Abstract
Background
Advances in the surgical treatment of musculoskeletal conditions have resulted in an interest in better defining and understanding patients’ expectations of these procedures, but the best ways to do this remain a topic of considerable debate.
Questions/purposes
(1) What validated instruments for the assessment of patient expectations of orthopaedic surgery have been used in published studies to date? (2) How were these expectation measures developed and validated? (3) What unvalidated instruments for the assessment of patient expectations have been used in published studies to date?
Methods
A systematic literature search was performed using the OVID Medline and EMBASE databases, in duplicate, to identify all studies that assessed patient expectations in orthopaedic surgery. Sixty-six studies were ultimately included in the present review.
Results
Seven validated expectation instruments were identified, all of which use patient-reported questionnaires. Five were specific to a particular procedure or affected anatomic location, whereas two were broadly applicable. Details of reliability and validity testing were available for all but one of these instruments. Forty additional unvalidated expectation assessment tools were identified. Thirteen were based on existing clinical outcome tools, and the others were study-specific, custom-developed tools. Only one of the unvalidated tools was used in more than one study.
Conclusions
Several validated expectation instruments have been developed for use by patients undergoing orthopaedic surgery. However, many tools have been reported without evidence of testing and validation. The wide range of untested instruments used in single studies substantially limits the interpretation and comparison of data concerning patient expectations.
Introduction
There have been marked improvements in the elective surgical treatment of musculoskeletal conditions over the past half century. Advances in the development of implantable medical devices including hardware and prostheses and improvements in surgical techniques have resulted in predictable structural and clinical results in the treatment of a number of previously debilitating conditions [29, 41]. Procedures such as hip and knee arthroplasty were initially developed with the goal of providing pain relief and some improvement in mobility in profoundly debilitated patients [6, 21]. However, as experience with elective orthopaedic procedures has grown and the populations deemed to be candidates for surgery have expanded [7], defining successful surgery similarly has evolved, most notably with greater weight attached to patient-reported outcomes and satisfaction [49]. Several authors have reported strong associations between fulfillment of patient expectations of orthopaedic surgery and postoperative satisfaction [4, 8, 47, 58, 60]. This has led to increasing interest among surgeons and researchers in better defining and understanding patients’ expectations of orthopaedic procedures with a goal of optimizing patient selection and preoperative education to ultimately influence patient satisfaction.
Patient expectations are a potentially complex and dynamic quality that can be difficult to define, measure, and analyze. For instance, patient expectations may vary depending on when in the course of care they are measured (before surgery, postoperatively, or at full recovery), by different diagnoses (such as malignant versus nonmalignant processes), and by anatomic location or patient age (eg, anterior cruciate ligament surgery in teens or THA in octogenarians). Second, as described by Saban and Penckofer [54] and Kravitz [26], expectations may be defined in at least two dimensions. They can be probabilistic reflecting the perceived likelihood of a particular outcome or event or value-based based on the importance attached to a particular outcome or event. Thus, a vast array of specific expectations may be held by patients, complicating the development of instruments and scores that would allow their quantification and comparison. Further complexity arises from the potential for many personal and contextual factors to influence expectations [26].
The purpose of the present study was to systematically review the published literature to answer the following questions: (1) What validated tools for the assessment of patient expectations of orthopaedic surgery have been used in published studies to date? (2) How were these expectation measures developed and validated? (3) What unvalidated instruments for the assessment of patient expectations have been used in published studies to date?
Materials and Methods
Search Strategy and Criteria
A manual electronic search of the OVID Medline and EMBASE databases, encompassing all included reports until the end of October 2012, was performed by two of the authors (MGZ, AM) to identify studies that assessed patient expectations with respect to orthopaedic surgery. The search was performed in duplicate with any disagreements in eligibility resolved by consensus discussion with all authors. The following search string was used limited to citation titles and abstracts: “(((orthopedic* or orthopaedic* or ((hip or knee or shoulder or elbow or ankle or spine or spinal or lumbar or cervical or hand or wrist) and (surgeon or surgery or replacement or arthroplasty))) and (expectation or expectations))”. One thousand seven hundred seventy-one records were identified with 1036 remaining after automated deduplication was performed using the OVID search interface.
Study Selection
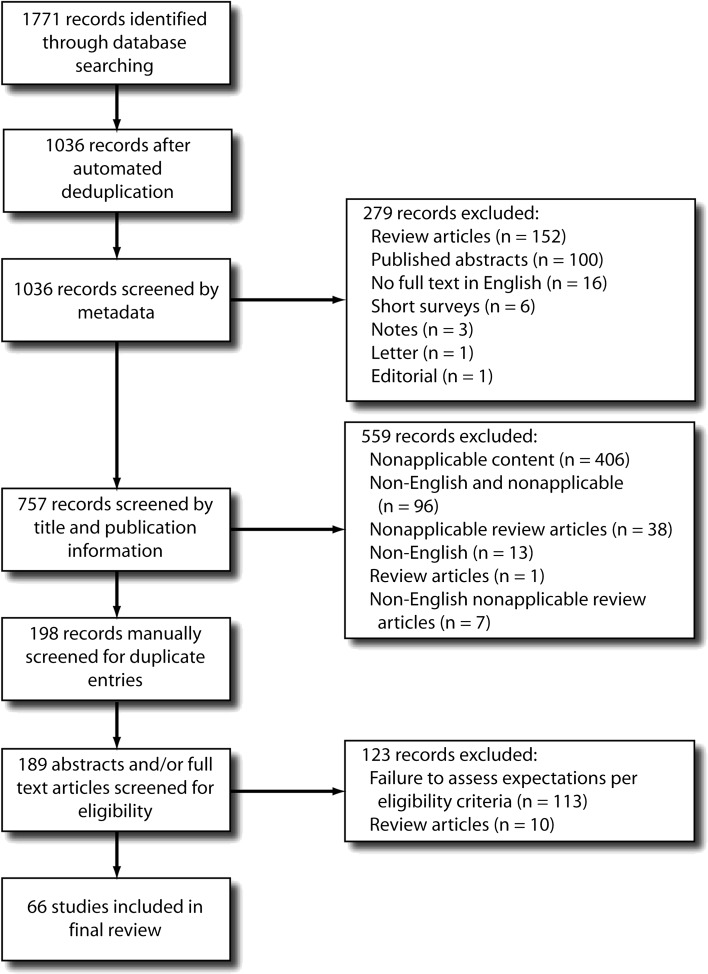
Citation records were extracted to Excel spreadsheet software (Microsoft Corp, Redmond, WA, USA) and sorted by publication-type metadata. No specialized systematic review software packages were used. Publication types not meeting our inclusion criteria were discarded (Fig. 1). Specifically, 100 abstracts, one letter, three notes, 152 review papers, six short surveys, one editorial, and 16 manuscripts with only abstracts published in English were discarded, leaving 757 records. The titles of these records were reviewed to further identify studies not meeting eligibility criteria with a further 559 studies excluded. These studies were excluded for the following reasons: not applicable based on the title alone (for example, did not report on patients with orthopaedic diagnoses = 406 records); non-English manuscripts concerning nonapplicable subject matter (96 records); review articles concerning nonapplicable subject matter (38 records); non-English manuscripts (11 records); review articles (one record); and non-English review articles concerning nonapplicable subject matter (seven records). The remaining 198 records were manually screened for duplicate entries with nine duplicate records identified and removed. All abstracts of the remaining 189 records were read by two reviewers (MGZ, AM). No systematic search of article bibliographies or conference proceedings was performed in an attempt to identify any additional unpublished or otherwise unidentified data. Full-length articles of abstracts that were considered as probably relevant or of unknown relevance were obtained and screened to definitively identify those studies that met our eligibility criteria described previously with 66 reports included in the final review.
Fig. 1.
A systematic search strategy was used to identify the studies included in the present review as summarized in this flow diagram.
Eligibility Criteria
Original studies of human subjects who (1) either underwent or were considered eligible for orthopaedic surgery for musculoskeletal conditions and (2) were assessed at any point during the study period concerning their expectations of any portion of the care cycle were included for review. We limited eligibility to studies that assessed patient expectations using either a probabilistic (ie, likelihood of a given outcome) or value-based (ie, importance attached to a given outcome) definition, which are the most commonly used descriptions in the context of medical care [26, 54]. In contradistinction, any assessment methods that exclusively investigated beliefs (premises held to be true by an individual), needs (outcomes perceived as necessary, irrespective of likelihood), or desires (outcomes or situations wanted by the respondent irrespective of perceived likelihood of attainment) were not included.
Review articles, letters to the editor, published abstracts, and case studies or reports concerning less than 10 patients were excluded. Additionally, only reports with full-text versions published in English were eligible for this review.
Because patient expectations are complex and multidimensional, any studies that assessed only a single patient expectation predetermined by the study authors (for example, expected time off work after surgery) or that limited their query to a single global assessment of whether expectations were met after surgery (for example, did surgery meet your expectations?) were excluded. Furthermore, to limit the review to measures of patient expectations, any studies that queried patients about their expectations through an exclusively qualitative approach, for example open-ended questioning without any subsequent structured categorization of responses, were also excluded.
Data Collection
Data extraction included the following elements: (1) study features, including year of publication and study design; (2) study population features, including number of patients, orthopaedic diagnosis(es), and surgical intervention(s); and (3) details of expectations assessment, including scoring methodology used, assessment time period(s), and information concerning score development and validation either directly from the study text or, if appropriate, from referenced studies describing these details.
Study Designs and Populations
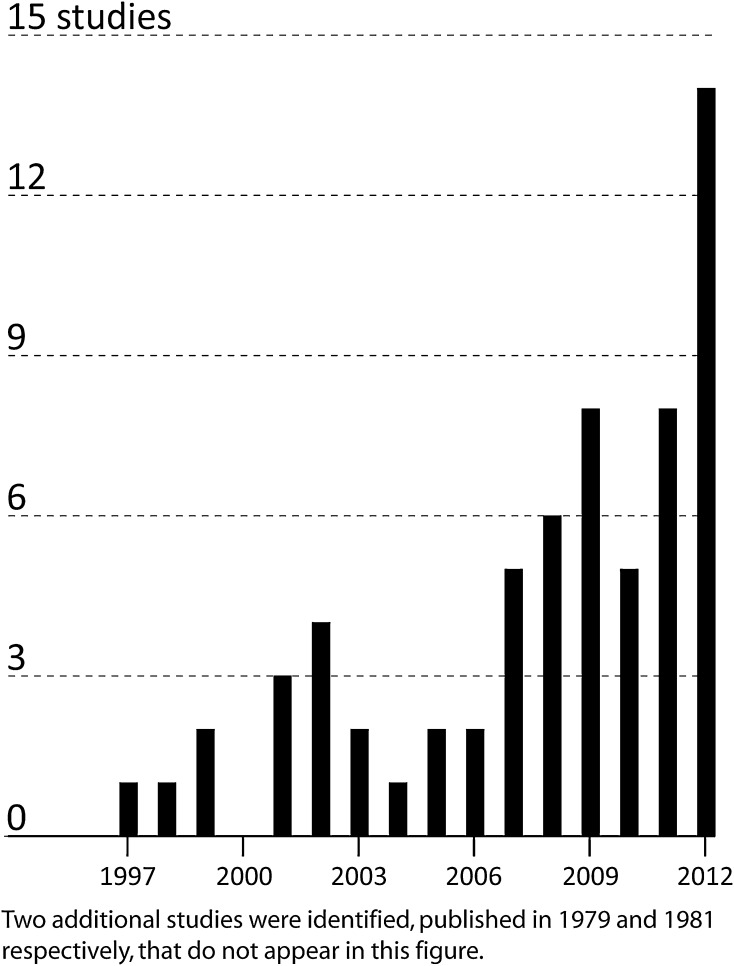
In general, there was an increasing frequency of studies assessing patient expectations over time (Fig. 2). Although the earliest study identified was from 1979, almost two-thirds of identified studies (41 of 66) were published within the last 5 years. A number of different study designs were identified. Forty studies (61%) had a prospective cohort design, assessing patients both pre- and postoperatively at multiple time points. Twenty-two studies had a cross-sectional design, of which 13 (20%) assessed patient expectations preoperatively and seven (11%) assessed patient expectations subsequent to surgical treatment. Finally, six studies (9%) had a retrospective cohort design, assessing patients at multiple time points through retrospective review of prospectively collected data.
Fig. 2.
The number of studies assessing patient expectations in orthopaedic surgery has increased steadily over the past 15 years.
Patient expectations concerning a range of different orthopaedic procedures were identified (Table 1). However, the majority of reports (36 of 66 [55%]) concerned either THA or TKA. An additional 18% of reports (12 of 66) investigated patients who underwent spine surgery, and 12% (eight of 66) reported on patients who underwent shoulder surgery. The remaining 10 studies (15%) reported on a variety of other surgical procedures. Although the large majority of studies were focused on specific procedures or pathologies, seven (11%) combined potentially disparate procedures into a single group (for example, orthopaedic day surgery or foot surgery).
Table 1.
Distribution of studies using expectation instruments by surgical procedure
| Orthopaedic diagnosis or procedure | Number of studies | Percent of total |
|---|---|---|
| THA | 8 | 12% |
| Revision THA | 2 | 3% |
| TKA | 11 | 17% |
| Revision THA | 1 | 2% |
| THA or TKA | 14 | 21% |
| Anterior cruciate ligament reconstruction or knee arthroscopy | 1 | 2% |
| Knee arthroscopy | 1 | 2% |
| Knee surgery | 1 | 2% |
| Lumbar spine surgery | 8 | 12% |
| Lumbar discectomy | 2 | 3% |
| Spine surgery | 2 | 3% |
| Total shoulder arthroplasty | 1 | 2% |
| Rotator cuff repair | 4 | 6% |
| Rotator cuff decompression/repair | 2 | 3% |
| Shoulder surgery | 1 | 2% |
| Hallux valgus correction | 1 | 2% |
| Foot surgery | 1 | 2% |
| Carpal tunnel release | 2 | 3% |
| Metacarpophalangeal joint arthroplasty | 1 | 2% |
| Hand surgery | 1 | 2% |
| Orthopaedic day surgery | 1 | 2% |
| Total | 66 | 100% |
Results
Expectation Measures for Which Development and Validity Data Are Available
Seven measures assessing patient expectations of orthopaedic surgery were identified for which the process of development was described and validity work undertaken (Table 2). These include the Hospital for Special Surgery (HSS) Expectations Surveys for the following procedures: knee arthroplasty, hip arthroplasty, nonarthroplasty knee surgery, and shoulder surgery [34, 36, 37]; the Expectations Domain of the New Knee Society Scoring System [48, 59]; the Expectations Domain of the Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) Instruments [62]; and the Sunnybrook Surgery Expectations Survey [50]. Each of the scores is specific to a particular surgical procedure or anatomic location except for the MODEMS scale and Sunnybrook score, which have been reported to not be joint- or procedure-specific [50, 62]. In all cases the tools are administered as a patient-completed questionnaire with between three and 20 items each graded with response items ranging between 3 and 5 points. All of these instruments assess patient expectations for the domains of pain and physical function with the HSS, MODEMS, and Sunnybrook scores additionally querying social factors and the HSS scores further probing psychological elements. Although the HSS scores assess value-based expectations (ie, the importance of various items after surgery and recovery), the remaining scores are probability-based (asking the perceived most likely status in terms of queried domains after surgery and recovery).
Table 2.
Validated instruments for the assessment of patient expectations
| Assessment tool | Applicable patients | Administration method | Features assessed | Type of expectation | Number of items | Item scoring method |
|---|---|---|---|---|---|---|
| HSS Knee Surgery Expectations Survey | Nonarthroplasty knee surgery | Self-administered questionnaire | Pain, physical function, social, psychological | Value-based | 20 | Adjectival items (5 categories) |
| HSS Knee Replacement Expectations Survey | Knee arthroplasty | Self-administered questionnaire | Pain, physical function, social, psychological | Value-based | 17 | Adjectival items (5 categories) |
| HSS Shoulder Surgery Expectations Survey | Shoulder surgery | Self-administered questionnaire | Pain, physical function, social, psychological | Value-based | 17 | Adjectival items (5 categories) |
| HSS Hip Replacement Expectations Survey | Hip arthroplasty | Self-administered questionnaire | Pain, physical function, social, psychological | Value-based | 18 | Adjectival items (5 categories) |
| New Knee Society Score - Expectations Domain | Knee arthroplasty | Self-administered questionnaire | Pain, physical function | Probability-based | 3 | Adjectival items (5 categories) |
| MODEMS Questionnaire - Expectations Domain | Range of musculoskeletal conditions | Self-administered questionnaire | Pain, physical function, social | Probability-based | 6 | Adjectival items (5 categories) |
| Sunnybrook Surgery Expectations Score | Orthopaedic surgery | Self-administered questionnaire | Pain, physical function, social | Probability-based | 6 | Adjectival items (4 or 5 categories) |
| Assessment tool | Source of items | Source of instrument contents | Test-retest reliability assessed? | Construct validity assessment | Content validity assessment | Criterion validity assessment | Reference |
|---|---|---|---|---|---|---|---|
| HSS Knee Surgery Expectations Survey | Patient-derived | Open-ended patient interviews | Yes (κ ≥ 0.40 for all items) | Compared with age, sex, education level, functional status | Use of patient interviews, expert review | Compared with AAOS-LLC, SF-36 | [37] |
| HSS Knee Replacement Expectations Survey | Patient-derived | Open-ended patient interviews | Yes (κ ≥ 0.40 for all items) | Compared with age, sex, education level, functional status | Use of patient interviews, expert review | Compared with AAOS-LLC, SF-36 | [37] |
| HSS Shoulder Surgery Expectations Survey | Patient-derived | Open-ended patient interviews | Yes (κ ≥ 0.40 for all items) | Compared with age, sex, education level, functional status | Use of patient interviews, expert review | Compared with SRQ, SF-36 | [34] |
| HSS Hip Replacement Expectations Survey | Patient-derived | Open-ended patient interviews | Yes (κ ≥ 0.40 for all items) | Compared with age, sex education level, functional status | Use of patient interviews, expert review | Compared with AAOS-LLC, SF-36 | [36] |
| New Knee Society Score - Expectations Domain | Unclear | Expert opinion | Unreported | Tested using exploratory factor analysis | Expert review | Compared with SF-12, KOOS | [48, 59] |
| MODEMS Questionnaire - Expectations Domain | Unclear | Unreported | Unreported | Details not reported | Details not reported | Details not reported | [62] |
| Sunnybrook Surgery Expectations Score | Unclear | Literature review + expert opinion | Unreported | Compared with age, sex | Literature review and expert opinion | Compared with SF-36 | [50] |
HSS = Hospital for Special Surgery; MODEMS = Musculoskeletal Outcomes Data Evaluation and Management System; SRQ = L’Insalata Shoulder Rating Questionnaire; KOOS = Knee Injury and Osteoarthritis Outcome Score.
How Were the Expectation Measures Developed and Validated?
The four HSS Expectation Surveys were all developed and validated by the same principal investigator using similar methodology and thus will be described in aggregate (Table 2) [34, 36, 37]. These questionnaires were developed using patient interviews and expert review with only items with moderate reliability or greater (Cohen’s kappa ≥ 0.40) in the draft survey retained for the final instrument. Content validity was established through the use of patient interviews and expert review to inform item selection, and concurrent criterion validity was confirmed by comparison to a number of previously validated patient-reported measures.
The Sunnybrook Surgery Expectations Score was developed based on a literature review and expert opinions with the intention of not being joint-specific [50]. No further information was identified concerning rationale for the selection of the specific items included in this tool. Test-retest reliability was ascertained on a sample of 25 patients awaiting shoulder surgery with at least moderate correlation for all survey items [50]. The investigator who developed this tool reported construct and concurrent criterion validity for the expectation score when compared with demographic factors and physical and mental component SF-36 scores [50]. The investigator has also reported use of this tool in patients undergoing rotator cuff repair [51].
The MODEMS expectations scale is a six-item instrument included as a domain in a number of different musculoskeletal assessment instruments and was developed as part of the now defunct MODEMS project spearheaded by the American Academy of Orthopaedic Surgeons [55, 62]. Good internal consistency (Cronbach’s alpha = 0.71) and test-retest reliability (Cohen’s kappa = 0.91) were demonstrated for an earlier version of this expectations scale included as part of the North American Spine Society Lumbar Spine Outcome Assessment Instrument [9], although the response options were subsequently changed from value to probability-based selections. All MODEMS questionnaires have been reported to be tested and validated [55], although we were not able to identify specific published information on the results of this process for the final version of the expectations scale.
The New Knee Society Scoring System was recently developed in an attempt to provide an updated outcome instrument for patients undergoing knee arthroplasty, encompassing both objective and subjective measures [59]. Separate but related versions of this instrument were developed for use before and after knee arthroplasty with the former including a patient expectations domain. A task force of members of the Knee Society created a draft instrument with the expectations domain modified from a questionnaire previously reported by Mahomed et al. [33]. The survey was refined through two phases of assessment (101 and 497 patients in each phase, respectively) on patients who either underwent primary unilateral TKA or were scheduled to do so. Construct and criterion validity were assessed as part of the development process, and the final version of the expectations domain was found to have good internal validity (Cronbach’s alpha = 0.79) [48].
Expectation Measures for Which Development and Validity Data Are Not Available
Several other methods of assessment of patient expectations were reported. These included: existing clinical assessment tools modified to assess expectations, custom tools developed specifically to assess patient expectations, and open-ended verbal or written assessments.
Thirteen different clinical assessment tools modified for the evaluation of expectations were identified (Table 3) [2, 13, 15, 19, 23, 25, 33, 39, 40, 43, 44, 46, 61, 65]. All of the modified instruments were designed for self-administration by patients. Excluding the modified Total Hip Arthroplasty Outcome Evaluation Questionnaire [13, 33, 40, 65], all of the instruments were only used in a single study identified in our review.
Table 3.
Clinical scores modified for the assessment of patient expectations
| Clinical outcome score used | Summary of modifications | Administration method | Type of expectation | Number of items | Item scoring method | Studies reporting its use | Published by investigators independent of those who originally modified the score | References |
|---|---|---|---|---|---|---|---|---|
| WOMAC | Question stems modified to query anticipated status 6 months after surgery | Self-administered questionnaire | probability-based | 24 | Adjectival items (4 categories) | Haddad et al. (2001) | N | [15] |
| Oxford Knee Score | Question stems modified to query anticipated status 6 months after surgery | Self-administered questionnaire | probability-based | 12 | Adjectival items (5 categories) | Moran et al. (2003) | N | [43] |
| Oxford Hip Score | Question stems modified to query anticipated status 6 months after surgery | Self-administered questionnaire | probability-based | 12 | Adjectival items (5 categories) | Moran et al. (2003) | N | [43] |
| QuickDASH | Question stems modified to query anticipated status once maximally recovered from surgery | Self-administered questionnaire | probability-based | 11 | Adjectival items (5 categories) | Hudak et al. (2004) | N | [19] |
| DASH | Question stems modified to query anticipated status after surgery (specific time period not specified) | Self-administered questionnaire | probability-based | 30 | Adjectival items (5 categories) | Kadzielski et al. (2008) | N | [25] |
| NAAS Lumbar Spine Questionnaire | Modification of questionnaire items and response options to query anticipated change in status as a result of surgery | Self-administered questionnaire | Probability-based | 8 | Skewed Likert items (5 categories) | Mannion et al. (2009) | N | [39] |
| KOOS | Patients queried concerning anticipated status for each of 5 KOOS domains as well as walking ability and leisure activities | Self-administered questionnaire | Probability-based | 7 | Adjectival and Likert items (5 to 7 categories) | Nilsdotter et al. (2009) | N | [46] |
| International Knee Documentation Committee Subjective Knee Form | Items used to inform a new questionnaire querying importance of changes in status as a result of surgery | Self-administered questionnaire | Value-based | 15 | Adjectival items (5 categories) | Becker et al. (2011) | N | [2] |
| Historical Leisure Activity Questionnaire | Question stems modified to query anticipated status 12 months after surgery | Self-administered questionnaire | Probability-based | 36 | Open-ended responses concerning frequency of activity participation | Jones et al. (2012) | N | [23] |
| Functional Questionnaire of Hannover for Osteoarthritis | Response options changed to query expectations of future status | Self-administered questionnaire | Probability-based | 18 | 3 response options | Suda et al. (2010) | N | [61] |
| Knee Society Pain Score | Question stem modified to query expected status 6 months after surgery | Self-administered questionnaire | Probability-based | 1 | 7 response options | Muniesa et al. (2010) | N | [44] |
| Total Hip Arthroplasty Outcome Evaluation Questionnaire | Two or three questions from 26-item questionnaire extracted, with variable modifications through addition of 0 to 2 questions and change in response options | Self-administered questionnaire | Probability-based | 3 or 4 | Combined open-ended, adjectival, limited response option, and VAS | Mahomed et al. (2002) Venkataramanan et al. (2006) Gandhi et al. (2009) Mannion et al. (2009) |
Y | [13, 33, 40, 65] |
| Schedule of the Individual Quality of Life-Direct Weights | Modified to query estimated satisfaction 3 months postoperatively for each of 5 domains selected by respondent as most important to their quality of life | Self-administered questionnaire | Value and probability-based | 5 | 10 centimeter VAS | Saban and Penckofer (2007) | N | [54] |
NB = no data concerning reliability or validity testing were reported for any of these scores when used in modified form for the assessment of patient expectations; DASH = Disabilities of the Arm, Shoulder and Hand; NASS = North American Spine Society; KOOS = Knee injury and Osteoarthritis Outcome Score; VAS = visual analog scale.
Twenty studies used custom questionnaires developed by the authors to assess patient expectations without any explicit description of the methodology, rationale, or source instrument behind their development [3, 5, 10, 12, 14, 16, 20, 22, 27, 28, 30–32, 45, 52, 53, 57, 64, 66, 68]. These questionnaires consisted of between two and 45 items, most frequently querying expectations regarding factors such as residual pain, degree of mobility, activities of daily living, recreational/social activities, ability to work, and complications. One study asked patients to pick from supplied lists of potential surgical complications and activities that the patient would be able to do postoperatively [28]. All of the questionnaires were self-completed by patients on paper. No two studies were found to use identical questionnaires.
Seven studies used patient interviews or open-ended self-response questions as a definitive assessment tool [1, 11, 18, 35, 38, 42, 67]. In all cases, the responses were subsequently categorized and grouped for analysis.
Discussion
The topic of patient expectations in orthopaedic surgery has recently become a particular focus of interest with the majority of reports on this subject published within the past 5 years. Given these recent additions to the knowledge in the field, the present review was undertaken in an attempt to identify the expectation assessment instruments used to date.
We acknowledge several limitations of the present study. First, despite the use of an accepted inclusive search strategy and careful staged review and assessment of results, it is possible that we have nevertheless failed to identify one or more patient expectation assessment instruments. This could be because the expectations tool has not been described in a peer-reviewed article indexed by the searched databases or was otherwise not captured by our search strategy. Second, although we carefully reviewed the full-text versions of all included studies, including any relevant additional articles referenced within these reports, it is possible that one of the expectations assessment tools was erroneously identified as not being tested or validated. This could be because of a failure of our search strategy to identify published reports of the development and/or testing of one or more of the included instruments. Additionally, given the systematic review methodology used, the findings of the present study can only be based on published material. However, given the large number of citations reviewed and the substantial number of tools identified in the present study, we believe nevertheless that we have identified expectations tools that accurately reflect the breadth of different instruments used to date.
We identified several reliable and validated instruments for the assessment of patient expectations of orthopaedic surgery. Both generic tools applicable to a wide range of musculoskeletal conditions and instruments specific to a particular anatomic location or intervention were documented. One instrument (the MODEMS Expectations Scale) appears to have been largely abandoned because of a failure to attract sufficient surgeons to contribute to a centralized data tracking registry [55]. The experience with the MODEMS initiative provided important lessons in terms of developing simple and user-friendly data collection methods, minimizing participant time burden, including rigorous quality control measures, and planning for financial sustainability, which are now being applied to the American Joint Replacement Registry [56]. However, the use of the HSS Expectation Surveys has recently been reported in several clinical studies from nonoriginating investigators [17, 24, 58, 63], which may potentially allow for comparison of patient expectations and their association with other clinical variables between different populations and studies. Additionally, the recent inclusion of an expectations domain in the New Knee Society Score further promises to expand opportunities for the investigation of this variable in patients undergoing TKA [48, 59]. However, although it has been recognized that patient expectations can be assessed using dimensions of values (states considered to be more or less important) or probabilities (states considered to be more or less likely) [26, 54], all of the validated instruments reported to date are limited to a single one of these two domains.
Unfortunately, the majority of studies identified in the present review used instruments that lacked adequate description of the development methodology or any evidence of testing and validation. Although many of these instruments may actually be effective, discriminative, and user-friendly in assessing patient expectations, the orthopaedic community should strive to confirm and publish the reliability and validity of these instruments. With 47 different expectation tools identified, and only five used by more than one group of investigators, it is virtually impossible to compare data concerning expectations between different studies. Combined, these factors substantially limit surgeons’ and researchers’ ability to critically appraise and compare the published studies to date. With the relationship between fulfillment of patient expectations and increased satisfaction well documented [4, 8, 47, 58, 60], these factors may ultimately be restricting opportunities for maximizing patient satisfaction after orthopaedic care. For these reasons, leadership from the orthopaedic community is needed to encourage the use of a limited number of high-quality, standardized instruments for the measurement of patient expectations.
The present review revealed that although there are several validated instruments for the assessment of patient expectations, a large number of primarily unvalidated tools continue to be used with few instruments used in more than one study. The use of valid, common, and comparable instruments is critical to the advancement of the understanding of patient expectations and their relationship to a range of demographic, clinical, and surgical factors. Of the scores reported to date, the HSS Expectations Surveys have been used in the greatest number of studies, although they are limited to the assessment of value-based expectations. Other instruments that measure probability-based expectations have been reported although with limited clinical use. Unless there is a compelling reason to do otherwise, researchers should consider the use of existing validated scores when assessing patient expectations concerning orthopaedic care. Ultimately, a limited number of carefully selected expectation assessment instruments must be defined, promoted, and adopted by orthopaedic surgeons and investigators to maximize their use. Given the known positive relationships between the fulfillment of patient expectations and satisfaction with orthopaedic surgical procedures, the use of high-quality expectation assessment instruments is critical to the optimization of patient care.
Footnotes
One or more of the authors (MGZ) serves on the editorial board of Expert Review of Medical Devices. One of the authors certifies that she (AM), or a member of her immediate family, has or may receive payments or benefits, during the study period, an amount of amount of less than USD 10,000 from Smith & Nephew, Inc (Memphis, TN, USA) and an amount of less than USD 10,000 from Biomet (Warsaw, IN, USA). One of the authors certifies that he (NNM), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Smith & Nephew and an amount of less than $10,000 from Biomet.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Abbott AD, Hedlund R, Tyni-Lenne R. Patients’ experience post-lumbar fusion regarding back problems, recovery and expectations in terms of the International Classification of Functioning, Disability and Health. Disabil Rehabil. 2011;33:1399–1408. doi: 10.3109/09638288.2010.533240. [DOI] [PubMed] [Google Scholar]
- 2.Becker R, Doring C, Denecke A, Brosz M. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1433–1441. doi: 10.1007/s00167-011-1621-y. [DOI] [PubMed] [Google Scholar]
- 3.Becker SJ, Makanji HS, Ring D. Expected and actual improvement of symptoms with carpal tunnel release. J Hand Surg Am. 2012;37:1324–1329 e1321–1325. [DOI] [PubMed]
- 4.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton KE, Wright V, Richards J. Patients’ expectations in relation to outcome of total hip replacment surgery. Ann Rheum Dis. 1979;38:471–474. doi: 10.1136/ard.38.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charnley J. Arthroplasty of the hip. A new operation. Lancet. 1961;7187:1129–1132. doi: 10.1016/S0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 7.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. doi: 10.1097/01.blo.0000188066.01833.4f. [DOI] [PubMed] [Google Scholar]
- 8.Culliton SE, Bryant DM, Overend TJ, MacDonald SJ, Chesworth BM. The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty. 2012;27:490–492. doi: 10.1016/j.arth.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine (Phila Pa 1976). 1996;21:741–749. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 10.de Beer J, Petruccelli D, Adili A, Piccirillo L, Wismer D, Winemaker M. Patient perspective survey of total hip vs total knee arthroplasty surgery. J Arthroplasty. 2012;27:865–869.e861–865. [DOI] [PubMed]
- 11.de Groot KI, Boeke S, Passchier J. Preoperative expectations of pain and recovery in relation to postoperative disappointment in patients undergoing lumbar surgery. Med Care. 1999;37:149–156. doi: 10.1097/00005650-199902000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Eisler T, Svensson O, Tengstrom A, Elmstedt E. Patient expectation and satisfaction in revision total hip arthroplasty. J Arthroplasty. 2002;17:457–462. doi: 10.1054/arth.2002.31245. [DOI] [PubMed] [Google Scholar]
- 13.Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty. 2009;24:716–721. doi: 10.1016/j.arth.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez Saenz de Tejada M, Escobar A, Herrera C, Garcia L, Aizpuru F, Sarasqueta C. Patient expectations and health-related quality of life outcomes following total joint replacement. Value Health. 2010;13:447–454. doi: 10.1111/j.1524-4733.2009.00685.x. [DOI] [PubMed] [Google Scholar]
- 15.Haddad FS, Garbuz DS, Chambers GK, Jagpal TJ, Masri BA, Duncan CP. The expectations of patients undergoing revision hip arthroplasty. J Arthroplasty. 2001;16:87–91. doi: 10.1054/arth.2001.17937. [DOI] [PubMed] [Google Scholar]
- 16.Haworth RJ, Hopkins J, Ells P, Ackroyd CE, Mowat AG. Expectations and outcome of total hip replacement. Rheumatol Rehabil. 1981;20:65–70. doi: 10.1093/rheumatology/20.2.65. [DOI] [PubMed] [Google Scholar]
- 17.Henn RF, 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93:2110–2115. doi: 10.2106/JBJS.J.01114. [DOI] [PubMed] [Google Scholar]
- 18.Hobbs N, Dixon D, Rasmussen S, Judge A, Dreinhofer KE, Gunther KP, Dieppe P. Patient preoperative expectations of total hip replacement in European orthopedic centers. Arthritis Care Res (Hoboken). 2011;63:1521–1527. doi: 10.1002/acr.20596. [DOI] [PubMed] [Google Scholar]
- 19.Hudak PL, Hogg-Johnson S, Bombardier C, McKeever PD, Wright JG. Testing a new theory of patient satisfaction with treatment outcome. Med Care. 2004;42:726–739. doi: 10.1097/01.mlr.0000132394.09032.81. [DOI] [PubMed] [Google Scholar]
- 20.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in ‘willingness’ to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 21.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173–180. [PubMed] [Google Scholar]
- 22.Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns. 1998;34:169–178. doi: 10.1016/S0738-3991(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 23.Jones DL, Bhanegaonkar AJ, Billings AA, Kriska AM, Irrgang JJ, Crossett LS, Kwoh CK. Differences between actual and expected leisure activities after total knee arthroplasty for osteoarthritis. J Arthroplasty. 2012;27:1289–1296. doi: 10.1016/j.arth.2011.10.030. [DOI] [PubMed] [Google Scholar]
- 24.Jourdan C, Poiraudeau S, Descamps S, Nizard R, Hamadouche M, Anract P, Boisgard S, Galvin M, Ravaud P. Comparison of patient and surgeon expectations of total hip arthroplasty. PLoS One. 2012;7:e30195. doi: 10.1371/journal.pone.0030195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kadzielski J, Malhotra LR, Zurakowski D, Lee SG, Jupiter JB, Ring D. Evaluation of preoperative expectations and patient satisfaction after carpal tunnel release. J Hand Surg Am. 2008;33:1783–1788. doi: 10.1016/j.jhsa.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 26.Kravitz RL. Patients’ expectations for medical care: an expanded formulation based on review of the literature. Med Care Res Rev. 1996;53:3–27. doi: 10.1177/107755879605300101. [DOI] [PubMed] [Google Scholar]
- 27.Lattig F, Fekete TF, O’Riordan D, Kleinstuck FS, Jeszenszky D, Porchet F, Mutter U, Mannion AF. A comparison of patient and surgeon pre-operative expectations of spinal surgery. Spine (Phila Pa 1976). 2012 Jul 20 [Epub ahead of print]. [DOI] [PubMed]
- 28.Lavernia CJ, Contreras JS, Parvizi J, Sharkey PF, Barrack R, Rossi MD. Do patient expectations about arthroplasty at initial presentation for hip or knee pain differ by sex and ethnicity? Clin Orthop Relat Res. 2012;470:2843–2853. doi: 10.1007/s11999-012-2431-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 30.Lingard EA, Sledge CB, Learmonth ID. Patient expectations regarding total knee arthroplasty: differences among the United States, United kingdom, and Australia. J Bone Joint Surg Am. 2006;88:1201–1207. doi: 10.2106/JBJS.E.00147. [DOI] [PubMed] [Google Scholar]
- 31.Lurie JD, Berven SH, Gibson-Chambers J, Tosteson T, Tosteson A, Hu SS, Weinstein JN. Patient preferences and expectations for care: determinants in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 2008;33:2663–2668. doi: 10.1097/BRS.0b013e31818cb0db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999;14:740–744. doi: 10.1046/j.1525-1497.1999.10417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 34.Mancuso CA, Altchek DW, Craig EV, Jones EC, Robbins L, Warren RF, Williams-Russo P. Patients’ expectations of shoulder surgery. J Shoulder Elbow Surg. 2002;11:541–549. doi: 10.1067/mse.2002.126764. [DOI] [PubMed] [Google Scholar]
- 35.Mancuso CA, Salvati EA, Johanson NA, Peterson MG, Charlson ME. Patients’ expectations and satisfaction with total hip arthroplasty. J Arthroplasty. 1997;12:387–396. doi: 10.1016/S0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- 36.Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty. J Arthroplasty. 2003;18:872–878. doi: 10.1016/S0883-5403(03)00276-6. [DOI] [PubMed] [Google Scholar]
- 37.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RF, Williams-Russo P. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83:1005–1012. doi: 10.1302/0301-620X.83B7.12105. [DOI] [PubMed] [Google Scholar]
- 38.Mandl LA, Burke FD, Shaw Wilgis EF, Lyman S, Katz JN, Chung KC. Could preoperative preferences and expectations influence surgical decision making? Rheumatoid arthritis patients contemplating metacarpophalangeal joint arthroplasty. Plast Reconstr Surg. 2008;121:175–180. doi: 10.1097/01.prs.0000295376.70930.7e. [DOI] [PubMed] [Google Scholar]
- 39.Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine (Phila Pa 1976). 2009;34:1590–1599. doi: 10.1097/BRS.0b013e31819fcd52. [DOI] [PubMed] [Google Scholar]
- 40.Mannion AF, Kampfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther. 2009;11:R139. doi: 10.1186/ar2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matter P. History of the AO and its global effect on operative fracture treatment. Clin Orthop Relat Res. 1998;347:11–18. doi: 10.1097/00003086-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 42.McHugh GA, Luker KA. Individuals’ expectations and challenges following total hip replacement: a qualitative study. Disabil Rehabil. 2012;34:1351–1357. doi: 10.3109/09638288.2011.644022. [DOI] [PubMed] [Google Scholar]
- 43.Moran M, Khan A, Sochart DH, Andrew G. Expect the best, prepare for the worst: surgeon and patient expectation of the outcome of primary total hip and knee replacement. Ann R Coll Surg Engl. 2003;85:204–206. doi: 10.1308/003588403321661415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muniesa JM, Marco E, Tejero M, Boza R, Duarte E, Escalada F, Caceres E. Analysis of the expectations of elderly patients before undergoing total knee replacement. Arch Gerontol Geriatr. 2010;51:e83–e87. doi: 10.1016/j.archger.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 45.Niemeyer P, Porichis S, Salzmann G, Südkamp NP. What patients expect about autologous chondrocyte implantation (ACI) for treatment of cartilage defects at the knee joint. Cartilage. 2012;3:13–19. doi: 10.1177/1947603511415840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80:55–61. doi: 10.1080/17453670902805007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 48.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, Chadha P, Daylamani DA, Scott WN, Bourne RB. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Novak EJ, Vail TP, Bozic KJ. Advances in orthopaedic outcomes research. J Surg Orthop Adv. 2008;17:200–203. [PubMed] [Google Scholar]
- 50.Razmjou H, Finkelstein JA, Yee A, Holtby R, Vidmar M, Ford M. Relationship between preoperative patient characteristics and expectations in candidates for total knee arthroplasty. Physiother Can. 2009;61:38–45. doi: 10.3138/physio.61.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Razmjou H, Lincoln S, Axelrod T, Holtby R. Factors contributing to failure of rotator cuff surgery in persons with work-related injuries. Physiother Can. 2008;60:125–133. doi: 10.3138/physio.60.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ronnberg K, Lind B, Zoega B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine (Phila Pa 1976). 2007;32:256–261. doi: 10.1097/01.brs.0000251876.98496.52. [DOI] [PubMed] [Google Scholar]
- 53.Rosenberger PH, Jokl P, Cameron A, Ickovics JR. Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy. 2005;21:562–569. doi: 10.1016/j.arthro.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 54.Saban KL, Penckofer SM. Patient expectations of quality of life following lumbar spinal surgery. J Neurosci Nurs. 2007;39:180–189. doi: 10.1097/01376517-200706000-00009. [DOI] [PubMed] [Google Scholar]
- 55.Saleh KJ, Bershadsky B, Cheng E, Kane R. Lessons learned from the hip and knee musculoskeletal outcomes data evaluation and management system. Clin Orthop Relat Res. 2004;429:272–278. doi: 10.1097/01.blo.0000137589.23853.61. [DOI] [PubMed] [Google Scholar]
- 56.Saleh KJ, Goldberg MJ. Joint registries and the lessons learned from MODEMS. American Academy of Orthopaedic Surgeons Bulletin. February 2004.
- 57.Schneider W, Knahr K. Surgery for hallux valgus. The expectations of patients and surgeons. Int Orthop. 2001;25:382–385. doi: 10.1007/s002640100289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94:974–981. doi: 10.1302/0301-620X.94B7.28219. [DOI] [PubMed] [Google Scholar]
- 59.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society Knee Scoring System. Clin Orthop Relat Res. 2012;470:3–19. doi: 10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Soroceanu A, Ching A, Abdu W, McGuire K. Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: a multicenter study. Spine (Phila Pa 1976). 2012;37:E103–E108. doi: 10.1097/BRS.0b013e3182245c1f. [DOI] [PubMed] [Google Scholar]
- 61.Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010;33:76–80. doi: 10.3928/01477447-20100104-07. [DOI] [PubMed] [Google Scholar]
- 62.Tashjian RZ, Bradley MP, Tocci S, Rey J, Henn RF, Green A. Factors influencing patient satisfaction after rotator cuff repair. J Shoulder Elbow Surg. 2007;16:752–758. doi: 10.1016/j.jse.2007.02.136. [DOI] [PubMed] [Google Scholar]
- 63.Tekin B, Unver B, Karatosun V. Expectations in patients with total knee arthroplasty. Acta Orthop Traumatol Turc. 2012;46:174–180. doi: 10.3944/AOTT.2012.2655. [DOI] [PubMed] [Google Scholar]
- 64.Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. Patients’ expectations and satisfaction in lumbar spine surgery. Spine (Phila Pa 1976). 2005;30:2689–2694. doi: 10.1097/01.brs.0000187876.14304.15. [DOI] [PubMed] [Google Scholar]
- 65.Venkataramanan V, Gignac MA, Mahomed NN, Davis AM. Expectations of recovery from revision knee replacement. Arthritis Rheum. 2006;55:314–321. doi: 10.1002/art.21856. [DOI] [PubMed] [Google Scholar]
- 66.Vissers MM, de Groot IB, Reijman M, Bussmann JB, Stam HJ, Verhaar JA. Functional capacity and actual daily activity do not contribute to patient satisfaction after total knee arthroplasty. BMC Musculoskelet Disord. 2010;11:121. doi: 10.1186/1471-2474-11-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wilkinson AN, Maher AJ. Patient expectations of podiatric surgery in the United Kingdom. J Foot Ankle Res. 2011;4:27. doi: 10.1186/1757-1146-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466:1154–1161. doi: 10.1007/s11999-008-0194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]