Abstract
Study Objectives:
One theoretical model suggests a pathway between pain and the development of depression through sleep problems. Here, we prospectively test the hypothesis that incident sleep problems, in those with persistent pain, increase risk of new onset probable depression, and investigate the role of “pain that interferes with daily life” (pain interference) on this pathway.
Design:
Prospective cohort study.
Setting:
Community based population study within UK.
Participants:
Participants with persistent pain nested within a larger longitudinal community study.
Measurements:
Participants were mailed health questionnaires at baseline (time 1) with follow-up at 3 years (time 2) and 6 years from baseline (time 3). Questionnaires at baseline and at follow up contained measures of sleep problems (Jenkins Sleep Questionnaire), depressive symptoms (Hospital Anxiety and Depressive Scale), and pain interference.
Results:
In total, 2,622 participants returned health questionnaires at all time points and indicated the presence of pain at each time point. After adjustment for age, gender, marital status, employment status, alcohol intake, smoking status, and body mass index, having a new period of sleep problems at year 3 more than trebled the risk of a new period of probable depression at year 6 (relative risk 3.47, 95% CI 1.97 to 6.03). Mediation analysis showed that pain interference played a significant but relatively minor role in the pathway.
Conclusion:
Clinicians treating patients with persistent pain may wish to consider options that involve addressing the prevention or treatment of sleep problems, in addition to their primary focus of pain management.
Citation:
Campbell P; Tang N; McBeth J; Lewis M; Main CJ; Croft PR; Morphy H; Dunn KM. The role of sleep problems in the development of depression in those with persistent pain: a prospective cohort study. SLEEP 2013;36(11):1693-1698.
Keywords: Persistent pain, pain interference, sleep problems, depression, cohort
INTRODUCTION
Musculoskeletal pain is very common in the general population.1,2 While many people recover quickly and have no further difficulties, musculoskeletal pain can lead to a number of other problems, such as psychological distress.3,4 Pain has been shown in prospective epidemiological studies to be a risk factor for the development of depression,5 with people reporting disabling spinal pain having over double the risk of developing depression.6 Evidence indicates that psychological factors such as depression can represent a significant barrier to recovery,7 and psychological interventions are now part of biopsychosocial treatment strategies.8,9 Therefore a reduction in the development of depression would be an important outcome for those who experience pain.
The factors and mechanisms linking psychological disorders such as depression with physical disorders such as pain are multifaceted. A model developed by Cohen and Rodriguez suggests biological, behavioral, cognitive, and social pathways by which physical disorders such as pain can lead to affective disturbance.10 One specific pathway they suggest is that in those who experience pain, sleep disturbance can lead to the development of depression.
There is some evidence to support this pathway. It is well established that sleep problems are a risk factor for developing depression independent of pain.11–13 Sleep problems are common in pain patients,14over half of the back pain sufferers in a Norwegian epidemiological study reported sleep problems, compared with less than a third of people without back pain.2 Furthermore, there is evidence that sleep problems can exacerbate pain.15,16 However, information on the time sequences in the causal pathways between sleep and depression in pain populations are not clear. For example, one recent cross-sectional study reported that sleep problems predicted depression in those with pain,17 whereas another case control study reported the opposite, with depression as a factor in the development of insomnia.18 Indeed two recent reviews, on sleep and pain, and depression and sleep problems, respectively,19,20 reported that the establishment of cause and effect is complex, with evidence of bi-directionality between sleep, pain, and depression compounded by a lack of longitudinal research. Such longitudinal research is needed if appropriate timing and targets for interventions are to be identified.
The objective of this study was to examine the pathways for the development of sleep problems from prior depression and the development of depression from prior sleep problems in those who report persistent pain. Additionally, given the evidence of the role of pain severity impacting on both sleep problems and depression,19–21 this study also considered the mediating role of disabling pain (“pain interference”) on these pathways. Explicitly this study, among people who indicated the presence of persistent pain, (1) tested whether those who develop sleep problems have an increased risk of subsequently developing probable depression, (2) investigated if those who develop probable depression have an increased risk of subsequently developing sleep problems and, (3) examined the role of pain interference on these two pathways. These hypotheses were tested in a nested cohort of participants with persistent pain from a longitudinal community health survey.
METHOD
Design
This was a prospective cohort study of participants with persistent pain nested within a larger longitudinal community study: the North Staffordshire Osteoarthritis Project (NorStOP).22 NorStOP is a prospective cohort study of general health, socioeconomic, and pain factors in a community sample of adults aged ≥ 50 years (n = 13,986). Full details of the NorStOP project can be found elsewhere.22,23 Briefly, contact details of participants were provided by 6 general practices (GP) in North Staffordshire.22,23 It is estimated that approximately 98% of the UK population are registered with a GP,24 and so this cohort was representative of the target community. Participants were mailed health questionnaires at baseline (time 1) with follow-up at 3 years (time 2) and 6 years from baseline (time 3). Non-responders received further postal reminders at 2 and 4 weeks after each initial mailing in all phases. Ethics approval was given by North Staffordshire Local Research Ethics Committee and Birmingham North East and Solihull Local Research Ethics Committee.
Participants
The pool of potential participants for the analyses in this current study were those who responded to questionnaires at all the time points and indicated the presence of pain at all the time points, forming a cohort with continuing (persistent) pain over a 6-year period; and who were free of sleep problems and probable depression at baseline.
Measures
The same instruments for pain, sleep problems, and probable depression at baseline and follow-up phases were contained in all the questionnaires. Data on demographic variables and potential confounders were also collected at baseline.
Pain
Pain presence was identified from a question on the occur-rence of pain within the previous 4 weeks that lasted ≥ 1 day. Pain persistence was defined as the presence of pain at all 3 time points; this criterion for the definition of persistent pain has been demonstrated using this methodology within this cohort previously.25,26
Pain interference was measured using the question: “During the past 4 weeks how much did pain interfere with your normal work (including both work outside the home and homework).” A 5-point response scale was used: “not at all,” “a little bit,” “moderately,” “quite a bit,” and “extremely.” Responses were categorized into 2 groups for the logistic regression; “not at all” and “a little bit” for “no interference” with the remaining responses forming a “pain interference” group following previous studies.22,23,26
Sleep Problems
Sleep problems were measured using the Jenkins Sleep Questionnaire.27 The questionnaire contains 4 questions about sleep problems over the past 4 weeks; “having trouble falling asleep,” “waking up several times per night,” “having trouble staying asleep,” and “waking up after the usual amount of sleep feeling tired and worn out.” A 3-point response scale was used for each question: “not at all,” “on some nights,” and “on most nights.” Participants were classified into 2 groups; those who indicated no problems or problems experienced on some nights, and those who indicated experiencing problems on most nights for at least one of the questions. This definition has been used previously.15,28
Depression
A measure of depressive symptoms was obtained using the Hospital Anxiety and Depression Scale (HADS).29 The measure asks about the experience of the depressive symptoms over the past week, and consists of 7 questions to produce a scale score from 0-21. The measure has established reliability and validity in non-clinical samples. Participants were classified into 2 groups: non-depressed (scores 0-7) and probably depressed (scores ≥ 8) using guidelines by the original authors.29
Demographic Factors and Confounders
Other factors collected at baseline were included as they have been shown to be associated with sleep problems and depression.5,30 Measures of age, gender, alcohol consumption (daily, once/twice weekly vs. once/twice monthly, once/twice yearly, never), smoking status (never vs. previously, current smoker), marital status (married vs. separated, divorced, widowed, cohabiting, single), employment status (employed vs. not working due to ill health, retired, unemployed, housekeeping, other), and body mass index (score ≥ 25 as overweight) were obtained.
Analysis
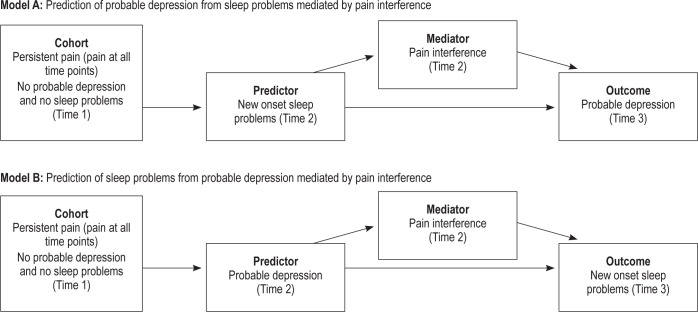
In accordance with outlined hypotheses, two analysis models were created. Model A tested whether having sleep problems increases the risk of developing probable depression with an examination of the mediating role of pain interference. Model B tested whether having probable depression increases the risk of developing sleep problems with an examination of the mediating role of pain interference (Figure 1).
Figure 1.
Mediation models.
To ensure assumptions on causality were met,31 restricted datasets were used for both models. Model A included only those within the nested cohort who were not categorized as having probable depression or sleep problems at baseline, and indicated no probable depression at the time of their new episode sleep problems at time 2 (n = 1,106). This ensured that the prediction of a new onset of probable depression (i.e., at time 3) was not preceded by a prior onset of probable depression (time 1 or time 2), and that the development of sleep problems (at time 2) was not preceded by previous probable depression (at time 1). Model B followed a similar pattern, excluding those who reported sleep problems and/or probable depression at baseline and reported sleep problems at time 2 (n = 848), to ensure the prediction of a new episode of sleep problems at time 3 from a new onset of probable depression at time 2.
Cox regression was used to determine Model A (risk of probable depression from prior sleep problems) and Model B (risk of sleep problems from prior probable depression). Unadjusted analyses were performed on the predictor variables (i.e., Model A—Sleep problems, Model B—Probable depression), then all variables, within their respective model, were placed in a multivariable analysis. Analysis was performed using STATA version 12.0 (STATA Corp). Binary mediation analysis was carried out on both models to test the role of pain interference using direct, indirect, and total effects, with adjustment for all confounders and demographic variables using STATA command “binary_mediation.”32 The mediation model followed guidance on mediation analysis with dichotomous data33; reporting coefficients between the independent variable and dependent variable (path c), the independent variable and the mediator variable (path a), the mediator variable and the dependent variable (path b) and the independent variable and the dependent variable adjusting for the mediation effect (path c′) as well as the overall proportion effect sizes (indirect effect, direct effect, and total effect, see Figures 2 and 3). Further analysis was carried out to consider the concurrent influence of the predictor on the outcome at the final time point (time 3). For Model A, Cox regression analysis was carried out to assess the influence of sleep problems at time 3 on probable depression at time 3, adjusted for sleep problems at time 2 as well as adjustment for age, gender, marital status, employment status, alcohol intake, smoking status, and BMI at baseline. A similar analysis was carried out for Model B, considering the influence of probable depression at time 3 on sleep problems at time 3 while adjusting for time 2 depression and the other baseline variables.
Figure 2.
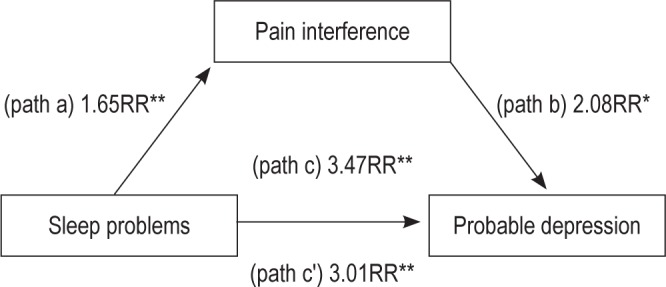
Mediation model on the association of sleep problems with later probable depression mediated by pain interference. Mediation model adjusted for age, gender, marital status, employment status, alcohol intake, smoking status, and body mass index. *P < 0.05, **P ≤ 0.001. RR, relative risk.
Figure 3.
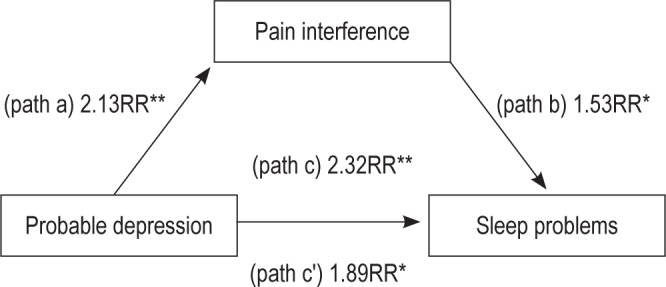
Mediation model on the association of probable depression with later sleep problems mediated by pain interference. Mediation model adjusted for age, gender, marital status, employment status, alcohol intake, smoking status, body mass index. *P < 0.05, **P ≤ 0.001. RR, relative risk.
Missing value analysis was carried out on missing data above 5%, testing for significant differences on key variables between those who responded with full data and those who did not.
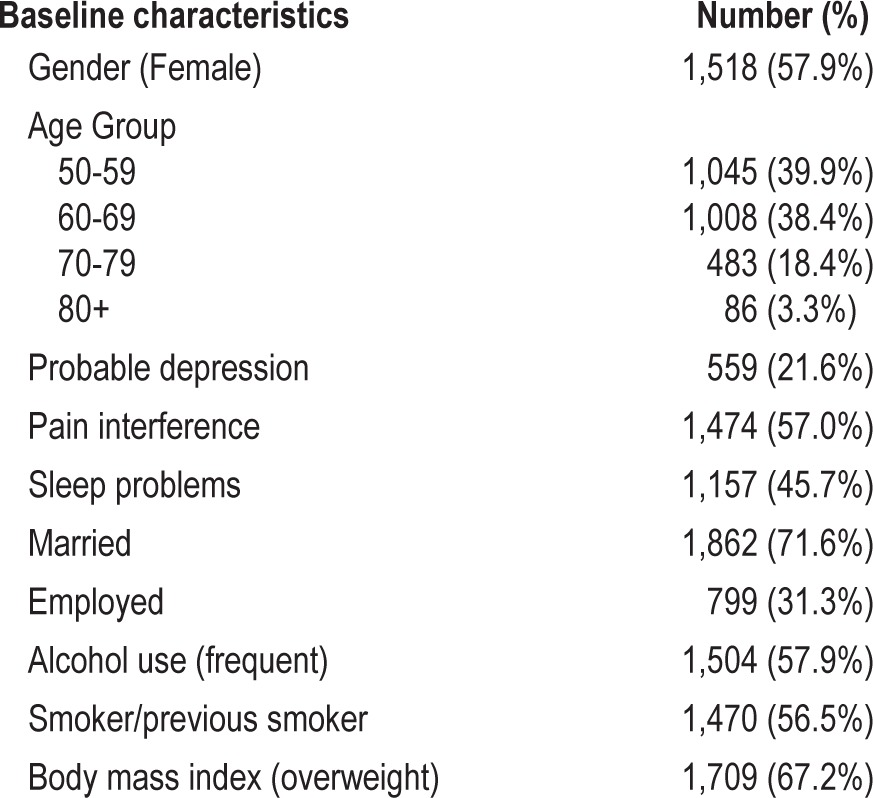
RESULTS
Baseline characteristics for the nested persistent pain cohort (n = 2,622) are described in Table 1. Prevalence rates for the key variables (probable depression, pain interference and sleep problems) were similar to baseline rates, and remained relatively stable at follow-up; probable depression, time 2 (21.7%) and time 3 (22.3%); pain interference, time 2 (57.0%) and time 3 (55.7%); and sleep problems, time 2 (49.6%) and time 3 (49.8%).
Table 1.
Baseline characteristics and prevalence figures
Prediction of Probable Depression by Sleep Problems Mediated by Pain Interference
For Model A (n = 1,106), the incidence of a new onset of probable depression (time 3) was 4.7%. Results for the unadjusted regression model show sleep problems at time 2 were associated with an increased risk of probable depression at time 3 (RR 2.85, 95% CI 1.62 to 5.02) compared to those who reported no sleep problems at time 2. The multivariable model (adjustment for baseline age, gender, marital status, employment status, alcohol intake, smoking status, and body mass index) showed that sleep problems more than trebled the risk of later probable depression (RR 3.47, 95%CI 1.97 to 6.03).
As shown in Figure 2, all coefficients are significant within the mediation model, indicating significant associations between all variables and also indicating the significant mediation effect of pain interference. Effect sizes for this mediation show that the indirect effect of sleep problems mediated by pain interference (0.04) is substantially smaller than the direct effect (0.26), indicating that pain interference, although significant, does not markedly contribute to the pathway between sleep problems and later probable depression. The overall total effect (r = 0.3) can be considered a medium effect size.34
Prediction of Sleep Problems by Probable Depression Mediated by Pain Interference
For Model B (n = 848) the incidence of sleep problems at time 3 is 18.1%. Unadjusted analysis shows probable depression (time 2) more than doubled the risk (RR 2.29, 95% CI 1.36 to 3.85) of development of sleep problems (time 3) compared to those who were categorized as having no probable depression. The multivariable model showed that adjustment made no marked difference to the risk estimate (RR 2.32, 95%CI 1.44 to 3.33).
Figure 3 shows the mediation analysis for Model B. All path coefficients are significant within the mediation model, indicating significant associations between all variables and the presence of a significant mediation effect. Effect sizes for this model show that the indirect effect of depression on the development of sleep problems, mediated by pain interference (0.03), is considerably smaller than the direct effect (0.12), indicating that pain interference plays a significant but minor role in the pathway. The total effect of the model is (r = 0.15), which can be considered a small effect size.34
Further analysis of the concurrent influence of sleep problems at time 3 on probable depression status at time 3 (Model A), while adjusting for sleep problems at time 2 and baseline variables (age, gender, marital status, employment status, alcohol intake, smoking status, and BMI), show that of those with probable depression, 53.2% also have sleep problems, compared to a rate of 24.6% in those without probable depression. Regression analysis shows concurrent sleep problems lead to over a doubling of risk for probable depression (RR 2.14 95% CI 1.07 to 4.28), over and above the influence of sleep problems on probable depression at time 2. Similar analysis on the influence of concurrent probable depression on sleep problems at time 3 (Model B) show that of those with sleep problems, 14.2% have probable depression compared to 3.9% of those without sleep problems. Regression analysis shows a more than doubling of the risk of sleep problems from concurrent probable depression (RR 2.49, 95% CI 1.37 to 4.49) over and above the influence of probable depression status at time 2.
Missing Values Analysis
Missing value analysis showed that only the Sleep Problems scale incurred item non-response above 5% (actual 6.2% at time 2, and 9.5% at time 3). Results of χ2 testing on missing item response showed that those who did not respond to the sleep questions at time 2 were less likely to report baseline pain interference (49% vs. 57%), and at time 3 were less likely to report baseline depression (17% vs. 22%). There were no significant differences found on any other variables. Complete case analysis was performed due to the low level of missing data in this cohort.
DISCUSSION
This study is the first to test, prospectively, the effect of new onset sleep problems on the later development of probable depression in those with persistent pain. The findings support the hypothesis that sleep problems increase the risk of future depression in those who report pain. However, the findings also show that people classified as probably depressed have increased risk of future onset of sleep problems. Regression analysis showed that a new episode of sleep problems more than trebles the risk of the later development of probable depression. Mediation analysis shows that the pathway of sleep to probable depression is stronger in effect size than the pathway of probable depression leading to new episode sleep problems. On both pathways, pain interference has a significant but minor role.
Comparison with Existing Literature
Two recent studies considered the link between pain, sleep problems, and depression, albeit with differing designs to this current study (e.g., cross-sectional, case-control, respectively).17,30 Both studies show similar direction of increasing sleep problems with increasing depression, although both studies report stronger direct effect coefficients for the pathway of sleep to depression than this study. One reason may be that those studies used clinical pain populations where the associations are likely to be stronger. However, our study was also exclusively concerned with the subsequent onset of probable depression in persons with new sleep problems in a persistent pain cohort. So, because the current study used restricted samples (i.e., we removed participants who reported sleep problems or probable depression at baseline to ensure new episode development of the predictor), this may have provided a more accurate estimate of the overall effect compared to when prevalent as well as incident sleep problems are considered.
Strengths and Weaknesses
A major strength of this study is the prospective longitudinal design, which has enabled the establishment of a clear time sequence between sleep and depression in those with persistent pain. We are unaware of any other study which has considered such relationships prospectively within a persistent pain cohort. This study's design overcomes some of the current criticisms of previous cross-sectional designs, where cause and effect are less clear.35 In addition, the time sequence design has helped to address the caution noted by Harman et al.,36 that there is a need to consider concurrent depression when assessing sleep problems. This is especially true as sleep problems are considered as a key diagnostic marker of depression.13,37,38 A further strength is the large sample size and the general population sample which enables generalizability for those in the community. A limitation is the subjective measurement of sleep problems, with objective (polysomnography, actigraphy) and subjective (questionnaire, interview, sleep diaries) methodology being preferred.19 However this would not be feasible in such a large epidemiologic study. Future studies would benefit from a greater exploration of the effect of pain interference or pain intensity on sleep, with more focused questions directly linking pain to sleep function both in terms of pain effects specifically during night activities and also reciprocal effects on next day functioning on the perception of pain.19 Another limitation is the time period between follow-up points (3 years), which could be considered as large. It is possible that key variables of interest (e.g., sleep problems, depressive symptoms, pain interference) could have developed and abated, prior to or after each follow-up. However, given the relative stability of the prevalence rates of the key variables at all time points, this seems unlikely. It is also true that while all participants within this cohort have indicated the presence of pain at all time points, they may have had pain-free episodes at any of the periods before and after responding. Nevertheless, previous research has used such categorizations of pain presence over time as a marker for persistent pain,26 and therefore we believe the findings have clinical relevance.
A key aim of this study was to test the hypothesis put forward by Cohen and Rodriguez10 that, in those with pain, one pathway to depression is through sleep problems. We chose an analysis model that utilized validated cutoff points to identify those with probable depression and those with significant sleep problems. While clinically useful (e.g., identification of subgroups who may benefit from treatment), the use of cutoffs may have missed important changes for individuals within those categories (e.g., someone just over the threshold of probable depression who subsequently has much higher levels of depressive symptoms). While we have included possible confounders (age, gender, alcohol use, marital status, employment status),5,30 we were unable to adjust for other potentially important factors (caffeine intake, comorbidity, life events, race, social class, medication use), which may have influenced our findings.39,40 The original cohort, from which this nested cohort has come, experienced loss to follow-up.26 While this may affect the overall proportions of the key variables in this nested cohort, we do not believe it will distinctly alter the association effects, given the stability of the key variables at all time points. It is possible, of course, that similar relationships would be found between sleep and depression in non-pain cohorts, and that there is nothing unique or specific about our findings in relation to the problem of pain. However, given the abundant evidence about the higher rate of sleep problems in pain patients, the independent effects of pain interference increasing risk of both sleep problems and probable depression, and the barrier to the active management of chronic pain represented by the development of depression, the associations we have uncovered here are of particular relevance and importance to the management of patients with persistent pain.
Clinical Relevance
The dual hypotheses tested within this study show the bi-directional relationship between sleep and depression, with both being predictive of each other. This confirms evidence from other longitudinal designs in non-pain populations.40,41 Our findings do show an additive effect of pain interference on the pathway of sleep to probable depression, and vice versa, but this effect is small. It may be, as other evidence has shown, that having pain increases the chance of developing either depression or sleep problems.6,7 Indeed, from our results, pain interference is shown to have independent associations with both sleep and probable depression, doubling the risk of future probable depression (Figure 2) and increasing risk of future sleep problems by over 50% (Figure 3). But once either condition (probable depression, sleep problems) is established, pain interference does not markedly mediate the pathway between the two. Moreover as the further analysis of concurrent influence of predictor variables has shown (i.e., concurrent sleep problems for Model A, concurrent probable depression for Model B), levels of effect are maintained. This finding suggests a compounding effect of sleep problems or depression on each other, which once established (both sleep problems and depression) may make treatment more complex. This therefore highlights the benefit of identifying and treating comorbidity such as this for those with persistent pain before additional problems arise. Also important is the finding that the total effect of sleep problems on the development of probable depression is considerably stronger than the effect of probable depression on sleep problems for those who report persistent pain. This has clinical implications: the clinician may wish to enquire about sleep problems experienced by their pain patients and consider treatment suited to address this. This might be a more acute issue for those actively seeking treatment (i.e., clinical population) compared to this population cohort. Tang and colleagues have shown high rates (> 50%) of clinical insomnia in those with clinical levels of chronic back pain.18 There is evidence that cognitive behavioral treatments of sleep disorders can be helpful in alleviating pain35 and can alter and reduce the severity of depression.13,42 It may be beneficial for clinicians involved in the treatment of those with persistent pain to consider and treat sleep problems alongside pain management.
CONCLUSION
This prospective longitudinal study has shown that a large proportion of those with persistent pain report sleep problems and depressive symptoms. Results show that prior sleep problems treble the risk of developing a probable case of depression. Clinicians may wish to consider treatment options that involve addressing sleep problems for those with persistent pain.
DISCLOSURE STATEMENT
This research was supported by the Wellcome Trust [083572]. The NorStOP study was supported by a Medical Research Council UK Programme Grant (grant code: G9900220) and Support for Science funding secured by the North Staffordshire Primary Care Research Consortium. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Thanks are extended to the research and administrative staff and respondents involved with the NorStOP study.
REFERENCES
- 1.Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet. 1999;354:1248–52. doi: 10.1016/s0140-6736(99)03057-3. [DOI] [PubMed] [Google Scholar]
- 2.Hagen K, Svebak S, Zwart JA. Incidence of musculoskeletal complaints in a large adult Norwegian county population. The HUNT Study. Spine (Phila Pa 1986) 2006;31:2146–50. doi: 10.1097/01.brs.0000231734.56161.6b. [DOI] [PubMed] [Google Scholar]
- 3.Gureje O, Simon GE, Von KM. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 4.Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Perri LM. Psychological aspects of persistent pain: current state of the science. J Pain. 2004;5:195–211. doi: 10.1016/j.jpain.2004.02.576. [DOI] [PubMed] [Google Scholar]
- 5.Magni G, Moreschi C, Rigatti-Luchini S, Merskey H. Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain. 1994;56:289–97. doi: 10.1016/0304-3959(94)90167-8. [DOI] [PubMed] [Google Scholar]
- 6.Carroll LJ, Cassidy JD, Cote P. Factors associated with the onset of an episode of depressive symptoms in the general population. J Clin Epidemiol. 2003;56:651–8. doi: 10.1016/s0895-4356(03)00118-5. [DOI] [PubMed] [Google Scholar]
- 7.Campbell LC, Clauw DJ, Keefe FJ. Persistent pain and depression: a biopsychosocial perspective. Biological Psychiatry. 2003;54:399–409. doi: 10.1016/s0006-3223(03)00545-6. [DOI] [PubMed] [Google Scholar]
- 8.Main CJ, George SZ. Psychologically informed practice for management of low back pain: future directions in practice and research. Phys Ther. 2011;91:820–4. doi: 10.2522/ptj.20110060. [DOI] [PubMed] [Google Scholar]
- 9.van Tulder M, Kovacs F, Muller G, et al. European guidelines for the management of low back pain. Acta Orthop Scan. 2002;73:20–5. doi: 10.1080/000164702760379503. [DOI] [PubMed] [Google Scholar]
- 10.Cohen S, Rodriquez MS. Pathways linking affective disturbances and physical disorders. Health Psychol. 1995;14:374–80. doi: 10.1037//0278-6133.14.5.374. [DOI] [PubMed] [Google Scholar]
- 11.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 12.Lustberg L, Reynolds CF. Depression and insomnia: questions of cause and effect. Sleep Med Rev. 2000;4:253–62. doi: 10.1053/smrv.1999.0075. [DOI] [PubMed] [Google Scholar]
- 13.Riemann D, Berger M, Voderholzer U. Sleep and depression--results from psychobiological studies: an overview. Biol Psychol. 57:67–103. doi: 10.1016/s0301-0511(01)00090-4. 2001l. [DOI] [PubMed] [Google Scholar]
- 14.Von KM. Case definitions in primary care. The need for clinical epidemiology. Gen Hosp Psychiatry. 1992;14:293–5. doi: 10.1016/0163-8343(92)90062-f. [DOI] [PubMed] [Google Scholar]
- 15.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 16.Smith MT, Quartana PJ, Okonkwo RM, Nasir A. Mechanisms by which sleep disturbance contributes to osteoarthritis pain: a conceptual model. Curr Pain Headache Rep. 2009;13:447–54. doi: 10.1007/s11916-009-0073-2. [DOI] [PubMed] [Google Scholar]
- 17.Miro E, Martinez MP, Sanchez AI, Prados G, Medina A. When is pain related to emotional distress and daily functioning in fibromyalgia syndrome? The mediating roles of self-efficacy and sleep quality. Br J Health Psychol. 2011;16:799–814. doi: 10.1111/j.2044-8287.2011.02016.x. [DOI] [PubMed] [Google Scholar]
- 18.Tang NK, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J Sleep Res. 2007;16:85–95. doi: 10.1111/j.1365-2869.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- 19.Kelly GA, Blake C, Power CK, O'Keeffe D, Fullen BM. The association between chronic low back pain and sleep: a systematic review. Clin J Pain. 2011;27:169–81. doi: 10.1097/AJP.0b013e3181f3bdd5. [DOI] [PubMed] [Google Scholar]
- 20.Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. 2010;14:35–46. doi: 10.1016/j.smrv.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Lautenbacher S. Pain, sleeping problems and their many relatives. Pain. 2012;153:1138. doi: 10.1016/j.pain.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Thomas E, Wilkie R, Peat G, Hill S, Dziedzic K, Croft P. The North Staffordshire Osteoarthritis Project--NorStOP: prospective, 3-year study of the epidemiology and management of clinical osteoarthritis in a general population of older adults. BMC Musculoskelet Disord. 2004;5:2. doi: 10.1186/1471-2474-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jordan KP, Thomas E, Peat G, Wilkie R, Croft P. Social risks for disabling pain in older people: a prospective study of individual and area characteristics. Pain. 2008;137:652–61. doi: 10.1016/j.pain.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 24.Bowling A. Research methods in health. Buckingham: Open University Press; 1997. [Google Scholar]
- 25.Lacey RJ, Lewis M, Jordan K, Jinks C, Sim J. Interrater reliability of scoring of pain drawings in a self-report health survey. Spine (Phila Pa 1986) 2005;30:E455–8. doi: 10.1097/01.brs.0000174274.38485.ee. [DOI] [PubMed] [Google Scholar]
- 26.Thomas E, Mottram S, Peat G, Wilkie R, Croft P. The effect of age on the onset of pain interference in a general population of older adults: prospective findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2007;129:21–7. doi: 10.1016/j.pain.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]
- 28.Boardman HF, Thomas E, Millson DS, Croft PR. Psychological, sleep, lifestyle, and comorbid associations with headache. Headache. 2005;45:657–69. doi: 10.1111/j.1526-4610.2005.05133.x. [DOI] [PubMed] [Google Scholar]
- 29.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 30.Naughton F, Ashworth P, Skevington SM. Does sleep quality predict pain-related disability in chronic pain patients? The mediating roles of depression and pain severity. Pain. 2007;127:243–52. doi: 10.1016/j.pain.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 31.West SG, Hepworth JT. Statistical issues in the study of temporal data: daily experiences. J Pers. 1991;59:609–62. doi: 10.1111/j.1467-6494.1991.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 32.Ender P. Mediation with binary mediator and/or response variables. UCLA. Academic Technology Services, Statistical Consulting Group. 2001. Accessed March 2012. http://www.ats.ucla.edu/stat/stata/faq/binary_mediation.htm.
- 33.MacKinnon D, Dwyer J. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1988. [Google Scholar]
- 35.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8:119–32. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 36.Harman K, Pivik RT, D'Eon JL, Wilson KG, Swenson JR, Matsunaga L. Sleep in depressed and nondepressed participants with chronic low back pain: electroencephalographic and behaviour findings. Sleep. 2002;25:775–83. [PubMed] [Google Scholar]
- 37.Manber R, Blasey C, Arnow B, et al. Assessing insomnia severity in depression: comparison of depression rating scales and sleep diaries. J Psychiatr Res. 2005;39:481–8. doi: 10.1016/j.jpsychires.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 38.Council on Scientific Affairs, American Medical Association. The etiologic features of depression in adults. Arch Fam Med. 1993;2:76–83. doi: 10.1001/archfami.2.1.76. [DOI] [PubMed] [Google Scholar]
- 39.Ohayon MM. Relationship between chronic painful physical condition and insomnia. J Psychiatr Res. 2005;39:151–9. doi: 10.1016/j.jpsychires.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 41.Kaneita Y, Yokoyama E, Harano S, et al. Associations between sleep disturbance and mental health status: a longitudinal study of Japanese junior high school students. Sleep Med. 2009;10:780–6. doi: 10.1016/j.sleep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 42.Berk M. Sleep and depression - theory and practice. Aust Fam Physician. 2009;38:302–4. [PubMed] [Google Scholar]