubMed] [Google Scholar]
- 57. Addington J, Saeedi H, Addington D (2006) Influence of social perception and social knowledge on cognitive and social functioning in early psychosis. Br J Psychiatry 189: 373–378 189/4/373 [pii]; 10.1192/bjp.bp.105.021022 [doi] [DOI] [PubMed] [Google Scholar]
- 58. Mancuso F, Horan WP, Kern RS, Green MF (2011) Social cognition in psychosis: multidimensional structure, clinical correlates, and relationship with functional outcome. Schizophr Res 125: 143–151 S0920-9964(10)01636-1 [pii]; 10.1016/j.schres.2010.11.007 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bar M (2007) The proactive brain: using analogies and associations to generate predictions. Trends Cogn Sci 11: 280–289 S1364-6613(07)00129-5 [pii]; 10.1016/j.tics.2007.05.005 [doi] [DOI] [PubMed] [Google Scholar]
- 60. Jung HT, Kim DW, Kim S, Im CH, Lee SH (2012) Reduced source activity of event-related potentials for affective facial pictures in schizophrenia patients. Schizophr Res 136: 150–159 S0920-9964(11)00558-5 [pii]; 10.1016/j.schres.2011.10.023 [doi] [DOI] [PubMed] [Google Scholar]
- 61. Srinivasan R, Tucker D, Murias M (1998) Estimating the spatial Nyquist of the human EEG. Behavior Research Methods, Instruments, & Computers 30: 8–19 10.3758/BF03209412. [Google Scholar]
- 62. Wagner M, Fuchs M, Kastner J (2004) Evaluation of sLORETA in the presence of noise and multiple sources. Brain Topogr 16: 277–280. [DOI] [PubMed] [Google Scholar]
- 63.Umbricht D, Javitt D, Novak G, Bates J, Pollack S, et al.. (1998) Effects of clozapine on auditory event-related potentials in schizophrenia. Biol Psychiatry 44: 716–725. S0006-3223(97)00524-6 [pii]. [DOI] [PubMed]
- 64. Korostenskaja M, Dapsys K, Siurkute A, Maciulis V, Ruksenas O, et al. (2005) Effects of olanzapine on auditory P300 and mismatch negativity (MMN) in schizophrenia spectrum disorders. Prog Neuropsychopharmacol Biol Psychiatry 29: 543–548 S0278-5846(05)00049-7 [pii]; 10.1016/j.pnpbp.2005.01.019 [doi] [DOI] [PubMed] [Google Scholar]
- 65. Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, et al. (2005) What does the PANSS mean? Schizophr Res 79: 231–238 S0920-9964(05)00161-1 [pii]; 10.1016/j.schres.2005.04.008 [doi] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Event-related potentials and mismatch waveforms by region (HC = Healthy Controls, SZ = Patients with Schizophrenia). Upper panel: ERPs for fearful faces; lower panel: ERPs for happy faces. Shaded intervals indicate time windows of amplitude measurements. Crosses mark time windows where deviant and standard waveforms differ significantly (i.e. significant mismatch waveform).
(EPS)