Abstract
Background
Plantar fasciitis is the most common cause of heel pain. It may remain symptomatic despite conservative treatment with orthoses and analgesia. There is conflicting evidence concerning the role of extracorporeal shock wave therapy (ESWT) in the management of this condition.
Questions/purposes
We investigated whether there was a significant difference in the change of (1) VAS scores and (2) Roles and Maudsley scores from baseline when treated with ESWT and placebo. Specifically we compared overall improvement from baseline composite VAS, reduction in overall VAS pain, success rate of improving overall VAS pain by 60%, success rate of improving VAS pain by 60% when taking first steps, doing daily activities, and during application of a pain pressure meter.
Methods
MEDLINE, Embase, and CINAHL databases were searched from January 1980 to January 2013 and a double extraction technique was used to obtain relevant studies. Studies had to be prospective randomized controlled trials on adults and must not have used local anesthesia as part of their treatment protocol. Studies must have specifically recruited patients who continued to be symptomatic despite a minimum of 3 months of conservative treatments. All papers were assessed regarding their methodologic quality and a meta-analysis performed. Seven prospective randomized controlled trials were included in this study. There were 369 patients included in the placebo group and 294 in the ESWT group.
Results
After ESWT, patients had better composite VAS scores (random effects model, standardized mean difference [SMD] = 0.38; 95% CI, 0.05, 0.72; z = 2.27). They also had a greater reduction in their absolute VAS scores compared with placebo (random effects model, SMD = 0.60; 95% CI, 0.34, 0.85; z = 4.64). Greater success of improving heel pain by 60% was observed after ESWT when taking first steps (random effects model, risk ratio [RR] = 1.30; 95% CI, 1.04, 1.62; z = 2.29) and during daily activities (random effects model, RR = 1.44; 95% CI, 1.13, 1.84; z = 2.96). Subjective measurement of pain using a pressure meter similarly favored ESWT (random effects model, RR = 1.37, 95% CI, 1.06, 1.78; z = 2.41). There was a significant difference in the change to “excellent - good” Roles and Maudsley scores in favor of the ESWT group.
Conclusions
ESWT is a safe and effective treatment of chronic plantar fasciitis refractory to nonoperative treatments. Improved pain scores with the use of ESWT were evident 12 weeks after treatment. The evidence suggests this improvement is maintained for up to 12 months. We recommend the use of ESWT for patients with substantial heel pain despite a minimum of 3 months of nonoperative treatment.
Introduction
Plantar fasciitis the most common cause of heel pain [15]. It is usually a self-limiting condition and treated nonoperatively in the majority of patients [2, 3, 20]. However, 10% to 20% develop chronic pain and may require surgery [15]. Surgery may be associated with long recovery times, failure rates as much as 17%, and can be unpopular for patients who wish to continue weightbearing during recovery [1, 3, 5, 15].
Extracorporeal shock wave therapy (ESWT) has been proposed as a potential method of treating patients with chronic disease without the need to stop weightbearing [10, 16, 21, 22].
Rompe et al. [18] questioned the role of ESWT in acute disease; however, the role of ESWT in refractory chronic disease is still undetermined.
Therefore we investigated whether there was a significant difference in the change of (1) VAS scores and (2) Roles and Maudsley scores [14] from baseline when treated with ESWT and placebo. Specifically we compared overall improvement from baseline composite VAS, reduction in overall VAS pain, success rate of improving overall VAS pain by 60%, success rate of improving VAS pain by 60% when taking first steps, when doing daily activities, and during application of a pain pressure meter.
Search Strategy and Criteria
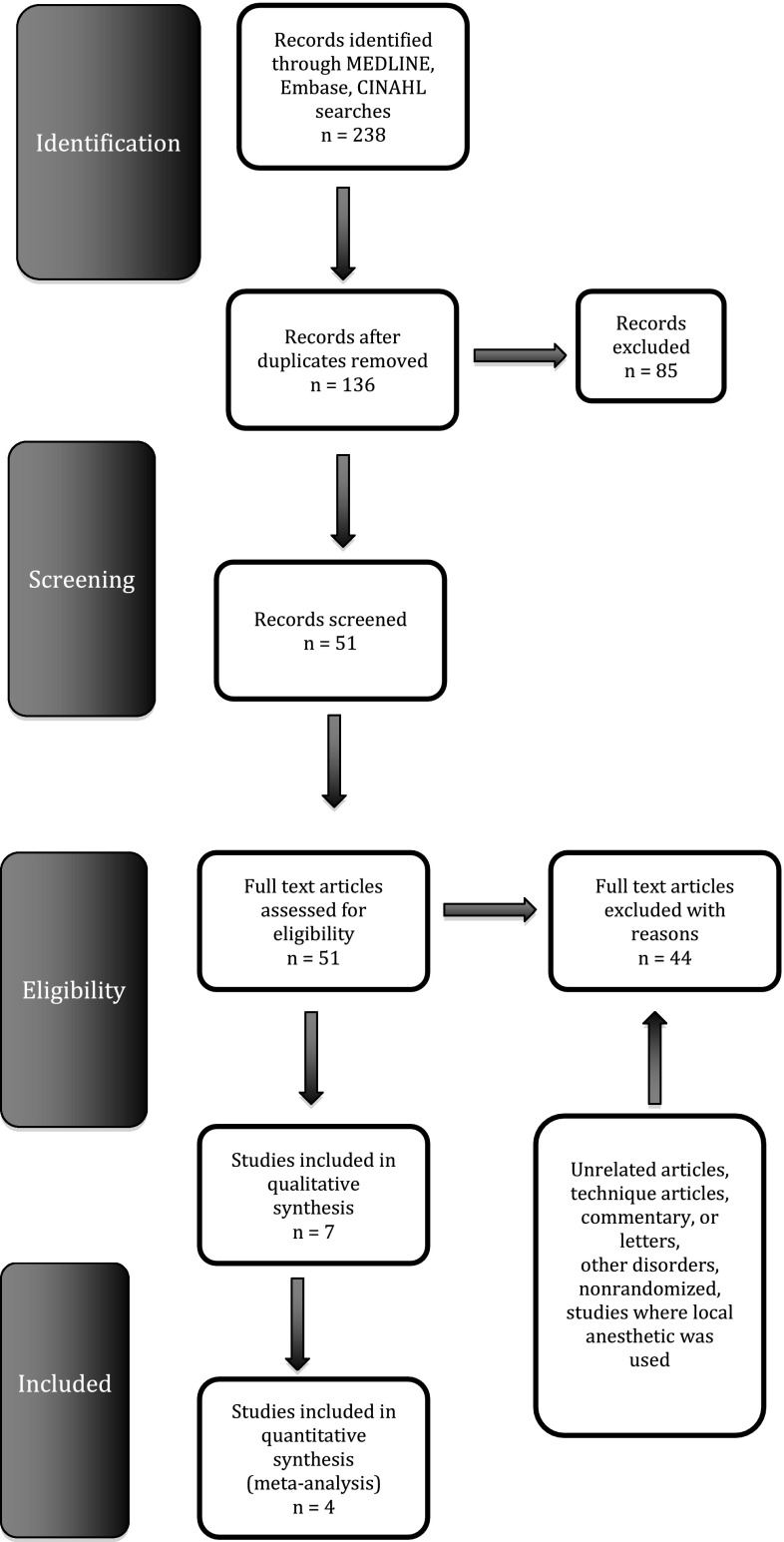
We searched the MEDLINE, Embase, and CINAHL databases to identify randomized controlled trials (RCTs) comparing ESWT without local anesthetic with placebo for the treatment of plantar fasciitis in adult patients between January 1980 and January 2013. The text words “plantar fasciitis,” “extracorporeal,” and “shock wave” were used in combination with the medical subject headings “plantar fasciopathy,” “heel pain syndrome,” “ESWT,” and “heel spur syndrome.” Irrelevant articles (ie, those failing to meet inclusion criteria), reviews, and meta-analyses evident from the titles and abstracts were excluded. Relevant articles referenced in these publications were obtained and the “related article” function was used to widen the results. No language restriction was applied. All abstracts, comparative studies, nonrandomized trials, and citations were searched comprehensively. This study conformed to QUOROM [12] and PRISMA guidelines [13]. A flowchart of the literature search is provided (Fig. 1). We screened 136 articles for relevance. On further scrutiny, we found seven RCTs meeting our inclusion criteria [6–8, 10, 11, 17, 20]. Each article was critically reviewed by two researchers (AA, MRSS) using a double-extraction method for eligibility. We included all prospective placebo-controlled RCTs whose patients had plantar fasciitis for a minimum of 3 months and had not responded to conservative treatment. Studies were excluded if local anesthesia was used as part of the treatment protocol. No language restriction was applied. Article extraction was performed independently and any conflict resolved before final analysis. The quality of included trials was rated using the Scottish Intercollegiate Guidelines Network scoring system [19] and the methods described by Jadad et al. (Table 1) [9].
Fig. 1.
The flowchart shows the process of study selection.
Table 1.
Methodologic qualities of prospective studies included
| Quality variable | Ibrahim et al. [8] (2010) | Gerdesmeyer et al. [6] (2008) | Gollwitzer et al. [7] (2007) | Malay et al. [10] (2006) | Speed et al. [20] (2003) | Rompe et al. [17] (2003) | Marks et al. [11] (2008) |
|---|---|---|---|---|---|---|---|
| Inclusion criteria | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Exclusion criteria | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Demographics comparable | 1 | 1 | 0 | 1 | 1 | 0 | 0 |
| Can the number of participating centers be determined? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Can the number of assessors be determined? | 1 | 0 | 0 | 0 | 0 | 1 | 1 |
| Can the reader determine where the assessor is on the learning curve for the reported procedure? | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Are diagnostic criteria clearly stated for clinical outcomes if required? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the treatment technique adequately described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is there any way that they have tried to standardize the technique? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is there any way that they have tried to standardize perioperative care? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the age and range given for patients in the ESWT group? | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Do the authors address whether there are any missing data? | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the age and range given for patients in the placebo group? | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Were patients in each group treated along similar timelines? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did all the patients asked to enter the study take part? | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Are dropout rates stated? | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| Are outcomes clearly defined? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Blinded assessors | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| Standardized assessment tools | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Analysis by intention to treat | 0 | 1 | 1 | 1 | 1 | 0 | 1 |
| Score | 16/20 | 14/20 | 16/20 | 16/20 | 16/20 | 16/20 | 16/20 |
Outcome measures were chosen if they were comparable to those of other papers. Outcomes focused on VAS scores for pain. The reduction in VAS pain composite scores, success rate of reducing VAS pain scores 60% at first steps, during daily activities, and Roles and Maudsley scores [14] were analyzed. The Roles and Maudsley score is an established subjective 4-point patient assessment of pain and limitations of activity (1 = excellent result with no symptoms following treatment; 2 = significant improvement from pretreatment; 3 = patient somewhat improved; 4 = poor, symptoms identical or worse than pretreatment) [14].
Seven RCTs comparing ESWT with placebo were identified from the electronic databases [6–8, 10, 11, 17, 20]. Three articles did not have comparable data and could not contribute to the quantitative analysis [11, 17, 20]. Characteristics of each trial are shown (Table 2). There were 369 patients in the ESWT group and 294 in the placebo group. The outcome measures extracted are shown (Table 3).
Table 2.
Treatment protocols for included studies
| Trial | Year | Type of treatment | Number of patients | Type of study | Nonoperative treatment time (months) | Local anesthetic used? | Shock waves administered | Number of sessions | Total number of impulses administered | EFD administered (mJ/mm2) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ibrahim et al. [8] | 2010 | ESWT | 25 | RCT | > 6 | No | Radial | 2 | 4000 | 0.16 |
| Placebo | 25 | |||||||||
| Gerdesmeyer et al. [6] | 2008 | ESWT | 125 | RCT | > 6 | No | Radial | 3 | 6000 | 0.16 |
| Placebo | 118 | |||||||||
| Marks et al. [11] | 2008 | ESWT | 16 | RCT | > 6 | No | NA | 3 | 4500 | 0.16 |
| Placebo | 9 | |||||||||
| Gollwitzer et al. [7] | 2007 | ESWT | 20 | RCT | > 6 | No | Focused | 3 | 6000 | 0.25 |
| Placebo | 20 | |||||||||
| Malay et al. [10] | 2006 | ESWT | 115 | RCT | > 6 | No | Radial | 1 | 3800 | NA |
| Placebo | 57 | |||||||||
| Rompe et al. [17] | 2003 | ESWT | 22 | RCT | > 12 | No | Focused | 3 | 6300 | 0.16 |
| Placebo | 23 | |||||||||
| Speed et al. [20] | 2003 | ESWT | 46 | RCT | > 3 | No | Focused | 3 | 4500 | 0.12 |
| Placebo | 42 |
EFD = energy flux density; ESWT = extracorporeal shock wave treatment; RCT = randomized controlled trial; NA = not available.
Table 3.
Outcome measures
| Study | Year | Type of treatment | Number of patients | Outcome measures | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| Ibrahim et al. [8] | 2010 | ESWT | 25 | 7.9 | 92%†
(n = 25) |
61.70% | ||||
| Placebo | 25 | 1.3 (p < 0.001) |
4%†
(n = 25) (p < 0.001) |
15.8% (p < 0.001) |
||||||
| Gerdesmeyer et al. [6] | 2008 | ESWT | 125 | 56% (SD, 39.3%) | 60.98% (n = 125) |
60.8% (n = 125) |
60% (n = 125) |
52.85 (n = 125) |
58.4 % (n = 125) |
|
| Placebo | 118 | 44.1% (SD, 41.8%) (p = 0.0220) |
42.24% (n = 118) (p = 0.002) |
48.31% (n = 118) (p = 0.0269) |
40.68% (n = 118) (p = 0.0014) |
39.66 (n = 118) (p = 0.0216) |
41.52% (n = 118) (p = 0.0031) |
|||
| Marks et al. [11] | 2008 | ESWT | 16 | |||||||
| Placebo | 9 | |||||||||
| Gollwitzer et al. [7] | 2007 | ESWT | 20 | 73.2%* (n = 20) |
55%* (n = 20) |
55%* (n = 20) |
50%* (n = 20) |
60%‡
(n = 20) |
60% (n = 20) |
|
| Placebo | 20 | 40.5%* (n = 20) (p = 0.0302) |
40%* (n = 20) (p = 0.2148) |
30%* (n = 20) (p = 0.0648) |
40%* (n = 20) (p = 0.3057) |
35%‡
(n = 20) (p = 0.0769) |
40% (n = 20) (p = 0.0416) |
|||
| Malay et al. [10] | 2006 | ESWT | 115 | 3.39 (n = 112) |
||||||
| Placebo | 57 | 1.78 (n = 56) (p < 0.001) |
||||||||
| Rompe et al. [17] | 2003 | ESWT | 22 | |||||||
| Placebo | 23 | |||||||||
| Speed et al. [20] | 2003 | ESWT | 46 | |||||||
| Placebo | 42 | |||||||||
1 = improvement in mean VAS composite scores (heel pain in the morning, doing daily activities, and application of dolorimeter) from baseline or mean % improvement (SD) after 12 weeks; 2 = reduction in mean VAS score (points) from baseline in participants’ assessment of heel pain at 12 weeks; 3 = success rate of heel pain improvement (> 60% reduction in VAS scores) at 12 weeks for at least two of three heel pain monitoring criteria; 4 = success rate of heel pain (> 60% reduction in VAS scores) when taking first steps in morning at 12 weeks; 5 = success rate of heel pain (> 60% reduction in VAS scores) while doing daily activities at 12 weeks; 6 = success rate of heel pain (> 60% reduction in VAS scores) after application of the dolorimeter at 12 weeks; 7 = reduction in Roles and Maudsley scores (excellent to good) at 12 weeks; * % median change not % mean change; †only one VAS score used; ‡F-meter used rather than a dolorimeter.
We performed statistical analyses using Review Manager Version 5.0 (The Nordic Cochrane Centre, Copenhagen, Denmark). A p value less than 0.05 was chosen as the significance level for outcome measures. For continuous data, the inverse variance method was used for the combination of standardized mean differences (SMDs). Binary data (success rate of achieving greater than 60% reduction in pain scores) were summarized as risk ratios (RR) and combined using the Mantel-Haenszel method. In each case, a heterogeneity test was performed and a random effects model was used for analyses. A random effects model was used uniformly across analyses for consistency and to deal with possible population heterogeneity. When SDs were not reported, they were estimated either from ranges or p values. Forest plots were used for the graphic display. Funnel plots were not constructed as they were deemed inappropriate with this number of studies.
We compared quantitative results from studies that quoted the percentage improvement in mean or median VAS score from baseline. We also compared percentage change in pain scores in trials using different pressure meters. The use of ESWT for treatment of plantar fasciitis is approved by the FDA.
Results
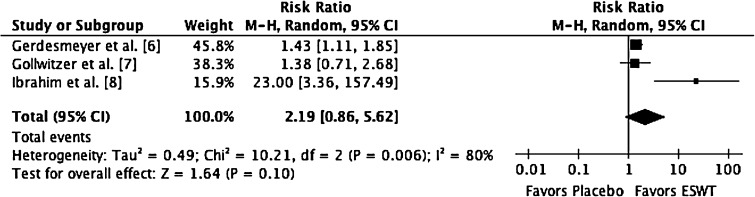
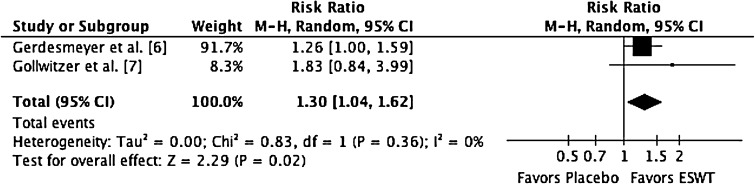
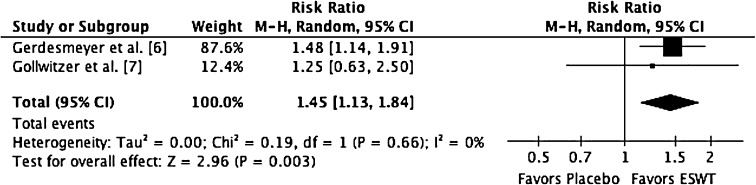
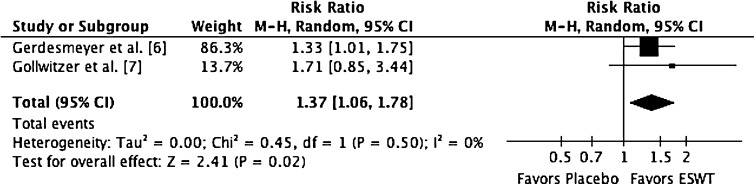
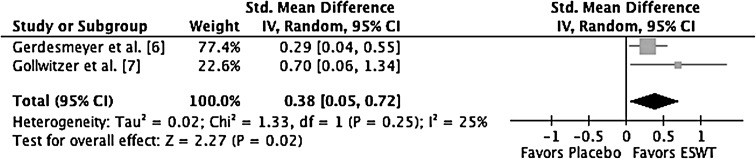
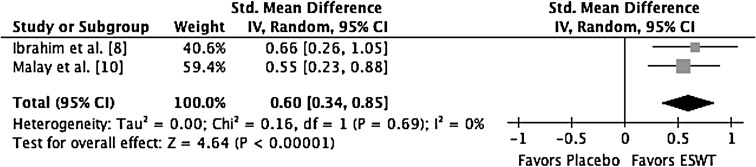
Two studies contributed to an analysis of the overall percentage improvement in mean VAS composite scores [6, 7]. There was no significant heterogeneity between these two trials (df = 1; I2 = 25; Q = 1.33; p = 0.25). After ESWT, patients had better composite pain scores after 12 weeks compared with placebo (random effects model, SMD = 0.38; 95% CI, 0.05, 0.72; z = 2.27; p = 0.02) (Fig. 2). Two studies reported on absolute reductions in VAS scores for heel pain [7, 9]. There was no significant heterogeneity between these two trials (df = 1; I2 = 0; Q = 0.00; p = 0.69). After ESWT, patients also had greater reduction in their VAS pain scores after 12 weeks compared with placebo (random effects model, SMD = 0.60; 95% CI, 0.34, 0.85; z = 4.64; p < 0.001) (Fig. 3). Three studies contributed to an analysis on overall success rate in heel pain improvement [5–7]. There was significant heterogeneity among trials (df = 2; I2 = 80; Q = 10.21; p < 0.01). There was no significant difference in overall success rate of heel pain improvement (> 60% reduction in two of three criteria) between ESWT without local anesthetic and placebo (random effects model, RR = 2.19; 95% CI, 0.86, 5.62; z = 1.64; p = 0.10) (Fig. 4). Two studies contributed to an analysis on the success rate of heel pain improvement when taking first steps [6, 7]. There was no significant heterogeneity between these two trials (df = 1; I2 = 0; Q = 0.83; p = 0.36). Pain was less after ESWT without local anesthetic compared with placebo (random effects model, RR = 1.30; 95% CI, 1.04, 1.62; z = 2.29; p < 0.02) (Fig. 5). Two studies contributed to the analysis of success rate of heel pain improvement while doing daily activities [6, 7]. There was no significant heterogeneity between these two trials (df = 1; I2 = 0; Q = 0.19; p = 0.66). Pain was less after ESWT without local anesthetic compared with placebo (random effects model, RR = 1.44; 95% CI, 1.13, 1.84; z = 2.96; p = 0.003) (Fig. 6). Two studies contributed to the analysis of the success rate of heel pain improvement after application of a pressure meter [6, 7]. There was no significant heterogeneity between these two trials (df = 1; I2 = 0; Q = 0.45; p = 0.50). Pain was less after ESWT without local anesthetic compared with placebo (random effects model, RR = 1.37; 95% CI, 1.06, 1.78; z = 2.41; p = 0.02) (Fig. 7).
Fig. 2.
This forest plot shows the overall percentage of improvement in mean VAS composite scores after 12 weeks. IV = inverse variance; Std. = standard; ESWT = extracorporeal shock wave therapy.
Fig. 3.
This forest plot shows the reduction in overall heel pain after 12 weeks. IV = inverse variance; Std. = standard; ESWT = extracorporeal shock wave therapy.
Fig. 4.
This forest plot shows the success rate of heel pain improvement when taking first steps after 12 weeks. M-H = Mantel-Haenszel; ESWT = extracorporeal shock wave therapy.
Fig. 5.
This forest plot shows the success rate of heel pain improvement when taking first steps after 12 weeks. M-H = Mantel-Haenszel; extracorporeal shock wave therapy.
Fig. 6.
This forest plot shows the success rate of heel pain improvement while doing daily activities after 12 weeks. M-H = Mantel-Haenszel; extracorporeal shock wave therapy.
Fig. 7.
This forest plot shows the success rate of heel pain improvement after application of pressure meter after 12 weeks. M-H = Mantel-Haenszel; ESWT = extracorporeal shock wave therapy.
Three studies contributed to the assessment [6–8]. As the data were not continuous, it was deemed more appropriate to discuss the results of the trials individually. At 12 weeks after treatment, authors of all three articles reported a significantly different change in “excellent to good” Roles and Maudsley scores in favor of the ESWT group.
Discussion
Plantar fasciopathy is usually self-limiting, but approximately 10% of patients still have symptoms despite treatment with nonsurgical measures [6]. Patients refractory to conservative measures often require surgery; however, this has been associated with long recovery times and potentially may result in longer periods off work and a delay to sporting activity [6]. Rompe et al. [18] questioned the role of ESWT in acute disease. This is the first meta-analysis focusing on patients with chronic disease. ESWT had favorable results in our analysis, with five of six outcome results reaching significance. Only one of the 12-week outcome results, “overall success rate of heel pain improvement”, did not reach significance. This might be a reflection of the lack of homogeneity among trials, as individually all three trials had results statistically favorable to the ESWT group. Longer-term followup data were not sufficient or comparable enough for meta-analysis; however, there have been encouraging results up to 12 months after treatment reported in individual articles. Ibrahim et al. [8] found a significant difference in the improvement of VAS heel pain scores at 24 weeks when comparing placebo with ESWT (100% versus 16% success; p < 0.001) in favor of ESWT. However, there were no other studies with the same outcomes to enable an analysis at this length of followup. Success rate in reducing VAS heel pain scores by 60% at 1-year followup also has favored ESWT (p = 0.0014) [6]. Mean reduction in patient self-assessment of pain on first walking in the morning also was found to be significantly better with ESWT compared with placebo (p < 0.0001) up to 1 year after treatment [17].
Speed et al. [20] concluded that there appeared to be no treatment effect of moderate-dose ESWT. Unfortunately, as the data presented in the paper were not comparable to others, it could not be included in the analysis. Of all the trials, it seems their trial was the only one not showing significantly favorable results after ESWT. There are two potential reasons for this. The followup of patients who had nonoperative treatment in their study was 3 months. Other studies included patients only if nonoperative treatment for 6 to 12 months failed (Table 2). Another potential reason is that the energy flux density administered in the study of Speed et al. [20] was the lowest of all the studies included. In a recent meta-analysis, Chang et al. [4] concluded that lower energy intensity shock waves are less effective.
There are some limitations to our study. First, the types of shock waves administered in the included trials were not the same. Some used focused waves whereas others used radial. The strength of the waves, number of shocks delivered, and time between treatments also varied among the trials. All but one of the outcome measures analyzed had no statistical heterogeneity between the trials included. As there seems to be agreement among included papers in their support of ESWT for treatment of chronic plantar fasciitis, the form of shock wave and treatment regime used may not be the most important factor for the improvement of symptoms. As analyses involved two to three studies, funnel plots were not deemed appropriate. Therefore the reader should be wary of the possibility of positive reporting bias when interpreting these results. Similarly, although the methodologic quality of included studies was good, the possibility exists that patients were not truly blinded to the treatment. As ESWT can be painful, subjects may have guessed which group they were in by the presence or absence of pain.
The main strengths of our review include the robust inclusion and exclusion criteria. Only including high scoring prospective RCTs added to the validity of the statistical results (Table 1). Including trials with patients with failed nonoperative treatments for a minimum of 3 months reduced the probability of a treatment appearing as effective when the patients would have recovered spontaneously. Excluding trials using local anesthetic also may have helped to reduce heterogeneity among compared trials.
Chang et al. [4] reported some of the controversies in using this form of treatment and provided recommendations on the most effective strengths of shock waves. However there still is no consensus or meta-analyses clarifying which type of shock waves (radial or focused) are more effective. There is lack of evidence on the length of effectiveness of this treatment and longer followup data are required. Future analyses could compare types of shock waves and report longer-term data. The evidence presented here may lead to financial savings by avoiding less effective measures and may result in less time off work or a shorter time away from sport. Future studies could quantify the potential savings of using ESWT compared with nonoperative measures with time and explore effectiveness of treatment when local anesthetic field blocks were used.
After reviewing our results with this meta-analysis, we believe that patients with chronic plantar fasciitis will be treated more effectively by ESWT without a local anesthetic than with a placebo. We recommend ESWT be used for patients not improving after 3 months of other nonoperative measures.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Imperial College London, Charing Cross Campus, London, UK.
References
- 1.ACFAS Clinical Practice Guideline Heel Pain Panel The diagnosis and treatment of heel pain. J Foot Ankle Surg. 2001;40:329–340. doi: 10.1016/S1067-2516(01)80071-5. [DOI] [PubMed] [Google Scholar]
- 2.Atkins D, Crawford F, Edwards J, Lambert M. A systematic review of treatments for the painful heel. Rheumatology (Oxford). 1999;38:968–973. doi: 10.1093/rheumatology/38.10.968. [DOI] [PubMed] [Google Scholar]
- 3.Buchbinder R. Clinical practice: plantar fasciitis. N Engl J Med. 2004;350:2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 4.Chang KV, Chen SY, Chen WS, Tu YK, Chien KL. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2012;93:1259–1268. doi: 10.1016/j.apmr.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003;3:CD000416. doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 6.Gerdesmeyer L, Frey C, Vester J, Maier M, Weil L, Jr, Weil L, Sr, Russlies M, Stienstra J, Scurran B, Fedder K, Diehl P, Lohrer H, Henne M, Gollwitzer H. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med. 2008;36:2100–2109. doi: 10.1177/0363546508324176. [DOI] [PubMed] [Google Scholar]
- 7.Gollwitzer H, Diehl P, von Korff A, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg. 2007;46:348–537. doi: 10.1053/j.jfas.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Ibrahim MI, Donatelli RA, Schmitz C, Hellman MA, Buxbaum F. Chronic plantar fasciitis treated with two sessions of radial extracorporeal shock wave therapy. Foot Ankle Int. 2010;31:391–397. doi: 10.3113/FAI.2010.0391. [DOI] [PubMed] [Google Scholar]
- 9.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 10.Malay DS, Pressman MM, Assili A, Kline JT, York S, Buren B, Heyman ER, Borowsky P, LeMay C. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg. 2006;45:196–210. doi: 10.1053/j.jfas.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. Extracorporeal shock-wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain: a double blind randomised controlled trial. Acta Orthop Belg. 2008;74:98–101. [PubMed] [Google Scholar]
- 12.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. QUOROM Group. Br J Surg. 2000;87:1448–1454. doi: 10.1046/j.1365-2168.2000.01610.x. [DOI] [PubMed] [Google Scholar]
- 13.PRISMA. Transparent Reporting of Systematic Reviews and Meta-Analyses. Available at: http://www.prisma-statement.org/statement.htm. Accessed November 23, 2012.
- 14.Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972;54:499–508. [PubMed] [Google Scholar]
- 15.Rompe JD. Plantar fasciopathy. Sports Med Arthrosc. 2009;17:100–104. doi: 10.1097/JSA.0b013e3181a3d60e. [DOI] [PubMed] [Google Scholar]
- 16.Rompe JD, Buch M, Gerdesmeyer L, Haake M, Loew M, Maier M, Heine J. Musculoskeletal shock wave therapy: current database of clinical research][in German. Z Orthop Ihre Grenzgeb. 2002;140:267–274. doi: 10.1055/s-2002-32477. [DOI] [PubMed] [Google Scholar]
- 17.Rompe JD, Decking J, Schoellner C, Nafe B. Shock wave application for chronic plantar fasciitis in running athletes: a prospective, randomized, placebo-controlled trial. Am J Sports Med. 2003;31:268–275. doi: 10.1177/03635465030310021901. [DOI] [PubMed] [Google Scholar]
- 18.Rompe JD, Furia J, Weil L, Maffulli N. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007;81–82:183–208. doi: 10.1093/bmb/ldm005. [DOI] [PubMed] [Google Scholar]
- 19.SIGN. Methodology checklist 1: systematic reviews and meta-analyses. Available at: http://www.sign.ac.uk/guidelines/fulltext/50/checklist1.html. Accessed November 23, 2012.
- 20.Speed CA, Nichols D, Wies J, Humphreys H, Richards C, Burnet S, Hazleman BL. Extracorporeal shock wave therapy for plantar fasciitis: a double blind randomised controlled trial. J Orthop Res. 2003;21:937–940. doi: 10.1016/S0736-0266(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 21.Theodore GH, Buch M, Amendola A, Bachmann C, Fleming LL, Zingas C. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int. 2004;25:290–297. doi: 10.1177/107110070402500503. [DOI] [PubMed] [Google Scholar]
- 22.Weil LS, Jr, Roukis TS, Weil LS, Borrelli AH. Extracorporeal shock wave therapy for the treatment of chronic plantar fasciitis: indications, protocol, intermediate results, and a comparison of results to fasciotomy. J Foot Ankle Surg. 2002;41:166–172. doi: 10.1016/S1067-2516(02)80066-7. [DOI] [PubMed] [Google Scholar]