Abstract
Background
Aseptic loosening of the femoral stem remains a significant reason for revision in total hip arthroplasty (THA). Although stem fixation methods have changed over time, there is relatively little evidence supporting cemented or uncemented stems as more durable constructs.
Questions/purposes
We examined whether there was a difference in survival to revision between cemented and uncemented THA stems (1) for any reason; (2) for aseptic loosening or loosening related to wear/osteolysis; (3) based on patient age groupings (as a proxy for patient activity level); and (4) based on procedural timeframe groupings between cemented and uncemented stems.
Methods
A total of 6498 primary cemented and uncemented THAs were registered in our community total joint replacement registry between 1991 and 2011. Analysis was performed to compare age, sex, procedural timeframe, and diagnosis for both groups. Our primary outcome was revision of the stem component for aseptic loosening or loosening secondary to wear/osteolysis. Analyses were done using Wilcoxon rank sum tests, Pearson’s chi-square tests, Kaplan Meier methods, and Cox regression.
Results
After adjusting for age, sex, primary diagnosis, and procedural timeframe as confounders, cemented femoral stem components were 1.63 times as likely as uncemented stems to be revised for any reason (p = 0.02) and 3.76 times as likely as uncemented stems to be revised for aseptic loosening or loosening related to wear/osteolysis (p < 0.001). When grouped by age, specifically in regard to revisions for aseptic loosening or loosening related to wear/osteolysis, uncemented stems had lower cumulative revision rates in patients aged < 70 years (p < 0.001) compared with cemented stems. There was a trend away from cemented fixation in our registry, which shifted from over 80% cemented stem use in 1996 to 3% in 2011.
Conclusions
We found that uncemented stems were associated with fewer revisions for aseptic loosening in patients < 70 years old, but when all reasons for revision were considered, neither group demonstrated superior survival. With a mean followup of 6.5 years, longer followup is needed to verify these results over time.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Approximately 200,000 people undergo THA each year in the United States [21] and that number is projected to increase in the next few decades to more than 500,000 in 2030 [19, 20]. The Charnley low friction arthroplasty developed in 1962 is still widely considered the gold standard for cemented femoral stems with excellent survival in long-term followup [3, 5, 30, 33].
However, some cemented femoral stems had a roughened surface texture, whereas others had a poly(methylmethacrylate) precoating and were associated with high revision rates secondary to osteolysis and aseptic loosening [6, 23, 31, 32]. In comparison to ingrowth stems, cemented stems may be more technically demanding and require more operative time and may result in increased marrow pressure and embolic phenomena unless special techniques are used to vent the pressure [11, 26, 28], although this has been contested [18].
Uncemented stems have generally demonstrated excellent survival rates [1, 7] with revisions, when required, usually being caused by aseptic loosening or osteolysis [12]. However, uncemented femoral stems with noncircumferential porous coating and designs coupled with inferior ultrahigh-molecular-weight polyethylene manufacturing or sterilization methods have been complicated by high rates revision resulting from osteolysis, loosening, and failure of bony ingrowth [8, 21, 29]. Iatrogenic fracture [2], thigh pain [25], and subsidence [4, 24] also occur more frequently in uncemented stems.
Surgeon preference for fixation technique of the femoral component in THA and the factors influencing that choice have evolved over time. There have been relatively few registry studies that have examined stem revision rates of cemented and uncemented femoral stems resulting from aseptic loosening or loosening related to wear/osteolysis [10, 15, 17, 22], and these do not necessarily reflect the changing practice patterns of North American community orthopaedists over time. We therefore compared the survival of cemented versus uncemented femoral components in a community-based total joint registry.
Specifically, we examined whether there was a difference in survival to revision (1) for any reason; (2) for aseptic loosening, wear, or osteolysis; (3) based on patient age groupings (as a proxy for patient activity level); and (4) based on procedural timeframe groupings between cemented and uncemented stems.
Patients and Methods
The HealthEast Joint Registry (HEJR) is a total joint registry that tracks hip and knee arthroplasties performed by 77 surgeons at five community hospitals in the St Paul, MN, USA, metropolitan area. Information on 6498 hip arthroplasties was collected in the HEJR between September 1, 1991, and September 30, 2011. Details of the data collection methods and application of statistical analyses in the HEJR have been previously reported [13].
All cemented and uncemented THAs were considered for inclusion (n = 6498). Constructs with recalled acetabular implants (DePuy ASR™, DePuy, Warsaw, IN, USA; Sulzer InterOp™, Zimmer, Warsaw, IN, USA) were included (n = 193); 4319 uncemented THAs and 2179 cemented THAs thus made up the study population. The constructs with recalled acetabular implants were included because the recalls were for the acetabular components, not the stems, and in no case was the failure of these acetabular component implicated in a stem failure.
Of the 6498 THAs included, 57% were female, the mean age was 65.4 years (range, 14–97 years), and the minimum followup was 0 years (mean, 6.5 years; range, 0–18.3 years). The minimum followup was selected based on registry standards for cumulative revision rate analysis and to capture early failures including iatrogenic fractures. There were 135 stems that were revised, 64 uncemented THAs and 71 cemented THAs. Our outcomes of interest included stem revision for any reason (wear/osteolysis, aseptic loosening, periprosthetic fracture, infection, dislocation, failure of bone ingrowth, mechanical failure/breakage, instability, unexplained pain, or other) and stem revision for the combined reasons of aseptic loosening or loosening related to wear/osteolysis.
There was no significant difference in primary diagnosis between the uncemented and cemented groups; patients with osteoarthritis comprised approximately 90% of each group. Patients with uncemented stems were younger, were more often male, were more often implanted in recent years, and had a shorter followup (Table 1).
Table 1.
Univariate analysis
| Category | Uncemented implant (n = 4319) | Cemented implant (n = 2179) | p value* |
|---|---|---|---|
| Followup (years), mean (SD) | 5.6 (4.8) | 10.5 (5.3) | < 0.0001 |
| Age (years), mean (SD) | 62.1 (12.1) | 71.9 (10.2) | < 0.0001 |
| Cost of implant, mean (SD) | $6074 ($1313) | $4491 ($1646) | < 0.0001 |
| Sex | |||
| Male | 2055 (48%) | 742 (34%) | < 0.0001 |
| Female | 2264 (52%) | 1437 (66%) | |
| Age categories (years) | |||
| < 55 | 1119 (26%) | 141 (6%) | < 0.0001 |
| 55–70 | 2051 (47%) | 699 (32%) | |
| > 70 | 1149 (27%) | 1339 (61%) | |
| Procedural timeframe | |||
| 1991–1998 | 513 (12%) | 1079 (50%) | < 0.0001 |
| 1999–2004 | 946 (22%) | 787 (36%) | |
| 2005–2011 | 2860 (66%) | 313 (14%) | |
| Primary diagnosis | |||
| Osteoarthritis | 3940 (91%) | 1958 (90%) | 0.07 |
| Aseptic necrosis | 201 (5%) | 104 (5%) | |
| Other | 178 (4%) | 117 (5%) | |
| Stem revision reason | |||
| Loosening related to wear/osteolysis | 5 (8%) | 5 (7%) | NA† |
| Aseptic loosening | 11 (17%) | 45 (63%) | |
| Periprosthetic fracture | 20 (31%) | 3 (4%) | |
| Infection | 7 (11%) | 5 (7%) | |
| Dislocation | 5 (8%) | 10 (14%) | |
| Failure of bone ingrowth | 12 (19%) | 0 (0%) | |
| Mechanical failure/breakage | 1 (2%) | 1 (1%) | |
| Instability | 0 (0%) | 2 (3%) | |
| Pain | 2 (3%) | 0 (0%) | |
| Other | 1 (2%) | 0 (0%) | |
* Probability values were calculated using the Wilcoxon rank-sum test for continuous variables and the Pearson’s chi-square test for categorical variables; † too many categories to calculate a meaningful p value; NA = not applicable.
Uncemented and cemented THAs were compared using Wilcoxon rank sum test for continuous variables (age and followup) and the Pearson’s chi-square test for categorical variables (sex, age categories, procedural timeframe, and primary diagnosis). Cumulative revision rates (CRRs) were calculated using the Kaplan-Meier survival method and were compared using the log-rank test. There were 1814 cemented stems and 2383 uncemented stems available for analysis at 5 years and 625 cemented stems and 303 uncemented at the 15-year interval. To determine the effect of age and procedural timeframe, CRRs for uncemented and cemented stems were created for each age group (< 55, 55–70, ≥ 70 years of age) and each timeframe (1991–1998, 1999–2004, 2005–2011). This was done in an effort to account for the evolution in bearing surface technology and polyethylene sterilization methods that might contribute to disparate rates of osteolysis and associated stem loosening over 20 years. Hazard ratios (relative risk of revision) were calculated using Cox proportional hazards regression and all variables mentioned previously were considered for potential confounding. Sex, age categories, primary diagnosis, and procedural timeframe categories were adjusted for in the Cox proportional hazards regression models.
Results
When all reasons for stem revision were included, uncemented and cemented stems showed similar cumulative revision rates (3.8%; 95% confidence interval [CI], 2.3%–4.9% versus 4.9%; 95% CI, 3.5%–6.3%, p = 0.09). However, after adjusting for confounders (sex, age categories, sex, primary diagnosis, and procedural timeframe), cemented femoral stem components were 1.63 (95% CI, 1.08–2.46) times as likely as uncemented stems to be revised for any reason (p = 0.02 (Table 2).
Table 2.
Cox proportional hazards regression (HR) models
| Revision type | Implant type | Crude HR (95% CI) | p value | Adjusted HR (95% CI)* | p value |
|---|---|---|---|---|---|
| All stem revisions | Uncemented implant | 1.00 (reference) | 1.00 (reference) | ||
| Cemented implant | 1.35 (0.95–1.35) | 0.09 | 1.63 (1.08–2.46) | 0.02 | |
| Stem revisions for aseptic loosening or loosening related to wear/osteolysis | Cemented implant | 1.00 (reference) | 1.00 (reference) | ||
| Uncemented implant | 3.02 (1.70–5.35) | 0.0002 | 3.76 (2.01–7.06) | < 0.0001 |
* Adjusted for age (< 55, 55–70, > 70 years), sex, year of index procedure (1991–1998, 1999–2004, 2005–2011), and diagnosis (osteoarthritis, aseptic necrosis, other); CI = confidence interval.
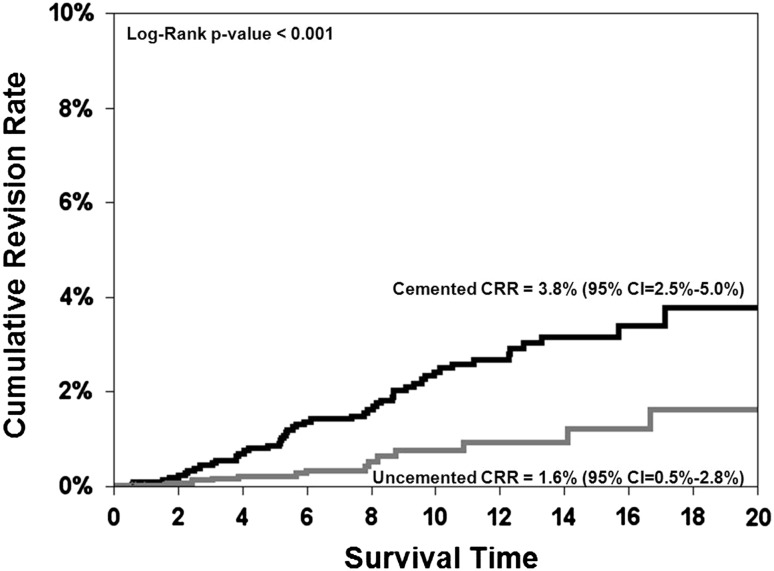
When compared with respect to revisions performed specifically for aseptic loosening or loosening related to wear/osteolysis, uncemented stems showed better survival with a lower CRR (1.6%; 95% CI, 0.5%–2.8% versus 3.8%; 95% CI, 2.5%–5.0%; p < 0.001; Fig. 1). A Cox proportional hazards regression model showed that cemented THAs were 3.76 (95% CI, 2.01–7.06) times as likely as uncemented THAs (p < 0.001) to have a stem revision for aseptic loosening or loosening related to wear/osteolysis after adjustment for age categories, sex, primary diagnosis, and procedural timeframe. Thirteen stems (seven cemented and six uncemented) were used in more than 100 cases with one uncemented stem (Secure-Fit®; Stryker, Kalamazoo, MI, USA) and one cemented stem (Perfecta®; Wright Medical, Arlington, TN, USA) demonstrating higher than expected cumulative revision rates (Table 3).
Fig. 1.
When compared with respect to revisions performed specifically for aseptic loosening or loosening related to wear/osteolysis, uncemented stems showed better survival.
Table 3.
Implant designs with the number of revisions and cumulative revision rates (CRRs)
| Stem | Uncemented designs | ||
|---|---|---|---|
| Number | Number revised | CRR (95% CI) | |
| Summit uncemented | 1559 | 12 | 0.8% (0.4%–1.3%) |
| Corail | 718 | 9 | 2.1% (0.4%–4.1%) |
| Accolade Plus TMZF | 308 | 2 | 1.7% (0%–1.4%) |
| Secur-Fit | 224 | 6 | 7.6% (0%–7.2%) |
| Citation TMZF | 177 | 2 | 1.4% (0%–3.2%) |
| Omniflex | 146 | 1 | 0.7% (0%–2.0%) |
| Cemented designs | |||
|---|---|---|---|
| Number | Number revised | CRR (95% CI) | |
| Summit cemented | 165 | 0 | 0% |
| Omnifit | 262 | 9 | 4.4% (1.5%–7.2%) |
| Ultima | 246 | 4 | 1.8% (0%–3.6%) |
| Premise | 243 | 7 | 4.0% (0.9%–7.2%) |
| ODC | 213 | 4 | 2.1% (0.1%–4.1%) |
| Perfecta PDA | 164 | 13 | 11.2% (4.0%–18.4%) |
| Omnifit Eon | 118 | 0 | 0% |
CI = confidence interval.
Patients < 55 years of age with uncemented stems had fewer stem revisions performed specifically as a result of aseptic loosening or loosening related to wear/osteolysis than patients with cemented stems (CRR 2.8%; 95% CI, 0%–5.9% versus 9.4%; 95% CI, 3.5%–15.2%; p < 0.001). Patients aged 55 to 70 years with uncemented stems had fewer revisions performed for all reasons (CRR 2.4%; 95% CI, 1.0%–3.8% versus 7.7%; 95% CI, 4.6%–10.7%; p = 0.001) and particularly for the aseptic loosening categories than patients with cemented stems (CRR 1.4%; 95% CI, 0.1%–2.7% versus 6.0%; 95% CI, 3.1%–8.9%; p < 0.001). When all reasons for stem revision were included, survival to revision based on patient age groupings between cemented and uncemented stems showed that patients < 55 years old with uncemented stems had no difference in CRRs than those with cemented stems (CRR 7.0%; 95% CI, 2.9%–11.0% versus 9.4%; 95% CI, 3.5%–15.2%; p = 0.09). For patients > 70 years old, uncemented and cemented stems had similar cumulative revision rates for all reasons (1.4%; 95% CI, 0.4%–2.4% versus 2.5%; 95% CI, 1.4%–3.5%; p = 0.62) and specifically for the aseptic loosening categories (0.1%; 95% CI, 0%–2.9% versus 1.6%; 95% CI, 0.7%–2.4%; p = 0.06).
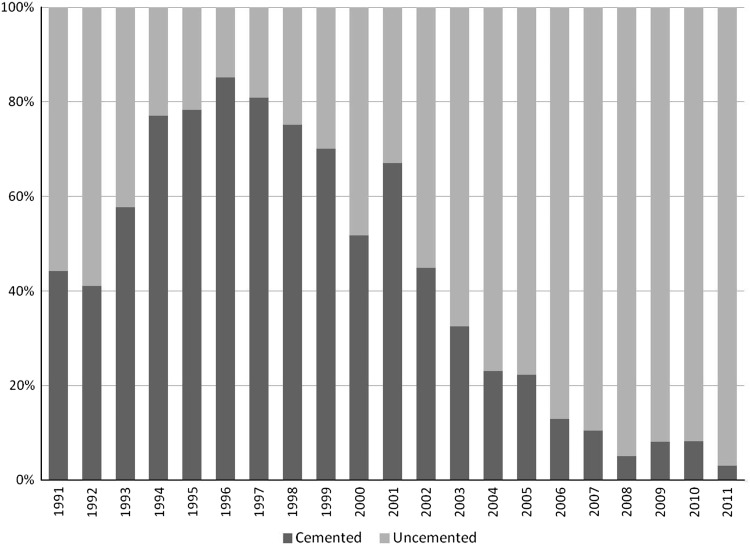
From 1991 to 2011, 6498 THAs were performed and recorded in the HEJR with nearly twice as many uncemented as cemented femoral stems implanted. From 1991 to 1998, a greater number of cemented stems were implanted (1079 cemented versus 513 uncemented) followed by a major shift toward uncemented implants between 1999 and the present (3806 uncemented versus 1100 cemented; Fig. 2). When implants were grouped into procedural timeframes and all reasons for stem revision were included, uncemented and cemented stems did not show a difference in cumulative revision rates for 1991 to 1998 (CRR 4.9%; 95% CI, 2.8%–6.9% versus 5.6%; 95% CI, 4.0%–7.3%; p = 0.52), 1999 to 2004 (CRR 1.8%; 95% CI, 0.7%–3.0% versus 3.1%; 95% CI, 1.8%–4.4%; p = 0.13), or 2005 to 2011 (CRR 2.6%; 95% CI, 0.3%–4.8% versus 0.3%; 95% CI, 0%–1.0%; p = 0.16). Revisions for aseptic loosening or loosening related to wear/osteolysis, however, were lower for uncemented stems placed during the timeframe 1999 to 2004 (CRR 0.2%; 95% CI, 0.0%–0.5% versus 2.5%; 95% CI, 1.3%–3.7%; p < 0.001) but not for 1991 to 1998 (CRR 3.1%; 95% CI, 1.4%–4.7% versus 4.1%; 95% CI, 2.6%–5.5%; p = 0.41) or 2005 to 2011 (CRR 0.04%; 95% CI, 0%–0.1% versus 0%; p = 0.73).
Fig. 2.
There has been a trend toward uncemented stem use in the registry over time.
Discussion
The decision on the part of the surgeon to use a cemented or uncemented stem is driven by numerous factors, yet during this time period most North American surgeons have used uncemented stems in greater numbers. We specifically chose to look at CRRs for cemented versus uncemented femoral stems for any reason and the specific indications of aseptic loosening and loosening related to wear/osteolysis to ascertain whether the transition to cementless stems was supported by lower revision rates in a community joint registry. The registry provides a unique glimpse into the community practice of arthroplasty, distinct from academic centers or larger national registries, which would allow us to answer this question as well as those related to patient age groupings and procedural timeframes.
Any joint registry study has inherent limitations. First, revision is a relatively crude outcome measure. We did not identify patients who may have been too medically infirm to undergo a revision procedure or who declined revision surgery despite a poor primary arthroplasty result. Additionally, the possibility exists that patients may have had revision surgery performed elsewhere, which would not be included in our study. We assumed these events occurred equally between the uncemented and cemented THA groups. Prior analysis of our registry suggests a 94% capture rate with only 6% of patients undergoing revision outside our capture [13], similar to the Scandinavian registries. The uncemented group had a higher percentage of young male patients, which increases revision risk, but shorter followup times resulting from the higher percentage performed in more recent timeframes. The CRR analyses and our regression model accounted for these differences. Finally, we made no attempt to account for the wide variety of bearing surfaces, polyethylene component thickness or shelf life, or sterilization methods that might contribute to wear and oxidative degradation of the polyethylene and, hence, osteolysis and subsequent stem failure. However, we did analyze stem survival in different timeframes to examine this potential effect. We also cannot account for different surgeons’ varying indications for when to use a cemented versus cementless stem, which might introduce selection bias that could influence these results. Despite these limitations, our registry offers a broad portrayal of modern total joint practice in a community setting.
We found that when all reasons for stem revision were considered, uncemented and cemented stems had comparable CRRs, but when age, sex, primary diagnosis, and procedural timeframe were included as confounders, cemented stems were at greater risk of revision. A 2010 study of the Swedish Hip Arthroplasty Register looking at revision-free component survival of THAs reported uncemented stems had a lower risk of stem revision for any reason [15]. However, the same registry reported in 2009 that uncemented prostheses underwent more revisions for periprosthetic fractures and intraoperative technical problems, whereas cemented prostheses had higher revision rates for loosening [12]. The 2011 report from the National Joint Registry for England and Wales found cemented THAs (cemented cup + cemented stem) to have lower revision rates with approximately half as many revisions at 7 years as uncemented THAs in patients younger than age 70 years. They suggest careful interpretation of these results, because patients in their registry with cemented THAs were more likely to be female, older, and in worse health than patients with uncemented THAs. Additionally, the relatively short-term followup of their study may underestimate any potential advantage of uncemented stems with respect to loosening. The authors did recommend all-cemented THA in patients older than age 70 years as a result of clear superiority in survivorship [27]. The Australian Orthopaedic Association National Joint Replacement Registry report from 2011, which also did not look specifically at stems, found hybrid THAs (uncemented cup + cemented stem) to have a lower CRR at 10 years than uncemented THAs (uncemented cups + uncemented stem) [14]. Importantly, the heterogeneity in the variables examined as well as some notable recalled design failures among uncemented THAs make the current registry data difficult to interpret. Overall, there does not appear to be compelling evidence in recent registry reports, including this one, to support the use of either cemented or cementless stems when all revision reasons are considered in the setting of stem failures alone.
Considering stem revisions performed specifically for aseptic loosening, wear, or osteolysis, our study found uncemented femoral stems to have less than half the CRR of cemented stems, mirroring other findings in the literature. In 2008 the Finnish Arthoplasty Register reviewed 50,968 primary THAs and found uncemented stems to have fewer revisions resulting from aseptic loosening than cemented stems at 10 and 15 years of followup [22]. A randomized controlled trial by Corten et al. [7] in 2011 likewise found cemented stems to have a 2.3 times increased risk of aseptic femoral stem revision (p = 0.002) at minimum 17-year followup. As noted earlier, this may reflect improvement in bearing surface longevity and decreased wear debris generation during the same timeframe as the increased use of uncemented stems.
Younger age has been associated with an increased risk of stem revision surgery in THA. In our study, patients < 70 years old with uncemented stems had significantly fewer revisions performed as a result of loosening, wear, or osteolysis than cemented stems. The Finnish Arthroplasty Register reported 0.5 times the risk for revision (95% CI, 0.3–0.7; p < 0.001) of extensively porous-coated stems compared with cemented stems for patients ≤ 55 years old [10]. Emerson et al. [9] retrospectively reviewed 180 THAs and found that although uncemented stems were implanted into a much younger, and presumably more active, cohort, these stems had 100% survival, compared with 84% survival of cemented stems, at 10 years of followup (p = 0.005). An analysis of the Norwegian registry looked at specific cementless designs compared with cemented stems. The authors found patients < 60 years with cemented stems to have a 6.8x greater risk (95% CI, 16–41; p < 0.001) for revision compared with hyaluronate acid-coated stems [16].
When looking at procedural timeframes in an attempt to account for some of the variation in bearing surfaces, the only significant difference in CRR was seen during 1999 to 2004, when uncemented stems had significantly fewer revisions for aseptic loosening or loosening associated with wear/osteolysis. Our lack of disparity in revision rates for the earlier time period, 1991 to 1998, might be attributed to problems associated with early uncemented stem designs such as a lack of circumferential coating, particularly when used with thin polyethylene liners [8, 16, 21, 29]. Our inability to show a significant difference in the CRR between uncemented and cemented designs in the most recent timeframe may reflect a diminished use of cemented stems in all but the most elderly and inactive patients, the increasing use of alternative bearing surfaces or less invasive approaches with uncemented designs, or some combination of these and other unexplored factors. The transition from cemented to uncemented femoral stems in North America is echoed in our registry with over 80% cemented stems inserted in 1996 contrasted to 3% in 2011. The reasons behind this change in practice are likely multifactorial.
In the setting of a 20-year community joint registry, we found comparable CRRs between cemented and uncemented stems when all reasons for revision were considered. When the focus was stem revisions performed specifically for aseptic loosening or loosening related to wear/osteolysis, uncemented stems demonstrated better survival in patients ≤ 70 years old. However, with a mean length of followup of only 6.5 years in the uncemented group, longer followup of this cohort in particular will be necessary to validate the results over time.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at HealthEast Hospitals, St Paul, MN, USA.
References
- 1.Berend ME. Cemented femoral fixation: a historical footnote. Orthopedics. 2006;29:791–792. doi: 10.3928/01477447-20060901-03. [DOI] [PubMed] [Google Scholar]
- 2.Berend ME, Smith A, Meding JB, Ritter MA, Lynch T, Davis K. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty. 2006;21(Suppl 2):53–59. doi: 10.1016/j.arth.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Campbell AC, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992;74:63–66. doi: 10.1302/0301-620X.74B1.1732268. [DOI] [PubMed] [Google Scholar]
- 5.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 6.Collis DK, Mohler CG. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Joint Surg Am. 2002;84:586–592. doi: 10.2106/00004623-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty? Minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011;469:209–217. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Nies F, Fidler MW. The Harris-Galante cementless femoral component: poor results in 57 hips followed for 3 years. Acta Orthop Scand. 1996;67:122–124. doi: 10.3109/17453679608994654. [DOI] [PubMed] [Google Scholar]
- 9.Emerson RH, Jr, Head WC, Emerson CB, Rosenfeldt W, Higgins LL. A comparison of cemented and cementless titanium femoral components used for primary total hip arthroplasty: a radiographic and survivorship study. J Arthroplasty. 2002;17:584–591. doi: 10.1054/arth.2002.32696. [DOI] [PubMed] [Google Scholar]
- 10.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0-22 years. Acta Orthop. 2005;76:28–41. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 11.Francis CW, Marder VJ, Evarts CM. Lower risk of thromboembolic disease after total hip replacement with non-cemented than with cemented prostheses. Lancet. 1986;1:769–771. doi: 10.1016/S0140-6736(86)91784-8. [DOI] [PubMed] [Google Scholar]
- 12.Garellick G, Karrholm J, Rogmark C, Herberts P. The Swedish Hip Arthroplasty Register. Annual Report 2009. Available at: http://www.shpr.se/Libraries/Documents/AnnualReport-2009-EN.sflb.ashx. Accessed February 5, 2012.
- 13.Gioe TJ, Killeen KK, Mehle S, Grimm K. Implementation and application of a community total joint registry: a twelve-year history. J Bone Joint Surg Am. 2006;88:1399–1404. doi: 10.2106/JBJS.E.01198. [DOI] [PubMed] [Google Scholar]
- 14.Graves S. Australian orthopaedic association national joint replacement registry. Hip and knee arthroplasty annual report 2011. Available at: http://www.surfacehippy.info/pdf/australian-nat-reg-2011.pdf . Accessed October 4, 2011.
- 15.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000;71:337–353. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 17.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Oh SW, Kim JS. Prevalence of fat embolism following bilateral simultaneous and unilateral total hip arthroplasty performed with or without cement: a prospective, randomized clinical study. J Bone Joint Surg Am. 2002;84:1372–1379. doi: 10.2106/00004623-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 20.Lane NE. Clinical practice. Osteoarthritis of the hip. N Engl J Med. 2007;357:1413–1421. doi: 10.1056/NEJMcp071112. [DOI] [PubMed] [Google Scholar]
- 21.Learmonth ID, Grobler GP, Dall DM, Jandera V. Loss of bone stock with cementless hip arthroplasty. J Arthroplasty. 1995;10:257–263. doi: 10.1016/S0883-5403(05)80171-8. [DOI] [PubMed] [Google Scholar]
- 22.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 23.Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. 2002;84:786–792. doi: 10.2106/00004623-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Pentlow AK, Heal JS. Subsidence of collarless uncemented femoral stems in total hips replacements performed for trauma. Injury. 2012;43:882–885. doi: 10.1016/j.injury.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 25.Pierannunzil LM. Thigh pain after total hip replacement: a pathophysiological review and a comprehensive classification. Orthopedics. 2008;31:691–699. doi: 10.3928/01477447-20110505-05. [DOI] [PubMed] [Google Scholar]
- 26.Pitto RP, Koessler M, Kuehle JW. Comparison of fixation of the femoral component without cement and fixation with use of a bone-vacuum cementing technique for the prevention of fat embolism during total hip arthroplasty. A prospective, randomized clinical trial. J Bone Joint Surg Am. 1999;81:831–843. doi: 10.2106/00004623-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Powers-Freeling L. National Joint Registry for England and Wales. 8th Annual Report 2011. Available at: http://www.njrcentre.org.uk/njrcentre/portals/0/documents/NJR%208th%20annual%20report%202011.Pdf. Accessed February 10, 2012.
- 28.Shah N, Porter M. Evolution of cemented stems. Orthopedics. 2005;28(Suppl):819–825. doi: 10.3928/0147-7447-20050802-04. [DOI] [PubMed] [Google Scholar]
- 29.Smith E, Harris WH. Increasing prevalence of femoral lysis in cementless total hip arthroplasty. J Arthroplasty. 1995;10:407–412. doi: 10.1016/S0883-5403(05)80138-X. [DOI] [PubMed] [Google Scholar]
- 30.Sochart DH, Porter ML. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Joint Surg Am. 1997;79:1599–1617. doi: 10.2106/00004623-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Sporer SM, Callaghan JJ, Olejniczak JP, Goetz DD, Johnston RC. The effects of surface roughness and polymethylmethacrylate precoating on the radiographic and clinical results of the Iowa hip prosthesis. A study of patients less than fifty years old. J Bone Joint Surg Am. 1999;81:481–492. doi: 10.1302/0301-620X.81B3.9140. [DOI] [PubMed] [Google Scholar]
- 32.Sylvain GM, Kassab S, Coutts R, Santore R. Early failure of a roughened surface, precoated femoral component in total hip arthroplasty. J Arthroplasty. 2001;16:141–148. doi: 10.1054/arth.2001.20541. [DOI] [PubMed] [Google Scholar]
- 33.Wroblewski BM, Siney PD. Charnley low-friction arthroplasty of the hip. Long-term results. Clin Orthop Relat Res. 1993;292:191–201. [PubMed] [Google Scholar]