Abstract
Background:
Obstructive sleep apnea (OSA) has been associated with increased frequency of excessive daytime sleepiness (EDS). Increased plasma TNF-α levels may mediate this association in adults, but conflicting results have been reported in children. We hypothesized that: (i) the higher the OSA severity in childhood, the higher the frequency of EDS and morning plasma TNF-α levels; and (ii) high TNF-α levels predict presence of EDS.
Methods:
Children without and with snoring underwent polysomnography. EDS was determined by parental response to specific questions, and plasma TNF-α levels were measured.
Results:
Children with moderate-to-severe OSA (n = 24; 5.7 ± 2 years; apnea-hypopnea index [AHI] 11.5 ± 5.1/h), but not participants with mild OSA (n = 22; 6 ± 2.5 years; AHI 2.1 ± 1/h) were at significantly higher risk for EDS than controls (n = 22; 6.8 ± 2.1 years; AHI 0.5 ± 0.3/h) (OR [95% CI] adjusted for age, gender, and obesity: 9.2 [1.7-50.2] and 3.8 [0.7-21.8], respectively). The 3 groups did not differ regarding TNF-α concentration (0.63 ± 0.2 vs 0.65 ± 0.18 vs 0.63 ± 0.17 pg/mL; P > 0.05). TNF-α levels were associated significantly with body mass index z-score (P < 0.05) and not with polysomnography indices (P > 0.05). Subjects with high TNF-α levels (> 0.57 pg/mL) were not at higher risk for EDS than participants with low levels (OR [95% CI] adjusted for age, gender, and obesity: 1.7 [0.5-5.7]).
Conclusions:
Increasing severity of OSA is associated with increasing frequency of EDS, but not with elevated plasma TNF-α concentration. High TNF-α levels cannot be used as predictor for the presence of EDS in children with sleep apnea.
Citation:
Alexopoulos EI; Theologi V; Malakasioti G; Maragozidis P; Tsilioni I; Chrousos G; Gourgoulianis K; Kaditis AG. Obstructive sleep apnea, excessive daytime sleepiness, and morning plasma TNF-α levels in Greek children. SLEEP 2013;36(11):1633-1638.
Keywords: Excessive daytime sleepiness, sleep apnea, tumor necrosis factor-alpha
INTRODUCTION
Excessive daytime sleepiness (EDS) is one of the most common morbid consequences of obstructive sleep apnea (OSA) and obesity in adults.1 In the initial pediatric reports, EDS was considered an infrequent symptom associated with sleep apnea and more emphasis was given to the presence of hyperactive behavior.2 However, in recent studies that were based on parental responses to questionnaires or objective testing (multiple sleep latency test), it was demonstrated that EDS may affect up to 50% of children with OSA.3–7
Increased tumor necrosis factor-α (TNF-α) plasma levels promote sleepiness and fatigue in adults with sleep apnea,1 but conflicting results have been reported in children.8–13 TNF-α concentration was associated with both OSA severity and EDS in only two of the few published pediatric reports.11,13 Nevertheless, in these two studies, much higher plasma levels of the cytokine were measured compared to previous publications.
Hence, the purpose of the present investigation was to clarify: (i) the potential association between severity of OSA and EDS; (ii) the reported correlation between severity of OSA and TNF-α plasma levels; and (iii) the role of TNF-α plasma levels as risk factor for EDS in children with sleep apnea. We hypothesized that: (i) the higher the severity of OSA in children, the higher the frequency of EDS and morning plasma TNF-α levels; and (ii) subjects with high TNF-α levels are more likely to have EDS.
METHODS
Participants
Consecutive children (2-13 years old) referred to the sleep disorders laboratory for polysomnography due to history of snoring and adenotonsillar hypertrophy and with AHI > 1 episode/h (OSA) were enrolled in the study. Healthy subjects without snoring who were recruited from the community and had AHI ≤ 1 episode/h were included as controls. Exclusion criteria for both patients and controls were: (i) symptoms or signs of acute or chronic inflammatory disorders; (ii) genetic syndromes; and (iii) neuromuscular disorders or cranio-facial abnormalities. The study was approved by the Institutional Review Board of the Larissa University Hospital, and informed consent was provided by the caregivers and assent by children with age 7 years or older.
Clinical Evaluation and Polysomnography
A detailed history was received from parents and all participants underwent physical examination. To evaluate the presence of EDS, 2 questions from the Pediatric Sleep Questionnaire (PSQ) were used: “Does your child have a problem with sleepiness during the day?” and “Has a teacher or other supervisor commented that your child appears sleepy during the day”?14 All parents were questioned about the number of hours of nocturnal sleep that their children usually received. Weight and standing height were recorded and body mass index (BMI) z-score was calculated.15 Obesity was defined as BMI z-score > 1.645.16 After direct inspection of the oropharynx, tonsillar size was graded from 1+ to 4+; tonsillar hypertrophy was diagnosed if size was > 2+.17
Overnight polysomnography was carried out in the sleep disorders laboratory, bedtime was determined by each child's routine and polysomnography was terminated upon final awakening. The Alice 4 computerized system (Philips-Respironics; Murrysville, PA) was used to record the following signals: 4-channel electroencephalogram (F4-M1, C4-M1, O2-M1, O1-M2); 2-channel electrooculogram (E1-M2, E2-M2); submental (3 electrodes) and tibial electromyogram; electrocardiogram (lead II); body position; oxygen saturation of hemoglobin by pulse oximetry ([SpO2] Nonin Medical; Plymouth, MN); and airflow and respiratory movements. Airflow was detected by thermocouple at the nose and mouth (Pro-Tech; Philips-Respironics) and by nasal pressure transducer (Pro-Tech; Philips-Respironics), and respiratory movements were monitored using thoracic and abdominal belts (piezoelectric transducers; Pro-Tech; Philips-Respironics).
Sleep stages and respiratory events were scored, and polysomnography indices were calculated according to the American Academy of Sleep Medicine recent recommendations.18 Respiratory arousals were defined as those occurring within 3 sec following an apnea, hypopnea, or snore.19 Apnea-hypopnea index (AHI) was the mean number of obstructive, central, and mixed apneas and hypopneas per hour of total sleep time.
Measurement of Morning Plasma TNF-α Concentration
A morning venous blood sample was collected from each participant in a test tube containing EDTA, was immediately centrifuged for 15 min at 1,000 × g, and the supernatant (plasma) was aliquoted and stored at -70°C. Samples were not subjected to freeze-thaw cycles and were assayed for TNF-α within 2 weeks after collection.11,20,21 A commercial ELISA kit (Human UltraSensitive ELISA kit; Invitrogen [formerly BioSource Europe]; Camarillo, CA) with a sensitivity of 0.09 pg/mL, an intra-assay coefficient of variation of 6.7%, and an inter-assay coefficient of variation of 9.7% was used.
Primary Outcome Measures, Explanatory Variables, and Data Analysis
Primary outcome measures of this study were: (i) EDS and (ii) morning plasma TNF-α levels. EDS was defined by a positive response to ≥ 1 of 2 PSQ questions. High TNF-α levels were those exceeding the median value in the control subjects. Severity of OSA was the main explanatory variable and was graded as: (i) no snoring and AHI ≤ 1 episode/h (controls); (ii) snoring and AHI > 1 and ≤ 5 episodes/h (mild OSA); and (iii) AHI > 5 episodes/h (moderate-to-severe OSA).
The 3 groups of participants (controls, mild OSA, and moderate-to-severe OSA) were compared with respect to age, gender, frequency of obesity and tonsillar hypertrophy, polysomnography indices, reported duration of nocturnal sleep, frequency of positive responses to the PSQ questions, and morning plasma TNF-α concentrations, using χ2 test (categorical characteristics) or one-way analysis of variance (continuous variables) followed by post hoc (Bonferroni) tests. Since EDS (outcome measure) is a categorical variable, univariate logistic regression analysis was used to calculate odds ratios (OR) and the corresponding 95% confidence intervals (CI) for the presence of EDS according to severity of OSA (dependent variable) or according to high or low TNF-α levels (dependent variable). Hence, OSA severity and TNF-α levels were treated as categorical characteristics. Multivariate logistic regression analysis was applied to adjust OR for age, gender, and obesity.
Given that TNF-α plasma concentration (outcome measure) is a continuous variable, multiple linear regression analysis was carried out to assess AHI (or SpO2 nadir or respiratory arousal index) and BMI z-score as predictors of morning plasma TNF-α levels. Thus, polysomnography indices (explanatory variables) were included as continuous variables.
RESULTS
Subject Characteristics and Polysomnography Findings
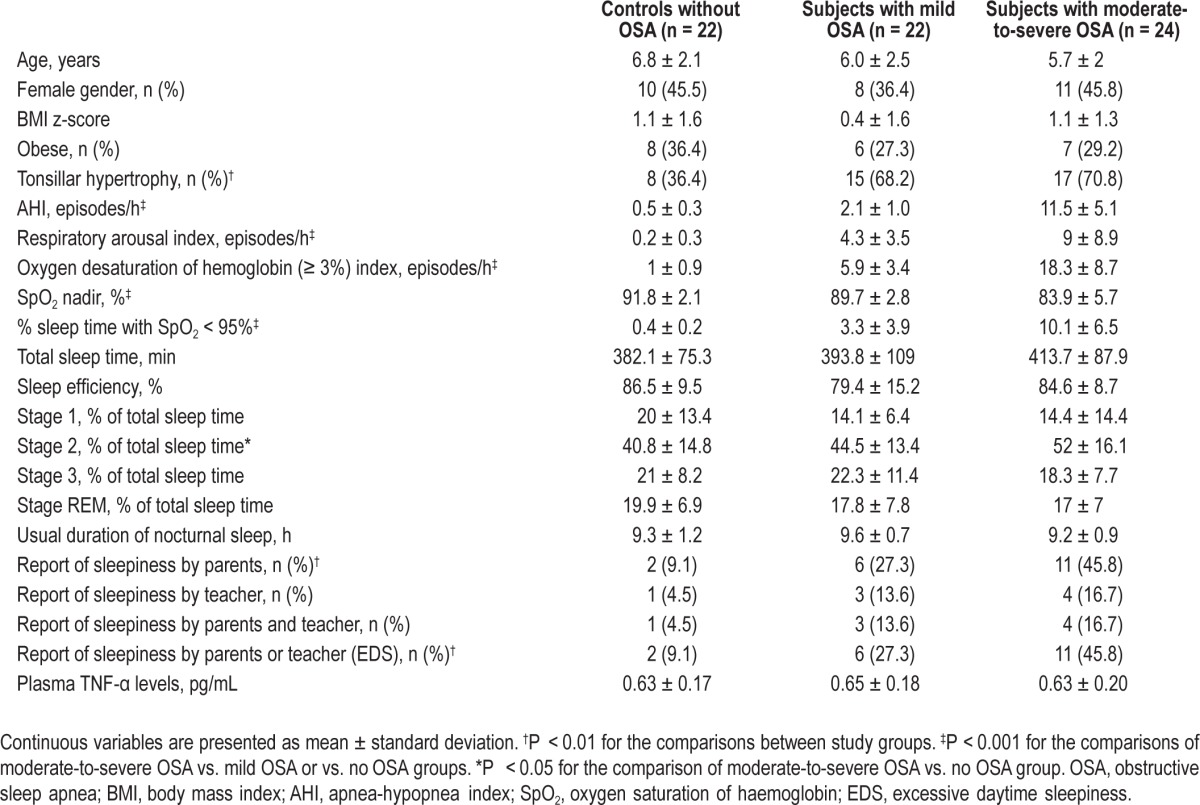
During the study period, 46 children with OSA and AHI > 1 episode/h and 22 subjects without snoring and an AHI ≤ 1 episode/h were recruited. Twenty-two participants with snoring had mild OSA, and the remaining 24 had moderate-to-severe OSA. Children with moderate-to-severe OSA had significantly worse polysomnography indices when compared to those with mild OSA or to controls (Table 1). The 3 study groups differed significantly in the prevalence of EDS, but they were similar in terms of duration of nocturnal sleep, age, BMI z-score, frequency of female or obese subjects, and sleepiness reported by teacher (Table 1).
Table 1.
Summary statistics and significance of comparisons regarding subjects' characteristics
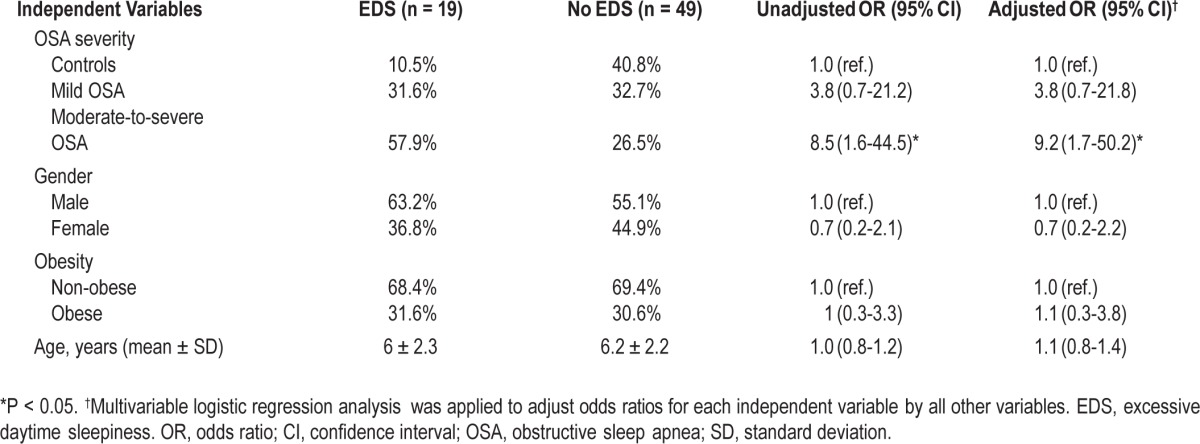
Effect of OSA on Risk for EDS
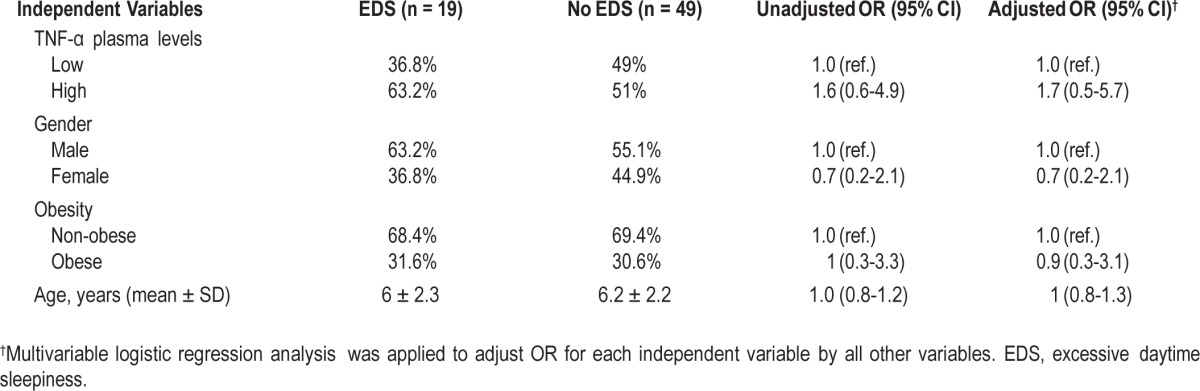
Children with moderate-to-severe OSA, but not participants with mild OSA, were at significantly higher risk for EDS than controls without snoring even after adjustment for age, gender, and obesity: 9.2 (1.7-50.2); P = 0.01, and 3.8 (0.7-21.8); P > 0.05, respectively (Table 2).
Table 2.
Odds ratios and 95% confidence intervals for potential predictors of excessive daytime sleepiness using logistic regression analysis
Effect of OSA Severity on TNF-α Levels
The 3 study groups were similar regarding morning plasma TNF-α levels (P > 0.05; Table 1 and Figure 1). BMI z-score— but not AHI, SpO2 nadir, or respiratory arousal index—was a significant predictor of morning plasma TNF-α levels (Table 3 and Figure 2).
Figure 1.
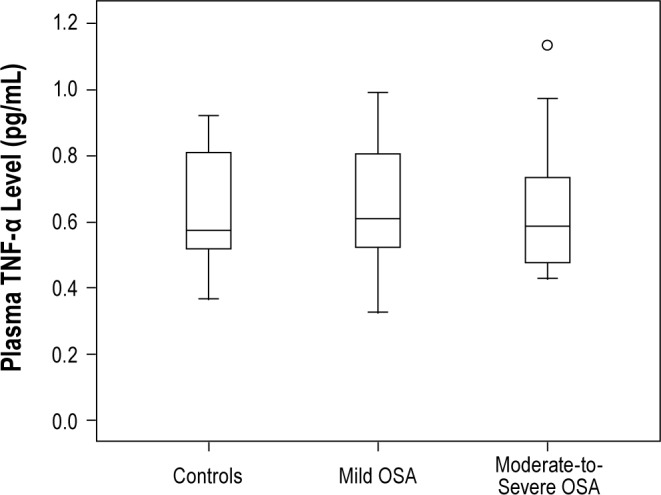
Boxplots representing morning plasma TNF-α levels in control participants and subjects with mild or moderate-to-severe OSA. There are no significant differences in terms of TNF-α levels between the three study groups.
Table 3.
Multiple linear regression analysis models for the evaluation of the independent effect of different variables on morning plasma TNF-α levels in children with and without obstructive sleep apnea.
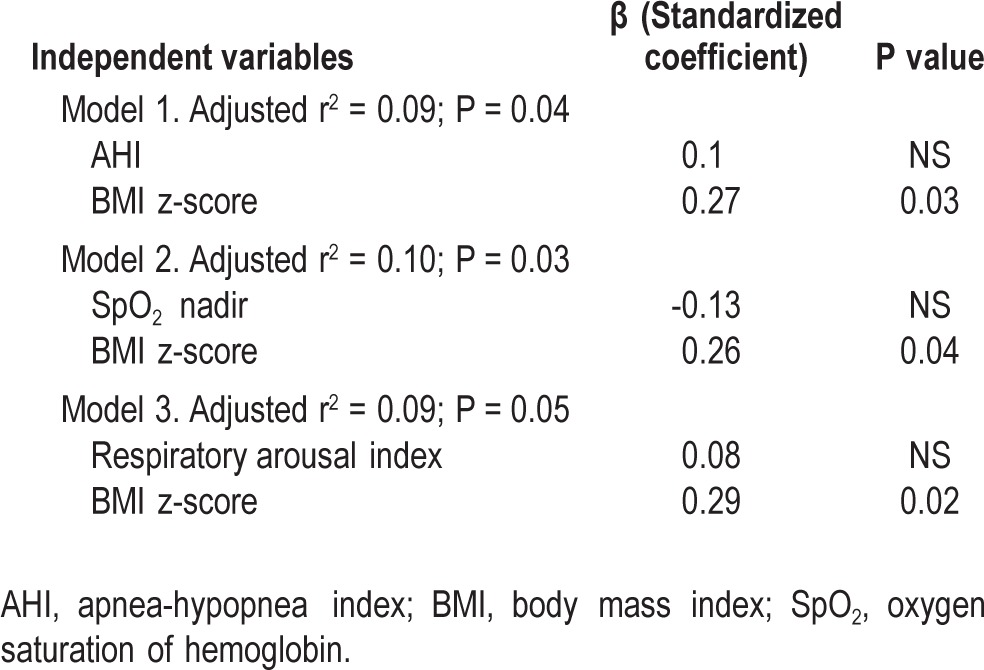
Figure 2.
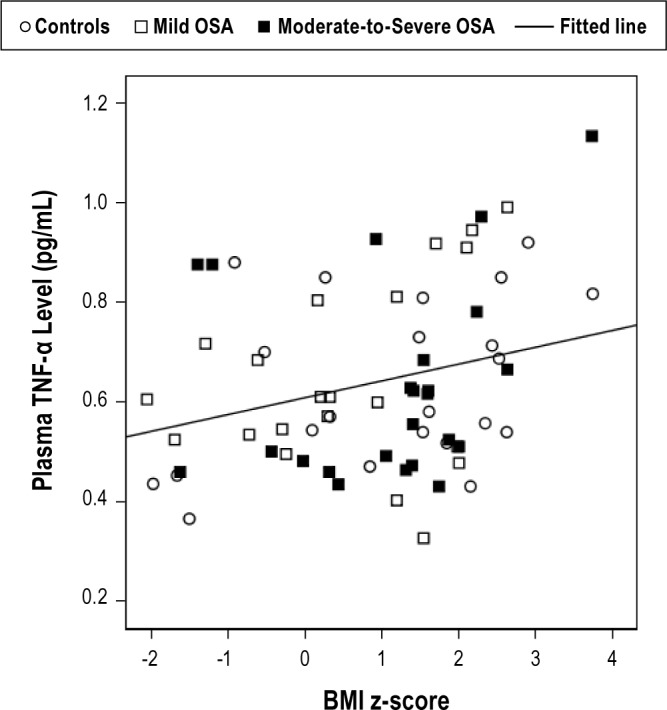
TNF-α plasma concentrations are significantly associated with BMI z-score (P < 0.05), and this relationship is not modified by severity of OSA.
Effect of High TNF-α Plasma Levels on Risk for EDS
The median TNF-α plasma concentration in control subjects was 0.57 pg/mL. Thus, 14 of 22 (63.6%) children with mild OSA and 12 of 24 (50%) subjects with moderate-to-severe OSA had high morning TNF-α plasma levels. High TNF-α plasma level was not a significant predictor of EDS (Table 4).
Table 4.
Odds ratios (OR) and 95% confidence intervals for high TNF-α level (> 0.57 pg/mL) as potential predictor of excessive daytime sleepiness with and without adjustment by other variables
DISCUSSION
In the current study, it was demonstrated that children with moderate-to-severe OSA are at increased risk of having EDS compared to healthy controls. Nevertheless, plasma TNF-α concentrations are not influenced by OSA severity and they cannot be used as predictor for the presence of EDS in children with sleep apnea. A modest association of TNF-α levels with the degree of adiposity was noted.
TNF-α is a transmembrane protein with an extracellular domain that is produced by a variety of cells (lymphocytes, epithelial, endothelial, and tumor cells).22 Shedding of the extracellular domain in the bloodstream releases the bioactive cytokine TNF-α, which has been implicated in the pathogenesis of asthma, inflammatory bowel disease, rheumatoid arthritis, sepsis, atherosclerosis, and other disorders.23
TNF-α along with interleukin-6 may mediate EDS in adults with sleep apnea and/or obesity.1 Severity of OSA and levels of inflammatory cytokines such as TNF-α and interleukin-6 correlate with the amount of visceral fat.1 Indeed, both TNF-α and interleukin-6 are directly produced in fat tissue examined by microperfusion, and their production is regulated by food intake and the sympathetic nervous system.24 The degree of sleepiness based on multiple sleep latency tests correlates with the degree of obesity.25
In the present study, plasma TNF-α levels were similar to those reported in most other published pediatric reports,8,9,12 and they did not correlate with severity of OSA. In the investigation by Li et al., median TNF-α plasma concentrations were 0.4 pg/ mL in the OSA group and 0.5 pg/mL in the control group.9 Tam et al. have reported median serum concentrations of 5.3 pg/mL in children with sleep apnea and 4.7 pg/mL in control subjects.8 More recently, Tsaoussoglou et al. have found mean plasma TNF-α concentrations ranging from 1.45 to 1.87 pg/mL in over-weight or obese children with OSA and in overweight, obese, or lean control subjects.12
In contrast, Gozal et al. have detected mean plasma TNF-α levels varying from 330.3 pg/mL (control participants) to 1,002.4 pg/mL (children with AHI ≥ 10/h) with reference values for healthy volunteers provided by the TNF-α assay manufacturer from 0 to 5.89 pg/mL.11 One factor possibly explaining the higher TNF-α levels in the investigation by Gozal et al. relative to other pediatric studies is the large proportion of obese participants, especially in the group with moderate-to-severe OSA.11 In a subsequent study from the same group, morning TNF-α levels and Epworth Sleepiness Scale scores were found to be increased in the presence of OSA.13
Recognition of EDS in children and adolescents is important because it may affect academic performance. There is no doubt that TNF-α contributes to the pathogenesis of EDS in OSA, since administration of a TNF-α antagonist, etanercept, is accompanied by marked reduction in EDS.26 Also a biallelic G to A polymorphism in the TNF-α gene promoter (-308 G/A) has been identified, and the minor allele (A) has been consistently associated with increased prevalence of OSA in adults27 and with increased Epworth Sleepiness Scale scores in children with sleep apnea.13
In our population of Greek children, high TNF-α concentrations were not associated with EDS, although participants with moderate-to-severe OSA had increased frequency of sleepiness. The discrepant findings of this report compared to the study by Khalyfa et al.13 in US children may be due to differences in: (i) the prevalence of TNF-α gene polymorphisms promoting synthesis of the cytokine; and (ii) the degree of adiposity in subjects with sleep apnea (much higher BMI z-scores in US children).13 Moreover, a single measurement of the TNF-α concentration in plasma does not necessarily reflect the 24-h activity of the cytokine. In addition, the TNF-α measurement may be affected by the conditions of sample collection and storage and the commercial assay used.20,21
It should be noted that obese adults with OSA have higher frequency of the TNF-α -308G/A gene polymorphism and higher plasma levels of the cytokine than obese controls without OSA.28 Thus, we speculate that the combination of certain genetic background and obesity should be present to demonstrate significant associations between OSA, TNF-α activity, and sleepiness as it has been found in studies with adult participants. This condition may not be fulfilled in all cohorts reported so far in the pediatric literature. In addition, differences in results of studies regarding the association of TNF-α and sleepiness between children and adults with OSA may be due to effects of age or other developmental processes.
One potential limitation of the current study is that the evaluation of EDS was based on parental responses to questions previously used in the TuCASA study and not on multiple sleep latency tests.3 Young teenagers participating in the study may have had an element of delayed sleep phase. Sleep hygiene and caffeine intake were not recorded, and nocturnal sleep duration was evaluated using parental report and not actigraphy. All the previous parameters could have confounding effects on the prevalence of EDS among study participants.
In conclusion, moderate-to-severe OSA, and not a high TNF-α plasma level, is associated with increased prevalence of EDS in childhood. Detection of TNF-α gene variants may be a better tool for the recognition of children with sleep apnea at risk for central nervous system morbidity than measurement of TNF-α plasma concentrations, which may not reflect the 24-h activity of the cytokine accurately.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENT
This work was supported by intramural funding (University of Thessaly Research Committee).
REFERENCES
- 1.Vgontzas AN, Papanicolaou DA, Bixler EO, et al. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–8. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 2.Carroll JL, McColley SA, Marcus CL, Curtis S, Loughlin GM. Inability of clinical history to distinguish primary snoring from obstructive sleep apnea syndrome in children. Chest. 1995;108:610–8. doi: 10.1378/chest.108.3.610. [DOI] [PubMed] [Google Scholar]
- 3.Goodwin JL, Kaemingk KL, Mulvaney SA, Morgan WJ, Quan SF. Clinical screening of school children for polysomnography to detect sleep-disordered breathing-the Tucson Children's Assessment of Sleep Apnea Study (TuCASA) J Clin Sleep Med. 2005;1:247–54. [PMC free article] [PubMed] [Google Scholar]
- 4.Chervin RD, Weatherly RA, Ruzicka DL, et al. Subjective sleepiness and polysomnographic correlates in children scheduled for adenotonsillectomy vs other surgical care. Sleep. 2006;29:495–503. [PMC free article] [PubMed] [Google Scholar]
- 5.Melendres MC, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics. 2004;114:768–75. doi: 10.1542/peds.2004-0730. [DOI] [PubMed] [Google Scholar]
- 6.Calhoun SL, Vgontzas AN, Fernandez-Mendoza J, et al. Prevalence and risk factors of excessive daytime sleepiness in a community sample of young children: the role of obesity, asthma, anxiety/depression, and sleep. Sleep. 2011;34:503–7. doi: 10.1093/sleep/34.4.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gozal D, Wang M, Pope DW., Jr Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics. 2001;108:693–7. doi: 10.1542/peds.108.3.693. [DOI] [PubMed] [Google Scholar]
- 8.Tam CS, Wong M, McBain R, Bailey S, Waters KA. Inflammatory measures in children with obstructive sleep apnoea. J Paediatr Child Health. 2006;42:277–82. doi: 10.1111/j.1440-1754.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- 9.Li AM, Lam HS, Chan MH, et al. Inflammatory cytokines and childhood obstructive sleep apnoea. Ann Acad Med Singapore. 2008;37:649–54. [PubMed] [Google Scholar]
- 10.Waters KA, Mast BT, Vella S, et al. Structural equation modeling of sleep apnea, inflammation, and metabolic dysfunction in children. J Sleep Res. 2007;16:388–95. doi: 10.1111/j.1365-2869.2007.00614.x. [DOI] [PubMed] [Google Scholar]
- 11.Gozal D, Serpero LD, Kheirandish-Gozal L, Capdevila OS, Khalyfa A, Tauman R. Sleep measures and morning plasma TNF-alpha levels in children with sleep-disordered breathing. Sleep. 2010;33:319–25. doi: 10.1093/sleep/33.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsaoussoglou M, Bixler EO, Calhoun S, Chrousos GP, Sauder K, Vgontzas AN. Sleep-disordered breathing in obese children is associated with prevalent excessive daytime sleepiness, inflammation, and metabolic abnormalities. J Clin Endocrinol Metab. 2010;95:143–50. doi: 10.1210/jc.2009-0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khalyfa A, Serpero LD, Kheirandish-Gozal L, Capdevila OS, Gozal D. TNF-alpha gene polymorphisms and excessive daytime sleepiness in pediatric obstructive sleep apnea. J Pediatr. 2011;158:77–82. doi: 10.1016/j.jpeds.2010.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 15.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002:1–190. [PubMed] [Google Scholar]
- 17.Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clin North Am. 1989;36:1551–69. doi: 10.1016/s0031-3955(16)36806-7. [DOI] [PubMed] [Google Scholar]
- 18.Iber C, Ancoli-Israel S, Chesson A, Quan S American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events : rules, terminology and technical specifications. [Google Scholar]
- 19.American Sleep Disorders Association. EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]
- 20.Exley AR, Cohen J. Optimal collection of blood samples for the measurement of tumor necrosis factor alpha. Cytokine. 1990;2:353–6. doi: 10.1016/1043-4666(90)90065-2. [DOI] [PubMed] [Google Scholar]
- 21.Matheson LA, Duong TT, Rosenberg AM, Yeung RS. Assessment of sample collection and storage methods for multicenter immunologic research in children. Journal of immunological methods. 2008;339:82–9. doi: 10.1016/j.jim.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Pennica D, Nedwin GE, Hayflick JS, et al. Human tumour necrosis factor: precursor structure, expression and homology to lymphotoxin. Nature. 1984;312:724–9. doi: 10.1038/312724a0. [DOI] [PubMed] [Google Scholar]
- 23.de Jager W, Hoppenreijs EP, Wulffraat NM, Wedderburn LR, Kuis W, Prakken BJ. Blood and synovial fluid cytokine signatures in patients with juvenile idiopathic arthritis: a cross-sectional study. Ann Rheum Dis. 2007;66:589–98. doi: 10.1136/ard.2006.061853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orban Z, Remaley AT, Sampson M, Trajanoski Z, Chrousos GP. The differential effect of food intake and beta-adrenergic stimulation on adipose-derived hormones and cytokines in man. J Clin Endocrinol Metab. 1999;84:2126–33. doi: 10.1210/jcem.84.6.5747. [DOI] [PubMed] [Google Scholar]
- 25.Marcus CL, Curtis S, Koerner CB, Joffe A, Serwint JR, Loughlin GM. Evaluation of pulmonary function and polysomnography in obese children and adolescents. Pediatr Pulmonol. 1996;21:176–83. doi: 10.1002/(SICI)1099-0496(199603)21:3<176::AID-PPUL5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 26.Vgontzas AN, Zoumakis E, Lin HM, Bixler EO, Trakada G, Chrousos GP. Marked decrease in sleepiness in patients with sleep apnea by etanercept, a tumor necrosis factor-alpha antagonist. J Clin Endocrinol Metab. 2004;89:4409–13. doi: 10.1210/jc.2003-031929. [DOI] [PubMed] [Google Scholar]
- 27.Varvarigou V, Dahabreh IJ, Malhotra A, Kales SN. A review of genetic association studies of obstructive sleep apnea: field synopsis and meta-analysis. Sleep. 34:1461–8. doi: 10.5665/sleep.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhushan B, Guleria R, Misra A, Luthra K, Vikram NK. TNF-alpha gene polymorphism and TNF-alpha levels in obese Asian Indians with obstructive sleep apnea. Respir Med. 2009;103:386–92. doi: 10.1016/j.rmed.2008.10.001. [DOI] [PubMed] [Google Scholar]


