Abstract
Background:
To characterize cross-cultural sleep patterns and sleep problems in a large sample of mothers of children (ages birth to 6 years) in multiple predominantly Asian and predominantly Caucasian countries.
Methods:
Mothers of 10,085 young children (predominantly Asian countries/regions: China, Hong Kong, India, Korea, Japan, Malaysia, Philippines, Singapore, Thailand; predominantly Caucasian countries: Australia, Canada, New Zealand, United Kingdom, United States) completed an internet-based expanded version of the Pittsburgh Sleep Quality Index.
Results:
Mothers in predominantly Asian countries/regions had later bedtimes, decreased number and duration of night wakings, more nighttime sleep, and more total sleep than mothers from predominantly Caucasian countries, P < 0.001. More than half (54.7%) of mothers reported having poor sleep, ranging from 50.9% of mothers in Malaysia to 77.8% of mothers in Japan. Sleep disturbance symptoms were quite common, especially symptoms related to insomnia, and were more likely to be reported by mothers in predominantly Caucasian countries. However, psychosocial factors, including having children of a younger age, being unemployed, and having a lower education level were the best predictors of poor sleep, whereas culture was not a significant predictor.
Conclusions:
Overall, mothers in predominantly Asian countries/regions reported later bedtimes but sleeping better and longer than mothers from predominantly Caucasian countries, which is dissimilar to cross-cultural findings of young children. Psychosocial factors were found to be the best predictors of poor sleep, irrespective of culture. Further studies are needed to understand the impact of these findings.
Citation:
Mindell JA; Sadeh A; Kwon R; Goh DYT. Cross-cultural comparison of maternal sleep. SLEEP 2013;36(11):1699-1706.
Keywords: Sleep, maternal, mother, adult, cross-cultural
INTRODUCTION
Sleep disturbances are highly prevalent in the general population and may particularly affect women.1 Furthermore, cultural context appears to play a role in individual sleep patterns and sleep complaints. The Study of Women's Health Across the Nation (SWAN) found in a sample of 12,603 women (ages 40-55) that 38% of women reported significant sleep disturbances.2 In this study, conducted in the United States, Caucasian women were more likely to report sleep difficulties (40%) than Japanese women (28%). In one cross-cultural study of adult sleep utilizing data collected from 16,483 university students (men and women) from 24 countries, results indicated significant differences in total sleep times across countries, with shortest total sleep times in Japan, Korea, and Taiwan.3 Finally, a recent large-scale study of survey data collected through the World Health Organization found that 16.9% of adults reported severe/extreme sleep problems, with prevalence rates ranging from 3.9% in Indonesia and Kenya to 40.0% in Bangladesh. In all eight countries surveyed, women reported higher rates of sleep complaints.1
The few cross-cultural studies conducted on women have looked at university students and older women. However, sleep of women is likely to be influenced by their children's sleep, especially those who have young children, thus making mothers particularly vulnerable to sleep problems. Studies on maternal sleep have primarily focused on the immediate post-partum period, indicating increased sleep disruption and insufficient sleep.4–7 Those studies that have been conducted past the newborn period have mostly focused on sleep in parents who are caregivers of children with medical issues (e.g., epilepsy, physically disabled, asthma, and cystic fibrosis),8–10 with no studies on sleep in mothers of typical children. Recent research has demonstrated that cross-cultural differences in sleep patterns are already evident in infancy and early childhood. A recent study of almost 30,000 young children (birth to 3 years) found that children from predominantly Asian countries had significantly later bedtimes, shorter total sleep times, and increased parental perception of sleep problems compared with children from predominantly Caucasian countries/regions.11
Overall, there has been little research comparing adult sleep across different countries in the world and a lack of data from some countries/regions, especially in terms of maternal sleep. As a start to collecting normative data on maternal sleep throughout the world, this study focuses on predominantly Caucasian and predominantly Asian countries/regions in North America, United Kingdom, and Asia-Pacific. Thus, the primary objective of this study was to characterize sleep patterns, sleep behaviors, and sleep problems in a large sample of mothers of children (ages birth to 6 years) in multiple predominantly Asian and predominantly Caucasian countries/regions.
METHODS
Participants
Mothers of 10,085 young children (830 Australia-New Zealand/AU-NZ, 749 Canada/CA, 1,215 China/CN, 586 Hong Kong/HK, 998 India/IN, 712 South Korea/KR, 499 Japan/JP, 513 Malaysia/MY, 396 Philippines/PH, 449 Singapore/SG, 565 Thailand/TH, 1,335 United States/US, and 1,238 United Kingdom/UK) participated in this study. Countries/regions were grouped as either predominantly Caucasian ([P-C] Australia, Canada, New Zealand, United Kingdom, and United States) or predominantly Asian ([P-A] China, Hong Kong, India, Japan, Korea, Singapore, Malaysia, Philippines, and Thailand).
The participants all had children between the ages of birth to 6 years, with children grouped according to the following ages: 0- to 2-month olds (n = 1,276), 3- to 11-month olds (n = 2,242), 12- to 23-month olds (n = 2,095), 24- to 35-month olds (n = 1,886), 36- to 47-month olds (n = 1,088), 48- to 59-month olds (n = 947), and 60- to 71-month olds (n = 551). Sample sizes were based on urban population, with a target of 800 participants for each country/region with < 100 million urban inhabitants and 1,200 participants for urban populations > 100 million. Data collection in each country/region was terminated when the target sample size was fulfilled.
Procedure
All data were collected online. In almost all countries/regions (Australia, China, India, Malaysia, Singapore, Philippines, UK, US), the questionnaire was set as a pop-up screen at a popular parenting website (BabyCenter). In 2 countries (Japan and Korea), recruitment was conducted via email utilizing mailing lists obtained from local marketing firms, and online advertising at other parenting sites. Completion of the questionnaire was voluntary; there were no exclusionary criteria; and this study was approved by an independent institutional review board. No identifying information was collected. A few areas offered incentives for completion (e.g., free samples or gift voucher), and participants were asked to provide their email address at the end of the survey if they were interested. The complete sample was collected between February 2011 and March 2012.
All participants completed the Pittsburgh Sleep Quality Index (PSQI).12,11 The PSQI is a widely used and well-validated 19-item self-report instrument that measures sleep disturbances in adults.13 The PSQI includes 7 subscale scores (sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, sleep medications, and daytime dysfunction), and provides a global score ranging from no sleep difficulty to severe difficulties. A global score > 5 indicates a “poor sleeper” and has been shown to have a diagnostic sensitivity of 89.6% and specificity of 86.5%.13 The expanded version of the PSQI used in this study included additional questions about night wakings and naps, but these additional questions were not included in the global score. Mothers completed this measure regarding their own sleep over the past 2 weeks rather than the past month to be consistent with other measures collected. The questionnaire was translated into each respective language and back-translated to ensure appropriate translation. For quality control, respondents could not provide extreme data (e.g., sleep onset latency > 5 h, total sleep time < 3 h).
In addition to the PSQI, demographic information was collected, including parental age, education, race, and employment status.
Statistical Analyses
Means and frequencies were used for demographic information. Analyses of variance were used to compare sleep variables across countries, with effect sizes (partial eta-squared) reported for all comparisons. Multivariate analysis of covariance analyses (MANCOVA) were performed on the following continuous variables: (1) bedtime (2) sleep onset latency, (3) duration and number of night wakings, (4) nighttime sleep, (5) wake time, (5) total sleep time, (6) daytime sleep (naps), and (7) PSQI score. In these analyses, the variables of mother's age, child's age, maternal education, and employment status (employed vs not employed) were used as covariates to control for their effects. Logistic regression was used to test the prediction of poor sleepers based on the PSQI. Chi-square analyses were conducted for categorical variables, including percent of poor sleepers (PSQI), percent of short sleepers (≤ 6 h) and sleep disturbance variables. Effect sizes reported for χ2 analyses are phi (φ). Logistic regression utilizing culture (P-A vs P-C), education level, employment status (employed vs non-employed), number of children, and child's and mother's age as predictors was conducted to predict poor versus good sleep using the PSQI total score (> 5 = poor). Because of the large cohort size and the multiple analyses, findings were considered significant if P < 0.001.
RESULTS
Demographics
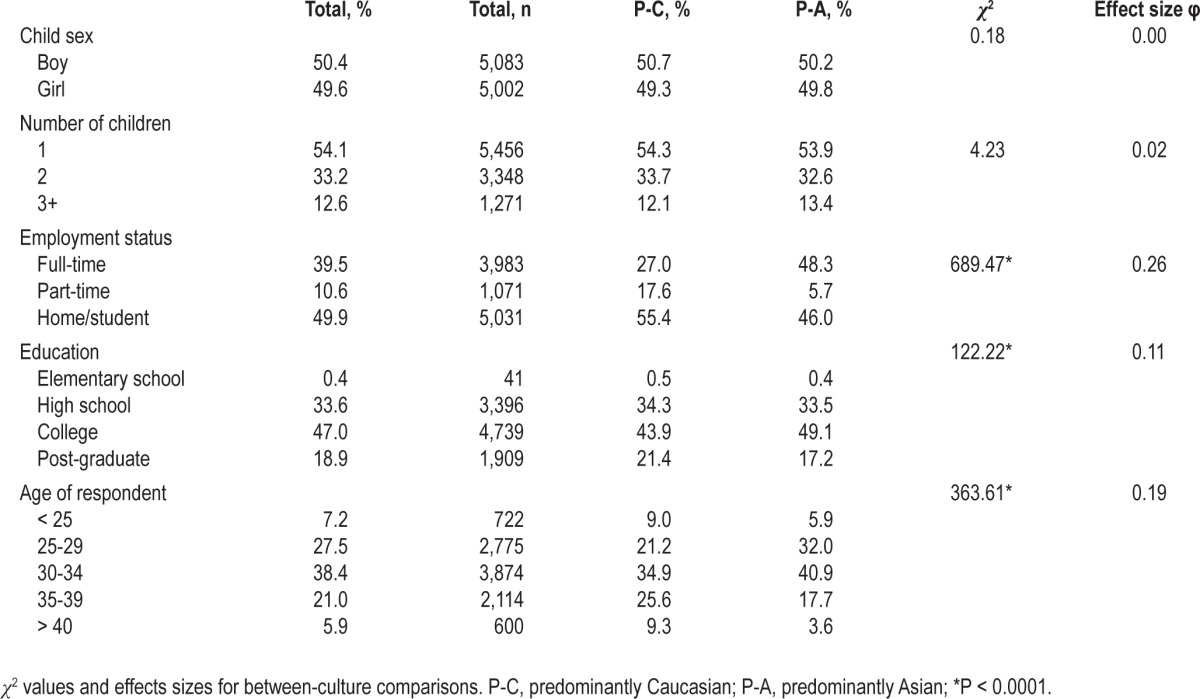
Complete demographic data for the entire sample, and within P-A and P-C, are provided in Table 1. Overall, there were an equal number of mothers of boys (50.4%) and girls (49.6%); approximately half of the respondents had just one child (54.1%). The average child age was 23.58 months (SD 18.86), with no difference between P-C (M 23.51) and P-A (M 23.64), P > 0.05. The majority of respondents (65.9%) were between 25 and 35 years old; most had a college education (65.9%); and almost half were at home full-time or were students (49.9%). There were significant differences between P-A and P-C for age of respondent, education of respondent, and employment status.
Table 1.
Participant demographics
Sleep Patterns
Data on nighttime and daytime sleep (see Table 2, 3, and 4) are presented for each country/region, as well as for predominantly Caucasian (P-C) and predominantly Asian (P-A). The MANCOVAs revealed an overall significant effect for the independent variables country (Wilks' lambda = 0.62; F = 44.3; P < 0.0001) and region (P-C vs. P-A; Wilks' lambda = 0.91; F = 113.2; P < 0.0001). All sleep measures significantly differed across country/region, with the greatest differences seen in bedtimes. Comparisons for all variables were also significant between P-C and P-A, except for wake times (see Table 4). Overall, mothers in P-A had later bedtimes, decreased number and duration of night wakings, more nighttime sleep, and more total sleep, although there were minimal effect sizes for these variables. Figures 1 and 2 present both bedtimes and total sleep (nighttime sleep + daytime sleep) across countries. Bedtimes were significantly later in P-A countries, with a difference of 1.5 hours. However, nighttime sleep was quite similar across all countries/regions, with the exception of Korea and China, with mothers in China and Korea obtaining 1 to 1.5 h more sleep than mothers in all other countries/regions. The percent of mothers with short sleep duration (≤ 6 h) was also calculated (see Figure 3). Overall, 25.7% of mothers obtained short sleep, with no significant differences between P-C and P-A, χ2 = 1.15, P = 0.284. There were, however, vast country-based differences in prevalence ranging from 8.8% (CN) to 40.0% (SG), P < 0.001.
Table 2.
Nighttime sleep variables across countries
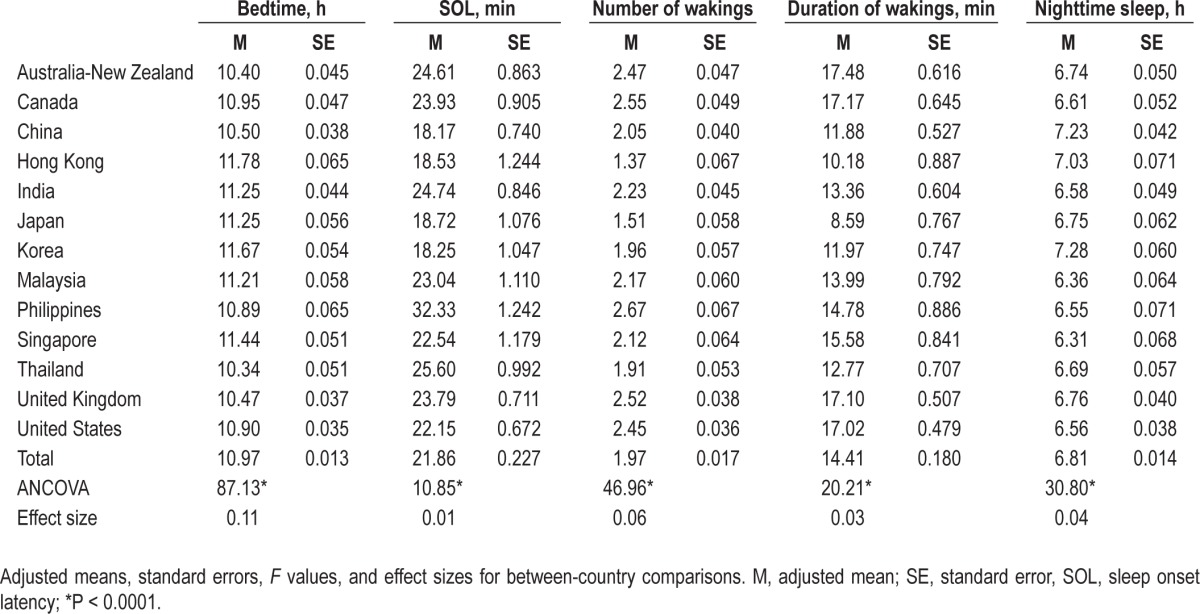
Table 3.
Daytime sleep variables across countries
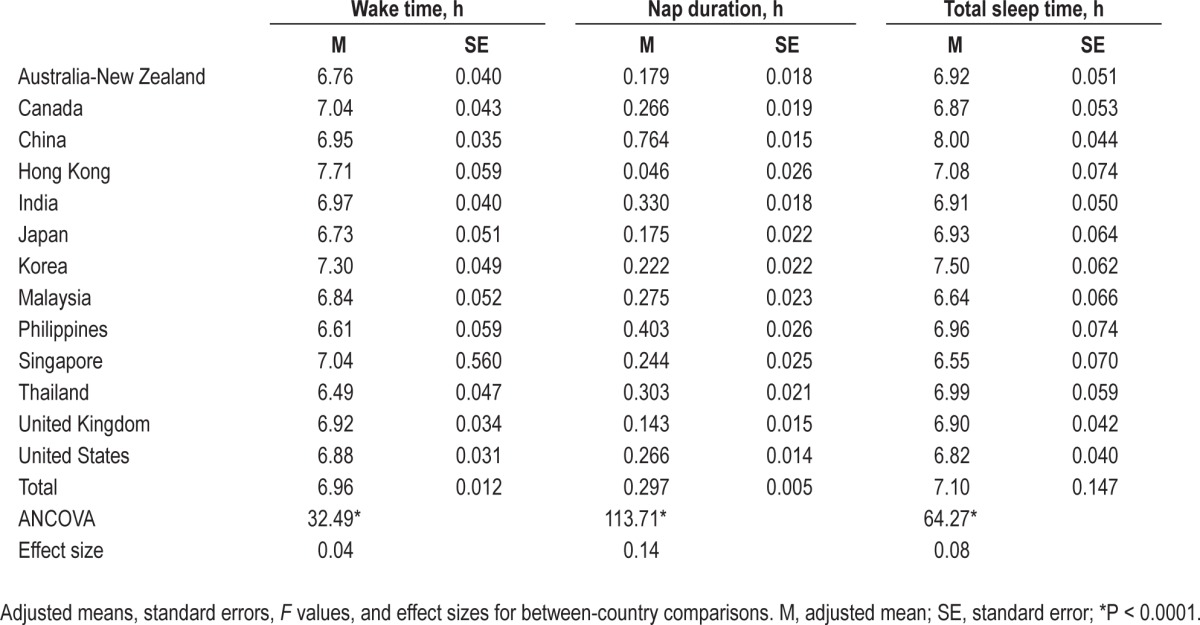
Table 4.
Sleep measures of predominantly Caucasian and predominantly Asian
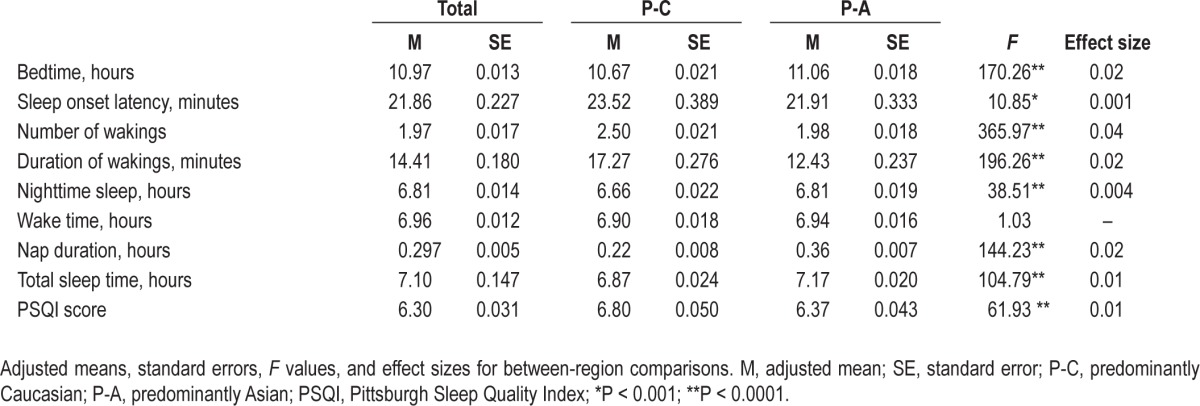
Figure 1.
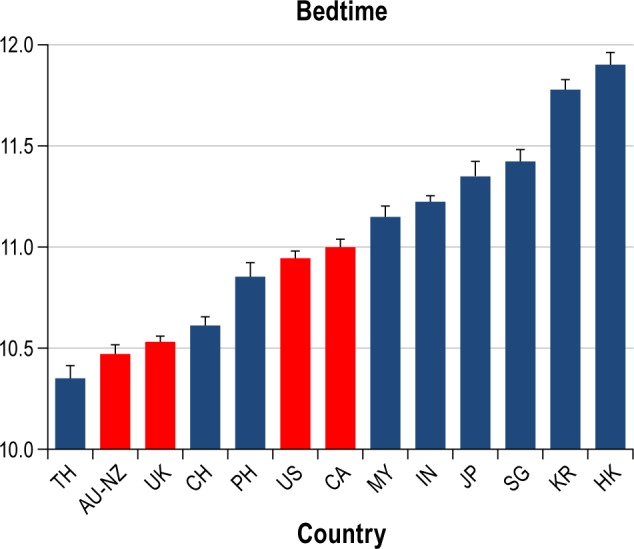
Bedtimes across countries. Predominantly Asian countries in blue, predominantly Caucasian countries in red. AU-NZ, Australia-New Zealand; CA, Canada; CN, China; HK, Hong Kong; IN, India; KR, South Korea; JP, Japan; MY, Malaysia; PH, Philippines; SG, Singapore; TH, Thailand; UK, United Kingdom; US, United States.
Figure 2.
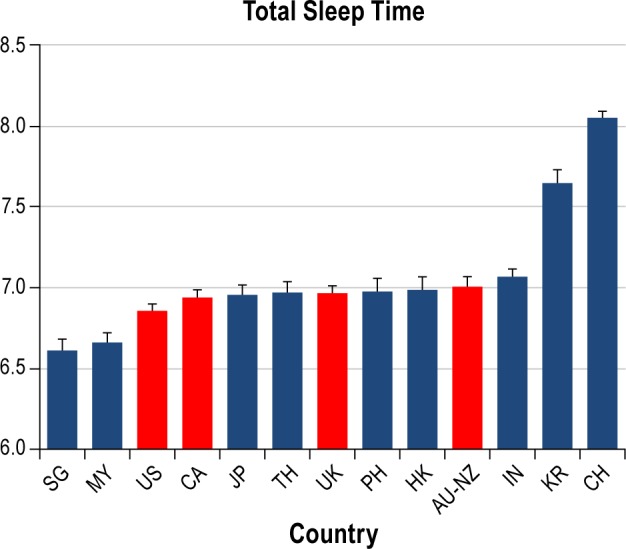
Total sleep times across countries. Predominantly Asian countries in blue, predominantly Caucasian countries in red. AU-NZ, Australia-New Zealand; CA, Canada; CN, China; HK, Hong Kong; IN, India; KR, South Korea; JP, Japan; MY, Malaysia; PH, Philippines; SG, Singapore; TH, Thailand; UK, United Kingdom; US, United States.
Figure 3.
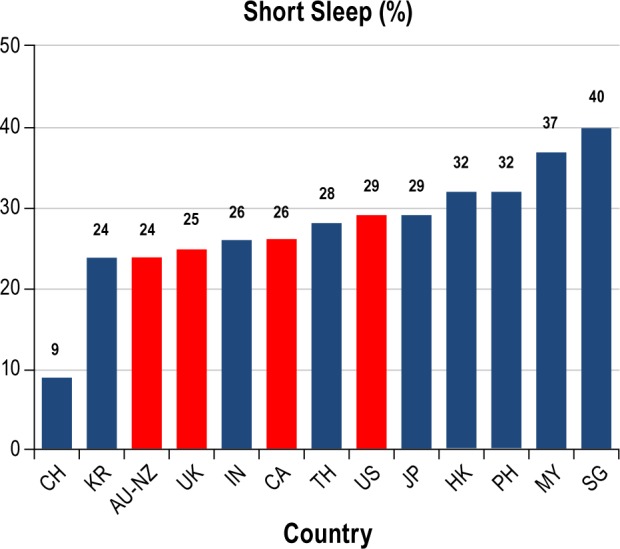
Percent short sleep duration across countries. Predominantly Asian countries in blue, predominantly Caucasian countries in red. AUNZ, Australia-New Zealand; CA, Canada; CN, China; HK, Hong Kong; IN, India; KR, South Korea; JP, Japan; MY, Malaysia; PH, Philippines; SG, Singapore; TH, Thailand; UK, United Kingdom; US, United States.
Mothers who worked full-time (n = 3,983) compared to mothers who worked part-time or were not employed (n = 6,102) had earlier bedtimes (10.84 vs 11.06), fell asleep quicker (19.96 vs 23.10 min), had fewer number and shorter duration of night wakings (1.82 times for 13.16 min vs 2.07 times for 15.20 min), and earlier wake times (6.67 vs 7.15), P < 0.0001. Interestingly, there were no differences in total nighttime sleep (6.79 vs 6.82 h), P = 0.41. However, full-time working mothers obtained less overall sleep across the 24-h day (6.99 vs 7.12 h), P < 0.0001.
Similarly, mothers of ≥ 3 children had more night wakings (1.96 vs 1.93 vs 2.15 wakings, respectively, for 1 child, 2 children, or ≥ 3 children), earlier wake times (7.02 vs 6.92 vs 6.81), less total nighttime sleep (6.85 vs 6.84 vs 6.63 h), and less total sleep (7.16 vs 7.11 vs 6.87 h), P < 0.0001. There were no differences in bedtimes (11.00 vs 10.93 vs 10.94), sleep onset latency (21.96 vs 21.26 vs 22.59 min), or night waking duration (14.30 vs 14.61 vs 15.25 min), P > 0.05.
Sleep Disturbances
Utilizing the PSQI global score, more than half (54.7%) of mothers reported poor sleep, ranging from 50.9% of mothers in Malaysia to 77.8% of mothers in Japan (Table 5, Figure 4). Sleep disturbance symptoms were quite common, especially symptoms related to insomnia, including taking > 30 min to fall asleep (12.3%) and waking during the night or too early in the morning (37.0%). These symptoms were more likely to be reported by mothers in predominantly Caucasian countries than mothers from predominantly Asian countries/regions (14.8% vs 10.6% for prolonged sleep onset latency; 46.2% vs 30.6% for night wakings or early morning awakenings), P < 0.0001. Approximately 5% of mothers reported loud snoring, with a similar percentage reporting trouble staying awake during the day (3.9%) and experiencing a lack of enthusiasm (5.5%).
Table 5.
Percent sleep problems (3 or more times per week)
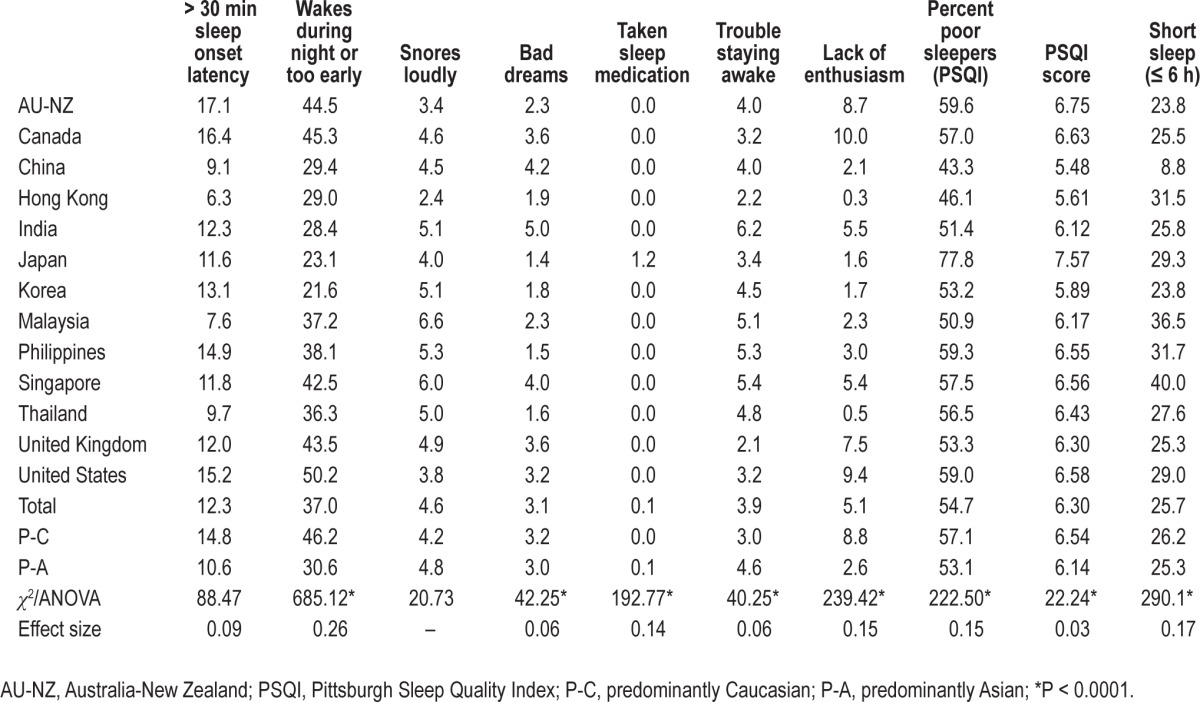
Figure 4.
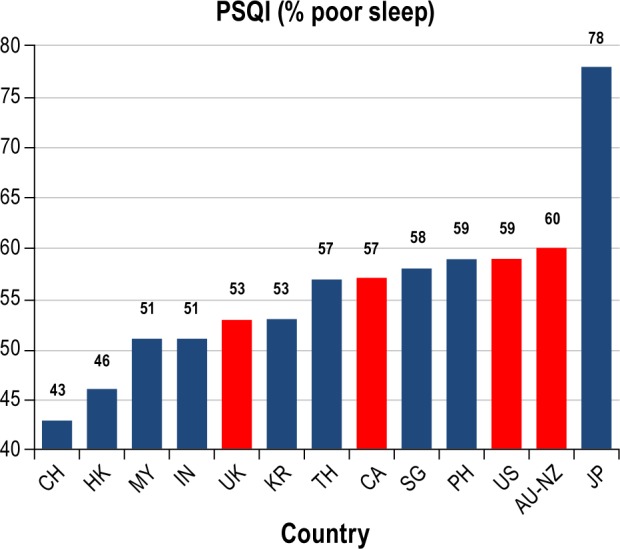
Percent poor sleepers across countries. Predominantly Asian countries in blue, predominantly Caucasian countries in red. AU-NZ, Australia-New Zealand; CA, Canada; CN, China; HK, Hong Kong; IN, India; KR, South Korea; JP, Japan; MY, Malaysia; PH, Philippines; SG, Singapore; TH, Thailand; UK, United Kingdom; US, United States.
Full-time working mothers had lower average PSQI scores (5.88 vs 6.58), with 48.4% of mothers employed full-time classified as poor sleepers compared to 58.8% of other mothers, P < 0.0001. Mothers with more children were significantly likely to have poorer PSQI scores (6.17 vs 6.37 vs 6.71), with 59.4% of mothers of ≥ 3 children classified as poor sleepers compared to 56.3% of mothers with 2 children and 47.1% of mothers of just one child, P < 0.0001.
Finally, the global analysis to predict poor versus good sleep (PSQI total score > 5 = poor), utilizing culture (P-A vs P-C), education level, employment status (employed vs non-employed), number of children, and child's and mother's age as predictors, was highly significant, χ2 = 262, P < 0.0001. Child's age (odds ratio = 1.10; CL = 1.07-1.12; Wald χ2 = 63.55), maternal education (odds ratio = 1.14; CL = 1.07-1.13; Wald χ2 = 38.11), and employment status (odds ratio = 0.65; CL. = 0.60-0.70; Wald χ2 = 113.68) were all significant predictors (P < 0.0001). Younger child, not being employed, and lower education level predicted higher likelihood of having poor sleep. Region (P-C vs P-A) was not found to be a significant predictor in this analysis.
DISCUSSION
This is the only large-scale cross-cultural survey of maternal sleep to date, and involves a large cohort of predominantly Caucasian and predominantly Asian mothers across 14 countries/regions. The most striking results of this study were the high percentage of mothers who were poor sleepers (PSQI score > 5) and getting insufficient sleep. Overall, 55% of mothers were found to be poor sleepers, ranging from 43% in China to 78% in Japan. This global score greater than 5 indicates that an individual is having severe difficulties in at least two sleep-related areas, or moderate difficulties in more than three areas.13 Other studies have found similar rates of poor sleeping in women. For example, a study that included 300 women from Taiwan found that 48% were considered poor sleepers.14 Similarly, in another study of older black and white women in the United States, 52% were classified as poor sleepers.15 In contrast, a lower prevalence of poor sleepers was found in a study conducted in Tehran, with 35% of women noted to be poor sleepers.16
Surprisingly, in our study only 3.9% of mothers reported having difficulty staying awake during the day, and only 5.1% indicated a lack of enthusiasm. The prevalence of these self-reported symptoms is lower than reported in other studies of women, although it is difficult to compare as the wording of the questions is different. For example, a study of 7,051 women in Sweden reported prevalence rates of 16.1% for excessive daytime sleepiness and 14.3% for fatigue.17 In this Swedish study, having children did not increase the risk for these daytime symptoms, which is similar to other studies of large samples of women.18 Not only was the risk not increased, but rather having children, as well as the total number of children, was actually negatively associated with reports of daytime sleepiness. The results of our survey, however, indicate that on a more global level the more children a women has, the more likely she is to have poor sleep, as well as later bedtimes, more night wakings, and less overall sleep. It may be that women of young children, although getting less sleep and having poorer sleep, need to be highly active throughout the day and are either able to compensate for insufficient sleep or ignore these feelings. These findings are consistent with other studies that have found that young women may be more resilient to sleep disruption.19 Furthermore, employment status had an interesting effect in our study, with mothers employed full-time outside the home getting more sleep and overall being more likely to be classified as good sleepers. It may be that these women are more likely to have additional help within the home or maintain more strict sleep schedules for themselves, and possibly their children. Further research needs to explore this finding of a positive relationship between full-time employment and sleep patterns and sleep disturbances. Interestingly, these psychosocial factors, including having children of a younger age, being unemployed, and having a lower educational level, were found to be the best predictors of poor sleep, irrespective of culture. These results are consistent with previous studies on the role of psychosocial factors, especially socioeconomic status, in women's poor sleep.20,21
As mentioned above, another interesting finding was the total sleep times obtained by the women in this study. Overall, women averaged 6.8 hours at night and 7.1 hours total sleep time. These amounts are lower compared to other normative samples. For example, studies of women in the immediate postpartum period found averages of 7.2 hours at night,7 and another study found total sleep time of 7.8 hours.22 Furthermore, in our study 26% of the mothers surveyed had short sleep duration (≤ 6 h). Such short sleep duration has been associated with significant performance deficits, cardiovascular risk, obesity, increased risk of motor vehicle accidents related to drowsy driving, and general health/psychological stress,23 which is concerning, especially in this particular population.
Another striking finding of this study was that total sleep times were remarkably consistent across countries, other than those mothers in China and Korea who obtained significantly more sleep. This result is quite different from our previous cross-cultural study of young children (birth to age 3) across the same countries/regions.11 In that study, there were vast country-based differences, as total sleep times varied by 101 minutes (11.62 h in Japan compared to 13.31 in New Zealand). Looking more specifically at the percentage of mothers with short sleep duration, country-based differences become more apparent, with prevalence rates ranging for most countries from 24% to 32%, although in China it was only 9% and in Singapore it was as high as 40%. This consistency in total sleep times is surprising given the vast country-based differences in bedtimes, ranging from 10:21 (Thailand) to 11:54 (Hong Kong), a range of over 1.5 hours. Differences in wake times and napping appear to compensate for the late bedtimes in some countries, resulting in these quite similar total sleep times.
As with all studies there are a number of limitations that must be considered when interpreting these findings. First, as can be expected from an Internet-based survey, the cohort in this study is skewed toward higher education. This bias, however, was likely consistent across all countries and we believe that we obtained similar segments of the population within each country/region. In addition, these results are likely not representative of all mothers within each country. We expect that this sample represents more urban-based populations, especially in the predominantly Asian countries, given the need for internet access to participate. Given that this was primarily a web-based study, it was also not possible to control for the possibility that participants completed the survey more than once or that the person actually had a child. However, cases with unreasonable responses were removed to exclude random or inconsistent data entry. This is an inherent limitation to web-based surveys. Mothers with concerns about their or their child's sleep also may have been more likely to participate, but again, it is expected that these differences are likely consistent across all countries. Finally, as always, the reliance on self-report has inherent limitations. Although the Pittsburgh Sleep Quality Index is a widely used instrument, there is the possibility that given that this is reported sleep, individuals in different cultures may have different subjective perceptions or response sets (e.g., for reporting difficulties). Finally, other basic sociodemographic information, such as socioeconomic status, marital status, household conditions (e.g., living with partner, living with parents), body weight, as well as physical and mental health status, were not collected, which may be important influences on maternal sleep.
Overall, this study is the first study to provide normative data of sleep for women of young children (birth to 6 years), across a large cross-cultural sample. A large percentage of these mothers experience poor sleep and a substantial number do not get adequate sleep. These results also indicate moderate cross-cultural differences in sleep patterns in maternal sleep; results that are not as dramatic as the cross-cultural differences in sleep in young children from these same countries/regions. These results, however, do provide a cultural perspective that can serve clinicians to be aware of normative sleep practices. Finally, further studies are needed to understand the impact of the poor sleep and sleep loss experienced by many mothers, as well as there is a need to expand our study of maternal sleep to other areas of the world (e.g., Latin America, Europe, Africa).
DISCLOSURE STATEMENT
This study was supported by Asia Pacific Pediatric Sleep Association (APPSA) and sponsored by Johnson & Johnson Consumer & Personal Products Worldwide, a division of Johnson & Johnson Consumer Companies, Inc. Dr. Mindell has served as a consultant and speaker for Johnson & Johnson. Dr. Sadeh has served as a consultant for Johnson & Johnson. Dr. Goh has served as a speaker for Johnson & Johnson. Dr. Kwon is an employee of Johnson & Johnson.
ABBREVIATIONS
- SD
standard deviation
- PSQI
Pittsburgh Sleep Quality Index
- P-A
predominantly Asian
- P-C
predominantly Caucasian
- AU-NZ
Australia-New Zealand
- CA
Canada
- CN
China
- HK
Hong Kong
- IN
India
- JP
Japan
- KR
South Korea
- MY
Malaysia
- PH
Philippines
- SG
Singapore
- TH
Thailand
- UK
United Kingdom
- US
United States
REFERENCES
- 1.Stranges S, Tigbe W, Gomez-Olive FX, Thorogood M, Kandala NB. Sleep problems: an emerging global epidemic? findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. 2012;35:1173–81. doi: 10.5665/sleep.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003;10:19–28. doi: 10.1097/00042192-200310010-00005. [DOI] [PubMed] [Google Scholar]
- 3.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166:1689–92. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong KL, Van Haeringen AR, Dadds MR, Cash R. Sleep deprivation or postnatal depression in later infancy: separating the chicken from the egg. J Paediatr Child Health. 1998;34:260–2. doi: 10.1046/j.1440-1754.1998.00213.x. [DOI] [PubMed] [Google Scholar]
- 5.Dorheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32:847–55. doi: 10.1093/sleep/32.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal D, Gay C, Lee K. Fragmented maternal sleep is more strongly correlated with depressive symptoms than infant temperament at three months postpartum. Arch Womens Ment Health. 2009;12:229–37. doi: 10.1007/s00737-009-0070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montgomery-Downs HE, Insana SP, Clegg-Kraynok MM, Mancini LM. Normative longitudinal maternal sleep: the first 4 postpartum months. Am J Obstetr Gynecol. 2010;203:465.e1–7. doi: 10.1016/j.ajog.2010.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaki D, Goldbart A, Daniel S, Fraser D, Shorer Z. Pediatric epilepsy and parental sleep quality. J Clin Sleep Med. 2011;7:502–6. doi: 10.5664/JCSM.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yılmaz O, Sogut A, Gulle S, Can D, Ertan P, Yuksel H. Sleep quality and depression–anxiety in mothers of children with two chronic respiratory diseases: Asthma and cystic fibrosis. J Cyst Fibros. 2008;7:495–500. doi: 10.1016/j.jcf.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda T, Nagai T, Kato-Nishimura K, Mohri I, Taniike M. Sleep problems in physically disabled children and burden on caregivers. Brain Dev. 2012;34:223–9. doi: 10.1016/j.braindev.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Mindell JA, Sadeh A, Wiegand B, How TH, Goh DY. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11:274–80. doi: 10.1016/j.sleep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Sadeh A. A brief screening questionnaire for infant sleep problems: Validation and findings for an Internet sample. Pediatrics. 2004;113:e570–e7. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 13.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 14.Ko SH, Chang SC, Chen CH. A comparative study of sleep quality between pregnant and nonpregnant Taiwanese women. J Nurs Scholarsh. 2010;42:23–30. doi: 10.1111/j.1547-5069.2009.01326.x. [DOI] [PubMed] [Google Scholar]
- 15.Beaudreau SA, Spira AP, Stewart A, et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med. 2012;13:36–42. doi: 10.1016/j.sleep.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asghari A, Farhadi M, Kamrava SK, Ghalehbaghi B, Nojomi M. Subjective sleep quality in urban population. Arch Iran Med. 2012;15:95–8. [PubMed] [Google Scholar]
- 17.Theorell-Haglöw J, Lindberg E, Janson C. What are the important risk factors for daytime sleepiness and fatigue in women? Sleep. 2006;29:751–7. doi: 10.1093/sleep/29.6.751. [DOI] [PubMed] [Google Scholar]
- 18.Baker FC, Wolfson AR, Lee KA. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: findings from the 2007 National Sleep Foundation “Sleep in America Poll”. J Women's Health. 2009;18:841–9. doi: 10.1089/jwh.2008.0986. [DOI] [PubMed] [Google Scholar]
- 19.Bixler EO, Papaliaga MN, Vgontzas AN, et al. Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J Sleep Res. 2009;18:221–8. doi: 10.1111/j.1365-2869.2008.00713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soltani M, Haytabakhsh MR, Najman JM, et al. Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Arch Womens Ment Health. 2012;15:237–47. doi: 10.1007/s00737-012-0281-3. [DOI] [PubMed] [Google Scholar]
- 21.Lallukka T, Sares-Jaske L, Kronholm E, et al. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health. 2012;12:565. doi: 10.1186/1471-2458-12-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dorheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Subjective and objective sleep among depressed and non-depressed postnatal women. Acta Psychiatr Scand. 2009;119:128–36. doi: 10.1111/j.1600-0447.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 23.Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–47. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


