Abstract
Objectives:
To examine the association between snoring and incident cardiovascular disease (CVD).
Design, Settings, and Participants:
This is a prospective study in which community dwelling older adults were evaluated at baseline, and followed up for an average of 9.9 years.
Measurements:
Data on snoring, daytime sleepiness, as well as demographic and clinical characteristics of study participants was collected at baseline, and participants were followed up every six months for an average of 9.9 years. Based on snoring and sleepiness status, 4 groups of participants were created: (1) No Snoring, No Sleepiness; (2) No Snoring, Sleepiness; (3) Snoring, No Sleepiness; (4) Snoring, Sleepiness. Incident CVD was defined as a diagnosis of myocardial infarction, angina pectoris, or congestive heart failure that resulted in overnight hospitalization during the follow-up period. Cox proportional hazard was used to estimate the risk of incident cardiovascular disease during follow-up by baseline snoring and sleepiness status.
Results:
A total of 2,320 participants with a mean age of 73.6 (2.9) years at baseline were included in the analysis. Fifty-two percent were women, and 58% were white. A total of 543 participants developed CVD events during the follow-up period. Participants who reported snoring associated with daytime sleepiness had significantly increased hazard ratio for CVD events (HR = 1.46 [1.03-2.08], P = 0.035) after adjusting for demographic and clinical confounding factors.
Conclusion:
The results suggest that self-reported snoring and daytime sleepiness status are associated with an increased risk of future cardiovascular disease among older adults.
Citation:
Endeshaw Y; Rice TB; Schwartz AV; Stone KL; Manini TM; Satterfield S; Cummings S; Harris T; Pahor M; for the Health ABC Study. Snoring, daytime sleepiness, and incident cardiovascular disease in the health, aging, and body composition study. SLEEP 2013;36(11):1737-1745.
Keywords: Snoring, daytime sleepiness, cardiovascular disease
INTRODUCTION
Snoring is not just a “common nuisance of sleep,” but is a condition that indicates increased resistance to airflow in the upper airway during sleep.1,2 The prevalence of habitual snoring, defined as snoring 3 or more days per week, among middle-aged and older adults has been reported to range from 10% to 20% among women and 29% to 39% among men.3–5 Snoring is one of the cardinal manifestations of obstructive sleep apnea and hypopnea (OSAH)6,7; however, over a third of individuals who report habitual snoring may not have significant apnea and hypopnea events.8 This indicates that snoring could also represent a separate clinical entity apart from OSAH. Previous epidemiological studies have reported significant association between snoring and diabetes mellitus,9 incident hypertension,10 angina pectoris,11 and incident coronary heart disease and stroke.3 Conversely, lack of association between snoring and incident cardiovascular events has also been reported. For example, among 380 middle-aged adults who had ambulatory recording of breathing status during sleep at baseline and were followed for 17 years, recorded snoring was not associated with incident cardiovascular disease (CVD) or mortality.12 While most of the study participants in the aforementioned studies are middle-aged adults, similar conflicting results on the adverse effects of snoring have also been reported among older adults. Both significant association and lack of association have been reported between snoring and CVD among the elderly.5,13,14 These conflicting results imply that the clinical significance of snoring has not been well established.
Daytime sleepiness is one of the common sleep-wake complaints reported by older adults and has been associated with multiple adverse outcomes, including psychiatric disorders, metabolic abnormalities, CVD, and mortality.5,15,16 Although sleep related breathing disorder (SRBD) is one of the multiple etiological factors of daytime sleepiness reported in previous studies,17,13,19 a significant proportion of older adults with SRBD may not report daytime sleepiness.18,19 It is also notable that adverse effects of SRBD have been reported to vary based on the presence or absence of daytime sleepiness. For example, the association between SRBD and CVD is stronger among participants who reported daytime sleepiness than those who did not report daytime sleepiness.20,21 Furthermore, treatment of SRBD with continuous positive airway pressure did not result in beneficial effect among participants with no daytime sleepiness.22 Among older adults, study participants with moderate or severe SRBD and reported daytime sleepiness had increased risk of mortality, whereas mortality was not increased among participants with SRBD and no reported daytime sleepiness.23 These findings suggest that daytime sleepiness could moderate (modify) adverse effects of SRBD; it is possible that this may explain, at least in part, the conflicting results in the relationship between SRBD and adverse outcomes previously reported.
In the current study, we examine the association between snoring and incident CVD among community dwelling adults older than 70 years of age. Because adverse effects of SRBD have been shown to vary based on the status of daytime sleepiness as mentioned above, we hypothesized that participants who reported snoring and daytime sleepiness at baseline would have increased risk of CVD during follow-up in comparison to those who report snoring but no daytime sleepiness.
METHODS
Study Population
The Health ABC Study is a prospective cohort study in which relatively healthy community-dwelling older adults who were 70 to 79 years old were recruited between March 1997 and July 1998; participants in the current study were followed up for an average of 9.9 years. A total of 3,075 participants (1,584 females and 1,491 males) were randomly selected from a list of Medicare beneficiaries residing in areas surrounding Pittsburgh, PA, and Memphis, TN. Participants who were independent in their activities of daily living, and were able to walk a quarter of a mile and climb 10 steps without difficulty were included in the study. At baseline, data related to prevalent medical conditions, sleep characteristics, daytime sleepiness, and medication use were collected using structured questionnaires.
Sleep Assessment
Sleep questionnaire was used to evaluate self-reported snoring status, daytime sleepiness, sleep duration, and use of sleep aids. The 2 questions used to assess snoring status were: “Have you ever snored?” and “How often do you snore?” The first question had 3 responses (yes, no, don't know), while the second question had 6 responses (never, rarely, sometimes, often, always, don't know). Based on these responses, participants who reported snoring often or always were grouped as habitual snorers, while the rest of participants, including those who reported “don't know” were grouped as non-habitual snorers. Information on snoring was obtained only at baseline. Daytime sleepiness was determined based on the following question: “How often do you feel sleepy during the day?” Responses included never, rarely, sometimes, often, and always; participants who reported felling sleepy sometimes, often, and always were categorized as having significant daytime sleepiness. Based on snoring and daytime sleepiness status, 4 categories were created as follows: “No habitual snoring and No sleepiness,” “No habitual snoring and Sleepiness,” “Habitual snoring and No sleepiness,” and “Habitual snoring and Sleepiness.” Self-reported sleep duration was assessed using the following question “How many hours of sleep do you usually get at night?” and participants responded with duration of sleep in hours. Use of sleep aids was determined based on the question “Do you take sleeping pills or other medication to help you sleep” with the following responses: “never,” “rarely,” “sometimes,” “often,” “almost always.” Based on these responses, 3 groups were created: (1) “Never” or “Rarely,” (2) “Sometimes,” and (3) “Often or Almost Always.” Additionally, information about subjective sleep problems was collected using the following questions. How often do you have trouble: (1) “falling asleep,” (2) “waking up from sleep with difficulty going back to sleep,” and (3) “waking up too early in the morning”? An “often” or “always” response to any of these questions was considered a significant sleep complaint. Objective monitoring (recording) of breathing during sleep was not performed.
Incident Cardiovascular Disease (CVD)
Information about hospitalization was obtained during 6-month follow-up interview or from a report by the participants during hospitalization or after discharge from the hospital. Following this, appropriate medical records were gathered from the respective health facility and based on the information obtained, first hospitalization due to CVD was adjudicated according to the study criteria.24 Criteria for definite myocar-dial infarction included (1) the presence of evolving diagnostic pattern on ECG, or (2) diagnostic ECG pattern and abnormal enzymes, or (3) cardiac pain and evolving ST-T pattern on ECG or equivocal ECG pattern. Criteria for definite angina pectoris included symptoms of chest pain, chest tightness, physician diagnosis of angina pectoris, and medical treatment for angina pectoris. Criteria for definite congestive heart failure (CHF) included physician diagnosis of CHF and medical treatment for CHF. The time interval between the day of first study visit (time zero) and the day of first hospitalization for these events was calculated to derive the time to event.
Baseline Characteristics of Study Participants
In addition to demographic characteristics, variables that were previously described to be associated with SRBD and/or CVD were included in the analysis; these included body mass index, mood and cognition status, smoking status, alcohol consumption, hypertension, diabetes mellitus, metabolic syndrome, comorbidity status, and medication use. Laboratory values for high density lipoprotein (HDL), as well as biomarkers of inflammation which were reported to be associated with SRBD, sleepiness, and heart disease (C-reactive protein [CRP], inter-leukin 6 [IL-6], and tumor necrosis factor-α [TNF-α])25 were also included. Weight and height were measured at baseline and body mass index is calculated based on the following formula (weight in kg divided by height in m2). Center for Epidemio-logic Studies Depression Scale (CES-D) and Modified Mini-Mental State Examination (3MSE) tests were used to determine mood and cognition status respectively. Hypertension status was determined based on self-reported history of hypertension and medication use for hypertension, or sitting systolic and/ or diastolic blood pressure values > 140 and/or > 90 mm Hg, respectively. Status of diabetes mellitus (DM) was determined based on self-reported history and use of medication for DM, or fasting blood sugar > 126 mg/dL. Previously reported criteria were used to identify participants with metabolic syndrome.26 Morbidity status was determined based on self-reported diagnosis of diseases using a method previously described,27 and this method was used with certain modifications to adjust to our dataset. A total of 18 conditions were identified, and these were categorized in to 10 domains based on specific organ systems involved, such as cardiovascular, pulmonary, and gastrointestinal. The sum of the number of organ systems (domains) involved is used to indicate comorbidity score. In addition, number of prescription medications is used to denote morbidity status, with increased number of medications indicating increased morbidity.
Statistical Analysis
Individuals with definite or possible coronary heart disease (CHD) and/or CHF at baseline based on criteria listed in the Appendix (N = 662), and those in whom data for CHD and/or CHF is missing (N = 93), were excluded from the study.
Baseline Characteristics
Demographic and clinical characteristics of participants were evaluated among participants by snoring and sleepiness status using one-way analysis of variance and χ2 analysis for continuous and categorical variables, respectively.
Incident Cardiovascular Disease
Person-year data was calculated based on the number of participants who developed a cardiovascular event and time-to-first cardiovascular event. Kaplan-Meier survival curve was used to plot pattern of CVD event free survival time by snoring/ sleepiness status. Cox proportional hazards models were used to evaluate unadjusted and adjusted associations between snoring/ sleepiness status and CVD events. Censoring of participants was performed when participants were lost to follow-up, at the time of death, or at the end of the follow-up period. Covariates for the Cox regression models were selected based on their significant association with snoring and sleepiness status on bivariable analysis, and biological or clinical importance such as significant association with CVD and SRDB in previous studies. In addition to unadjusted model (Model 1), 3 additional Cox proportional hazards models were created. Model 2 included age in years, sex, race, marital status, years of education, BMI, alcohol use status, use of sleeping pills, and sleep duration. Model 3 included variables in Model 2 and traditional risk factors for cardiovascular disease such as smoking status, CES-D score, hypertension, diabetes mellitus, and low HDL cholesterol. In addition to variables in Model 3, Model 4 included biomarkers of inflammation that have been previously reported to be associated with both SRBD and CVD (CRP, IL-6, and TNF-α).25 Log-log plot was used to evaluate the proportional hazard assumption.
Cox-regression analysis was repeated using multiple imputation method to account for missing data, as well as bootstrapping resampling method. A two-sided P value < 0.05 was used to indicate statistical significance. Analyses were performed using IBM statistics SPSS 19 software.
RESULTS
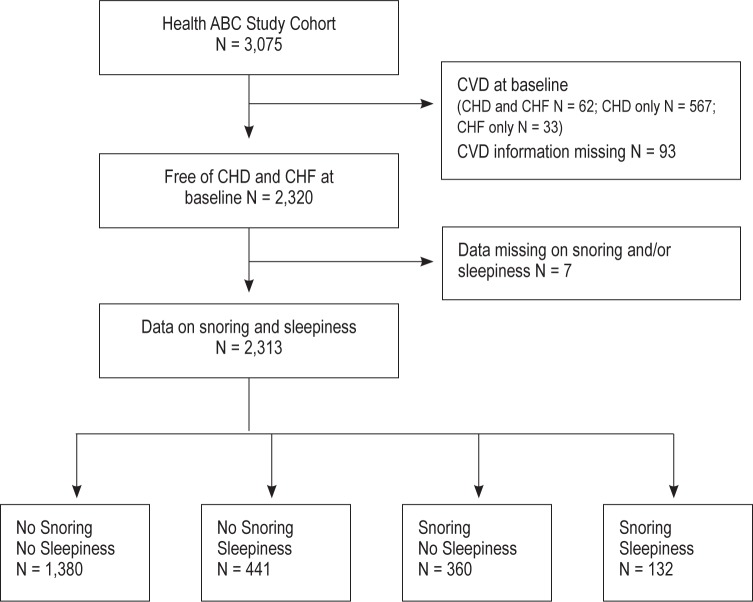
At baseline, there were 1,039 male (45%) and 1,281 female (55%) participants free of CHD and CHF (Figure 1); mean (SD) age was 73.5 (2.9) years. Fifty-nine percent of participants were white and 41% black; 52% were from Memphis. Baseline snoring and daytime sleepiness responses were available for 2,313 participants; of these, 1,380 (60%) reported no habitual snoring and no daytime sleepiness, 441 participants (19%) reported daytime sleepiness with no habitual snoring, 360 participants (15%) reported habitual snoring without daytime sleepiness, and 132 participants (6%) reported habitual snoring and daytime sleepiness. Habitual snoring was more commonly reported by males than females (28% vs. 16%, respectively, χ2 = 55.5, P < 0.001), and there was no significant difference in snoring frequency by racial group or by study site.
Figure 1.
Flowchart showing selection of participants in the current study. ABC, Aging and Body Composition; CVD, cardiovascular disease; CHD, coronary heart disease; CHF, congestive heart failure.
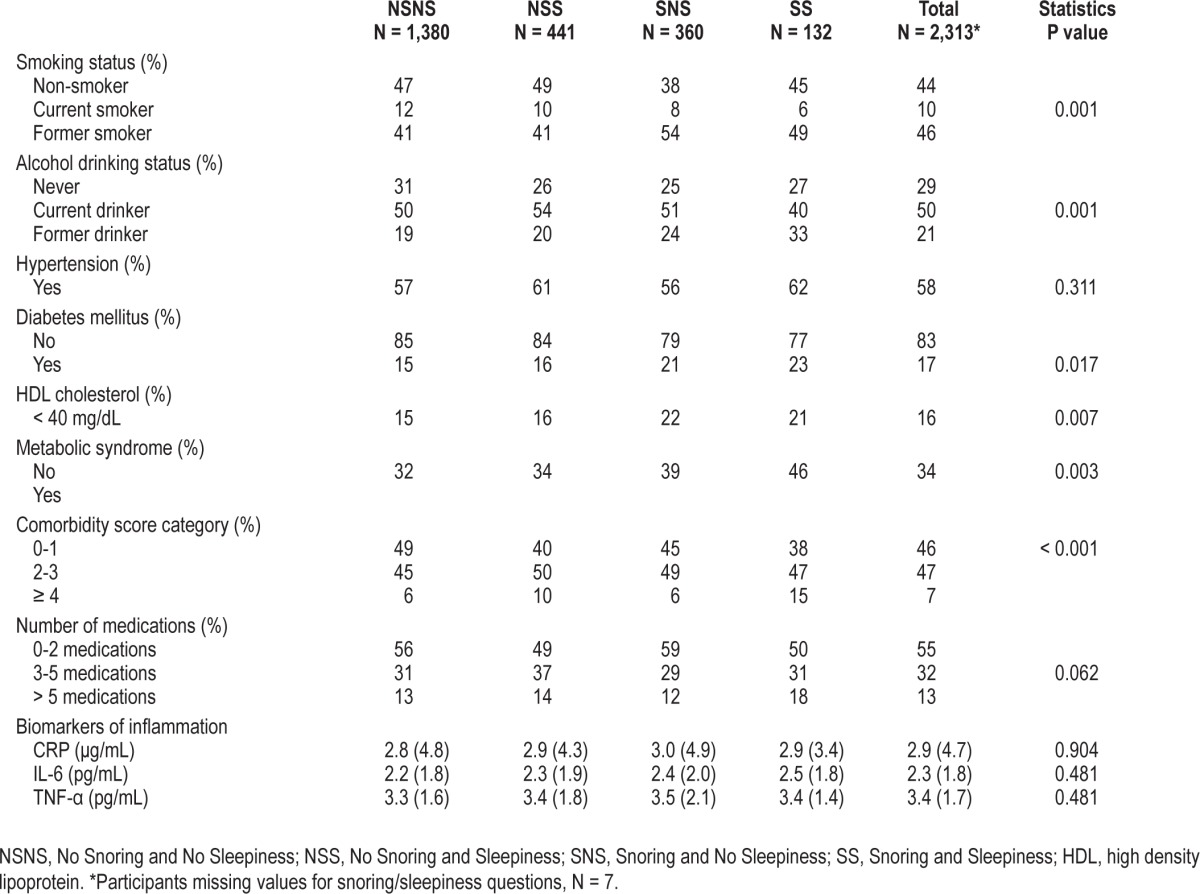
Table 1 shows baseline demographic and selected clinical characteristics by snoring/sleepiness status. As shown, the proportion of obese participants was much higher among participants in the snoring and sleepiness groups than other groups. The proportion of participants who reported short sleep duration was higher among those in the snoring and sleepiness group, while the proportion of participants who reported long sleep duration was higher among snoring and no sleepiness group. It is also notable that the proportion of participants with sleep complaints was higher among those who reported snoring and sleepiness, while the rate of sleep complaints among those with snoring and no sleepiness was similar to those who reported no snoring and no sleepiness. Table 2 shows more clinical characteristics of participants by snoring/sleepiness status. The prevalence of diabetes mellitus, low HDL status, and metabolic syndrome, as well as disease burden based on comorbidity score, was significantly higher among participants who reported snoring associated with sleepiness.
Table 1.
Demographic and selected clinical characteristics of participants by snoring/sleepiness status
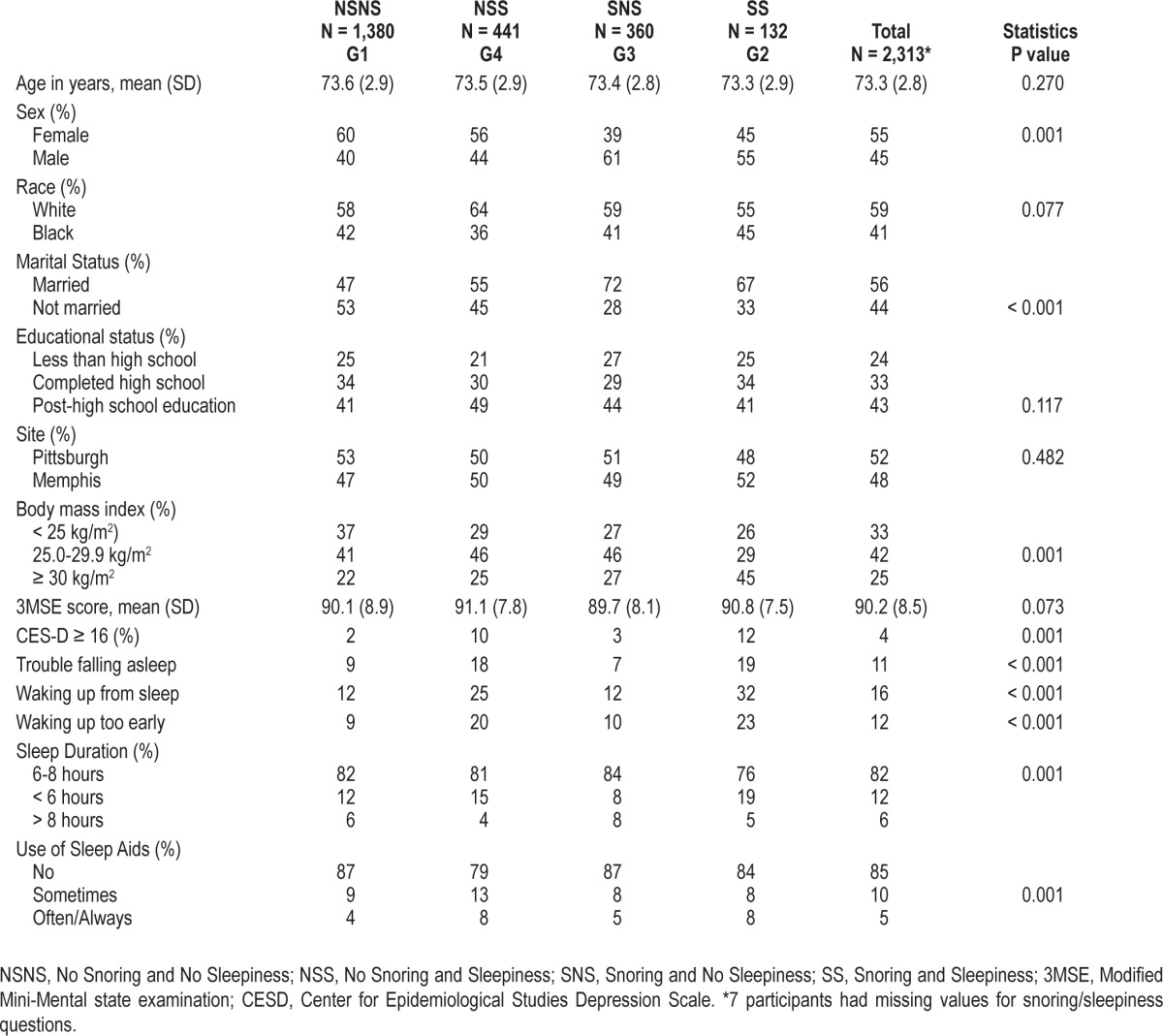
Table 2.
Selected clinical characteristics of participants by snoring/sleepiness status
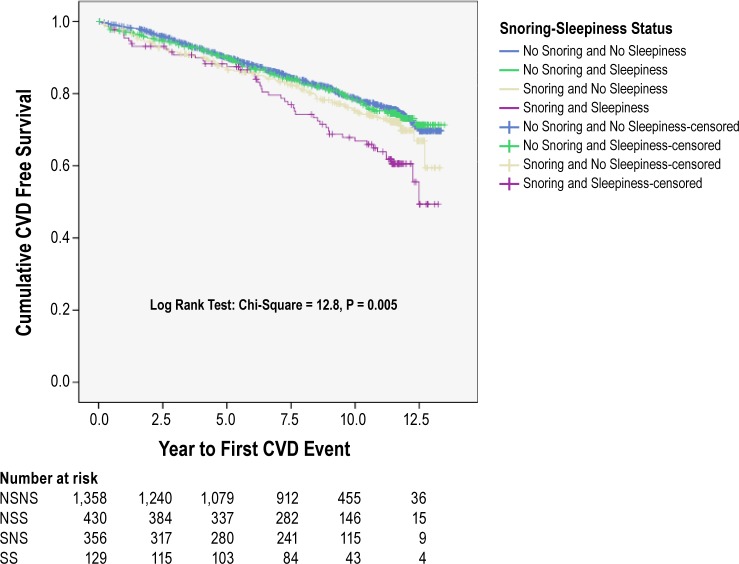
The average (SD) follow-up period was 9.9 (3.1) years. A total of 543 participants (24%) had one or more definite CVD events. Table 3 shows the distribution of CVD event rates by snoring/sleepiness status. Overall, 36% of participants who reported habitual snoring and sleepiness had incident cardiovascular events, while the corresponding proportions for those with no snoring/no sleepiness, no snoring/sleepiness, and snoring/no sleepiness status were 22%, 23%, and 26%, respectively (χ2 = 14.2, df = 3, P = 0.003). Figure 2 shows Kaplan-Meier survival curves by snoring and sleepiness status and number of participants at risk at each follow-up periods. As shown, CVD free survival during the follow up period was significantly decreased among participants who reported habitual snoring and daytime sleepiness at baseline (Log Rank test P = 0.005).
Table 3.
Proportion of participants with cardiovascular events during average follow-up of 9.9 years
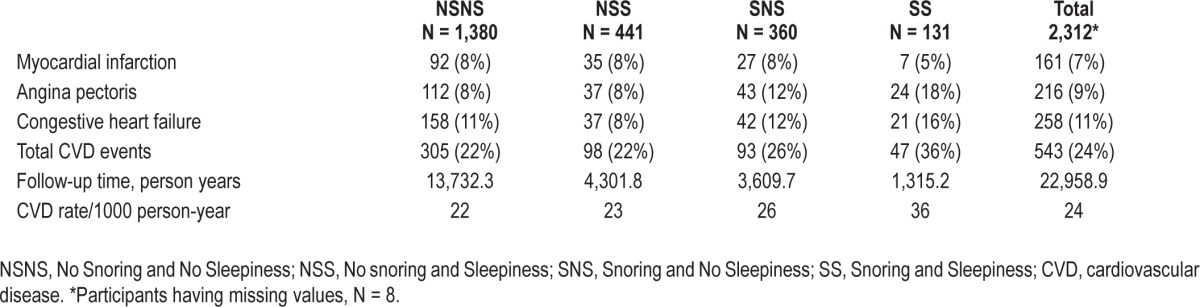
Figure 2.
Kaplan-Meier Curve by Snoring and Sleepiness Status. NSNS, No Snoring and No Sleepiness; NSS, No Snoring and Sleepiness; SNS, Snoring and No Sleepiness; SS, Snoring and Sleepiness.
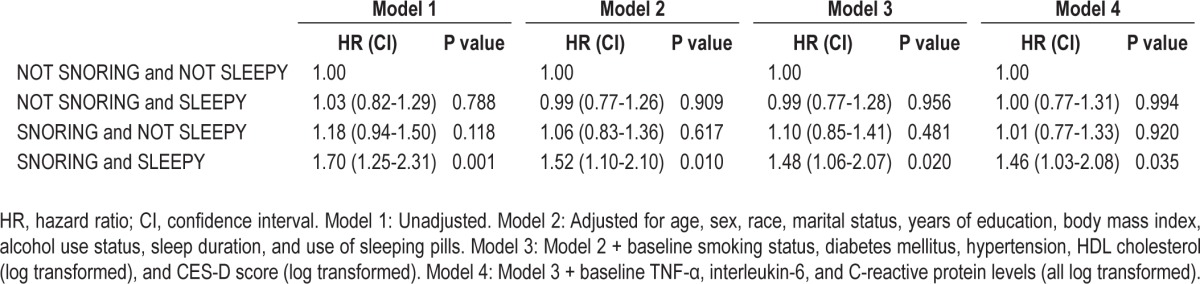
Table 4 shows unadjusted and adjusted results of Cox proportional hazard ratio by snoring and sleepiness status. As shown, participants who reported snoring associated with daytime sleepiness had significantly increased hazard ratio for CVD events in comparison to those who did not report either (HR [CI] 1.46 [1.03-2.08]), even after controlling for possible confounding factors. No significant interaction was observed between snoring/sleepiness status and age, sex, race, body mass index, and sleep duration. A total of 1,001 (43%) participants died during the follow-up period; the proportions of participants who died in the snoring-sleepiness, snoring-no sleepiness, no snoring-sleepiness, and no snoring-no sleepiness groups were 45%, 46%, 44%, and 46%, respectively. There was no significant difference in mortality among participants in the different snoring-sleepiness groups.
Table 4.
Cox regression model (outcome variable = incident cardiovascular disease)
In addition to snoring and sleepiness status, other variables that showed significant association with incident CVD in the model include age (HR [CI] = 1.04 [1.00-1.07]), male sex (HR [CI] = 1.60 [1.25-2.04]), current smoking status (HR [CI] = 1.48 [1.05-2.09]), hypertension (HR [CI] = 1.47 [1.19-1.81]), diabetes mellitus (HR [CI] = 1.38 [1.09-1.75]), and IL-6 level (HR [CI] = 1.40 [1.17-1.66]). In the presence of hypertension and diabetes mellitus, comorbidity score did not show a significant association with incident CVD when it was added in to the model; and it is not included in the final model as a covariate.
Statistical analysis was repeated using “often” and “always” response to indicate significant daytime sleepiness. Based on this criterion, the proportion of participants who reported daytime sleepiness was 115 of 2,316 (5%); among those who reported habitual snoring, it was 30 of 492 (6%). There was no significant association between snoring and sleepiness status and incident CVD using this criterion to define daytime sleepiness.
Results of Cox regression analyses examining the association between snoring and sleepiness status and incident CVD using multiple imputations to account for missing data (HR 1.40 [1.01-1.92]) and bootstrapping resampling method (HR 1.51 [1.06-2.14]) were similar to the main result indicated above.
DISCUSSION
Results of this prospective study demonstrate increased risk of incident cardiovascular disease among study participants who report snoring associated with daytime sleepiness at baseline. We also found that the risk of cardiovascular events among participants reporting snoring without daytime sleepiness was not significantly different from those reporting no snoring and no daytime sleepiness. These findings are in agreement with previous reports that indicated that the association between SRBD and adverse outcomes may be moderated by daytime sleepiness.20–22 Previous studies that examined the association between snoring only, and CVD or mortality among older adults did not find significant associations;5,28 and our results are also in agreement with these findings. In contrast, a previous longitudinal study reporting significant association between daytime sleepiness and incident CVD, as well as increased mortality, did not find interaction between snoring and daytime sleepiness.5 However, the criteria for defining both snoring and daytime sleepiness in that study were different from the criteria used in the current study; this may explain the difference in the results of the two studies.
Previous studies have reported significant association between daytime sleepiness and increased risk of cardiovascular disease among community dwelling older adults, in both cross-sectional29,30 and prospective studies.5,15 However, in the current study, the risk of cardiovascular events among participants who reported daytime sleepiness was only elevated in those who also reported snoring. In one previous study in which 3,100 participants 30 to 69 years old were followed up for 10 years, increased risk of mortality was reported among those reporting snoring and daytime sleepiness, in comparison to those reporting no snoring and no daytime sleepiness31; however, this effect was seen predominantly among participants younger than 60 years old, and no details on incident cardiovascular disease were reported in this study. To our knowledge, this is the first study to report significant association between snoring and sleepiness status and incident cardiovascular disease in a cohort of older adults greater than 70 years of age.
Several possible mechanisms may contribute to increased risk of incident cardiovascular disease among those with snoring and sleepiness. Snoring is strongly associated with OSAH and is described as one of the cardinal manifestation of OSAH.6 Although moderate to severe OSAH is reported to occur in about 20% of older adults,8 the relationship between OSAH and cardiovascular disease in this group is not well established. For example, reports from a recently completed prospective study (Sleep Heart Health Study) indicated no significant association between sleep apnea and coronary heart disease among participants ≥ 70 years old, no independent association between sleep apnea and incident hypertension among participants > 65 years old,32 significantly increased risk of death only in men < 70 years old,33 and independent association between sleep apnea and congestive heart failure only in male participants.34 Similar results were reported in cross-sectional analysis in which independent associations were reported between sleep apnea and hypertension,35 as well as other cardiovascular risk factors,36 but these associations were significant predominantly among participants < 65 years old. In fact, one previous study has reported decreased mortality among older adults with moderate sleep apnea,37 suggesting that moderate sleep apnea in this group of the population may provide a “survival advantage.”
On the other hand, other studies have reported significant association between sleep apnea and adverse outcomes such as non-dipping of blood pressure during sleep,38 increased cardiovascular disease,39 and increased mortality39,23 among older adults. It is possible that snoring and sleepiness status may represent severe form of OSAH, and this may explain the mechanism in the association reported in the current study.
It is notable that previous studies have reported increased sleep fragmentation and more severe oxygen desaturation among participants with OSAH and daytime sleepiness than those with OSAH and no daytime sleepiness.40 These changes have been described to be associated with increased sympathetic activity and chronic inflammation, which could explain the association between OSAH and increased cardiovascular morbidity among those with daytime sleepiness.41 In the current study, sleep complaints were more commonly reported among participants who reported snoring and daytime sleepiness (Table 1), and this may indicate more sleep disruption in this group of study participants.
However, snoring and sleepiness could also occur without clinically significant sleep apnea, i.e., apnea hypopnea index < 5 per hour of sleep.19,42 Among study participants with snoring and no sleep apnea, independent association between snoring and carotid atherosclerosis has been reported,43 suggesting that snoring may have adverse cardiovascular effect independent of OSAH. Additionally, individuals with snoring associated with resistance to airflow and no significant apnea or hypopnea events have been described to have daytime sleepiness and multiple arousals from sleep due to increase in respiratory effort, a condition referred to as upper airway resistance syndrome (UARS).44 Although we are not aware of previous reports that have described pathophysiological mechanisms associated with UARS, similar to OSAH, frequent arousals associated with UARS may result in increased sympathetic activity, and this may mediate the adverse effects associated with this disorder.45 These mechanisms could explain, at least in part, the mechanism involved in the relationship between snoring and sleepiness status, and cardiovascular disease reported in the current study.
Other findings of importance in the current study include significantly increased prevalence of diabetes mellitus, metabolic syndrome, and low HDL cholesterol among participants who reported snoring and sleepiness (Table 2). Although these associations have been previously reported, these reports were mostly among middle-aged adults,33,46,47 and our findings extend these previous reports to older adults > 70 years of age. Of note, one previous study using the same dataset has reported a significant association between daytime napping and diabetes mellitus, but snoring status was not reported in the study.48 Given the common occurrence of these morbidities among older adults, a more detailed examination of these relationships would be warranted.
The current study has several strengths. Participants were community-dwelling older adults ≥ 70 years of age, who were regularly followed up for an average of about 9.9 years. In addition, data collection in general and collection of data related to cardiovascular outcomes in particular were performed using well-defined criteria; and this has made it possible to determine the association between our exposure and outcome variables after controlling for potential confounding factors. However, results of the current study should be interpreted in light of the following limitations. Although one of the strengths of the current study is inclusion of non-Hispanic white and black participants, the study did not include Hispanic or Asian participants, and results may not apply to these groups. Because study participants were relatively healthy at recruitment, study participants may not be representatives of older adults with poor health and/or functional status. Information about both snoring status and daytime sleepiness were obtained by self-report, and daytime sleepiness was determined using a single question. Self-reported snoring has been reported to have low sensitivity when compared to objectively measured (recorded) snoring.49 In addition, participants in the current study who reported “don't know” and “sometimes” to the “snoring” question were also grouped as having “non-habitual snoring,” although participants in both these groups could have significant SRBD.50 This could result in misclassification of study participants; however, this exposure was measured before the outcome of incident CVD was known, and the misclassification should therefore be non-differential with respect to the outcome. The effect of this kind of misclassification would be to attenuate the association between our exposure of interest (snoring and sleepiness status) and incident cardiovascular outcome, and not to exaggerate the association. Data on status of treatment of SRBD among study participants were not available, and this may have some effect on the outcome; however, the effect of successful treatment would also be to attenuate the relationship between exposure and outcome. We were not able to show increased risk for CVD when a more stringent criterion was used for the daytime sleepiness question. We think that the low number of participants with daytime sleepiness using the more stringent criterion in the current study may account, at least in part, for this unexpected finding. Lastly, the questions used for assessment of snoring and daytime sleepiness are not validated in older adults, and their reliability and validity may be limited.
In conclusion, we report that self-reported habitual snoring combined with daytime sleepiness status, but not either factor alone, among community dwelling older adults increase the risk of cardiovascular disease. While previous studies have reported similar associations among mostly middle-aged adults, to our knowledge, this is the first study to report such finding among adults older than 70 years of age. We think that these symptoms could be used as a simple and inexpensive method to identify older adults at increased risk for CVD. Given the high prevalence of cardiovascular morbidity in this group of the population, this may have significant implications in improving CV health status and reducing health care expenditure. Future studies should focus in determining whether successful treatment of SRBD in this group of the population has any impact in preventing or improving the course of cardiovascular diseases.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research was supported in part by the Intramural Research Program of the National Institute of Health (NIH), National Institute on Aging (NIA), by NIA contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050, NINR grant R01-NR012459 and P30 AG028740 Claude D. Pepper Older Americans Independence Center.
SUPPLEMENTAL MATERIAL
APPENDIX
Definite coronary heart disease (CHD)
Self-reported history of coronary artery bypass graft surgery, percutaneous coronary angioplasty, or carotid endarterectomy, OR
Self-reported history of myocardial infarction or angina and use of anti-angina meds, OR
Major Q wave abnormality on 12-lead electrocardiogram (ECG), OR
Possible CHD
Self-reported history of MI or angina, but no history of cardiovascular procedures stated above and no use of anti-angina medication, OR
Complete left bundle branch by 12-lead ECG.
Definite congestive heart failure (CHF)
Self-reported heart failure and use of diuretic and vasodilator drug or use of cardiac glycoside.
Possible CHF
Self-reported heart failure, but no use of diuretic, vasodilator and cardiac glycoside.
REFERENCES
- 1.Robin IG. Snoring. Proc R Soc Med. 1948;41:151–3. doi: 10.1177/003591574804100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robin IG. Snoring. Proc R Soc Med. 1968;61:575–82. doi: 10.1177/003591576806100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu FB, Willett WC, Manson JE, et al. Snoring and risk of cardiovascular disease in women. J Am Coll Cardiol. 2000;35:308–13. doi: 10.1016/s0735-1097(99)00540-9. [DOI] [PubMed] [Google Scholar]
- 4.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;26:74–9. [PubMed] [Google Scholar]
- 5.Newman AB, Spiekerman CF, Enright P, et al. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research Group. J Am Geriatr Soc. 2000;48:115–23. doi: 10.1111/j.1532-5415.2000.tb03901.x. [DOI] [PubMed] [Google Scholar]
- 6.Lugaresi E. Snoring. Electroencephalogr Clin Neurophysiol. 1975;39:59–64. doi: 10.1016/0013-4694(75)90127-3. [DOI] [PubMed] [Google Scholar]
- 7.Zwillich C. The clinical significance of snoring. Arch Intern Med. 1979;139:24. [PubMed] [Google Scholar]
- 8.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 9.Valham F, Stegmayr B, Eriksson M, et al. Snoring and witnessed sleep apnea is related to diabetes mellitus in women. Sleep Med. 2009;10:112–7. doi: 10.1016/j.sleep.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Hu FB, Willett WC, Colditz GA, et al. Prospective study of snoring and risk of hypertension in women. Am J Epidemiol. 1999;150:806–16. doi: 10.1093/oxfordjournals.aje.a010085. [DOI] [PubMed] [Google Scholar]
- 11.Koskenvuo M, Kaprio J, Partinen M, et al. Snoring as a risk factor for hypertension and angina pectoris. Lancet. 1985;1:893–6. doi: 10.1016/s0140-6736(85)91672-1. [DOI] [PubMed] [Google Scholar]
- 12.Marshall NS, Wong KK, Cullen SR, et al. Snoring is not associated with all-cause mortality, incident cardiovascular disease, or stroke in the busselton health study. Sleep. 2012;35:1235–40. doi: 10.5665/sleep.2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enright PL, Newman AB, Wahl PW, et al. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996;19:531–8. doi: 10.1093/sleep/19.7.531. [DOI] [PubMed] [Google Scholar]
- 14.Jennum P, Schultz-Larsen K, Christensen N. Snoring, sympathetic activity and cardiovascular risk factors in a 70 year old population. Eur J Epidemiol. 1993;9:477–82. doi: 10.1007/BF00209524. [DOI] [PubMed] [Google Scholar]
- 15.Empana JP, Dauvilliers Y, Dartigues JF, et al. Excessive daytime sleepiness is an independent risk indicator for cardiovascular mortality in community-dwelling elderly: the three city study. Stroke. 2009;40:1219–24. doi: 10.1161/STROKEAHA.108.530824. [DOI] [PubMed] [Google Scholar]
- 16.Bixler EO, Vgontzas AN, Lin HM, et al. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90:4510–5. doi: 10.1210/jc.2005-0035. [DOI] [PubMed] [Google Scholar]
- 17.Pack AI, Dinges DF, Gehrman PR, et al. Risk factors for excessive sleepiness in older adults. Ann Neurol. 2006;59:893–904. doi: 10.1002/ana.20863. [DOI] [PubMed] [Google Scholar]
- 18.Johansson P, Alehagen U, Svanborg E, et al. Sleep disordered breathing in an elderly community-living population: Relationship to cardiac function, insomnia symptoms and daytime sleepiness. Sleep Med. 2009;10:1005–11. doi: 10.1016/j.sleep.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Gottlieb DJ, Whitney CW, Bonekat WH, et al. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med. 1999;159:502–7. doi: 10.1164/ajrccm.159.2.9804051. [DOI] [PubMed] [Google Scholar]
- 20.Kapur VK, Resnick HE, Gottlieb DJ. Sleep disordered breathing and hypertension: does self-reported sleepiness modify the association? Sleep. 2008;31:1127–32. [PMC free article] [PubMed] [Google Scholar]
- 21.Choi JB, Nelesen R, Loredo JS, et al. Sleepiness in obstructive sleep apnea: a harbinger of impaired cardiac function? Sleep. 2006;29:1531–6. doi: 10.1093/sleep/29.12.1531. [DOI] [PubMed] [Google Scholar]
- 22.Barbe F, Mayoralas LR, Duran J, et al. Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness. a randomized, controlled trial. Ann Intern Med. 2001;134:1015–23. doi: 10.7326/0003-4819-134-11-200106050-00007. [DOI] [PubMed] [Google Scholar]
- 23.Gooneratne NS, Richards KC, Joffe M, et al. Sleep disordered breathing with excessive daytime sleepiness is a risk factor for mortality in older adults. Sleep. 2011;34:435–42. doi: 10.1093/sleep/34.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–85. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 25.Pai JK, Pischon T, Ma J, et al. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351:2599–610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 27.Rigler SK, Studenski S, Wallace D, et al. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clin Rehabil. 2002;16:420–8. doi: 10.1191/0269215502cr515oa. [DOI] [PubMed] [Google Scholar]
- 28.Jennum P, Schultz-Larsen K, Davidsen M, Christensen NJ. Snoring and risk of stroke and ischaemic heart disease in a 70 year old population. A 6-year follow-up study. Int J Epidemiol. 1994;23:1159–64. doi: 10.1093/ije/23.6.1159. [DOI] [PubMed] [Google Scholar]
- 29.Merlino G, Piani A, Gigli GL, et al. Daytime sleepiness is associated with dementia and cognitive decline in older Italian adults: a population-based study. Sleep Med. 2010;11:372–7. doi: 10.1016/j.sleep.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 30.Ohayon MM, Vecchierini MF. Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med. 2002;162:201–8. doi: 10.1001/archinte.162.2.201. [DOI] [PubMed] [Google Scholar]
- 31.Lindberg E, Janson C, Svardsudd K, Gislason T, Hetta J, Boman G. Increased mortality among sleepy snorers: a prospective population based study. Thorax. 1998;53:631–7. doi: 10.1136/thx.53.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Connor GT, Caffo B, Newman AB, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179:1159–64. doi: 10.1164/rccm.200712-1809OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haas DC, Foster GL, Nieto FJ, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111:614–21. doi: 10.1161/01.CIR.0000154540.62381.CF. [DOI] [PubMed] [Google Scholar]
- 36.Newman AB, Nieto FJ, Guidry U, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol. 2001;154:50–9. doi: 10.1093/aje/154.1.50. [DOI] [PubMed] [Google Scholar]
- 37.Lavie P, Lavie L. Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res. 2009;18:397–403. doi: 10.1111/j.1365-2869.2009.00754.x. [DOI] [PubMed] [Google Scholar]
- 38.Endeshaw YW, White WB, Kutner M, Ouslander JG, Bliwise DL. Sleep-disordered breathing and 24-hour blood pressure pattern among older adults. J Gerontol A Biol Sci Med Sci. 2009;64:280–5. doi: 10.1093/gerona/gln011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johansson P, Alehagen U, Ulander M, Svanborg E, Dahlström U, Broström A. Sleep disordered breathing in community dwelling elderly: associations with cardiovascular disease, impaired systolic function, and mortality after a six-year follow-up. Sleep Med. 2011;12:748–53. doi: 10.1016/j.sleep.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 40.Sun Y, Ning Y, Huang L, et al. Polysomnographic characteristics of daytime sleepiness in obstructive sleep apnea syndrome. Sleep Breath. 2012;16:375–81. doi: 10.1007/s11325-011-0515-z. [DOI] [PubMed] [Google Scholar]
- 41.Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90:47–112. doi: 10.1152/physrev.00043.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 43.Lee SA, Amis TC, Byth K, et al. Heavy snoring as a cause of carotid artery atherosclerosis. Sleep. 2008;31:1207–13. [PMC free article] [PubMed] [Google Scholar]
- 44.Guilleminault C, Stoohs R, Clerk A, et al. A cause of excessive daytime sleepiness. The upper airway resistance syndrome. Chest. 1993;104:781–7. doi: 10.1378/chest.104.3.781. [DOI] [PubMed] [Google Scholar]
- 45.Leung RS, Bradley TD. Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med. 2001;164:2147–65. doi: 10.1164/ajrccm.164.12.2107045. [DOI] [PubMed] [Google Scholar]
- 46.Theorell-Haglow J, Berne C, Janson C, Lindberg E. The role of obstructive sleep apnea in metabolic syndrome: a population-based study in women. Sleep Med. 2011;12:329–34. doi: 10.1016/j.sleep.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 47.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 48.Goldman SE, Hall M, Boudreau R, et al. Association between nighttime sleep and napping in older adults. Sleep. 2008;31:733–40. doi: 10.1093/sleep/31.5.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lindberg E, Elmasry A, Janson C, Gislason T. Reported snoring--does validity differ by age? J Sleep Res. 2000;9:197–200. doi: 10.1046/j.1365-2869.2000.00199.x. [DOI] [PubMed] [Google Scholar]
- 50.Bliwise DL, Nekich JC, Dement WC. Relative validity of self-reported snoring as a symptom of sleep apnea in a sleep clinic population. Chest. 1991;99:600–8. doi: 10.1378/chest.99.3.600. [DOI] [PubMed] [Google Scholar]