Abstract
Study Objectives:
To evaluate the effect of a housing transition on sleep quality and quality of life in slum dwellers, participating in a slum housing upgrading program.
Design:
Observational before-and-after study with a convergent-parallel mixed method design.
Setting:
Five slums located in the metropolitan area of Buenos Aires, Argentina.
Participants:
A total of 150 slum dwellers benefited by a housing program of the nonprofit organization TECHO (spanish word for “roof”).
Interventions:
Participants moved from their very low-quality house to a basic prefabricated 18 m2 modular house provided by TECHO.
Measurements and Results:
The Pittsburgh Sleep Quality Index (PSQI) and World Health Organization Quality of Life brief scale (WHOQOL-BREF) were administered before and after housing upgrading. Data about housing conditions, income, education, sleeping conditions, and cardiovascular risk were also collected. Semistructured interviews were used to expand and nuance quantitative data obtained from a poorly educated sample. Results showed that sleep quality significantly increased after the housing program (z = -6.57, P < 0.001). Overall quality of life (z = -6.85, P < 0.001), physical health domain (z = -4.35, P < 0.001), psychological well-being domain (z = -3.72, P < 0.001) and environmental domain (z = -7.10, P < 0.001) of WHOQOL-BREF were also improved. Interviews demonstrated the importance of serenity for improving quality of life.
Conclusions:
A minimal improvement in the quality of basic housing can significantly increase sleep quality and quality of life among slum dwellers. Understanding sleep and daily life conditions in informal urban settlements could help to define what kind of low-cost intervention may improve sleep quality, quality of life, and reduce existent sleep disparity.
Citation:
Simonelli G; Leanza Y; Boilard A; Hyland M; Augustinavicius JL; Cardinali DP; Vallières A; Pérez-Chada D; Vigo DE. Sleep and quality of life in urban poverty: the effect of a slum housing upgrading program. SLEEP 2013;36(11):1669-1676.
Keywords: Sleep, poverty, slums, quality of life, mixed method design
INTRODUCTION
The unprecedented urban growth in the face of increasing poverty and social inequity in developing countries is posing an immense challenge for governments at all levels. Urbanization of poverty is shown mainly by the proliferation and expansion of slums.1 Such places often contain houses built using plywood, wood boards, cardboard, corrugated metal, and sheets of plastic.
More than one billion people, approximately 14% of the global population, are slum dwellers.2 According to United Nations Human Settlements Programme (UN-HABITAT) predictions, the number of slum dwellers could double by the year 2030, due to the increase in poverty and social inequality in the context of extraordinary urban growth.3
In Latin America and the Caribbean, despite the significant economic progress over the past two decades, many of the region's city inhabitants are poorly housed. Of the 130 million urban families in the region, five million rely on another family for shelter, three million live in houses that are beyond repair, and another 34 million live in houses that lack either title, water, sewerage, adequate flooring, or sufficient space.4
Although the term “slum” has a colloquial meaning in today's social context, there is no internationally accepted academic definition for a slum. The Latin American youth-led nonprofit organization TECHO (spanish word for “roof”), which is active in 19 countries of Latin America and the Caribbean, defines slums as settlements of eight or more families occupying land and lacking at least one of three basic services: water, electricity, or sewer. Through the joint work of families living in extreme poverty and young volunteers, TECHO seeks to overcome poverty in slums. TECHO′s first phase of intervention is an assessment of the family's need and promotion of organization, participation, and community coresponsibility. During the second phase, TECHO focuses on building transitional housing to urgently address the need for adequate shelter that is present in most slums. These transitional houses are based on a prefabricated 18 m2 module that is elevated off the floor, includes a zinc roof, and is built in 2 days.
Slums can vary substantially in their structure, composition, and culture; those involved in our study differed in a variety of aspects that ranged from electricity access to flood risk, from crime to contamination and the size of parcels. Nevertheless, slum dwellers do share the fact that they live in the most adverse of circumstances. In this context, poor sleep could amplify other health-related problems typical of the slum environment, such as psychological distress, poor diet, a sedentary lifestyle, and cardiovascular disease, demonstrating its important role in chronic illness and health.5–12 However, the quality of sleep, sleep routine, sleep context, and sleep habits among slum dwellers have not yet been examined in the scientific literature. Understanding sleep disparity within this unique population could provide insight into quality-of-life parameters, and can aid with the development and use of novel interventions. Our study evaluates the effect of a housing transition on quality of life, sleep quality, and sleep conditions of slum dwellers who participated in the slum-housing upgrading program run by the nonprofit organization TECHO in the metropolitan area of Buenos Aires, Argentina.
METHODS
Participants
This study was conducted in accordance with the Declaration of Helsinki. Participants gave written informed consent and the study was approved in advance by an Independent Human Subjects Review Board.
A total of 150 adult slum dwellers on the waiting list for the TECHO housing program were invited to participate in the study between the months of April and October 2011. They were all residents of slums located in the metropolitan area of Buenos Aires, Argentina. All participants met selection criteria defined by TECHO. These criteria are based on a thorough evaluation of housing conditions, income, family size and composition, health conditions, and access to social networks.
Of the 150 participants (91 females and 59 males), 77 (47 females and 30 males) successfully completed the protocol by answering questionnaires before and 1 mo after the housing improvement. Seventy participants could not be reached either by phone or during either of two attempts to visit the home in person for the second assessment. Three subjects did not move to the TECHO house during the course of the study. A total of 30 (19 females and 11 males) were available for a reinterview after 6 mo with the same measurement tools. A subgroup of 21 subjects (14 females and 7 males), who participated in all the instances previously described, also took part in brief semistructured interviews between 1 and 6 mo after transition (Figure 1).
Figure 1.
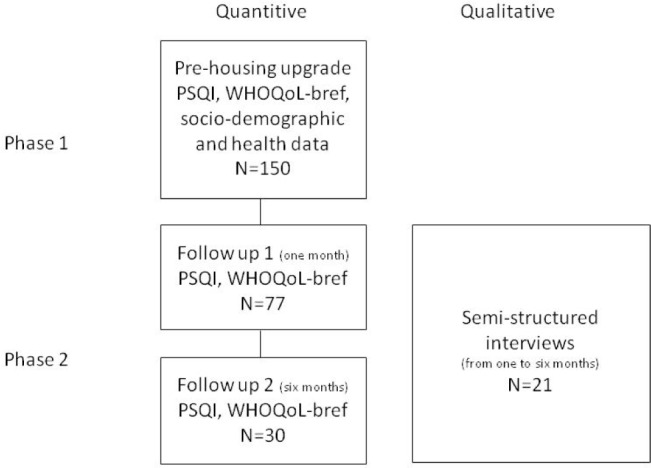
Flowchart of research. Phase 1 involved acquiring quantitative data before housing upgrade. Phase 2 involved acquiring quantitative data at 1 and 6 mo after house upgrade took place. During that period qualitative data was obtained through semistructured interviews.
The mean (standard deviation [SD]) age of the initial sample was 30.6 (9.12) y with a body mass index (BMI) of 26.0 (5.16) kg/m2. The average income per family member was considerably below the poverty line according to the national standard measured by access to an average diet. The families also matched at least two criteria from unsatisfied basic needs (more than three people living in the same room, living in a substandard house/tenancy, children aged 6 to 12 y not attending school and no sewage service), another complementary tool used to measure poverty. The entire sample attended primary school; however, only 46% completed the seventh grade (from a total of 12 y of compulsory education). A total of 4% had finished high school and none had attended postsecondary school.
Measurement Tools
Sociodemographic and Health Data
Participants were asked about income level, formal education, and attained demographic and health data including age, height, body weight, and the presence (yes or no) of smoking habits, cardiovascular disease family history, and diagnosed diabetes, hypertension, or dyslipidemia. BMI was calculated (kg/m2), defining overweight as BMI ≥ 25 kg/m2 and obesity as BMI ≥ 30 kg/m2. Participants answered one question about self-perceived psychological stress with a five-point Likert response scale: (1) never experienced stress; (2) seldom; (3) quite often; (4) very often; (5) always. Stress was defined as a feeling of tension, irritability, or anxiety, or as having sleeping difficulties as a result of conditions at work or at home in the past month. In Argentina, access to public healthcare is widespread and slums at the study did have primary health facilities relatively close.
Sleep and Sleep Quality
Housing and sleeping conditions were evaluated based on a seven-item questionnaire. Participants were asked “how many people do you share the place with?”, and about structural aspects of their houses, such as their roof structure, floor, and the presence of dampness in the home. They were also asked “how many people do you share your bed with, besides your partner?” and they had to choose among three possible answers: “none”, ”one person” and “more than one person”. A response of “none” could be one person in the bed (subject with no partner) or two people in the bed (subject with a partner). Taking into account that the program rarely takes people who do not have children, this question was asked to assess how many extra people were on the bed of the parent/s and see if there was a modification in this behavior after transition, leaving aside the partner if they had one.
The Pittsburgh Sleep Quality Index13 (PSQI) is composed of 19 self-rated questions for assessing subjective sleep quality over the previous month. A Spanish version of this questionnaire was used.14 The questions generate seven component domain scores: subjective sleep quality; sleep latency; sleep duration; habitual sleep efficiency; sleep disturbances; use of sleep medication; and daytime dysfunction. Each of them is weighted equally from 0 to 3 and the global PSQI score ranges from 0 to 21, with higher scores indicating poorer sleep quality. A global score of PSQI > 5 yields a diagnostic sensitivity of 89.6% and specificity 86.5% (kappa = 0.75 P < 0.001) in distinguishing good and poor sleepers.13 Thus, its psychometric properties are adequate.13
Quality of Life
World Health Organization Quality of Life Brief Scale (WHOQOL-BREF) was used. The brief version of WHOQOL is a self-report generic quality of life (QOL) inventory of 26 items, including four domains: (1) physical health: activities of daily living, dependence on medicinal substances and medical aids, energy and fatigue, mobility, pain and discomfort, sleep and rest, work capacity;. (2) psychological well-being: bodily image and appearance, negative feelings, positive feelings, self-esteem, spirituality/religion/personal beliefs, thinking, learning, memory and concentration; (3) social relationships: personal relationships, social support, sexual activity; and (4) environment: financial resources, freedom, physical safety and security, health and social care: accessibility and quality, home environment, opportunities for acquiring new information and skills, participation in and opportunities for recreation/leisure activities, physical environment (pollution/noise/ traffic/climate), transport. Two of the items measure overall QOL/health. The questions are rated on a five-point Likert scale (1 = very dissatisfied/very poor to 5 = very satisfied/very good) and the results are transformed into scales ranging from 0 to 100 for each domain, according to the scoring instructions from the WHOQOL group. Higher scores indicate better QOL, although there is no cutoff point for its classification.15,16
Semistructured Interviews
Interviews were done in person at participants' houses. Three main themes were explored during this interview with open-ended questions: (1) changes in life with the new house (health, job, family relations, house organization, etc); (2) differences in sleep before and after moving into the new house; (3) sleep organization in the new house (time, day/night routine, bed sharing, etc). Interviews were transcribed for analysis purpose.
Design and Procedures
This is an observational before-and-after study with a convergent-parallel mixed method design. The first (before) phase used questionnaires to evaluate quality of life and sleep quality before moving into the new house. The second (after) phase explored quality of life and sleep quality changes through the same questionnaires 1 and 6 mo after the housing improvement. It also included semistructured interviews taken once within this period. This second phase follows a mixed method convergent parallel design. The objective of such a design is to obtain different but complementary data on the same phenomenon (convergent). The two sets of data, quantitative and qualitative, are obtained at the same time in the research process (parallel).17 Figure 1 presents the different methods used during the two phases of the research. We choose to include a qualitative data collection for three reasons: (1) we were interested in the meaning of the house change that would not be captured by questionnaires only; (2) research participants with low or no school experience are not familiar with questionnaires, and thus quantitative results might be biased; (3) including interviews would not only deepen our understanding of the phenomenon but also help us validate and nuance quantitative data.
Analysis
Data are shown as percentage for categorical variables, and mean (standard error of the mean [SEM]) for numerical variables. Association of sex with PSQI and QOL was assessed by a Mann-Whitney U test. Association of age with PSQI and QOL was assessed by a Spearman rank correlation test. One-mo and 6-mo follow-up measurements after the housing upgrade were compared with baseline measurements; the differences were assessed by the McNemar test for categorical variables and by the Wilcoxon test for numerical variables, and P values were adjusted by the Bonferroni method. Correlations between numerical values of PSQI and QOL were assessed through the Spearman rank correlation test. Spearman partial correlations were used to examine numerical associations adjusting for age and sex. Nonparametric statistics were used to avoid strict assumptions about the level of measurement and normality of the assessed variables.18
For semistructured interviews a thematic analysis was performed with the software QDA Miner. Such an analysis consists of systematically locating and organizing the different themes contained in a text corpus (e.g., wake-up routine, life changes for the children …).19 This operation is called coding. By coding the coder builds a thematic tree, which includes all themes and organizes them in a hierarchical mode. We also set up an interrater agreement procedure to validate the chosen codes. This procedure involved a second coder to check the coding and organization of codes of the first coder, after five interviews were coded. In case of disagreement, the coders discussed until they reach an agreement. The first coder then continued the coding of the remaining interviews with the new coding tree. A second check with both coders was done when all interviews were coded. Sex, age, number of people in the house. and employment (variables) were included in the software for each participant. Subsequently, analyses of frequency of codes and variables were performed to ascertain the principal trends in participant discourse. Minor perspectives were also analyzed to include all aspects related to change and sleep experience.
RESULTS
Housing and Medical Conditions
Housing conditions significantly improved after the program. The percentage of people who reported struggling weekly with structural aspects of their roof decreased from 57.3% to 2.6% (χ2 = 41.19, P < 0.001); the number of cases in which rain was considered a big problem decreased from 70.0% to 3.9% (χ2 = 46.17, P < 0.001) and the number of cases where dampness was considered a major problem decreased from 73.3% to 1.3% (χ2 = 51.15, P < 0.001). Overall dissatisfaction with housing conditions decreased from 78.7% to 2.6% (χ2 = 58.07, P < 0.001).
Some coronary risk factors were prevalent in the studied sample. A total of 19.3% of participants reported having a diagnosis of hypertension and 54.7% smoked, whereas 1.3% had a diagnosis of diabetes and 2.6% had a diagnosis of dyslipidemia. A total of 41.3% of participants had at least one first-degree relative with cardiovascular disease. Before the housing intervention, 39.3% of participants reported being stressed quite often, after 1 mo and 6 mo that percentage decreased to 5.6% and 3.3%, respectively (z = -4.38, P < 0.001).
Quality of Life
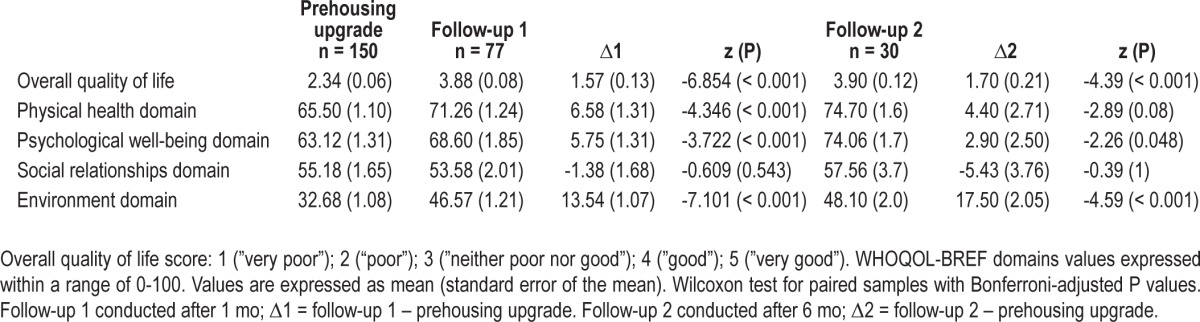
Before the housing transition overall quality of life was rated as “poor” or “very poor” by 63.1% of participants; whereas only 8.0% rated their overall quality of life as “good” or “very good”. When it came to self-perception of health, 20.7% reported being dissatisfied or very dissatisfied with their health, whereas 34.6% were either satisfied or very satisfied. The scores for the different domains of WHOQOL-BREF at the three time points are summarized in Table 1. The most significant difference was seen in overall quality of life and environment domain, whereas changes were nonsignificant as far as the social relationship domain (Table 1). Before housing improvement, the psychological well-being domain (z = -1.97, P = 0.049) and the social relationships domain (z = -2.59, P = 0.009) scores were significantly lower among women. No significant association was found between QOL and age, before or after the housing intervention.
Table 1.
Quality of life (WHOQOL-BREF) before and after house upgrading
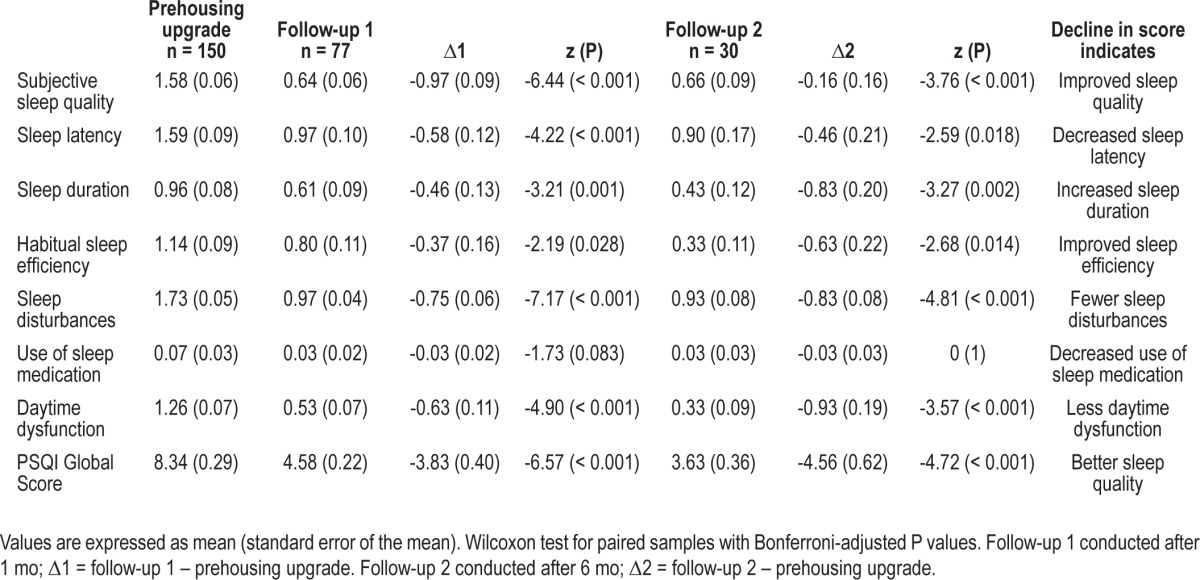
Sleep and Sleep Quality
Regarding sleep, the average number of people sharing a room at night was 3.6 (0.15) at study onset; there were no significant changes in room sharing after the intervention. From our sample, 35.3% shared their bed at nighttime with at least two people in addition to their regular partner, a total of 38.7% shared the bed with one person other than their partner, and only 26% did not share the bed at night with anyone else but their partner. After the housing upgrade, 54.5% were not sharing their bed with anyone else but their partner (binomial distribution, P ≤ 0.001). Baseline results show that 76.7% of participants had a global PSQI score > 5, whereas after the program 70.1% had a global PSQI score ≤ 5 (χ2 = 26.44, P < 0.001). Differences of PSQI and PSQI-specific domains before and after the intervention are summarized in Table 2. Marked improvements were seen in subjective sleep quality, sleep disturbances, and daytime dysfunction. The use of sleep medication was similar before and after intervention. After 6 mo of follow-up, results remain mostly the same (Table 2). Before the housing upgrade, the mean global PSQI score was higher among women (z = -2.13, P = 0.03). After the housing upgrade, PSQI did not differ between sexes. No other significant association was found between PSQI and age, before or after housing intervention.
Table 2.
Pittsburgh Sleep Quality Index components before and after house upgrading
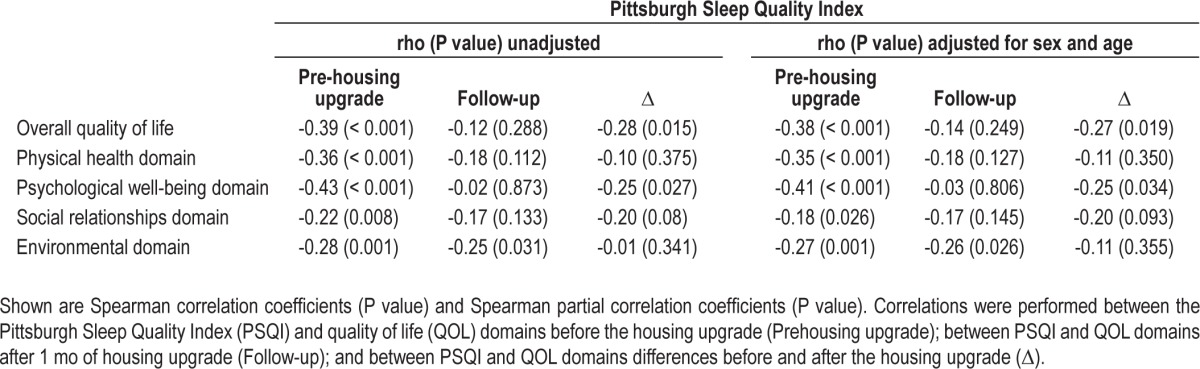
Associations between Sleep and Quality of Life
Before the housing upgrade, significant negative correlations were found between PSQI and overall quality of life, the psychological well-being domain, the physical health domain, the environment domain, and the social relationships domain. After the housing upgrade, only a significant negative correlation between PSQI and the environment domain was found. Regarding the changes in sleep and QOL, significant negative correlations were found between change in PSQI and change in overall quality of life and between change in PSQI and change in the psychological well-being domain (Table 3). Effect size and significance remained almost unchanged after adjusting for age and sex (Table 3).
Table 3.
Correlations between Pittsburgh Sleep Quality Index and Quality of Life domains
Semistructured Interviews
Three major themes were apparent upon analysis of the semi-structured interviews. First, the change of physical environment and the comfort gain are essential, especially the protection against the rain, the cold, and the humidity:
“Allá llovía y tenías que andar con los tachos, tenías que correr las cosas, porque se te arruinan. A mí la última vez que había llovido se me inundó todo, después tuve que levantar una altura.” [It used to rain inside my house, I would have to go around with buckets, moving stuff all over so they would not get ruined. After the last rain, I had a flood in my house, we had to lift the floor few inches.] [C6, female, 53]
This first theme includes also the new possibility to own some goods which will enhance life comfort:
“Antes como la otra casa era chiquita, no podíamos tener nada. Teníamos lo necesario, teníamos las camas de los chicos, la tele y nada más. Ahora pensamos comprar cosas, llenar la casa, no de tantas cosas pero de lo necesario.” [The old house was very small, we could not have anything. We had the indispensable; we had the beds of the kids, the TV set and nothing else. Now we are thinking about buying more stuff to fill the house, not too much, but what we now think it is needful.] [A4, female, 24]
The second theme was related to sleep; participants slept better and more peacefully:
“…porque antes estaba siempre con pesadillas, o no dormía directamente, por escuchar un ruidito o por estar insegura, que rompan algo y entren, la casa estaba armada así nomás. Acá yo estoy más segura, si me quieren entrar, a robar, voy a escucharlos, y me siento más segura, y duermo más tranquila, también pensando en los chicos.” […because before I was always having nightmares, or I would just not sleep at all because little noises or because feeling insecure about my house being broken by people trying to break into, the house was build just like that. Here I am more secure about people trying to break into, I will be able to hear them and I feel more safe, I am sleeping more tranquil, also thinking about my kids.] [D2, female, 33]
Those who had employment and the female participants talked more frequently about this peacefulness associated with sleep. Both employees and females have to follow a daily routine in order to keep their job and/or to take care of the children (it is clear from participants' discourse that mothers are systematically in charges of family duties: bringing children to school, housekeeping). This is the only theme that differs according to two out of the four variables included in the qualitative analysis (sex, age, employment, and number of people in the house).
The third theme is the feeling of serenity. After moving to their new house participants felt more peaceful. The Spanish word tranquilo, equivalent to serenity, was central in participants' discourse:
“No era como antes, que no estaba tranquilo, hay menos peleas, hablamos más, comemos en familia, digamos que estamos bien, contentos…” [It is not like it used to be, it was not peaceful, there are less fights at home, we speak each other more, we eat in family, we think we are fine, happy…] [C4, male, 30]
This feeling is complementary to the one associated with sleep. Some participants talk about it as feeling more secure:
“Era el miedo, por ejemplo a veces se agarran a tiros (tiroteo) acá en frente, y me da miedo que pasen las balas, pero después me siento muy segura en todo sentido.” [It was the fear, for example sometimes there are shooting right in front of my house, I would be scared of bullets passing through, but now I feel very secure in all the senses.] [D2, female, 33]
This serenity has major effects on different spheres of participants' life. We have just shown it for daily routine (employment and family life) and sleep, and it has also consequences on social interactions:
“Y me está ayudando bastante, es más, la convivencia que tenía antes no era nada que ver, mejoró mucho, mejoró mucho.” [It is helping me a lot, to say, the conviviality we had has nothing to do with the one we have now, it improved a lot, it improved a lot.] [A1, male, 26]
A less frequent but still meaningful theme was that the house was a new beginning, a new start in their life:
“Ahora estoy invirtiendo en la casa, antes no la invertía en nada, miraba mi casa y no me daban ganas…necesitaba este empujón.”
“La casa fue el empujón?”
“Sí, sí, un empujón enorme, fue como que me hizo pensar ‘dale! Pensá en tu casa!’”
[Now I am investing in my house, before I would not invest it anywhere, I would look at my house and would not feel like it… I needed this push forward.
The house was this push forward? (Q)
Yes, the house was the push forward; it made me think “come on! It is time to work on your house!”] [D1, female, 35]
DISCUSSION
The main result of this study is that the slum-housing upgrade had a significant positive effect on sleep quality and QOL. This could be shown in both quantitative and qualitative results. Using a mixed design allowed us to demonstrate the importance of serenity for improving QOL and sleep quality as a function of improved housing conditions.
Having a new house (material comfort) helped people feel more secure and peaceful; serenity was central in participants' discourse. It is clear that sleep occurs when one feels sufficiently safe and secure to downregulate vigilance and alertness.20 In this context our findings support the idea that sleep is a naturally vulnerable state that is facilitated by feelings of safety in one's environment.21,22 At the same time, anxiety that stems from one's social relationships has been shown to have an effect on sleep quality.23 Our qualitative data suggest that feeling safe and serene has major effects on three different spheres of participants' lives: social interactions, daily routine, and sleep. We propose that these changes have an effect on the quality of their life; in turn, this will give them the motivation to move on. That is what we call “el ciclo tranquilo” [the serenity cycle] to keep the central word participants used (Figure 2). Note that the social relationships domain of the WHOQOLBREF showed no significant difference in the before and after statistics, but we know from the interviews the house change had meaningful effect on social life of participants. Probably the WHOQOL-BREF does not measure specific aspects of slum dwellers' life in the Argentine context.
Figure 2.
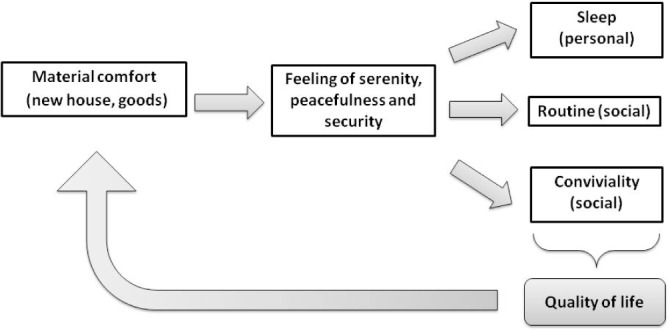
The serenity cycle (“El ciclo tranquilo”). Improved housing conditions provoke feelings of safety and serenity on the participants that affects on sleep, social interactions and daily routine. These changes affect quality of life, motivating them to move on.
Sleep quality was associated with most of QOL domains before the intervention. Improved sleep quality (lower PSQI) was associated with improved overall QOL and improved psychological well-being. After the intervention, only the environmental QOL domain remained significantly associated with sleep quality. Overall, these results demonstrate that sleep is a major determinant of quality of life in the context of poor housing conditions. Once housing conditions are improved, other factors may arise as possible determinants of QOL, reducing the relative importance of sleep in this association.
In this regard, sex and age were included as confounders when analyzing the relationship between sleep and QOL. Previous studies have shown that women and older adults have poorer subjective sleep quality than men and younger adults, respectively.24–26 In our sample, it was found that women were significantly poorer sleepers than men at baseline but not at the follow-up measurements. It is probable that the effects of poor housing conditions on sleep differ by sex. The lack of correlation between sleep and age in our study may be related to the large proportion of young people in our sample. In any case, the relationship between sleep and QOL remained unchanged after adjusting for age and gender.
Interestingly, the environmental domain of WHOQOLBREF was the only domain that remained significantly and negatively associated with sleep quality after upgrade. Looking at the qualitative results allows us to fine-tune our interpretation of this correlation. The environmental domain includes nine dimensions: home environment, physical safety and security, health and social care, financial resources, freedom, opportunities for acquiring new information and skills, participation in and opportunities for leisure activities, physical environment, and transport. Comfort gain and security were major themes positively associated with the house change. Furthermore, in Argentina, there is widespread access to public health care and informal access to medication is common: our results show the participants′ use of sleep medication was similar before and after intervention, even if we have no information about the kind of medication used. These results show that some dimensions of the environmental domain were already addressed (health care) or improved with the house change (home environment and security). However, the housing upgrading took place in the same parcel where previous low quality house was located, i.e., all other aspects of this domain have remained unchanged and are probably more meaningful for this population, specially financial resources, physical environment and opportunities for acquiring new information and skills. The combination of the house upgrading program with other programs that would address education and access to financial resources (such as microcredit programs), for example, would certainly help to improve QOL (and sleep) of these populations.
It has been proposed that sleep quality is a significant mediator and amplifying factor in the association between neighborhood disorder and psychological distress.5,27 Additionally, being a resident of a disadvantaged neighborhood and low socioeconomics in general, have been associated with poor sleep and worse self-reported health.28–30 Interestingly, our results show that a good sleep is possible even in a very poor and adverse environment, once you have four solid walls and a roof and you feel serene.
The structural instability of slum houses limits available functional space and complicates the use of space within the house. For example, slum houses often have leaky roofs and are in constant danger of structural collapse. These unpredictable external factors can affect the behavioral dynamics inside the house. Both slum houses and transitional houses have limited physical space for their occupants, which may explain the nonsignificant change in room sharing before and after the intervention. Given that participation in the program was prioritized for families with children over families without children, we were interested in assessing whether there was a voluntary reduction in parental bed sharing after transition. Our results showed that more than a quarter of participants no longer found it necessary to share their beds at night with someone else who was not their partner after the transition to the new house.
Considering the potential limitations in gathering paper and pencil data from a poorly educated sample, acquiring qualitative data provided additional information to expand our quantitative results. Quantitative data alone did not provide information about the meaning of behavioral changes in sleep due to the house improvement and could be wrongly interpreted. The use of semistructured interviews allows us to explore participant's social interaction with more sensitivity than by using the WHOQOL-BREF social relationships domain.
Working with this disadvantaged population involved several challenges. All the questionnaires had to be assessed by a trained interviewer, and reinterviewing participants was time consuming and labor intensive. In this regard, the reduction of the sample size after the follow-up period was one of the limitations of the quantitative aspect of our study. Participant attrition at follow-up was due to several difficulties: random home visits had to be performed when arranging for a second visit was not possible, a majority of participants had no access to a cell phone at the time of study completion; many slum dwellers have informal jobs without a predictable schedule that made arranging meetings problematic; most slums lack public transportation and paved streets, access during adverse weather conditions was not possible; for interviewer′s security, time spent at the slums was strictly limited to daylight hours, and therefore, the time available each day for data collection was reduced. Optimization of the limited time available to perform each interview was crucial, especially because one of the central goals of the study was to acquire sleep data. The WHOQOL-BREF was also selected for this reason in lieu of longer QOL questionnaires. Further, the slum dwellers participating on the housing program were preselected by nonprofit TECHO criteria, which may have affected the representativeness of the sample.
In the future, the use of physiological measurements may be necessary to glean a broader perspective of sleep in urban slums. The neighborhood structure, location, and other slum conditions should also be taken into account because slums can vary substantially between one another in their composition and its level of urbanization and integration to the city. The addition of semistructured interviews was necessary to fine-tune interpretations of answers to standardized questionnaires that are not context sensitive enough to grasp the nuances of day-to-day life experiences of marginalized populations. More mixed methods research could enhance and nuance knowledge about sleep. The ciclo tranquilo model must be tested in other contexts.
Concurrent investigations of low cost housing interventions that can lessen the adverse societal effects of poor sleep with a consequent effect on quality of life are also warranted.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. This study was conducted in accordance with the Declaration of Helsinki and approved in advance by an ethics committee. Guido Simonelli and Martin Hyland are senior medical students at Faculty of Medicine at the University of Buenos Aires. Dr. Cardinali and Dr. Vigo are Research Career Awardees from the Argentine Research Council (CONICET). Their work was partially supported by grants from Agencia Nacional de Promoción Científica y Tecnológica, Argentina (PICT 2007-01045, PICT 2010-1465 and PICTO-AUSTRAL 00124) and Universidad de Buenos Aires (M048).
ACKNOWLEDGMENTS
The authors thank Ignacio Gregorini and Agustín Algorta from TECHO for their invaluable support. We are indebted with Francisco Della Vecchia, Facundo Paniagua, Agustín Folgueira, Marina García, Cameron Miller, and Michael Salemi who kindly helped in the field work. We thank Graciela Romanelli for her technical assistance and Marcela González Arcila and other colleagues for their thoughtful comments. This project would not have been possible without families participating in TECHO's program, our deepest gratitude to them.
REFERENCES
- 1.UN HABITAT & Cities Alliance. Analytical perspective of pro-poor slum upgrading frameworks. 2006.
- 2.UN-HABITAT. State of the world's cities 2006/7. London: Earthscan Publications Ltd; 2007. [Google Scholar]
- 3.UN-HABITAT. Earthscan Publications Ltd; 2003. The challenge of slums: global report on human settlements. [Google Scholar]
- 4.Bouillon CP, editor. Palgrave Macmillan; 2012. Room for development: housing markets in Latin America and the Caribbean. [Google Scholar]
- 5.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15:1006–13. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Kamphuis CB, van Lenthe FJ, Giskes K, Brug J, Mackenbach JP. Perceived environmental determinants of physical activity and fruit and vegetable consumption among high and low socioeconomic groups in the Netherlands. Health Place. 2007;13:493–503. doi: 10.1016/j.healthplace.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Wilson DK, Kirtland KA, Ainsworth BE, Addy CL. Socioeconomic status and perceptions of access and safety for physical activity. Ann Behav Med. 2004;28:20–8. doi: 10.1207/s15324796abm2801_4. [DOI] [PubMed] [Google Scholar]
- 8.Johnson SL, Solomon BS, Shields WC, McDonald EM, McKenzie LB, Gielen AC. Neighborhood violence and its association with mothers' health: assessing the relative importance of perceived safety and exposure to violence. J Urban Health. 2009;86:538–50. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;11:380, 611–9. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 10.Graham JP, Corella Barud V, Avitia Diaz R, Gurian P. The in-home environment and household health: a cross-sectional study of informal urban settlements in northern Mexico. Int J Environ Res Public Health. 2005;2:394–402. doi: 10.3390/ijerph2005030003. [DOI] [PubMed] [Google Scholar]
- 11.Unger A, Riley LW. Slum health: from understanding to action. PLoS Med. 2007;4:1561–6. doi: 10.1371/journal.pmed.0040295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riley LW, Ko AI, Unger A, Reis MG. Slum health: diseases of neglected populations. BMC Int Health Hum Rights. 2007;7:2. doi: 10.1186/1472-698X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 14.Escobar-Cordoba F, Eslava-Schmalbach J. [Colombian validation of the Pittsburgh Sleep Quality Index] Rev Neurol. 2005;40:150–5. [PubMed] [Google Scholar]
- 15.Skevington SM, Lotfy M, O'Connell KA. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 16.Lucas-Carrasco R. The WHO quality of life (WHOQOL) questionnaire: Spanish development and validation studies. Qual Life Res. 2012;21:161–5. doi: 10.1007/s11136-011-9926-3. [DOI] [PubMed] [Google Scholar]
- 17.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. second edition. Thousand Oaks, CA: SAGE Publications; 2011. [Google Scholar]
- 18.Abreu MN, Siqueira AL, Cardoso CS, Caiaffa WT. Ordinal logistic regression models: application in quality of life studies. Cad Saude Publica. 2008;24:s581–91. doi: 10.1590/s0102-311x2008001600010. [DOI] [PubMed] [Google Scholar]
- 19.Paillé P, Mucchielli A. L'analyse qualitative en sciences humaines et sociales. 2e ed. Paris: 2008. [Google Scholar]
- 20.Salminen S, Oksanen T, Vahtera J, et al. Sleep disturbances as a predictor of occupational injuries among public sector workers. J Sleep Res. 2010;19:207–13. doi: 10.1111/j.1365-2869.2009.00780.x. [DOI] [PubMed] [Google Scholar]
- 21.Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: examining the covariation between relationship quality and sleep. Sleep Med Rev. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dahl RE, El-Sheikh M. Considering sleep in a family context: introduction to the special issue. J Fam Psychol. 2007;21:1–3. doi: 10.1037/0893-3200.21.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Carmichael CL, Reis HT. Attachment, sleep quality, and depressed affect. Health Psychol. 2005;24:526–31. doi: 10.1037/0278-6133.24.5.526. [DOI] [PubMed] [Google Scholar]
- 24.Doi Y, Minowa M, Uchiyama M, Okawa M. Subjective sleep quality and sleep problems in the general Japanese adult population. Psychiatry Clin Neurosci. 2001;55:213–5. doi: 10.1046/j.1440-1819.2001.00830.x. [DOI] [PubMed] [Google Scholar]
- 25.Asghari A, Farhadi M, Kamrava SK, Ghalehbaghi B, Nojomi M. Subjective sleep quality in urban population. Arch Iran Med. 2012;15:95–8. [PubMed] [Google Scholar]
- 26.Zeitlhofer J, Schmeiser-Rieder A, Tribl G, et al. Sleep and quality of life in the Austrian population. Acta Neurol Scand. 2000;102:249–57. doi: 10.1034/j.1600-0404.2000.102004249.x. [DOI] [PubMed] [Google Scholar]
- 27.Van Cauter E, Spiegel K. Sleep as a mediator of the relationship between socioeconomic status and health: a hypothesis. Ann N Y Acad Sci. 1999;896:254–61. doi: 10.1111/j.1749-6632.1999.tb08120.x. [DOI] [PubMed] [Google Scholar]
- 28.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–76. [PubMed] [Google Scholar]
- 30.Mackenbach JP, Howden-Chapman P. New perspectives on socioeconomic inequalities in health. Perspect Biol Med. 2003;46:428–44. doi: 10.1353/pbm.2003.0039. [DOI] [PubMed] [Google Scholar]


