Abstract
Deregulation of soluble apoptosis stimulating fragment (sFas) plays an important role in glomerulonephritis (GN). The study assed the influence of immunosuppressive treatment on serum and urine sFas in patients with proliferative (PGN) and non-proliferative (NPGN) GN, and evaluated the potential of sFas measurements in predicting outcomes. Eighty-four patients with GN (45 males and 39 females) were included. Serum concentration (ng/mL) and urinary excretion (ng/mg of urinary creatinine) of sFas were measured before and after the treatment. After 12 months of therapy with steroids and cyclophosphamide, patients were divided into two subgroups according to the treatment results: Responders (R) and Non-Responders (NR). The sFas urinary excretion was reduced after treatment in both PGN and NPGN (from 17.12 ± 15 to 5.3 ± 4.2, P = 0.008 and from 10.11 ± 6.1 to 3.4 ± 3.0, P = 0.039; respectively) whereas the sFas serum concentration remained unchanged. In PGN, pre-treatment urinary sFas concentration was significantly lower in the Responders than in Non-Responders (2.3 ± 3.1 vs 19.4 ± 14.1, P = 0.003), and was lower still than in both R (P = 0.044) and NR (P = 0.042) subgroups with NPGN. The immunosuppressive treatment reduced sFas urinary excretion in proliferative and non-proliferative GN and results suggest that the lower urinary sFas may be linked with favorable therapy outcomes in patients with PGN.
Keywords: Immunosuppressive Treatment, Primary Glomerulonephritis, Apoptosis, Treatment Outcomes
INTRODUCTION
The Fas - Apoptosis Stimulating Fragment - ligand (Fas-L) is responsible for initiating cell apoptosis, which may be modulated by cross-linking with the Fas receptor. Soluble Fas (sFas) blocks Fas-L and subsequently inhibits apoptosis, causing damage to the glomeruli and usually accelerating the progression of glomerulonephritis (1, 2). The cytotoxic actions mediated via Fas-L may contribute to inflammatory immune responses (3) and Fas-L expression positively correlates with the stage of kidney injury (4). The mRNAs of Fas and Fas-L were also increased in the glomerulus after anti-glomerular basement membrane antibody administration in rats (3).
Primary glomerulonephritis (GN) is an immune-mediated disease affecting both the glomeruli and interstitium with or without an infiltration of inflammatory cells associated with protein overabsorption by renal tubules (5). Proliferative (PGN) and non-proliferative (NPGN) types of GN were historically differentiated by the presence of leukocyte infiltration, cell proliferation and an imbalance of glomerular extracellular matrix turnover (the predominance of its production or degradation), as well as their involvement in the injury of kidney structures (6). Proliferative primary glomerulonephritis comprises mesangial proliferative GN (MesGN), membrano-proliferative GN (MPGN) and immunoglobulin A nephropathy (IgAN), while non-proliferative GN consists of minimal change disease (MCD), focal glomerulosclerosis (FSGS), and membranous nephropathy (MN) (6). In general, proliferative GN may be characterized by glomerular fibrosis - a complicated process initiating cell cytotoxicity and involving many factors, including Fas (1-3, 7, 8). Once induced by Fas an apoptosis helps to prevent local foci of atrophy caused by progressive fibrosis affecting mainly renal tubules (1-3, 7, 8). This process if inhibited by over-synthesized sFas may accelerate kidney injury. End-stage renal disease is an unfavorable outcome of fibrosis enhancement in primary glomerulonephritis. The introduction of a course of immunosuppressive therapy (IS) composed of corticosteroids and cyclophosphamide significantly improved GN outcome but did not exclude resistance to such routine treatment (9-13).
Due to the unpredictable course of GN and response to therapy, treatment individualization and optimization is often impossible. Hence, the search for more reliable predictors which might allow an adjusted and adequate immunosuppressive treatment scheme to be identified for individuals continues. This study was conducted to determine whether in severe courses of GN, sFas may be regarded as a complementing factor when deciding to introduce aggressive treatment in sensitive cases, or disqualify it to prevent IS complications. The aims of the study were:
- To compare sFas serum concentration and urinary excretion between patients with primary GN and healthy participants.
- To assess the influence of immunosuppressive treatment on the serum and urine sFas levels in patients with proliferative and non-proliferative primary glomerulonephritis and,
- To evaluate the potential of using sFas serum concentration and urine excretion measurements to predict the response to immunosuppressive treatment.
MATERIALS AND METHODS
The study was conducted from autumn 2002 to spring 2010 year, in 84 patients (45 males and 39 female) mean age 41.44 ± 13.25 yr with primary glomerulonephritis. The control group consisted of 18 age-matched healthy subjects. The structure of the study group (including glomerulonephritis type divisions) and the control group is shown in Table 1. Only patients with a severe course of GN i.e. nephrotic range proteinuria or deterioration of kidney function, reflected in an increase of serum creatinine concentration by more than 50% of baseline values, despite steroid treatment were included in this study. The diagnosis was established based on clinical symptoms, laboratory tests, accessory investigations and kidney biopsy.
Table 1.
The structure of the study group (including subdivisions) according to primary glomerulonephritis type and the control group
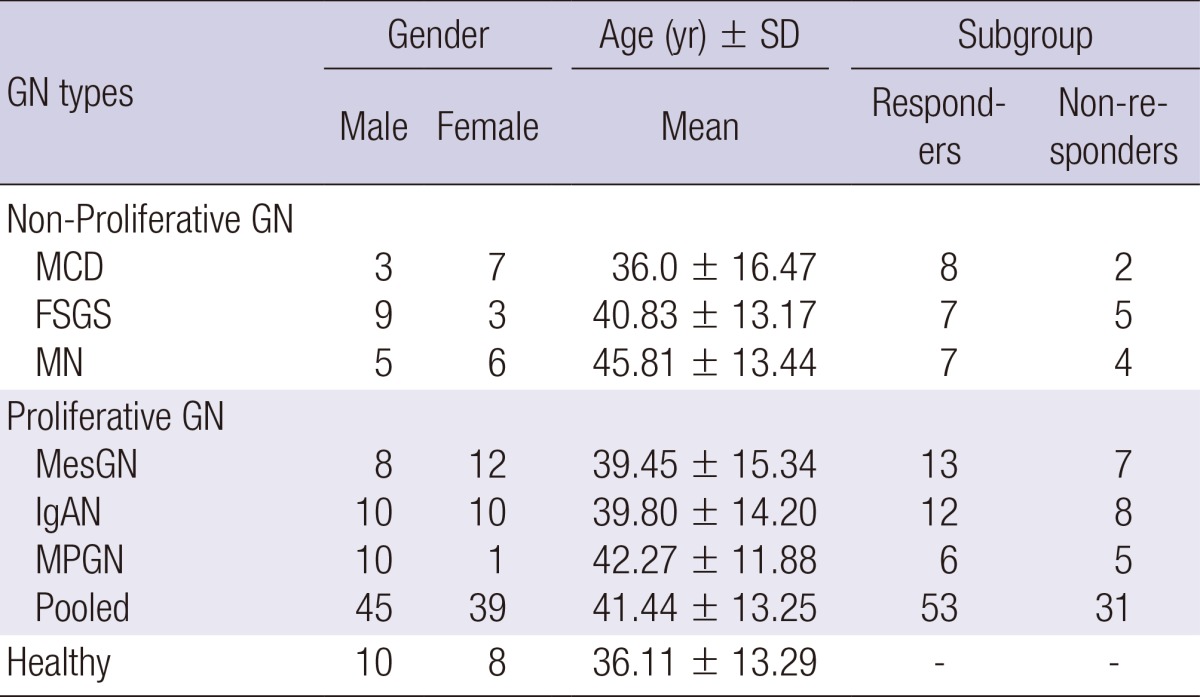
GN, glomerulionephritis; MCD, minimal change disease; FSGS, focal segmantal glomerulosclerosis; MN, membranous nephropathy; MesGN, mesangio-proliferative glomerulonephritis; IgAN, immunoglobulin A nephropathy; MPGN, membrano-proliferative glomerulionephritis.
All of the biopsy specimens were evaluated by light and immunofluorescence microscopy in Department of Kidney Pathology Medical University of Lodz. In addition, the percentage of interstitial volume was calculated using a computerized morphometric analysis of interstitium quantity (14, 15). The degree of glomerulosclerosis (GSC), based on number of involved glomeruli, and the intraglomerular extent of sclerosis were semiquantitatively estimated according to a scoring system proposed by Fuiano et al. (16). The GSC was graded on a four-point scale: normal (0), mild (1), moderate (2), and severe (3). The type of primary glomerulonephritis was identified by microscopic evaluation, and mesangio-proliferative GN was diagnosed after the exclusion of other proliferative glomerulonephritis (14-17).
Also, the urinary excretion of proteins, expressed in milligrams per milligram of creatinine in urine (mg/mg Cr) and total serum proteins, were measured.
All participants were treated with antihypertensive drugs (angiotensin converting enzyme inhibitors or angiotensin receptor blocker and calcium channel blockers) to establish and maintain blood pressure values according to recommendations (18, 19). In addition, statins were introduced to stabilize the lipid profile (atorvastatin at a mean dose of 20 mg/day). The primary aim was to reduce low density lipoprotein (LDL) serum concentration to below 100 mg/dL (20). Those variables were assessed at baseline and serially throughout the treatment to monitor the status of the patients. Finally all tests were repeated after 1 yr (± 3 months) of immunosuppressive treatment.
All subjects received an identical immunosuppressive protocol which consisted of initial pulse therapy with methylprednisolone (a calculated aggregate dose 1,000 mg per 20 kg body weight, administered 1,000 mg in every other day) followed by oral prednisone (25-30 mg/day) and cyclophosphamide in 6 monthly given pulses 0.6 g/b.m2. The cumulative dose of cyclophosphamide did not exceed 6 grams. Before the initiation of treatment, the potential foci of infection was diagnosed and eliminated as a routine in all participants. A treatment scheme including pulses of steroids and cyclophosphamide (CPH) was restricted to cases of progressive GN with severe disease course (decreasing of eGFR) and was chosen as a rescue protocol. The introduction of cyclophosphamide as primary treatment is controversial in different types of GN although many authors describe it offers greater benefits than other immunosuppressive agents (21-32). CPH pulse treatment combined with steroids is regarded as well tolerated and effective, especially in steroid-dependent or corticosteroid resistant, severe nephrotic syndrome or in GN with progressive worsening of eGFR and diffuse microscopic lesions, irrespective of primary glomerulonephritis type (21-32).
To assess the influence of immunosuppressive therapy on cytokine activity, the blood and urine of healthy participants, as well as pre- and post-treatment blood and urine samples from patients, were prospectively collected to EDTA (ethylenediaminetetraacetic acid) tubes, centrifuged and stored at -70℃ until analysis. When completed, the serum concentrations and urinary excretion of soluble Fas were measured by enzyme-linked immunosorbent assay (ELISA) using commercial immunoassays according to manufacturer's instructions (Biosource® Europe S.A., Nivelles, Belgium). All tests were performed in a certified local laboratory.
To evaluate the potential of sFas in predicting GN outcomes after one year of treatment, patients were divided retrospectively into two subgroups according to their response to the therapy: R (Responders; proteinuria < 0.5 g/day, e.g. < 6 mg/mg urine Cr and improved or stable kidney function - serum creatinine change within a range of 15%), NR (Non-Responders; proteinuria > 0.5 g/day, e.g. > 6 mg/mg urine Cr and/or deterioration of kidney function - over 15% increase of serum creatinine concentration). When completed, the division allowed sFas to be evaluated retrospectively at baseline in R and NR. The structure of subgroups, divided according to type of primary glomerulonephritis, is presented in Table 1. No differences in distribution between subgroups R and NR were noticed (Table 1). No comorbidities, including diabetes, obesity or severe infections, which may affect the final evaluation in both subgroups were noted. The gender structure in the subgroups and the control group was homogenous. The study group and the control group were sex and age matched.
To verify the potency of sFas measurements to predict GN favorable outcomes and to indicate sFas abnormal urine excretion pointing the worse pre-treatment prognosis, the cut off value was calculated using ROC curve.
Statistical analysis
Comparisons within and between groups were made with the non-parametrical the Kruskal-Wallis ANOVA for multivariate analysis. The Fisher's exact probability test was used for sex comparison and Wilcoxon's rank sum test for the changes of clinical parameters during the treatment. Relations between variables were analyzed by Spearman rank (R) correlation coefficients. A logistic regression was performed to analyze potential confounders in the cohort. Differences were considered significant for P < 0.05. The results are expressed, as appropriate, mean ± standard deviation and median (range).
Ethics statement
The study protocol was approved by the Medical University of Łódź Bioethics Committee, Resolution No. RNN/9/04/KE. According to principles of GCP, the informed consents have been obtained from all patients prior to their inclusion in the study.
RESULTS
Clinical data
As shown in Table 2, before the treatment, no statistically significant differences in biopsy findings (percentage of interstitium volume and glomerulosclerosis grade) or biochemical parameters (total serum proteins, serum creatinine concentration) were observed between R and NR subgroups in either type of GN (for all comparisons). In proliferative GN, the only parameter which differed between both subgroups was significantly lowered pretreatment LDL serum concentration in R subgroup. In both subgroups of non-proliferative GN pre-treatment protein urine excretion was significantly higher than in proliferative GN.
Table 2.
Biopsy findings and biochemical parameters in proliferative and non-proliferative glomerulonephritis divided into Responders and Non-Responders subgroups (mean±SD)
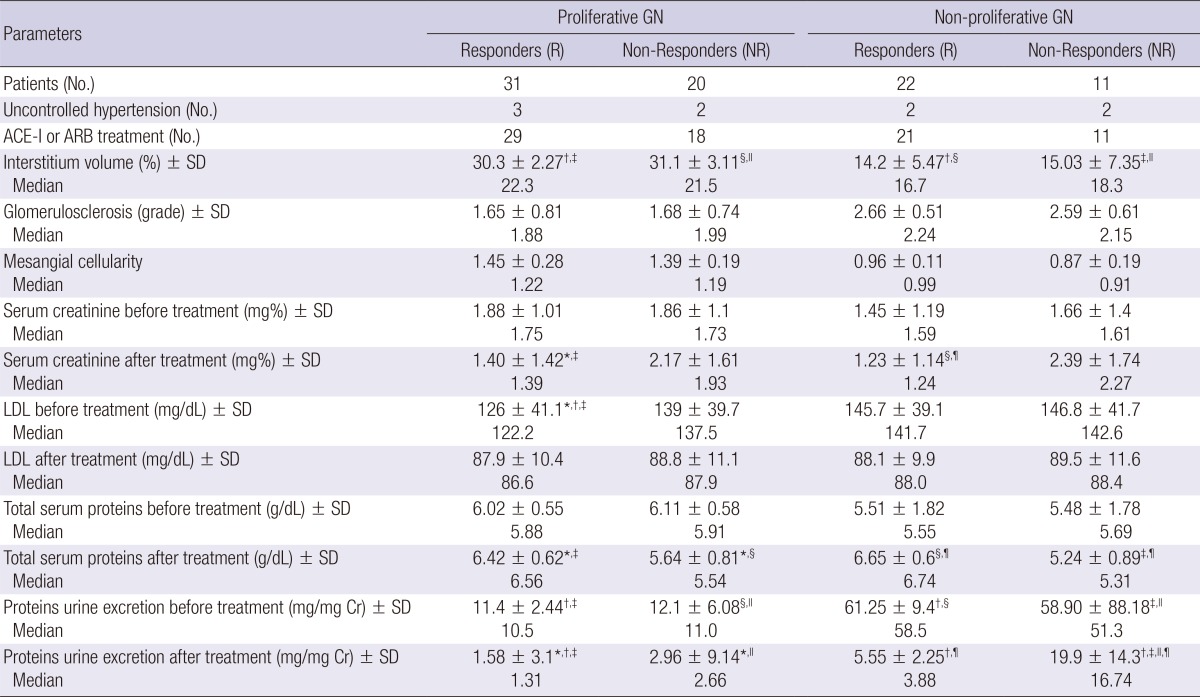
Differences were considered significant for P < 0.05 (Kruskal-Wallis ANOVA); *Proliferative GN R vs NR; †Proliferative GN R vs non-proliferative GN R; ‡Proliferative GN R vs non-proliferative GN NR; §Proliferative GN NR vs non-proliferative GN R; ∥Proliferative GN NR vs non-proliferative GN NR; ¶Non-proliferative GN R vs NR.
Before treatment, significant positive correlations between serum creatinine concentration and interstitium volume (ρ = 0.263, P = 0.029), and glomerulosclerosis grade (ρ = 0.294, P = 0.036) in proliferative glomerulonephritis were found. Also in non-proliferative primary glomerulonephritis, a positive correlation between serum creatinine and interstitium volume (ρ = 0.28, P = 0.043), and glomerulosclerosis grade (ρ = 0.22, P = 0.038) were noted.
The differences between the R and NR subgroups regarding both proliferative and non-proliferative primary glomerulonephritis in post-treatment: total serum proteins (higher in R subgroup), serum creatinine concentration and protein urine excretion (lower in R subgroup) were found to be statistically significant, as expected, and followed from assumed subdivision to Responders and Non-Responders, however, there was no difference in post-treatment protein urine excretion between NR proliferative and R non-proliferative glomerulonephritis. The introduction of statins resulted in post-treatment LDL reduction and its serum concentrations in R and NR subgroups did not differ statistically for both proliferative and non-proliferative GN.
Serum sFas
Serum sFas levels before treatment did not differ statistically between proliferative and non-proliferative primary glomerulonephritis patients. In comparison to healthy subjects, the sFas serum concentration in both types of GN were significantly higher (P = 0.039 and P = 0.008, respectively). Although the post-treatment serum sFas values decreased in proliferative and non-proliferative GN, the reduction observed was not statistically significant. The results are presented in Table 3. No difference was seen in pre-treatment sFas serum concentrations between treatment response subgroups (R and NR), irrespective of whether proliferative or non-proliferative primary glomerulonephritis was analyzed-Table 4.
Table 3.
Pre and post-treatment serum concentration and urinary excretion of sFas in proliferative and non-proliferative glomerulonephritis (GN)
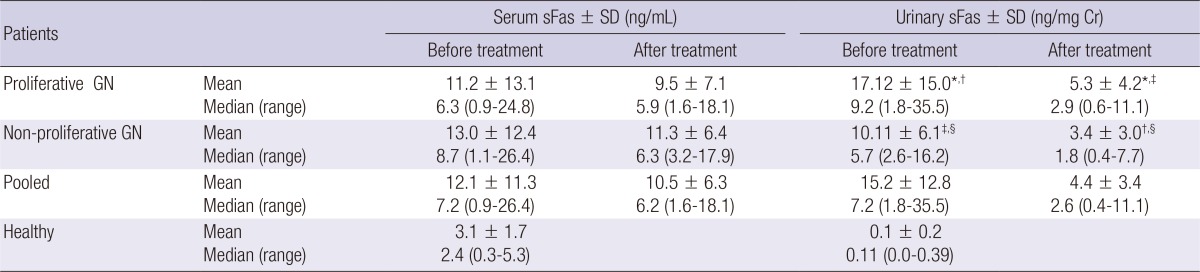
Differences were considered significant for P < 0.05 (Kruskal-Wallis ANOVA). *Proliferative GN before vs after treatment; †Proliferative GN before treatment vs Non-proliferave GN after treatment; ‡Proliferative GN after treatment vs Non-proliferative GN before treatment; §Non-proliferative GN before vs after treatment.
Table 4.
Pre-treatment serum concentration and urinary excretion of sFas in proliferative and non-proliferative glomerulonephritis (GN) divided into Responders (R) and Non-Responders (NR) subgroups
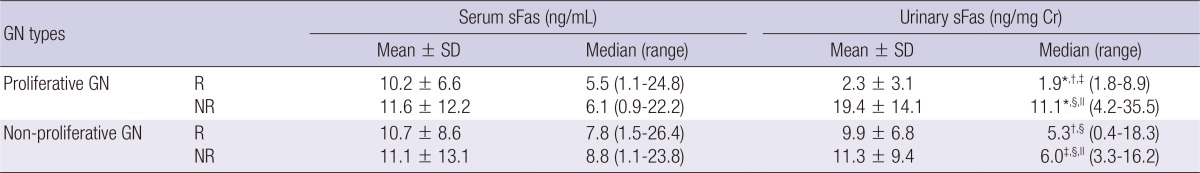
Differences were considered significant for P < 0.05 (Kruskal-Wallis ANOVA); *Proliferative GN R vs NR; †Proliferative GN R vs non-proliferative GN R; ‡Proliferative GN R vs non-proliferative GN NR; §Proliferative GN NR vs non-proliferative GN R; ∥Proliferative GN NR vs non-proliferative GN NR.
With respect to pre- and post-treatment sFas, no correlations between serum concentration and other confounders were found, irrespectively of the type of primary glomerulonephritis.
Urinary sFas
A comparison to the control group showed highly increased sFas urinary excretions in patients with proliferative and non-proliferative primary glomerulonephritis (P = 0.006 and P = 0.007-Table 3). The urinary excretion of sFas before treatment positively correlated with interstitium volume, glomerulosclerosis grade and serum creatinine concentration (ρ = 0.31, P = 0.022; ρ = 0.32, P = 0.025; ρ = 0.35, P = 0.034; respectively). The urinary sFas was higher in PGN than in NPGN (P = 0.042). The treatment significantly reduced urinary sFas in both primary glomerulonephritis types, but sFas urinary excretion was still higher in patients with proliferative GN (P = 0.044). All results are presented in Table 3. The pre-treatment soluble Fas urinary excretion value in PGN positively correlated with interstitium volume, glomerulosclerosis grade and serum creatinine concentration (ρ = 0.33, P = 0.024; ρ = 0.31, P = 0.031; ρ = 0.29, P = 0.019; respectively).
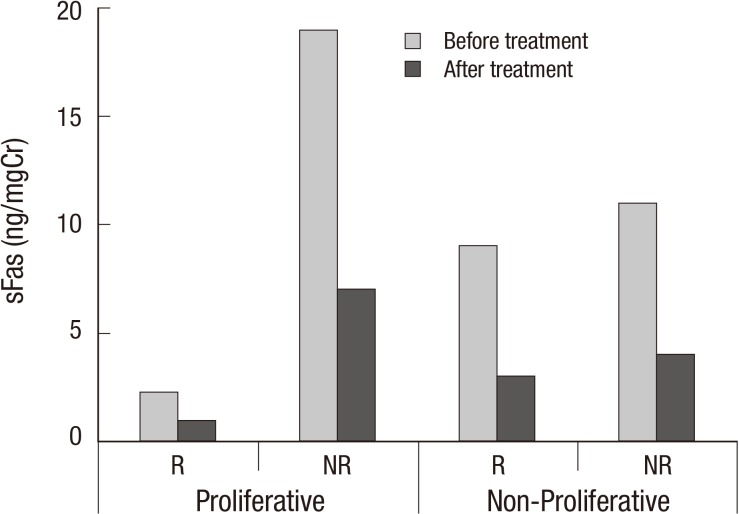
In non-proliferative GN, sFas urinary excretion did not differ between the R and NR subgroups. In contrast, in proliferative glomerulonephritis, the urinary excretion of sFas was significantly lower in the R subgroup than the NR, though the values were still higher than in the healthy subjects (P = 0.033). It is noteworthy that sFas excretion in the R subgroup was significantly reduced in comparison to that of the R and NR subgroups in non-proliferative. Interestingly, urinary sFas in the Non-Responders proliferative GN was higher than both R or NR subgroups in non-proliferative glomerulonephritis (Table 4).
The calculated ROC curve indicated the cut off value of the urinary sFas excretion as 9.68 pg/mg of urinary creatinine and the AUC was 0.88 (95%CI 0.78-0.92). Only Responders in proliferative type of primary glomerulonephritis sFas urinary excretion was lower than calculated cut off value (P = 0.005), furthermore in non of participants from R subgroup of PGN this limit was exceeded (Table 4).
The pre-treatment and post-treatment urinary excretion of sFas in proliferative and non-proliferative glomerulonephritis (GN) divided into Responders (R) and Non-Responders (NR) subgroups are presented on Fig. 1. Irrespectively of the type of GN or to the response to the treatment, all comparisons pointed the significant differences between pre- and after treatment urinary sFas excretion (P < 0.05 for all comparisons).
Fig. 1.
Pre-treatment and post-treatment urinary excretion of sFas in proliferative and non-proliferative glomerulonephritis (GN) divided into Responders (R) and Non-Responders (NR) subgroups.
The Responders pre-treatment urinary sFas value in the proliferative GN group negatively correlated with their post-treatment serum proteins (ρ = -0.273, P = 0.015) and positively with proteinuria and serum creatinine after treatment (ρ = 0.312, P = 0.018 and ρ = 0.262, P = 0.028; respectively). The evaluation of pre-treatment urinary sFas values in Non-Responders (proliferative GN) revealed a positive correlation with post-treatment serum creatinine (ρ = 0.41, P = 0.007) and proteinuria values (ρ = 0.39, P = 0.005). The logistic regression analysis of the pretreatment variables indicated that only the urinary sFas was the exclusive predictive marker of the treatment outcomes in the whole cohort (Table 5).
Table 5.
Multiple logistic regression analysis of the pre-treatment variables which may influence the response to the immunosuppressive treatment (a whole cohort of Responders)
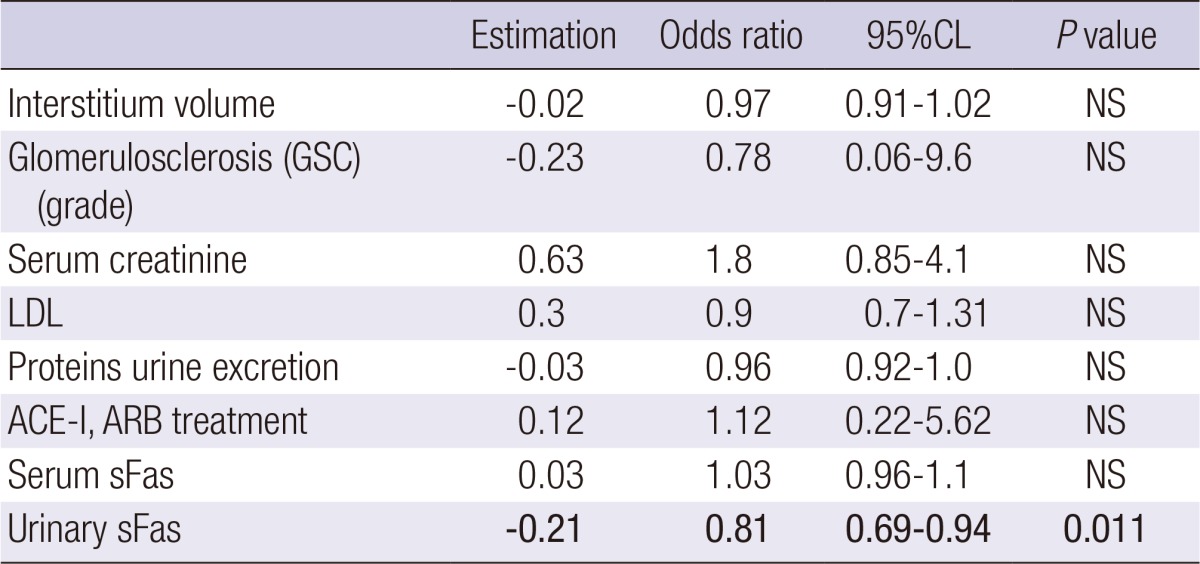
ARB, angiotensin II receptor blocker; ACE-i, converting enzyme inhibitor; GN, glomerulonephritis; NPGN, non-proliferative; LDL, low density lipoproteins.
DISCUSSION
In the present study, only participants with severe proteinuria and/or an increase of serum creatinine were selected. The unsuccessful use of initial isolated steroid therapy (i.v. pulses) necessitated the need for combined treatment with cyclophosphamide in the study cohort. Although this immunosuppressive protocol exceeds the scope of standard therapy for some types of primary glomerulonephritis, many authors suggest its efficacy (21-32). However, the patients to be treated according this therapeutic strategy must be carefully selected, and only subjects with a severe course of GN should be chosen (21-32). In this study, one third of non-proliferative glomerulonephritis and nearly 40% of the patients with proliferative GN, despite the intensive treatment, had no improvement in proteinuria and/or kidney function after therapy prolonged to 1 yr. This appears to confirm the observation that the clinical course of GN still remains unpredictable in a significant number of the patients and therefore no uniform therapeutic strategy based on routine clinical and biochemical assessments can be proposed (32-34). The initial introduction of not radical immunosuppressive schemes may be not sufficient, hence more aggressive therapeutic strategies in those particularly complicated cases merit further investigation (21-32).
However serum sFas in the study group was significantly higher than in the healthy participants and elevated in comparison to other studies (35-37). Pre and post-treatment sFas serum concentrations showed no differences, irrespective of the type of glomerulonephritis. In the present study, highly elevated serum sFas values seem to be associated with a significant deterioration of kidney function in majority of participants. In contrast, in other studies on primary glomerulonephritis, sFas results were obtained mainly in patients with normal or only slightly impaired kidney function (35-37). Identical sFas values obtained in healthy participants in other studies, implying that the chosen methodology is correct (35-37).
Urinary sFas excretion has been occasionally evaluated (37). In the present study, urinary sFas was found to be lower after treatment than before in both the proliferative and non-proliferative GN groups. The decrease in sFas urinary excretion after the introduction of immunosuppressive therapy seems to be a good prognosis of favorable treatment outcome however the pooled result was still higher than the mean urinary sFas in Responders with PGN.
To confirm the potential of baseline sFas measurements in predicting the prognosis of GN, the subdivision into Responders and Non-Responders subgroups was needed. The retrospective analysis of gathered material showed that in proliferative and non-proliferative primary glomerulonephritis, no differences between R and NR subgroups were found with respect to pre-treatment biopsy findings and biochemical data.
The only parameter that varies between the Responders and Non-Responders subgroups is the urinary excretion of sFas in the proliferative GN group. In the Responders subgroup, the action of urinary sFas was comparable with that of urinary sFas described by Kacprzyk (37). In Non-Responders, sFas urinary excretion values were even lower than in patients with IgA nephropathy (37). Although, in R and NR subgroups all post-treatment urinary sFas were lower than pre-treatment, still the lowest was noted in responders with proliferative GN. The presented study results suggested that lower sFas urinary excretion may be linked with a good prognosis, and increased excretion with the risk of glomerulonephritis progression. This is in accord with other studies (37). Also the correlations between urinary sFas and post-treatment creatinine and proteinuria shown here in the proliferative GN group, which are positive in Non-Responders as well as in Responders, highlight the potential value of sFas measurements.
To verify the potency of sFas measurements in predicting GN the cut off value of sFas urinary excretion was calculated using ROC curve. It indicated that sFas urinary excretion was lower only in Responders (proliferative type of primary glomerulonephritis).
sFas inhibits apoptosis and creates the conditions conducive to uncontrolled glomerular and mesangial cell proliferation. It decreases the number of TUNNEL-positive cells in the glomeruli, promoting its progressive injury in the mechanism of apoptosis-proliferation deregulation (36, 37). The significantly increased pre-treatment values for urinary excretion of sFas in Non-Responders with proliferative GN seem to support this.
However, in some types of primary glomerulonephritis, proteinuria is regarded as an independent risk factor and a predictor of renal function deterioration; in some cases, it is not in fact accurate at baseline (38). In others, creatinine clearance, hypertension and severity of biopsy pathological lesions play the key role (39). Surprisingly, in this study, risk factors traditionally regarded as contributory for treatment outcome were found to be unreliable.
The decision to introduce immunosuppressive therapy is strictly based on patient general status, clinical and biochemical parameters. The clinician, basing his decision on own experience and guidelines, is obliged to individualize the treatment to achieve high effectiveness and avoid therapy disadvantages. It appears that the pre-treatment examinations of urinary sFas may become an additional argument in the optimization of treatment. Nevertheless, further studies evaluating sFas in glomerulonephritis, especially the proliferative type, are needed.
In this study, only a selected group of patients with a severe course of GN were evaluated and due to this limitation the number of participants is relatively small. Additionally, all participants were selected to undergo an immunosuppressive treatment protocol selected by the center and not widely recruited, but this was undoubtedly efficient in severe cases of glomerulonephritis (17-28). Although these disadvantages may detract from the results of post-treatment sFas evaluation, and a retrospective analysis (R and NR subdivisions) may be presumed to be less significant than a prospective trial, multivariate logistic evaluation using sFas as an exclusive contributory predictor of therapy outcomes should not be underestimated.
In conclusion, both sFas serum concentration and urinary excretion were highly elevated in patients. The immunosuppressive treatment reduced sFas urinary excretion in proliferative and non-proliferative primary glomerulonephritis. The study results suggest that the lower urinary sFas may be linked with favorable therapy outcomes in patients with proliferative primary glomerulonephritis, however further evaluations are needed.
Footnotes
The author has no conflicts of interest to disclose.
References
- 1.Sato M, Konuma T, Yanagisawa N, Haizuka H, Asakura H, Nakashima Y. Fas-Fas ligand system in the peripheral blood of patients with renal diseases. Nephron. 2000;85:107–113. doi: 10.1159/000045642. [DOI] [PubMed] [Google Scholar]
- 2.Cheng J, Zhou T, Liu C, Shapiro JP, Brauer MJ, Kiefer MC, Barr PJ, Mountz JD. Protection from Fas-mediated apoptosis by a soluble form of the Fas molecule. Science. 1994;263:1759–1762. doi: 10.1126/science.7510905. [DOI] [PubMed] [Google Scholar]
- 3.Fujinaka H, Yamamoto T, Feng L, Nameta M, Garcia G, Chen S, El-shemi AA, Ohshiro K, Katsuyama K, Yoshida Y, et al. Anti-perforin antibody treatment ameliorates experimental crescentic glomerulonephritis in WKY rats. Kidney Int. 2007;72:823–830. doi: 10.1038/sj.ki.5002424. [DOI] [PubMed] [Google Scholar]
- 4.Lorz C, Ortiz A, Justo P, González-Cuadrado S, Duque N, Gómez-Guerrero C, Egido J. Proapoptotic Fas ligand is expressed by normal kidney tubular epithelium and injured glomeruli. J Am Soc Nephrol. 2000;11:1266–1277. doi: 10.1681/ASN.V1171266. [DOI] [PubMed] [Google Scholar]
- 5.Remuzzi G, Bertani T. Is glomerulosclerosis a consequence of altered glomerular permeability to macromolecules? Kidney Int. 1990;38:384–394. doi: 10.1038/ki.1990.217. [DOI] [PubMed] [Google Scholar]
- 6.Couser WG. Glomerulonephritis. Lancet. 1999;353:1509–1515. doi: 10.1016/S0140-6736(98)06195-9. [DOI] [PubMed] [Google Scholar]
- 7.Chatziantoniou C, Boffa JJ, Tharaux PL, Flamant M, Ronco P, Dussaule JC. Progression and regression in renal vascular and glomerular fibrosis. Int J Exp Pathol. 2004;85:1–11. doi: 10.1111/j.0959-9673.2004.00376.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strutz F, Zeisberg M. Renal fibroblasts and myofibroblasts in chronic kidney disease. J Am Soc Nephrol. 2006;17:2992–2998. doi: 10.1681/ASN.2006050420. [DOI] [PubMed] [Google Scholar]
- 9.Coppo R, Ponticelli C. Minimal change nephropathy. In: Ponticelli C, Glassock RJ, editors. Treatment of primary glomerulonephritis. 2nd ed. Oxford: Oxford University Press; 2009. pp. 179–210. [Google Scholar]
- 10.Scolari F, Ponticelli C. Focal and segmental glomerulosclerosis. In: Ponticelli C, Glassock RJ, editors. Treatment of primary glomerulonephritis. 2nd ed. Oxford: Oxford University Press; 2009. pp. 215–256. [Google Scholar]
- 11.Passerini P, Ponticelli C. Membranous nephropathy. In: Ponticelli C, Glassock RJ, editors. Treatment of primary glomerulonephritis. 2nd ed. Oxford: Oxford University Press; 2009. pp. 261–308. [Google Scholar]
- 12.Glassock RJ, Lee G. Immunoglobulin A nephropathy. In: Ponticelli C, Glassock RJ, editors. Treatment of primary glomerulonephritis. 2nd ed. Oxford: Oxford University Press; 2009. pp. 313–361. [Google Scholar]
- 13.Glassock RJ. Membranoprolipherative glomerulonephritis. In: Ponticelli C, Glassock RJ, editors. Treatment of primary glomerulonephritis. 2nd ed. Oxford: Oxford University Press; 2009. pp. 375–393. [Google Scholar]
- 14.D'Amico G. Tubulo-interstitial damage in glomerular diseases: its role in the progression of the renal damage. Nephrol Dial Transplant. 1998;13:80–85. doi: 10.1093/ndt/13.suppl_1.80. [DOI] [PubMed] [Google Scholar]
- 15.Okoń K, Sułowicz W, Smoleński O, Sydor A, Chruściel B, Kirker-Nowak A, Rosiek Z, Sysło K, Stachura J. Predicting kidney function from renal biopsy: semiquantitative versus quantitative approach. Pol J Pathol. 2007;58:65–71. [PubMed] [Google Scholar]
- 16.Fuiano G, Sund S, Mazza G, Rosa M, Caglioti A, Gallo G, Natale G, Andreucci M, Memoli B, De Nicola L, et al. Renal hemodynamic response to maximal vasodilating stimulus in healthy older subjects. Kidney Int. 2001;59:1052–1058. doi: 10.1046/j.1523-1755.2001.0590031052.x. [DOI] [PubMed] [Google Scholar]
- 17.Glassock RJ, Cohen AH. The primary glomerulopathies. Dis Mon. 1996;42:329–383. doi: 10.1016/s0011-5029(96)90021-8. [DOI] [PubMed] [Google Scholar]
- 18.Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009) Hypertens Res. 2009;32:3–107. [PubMed] [Google Scholar]
- 19.Fujita T, Ando K, Nishimura H, Ideura T, Yasuda G, Isshiki M, Takahashi K Cilnidipine versus Amlodipine Randomised Trial for Evaluation in Renal Desease(CARTER) Study Investigators. Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin-angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int. 2007;72:1543–1549. doi: 10.1038/sj.ki.5002623. [DOI] [PubMed] [Google Scholar]
- 20.National Kidney Foundation. K/DOQI clinical practice guidelines for managing dyslipidemias in chronic kidney disease. Am J Kidney Dis. 2003;41:S1–S91. [PubMed] [Google Scholar]
- 21.Yuan J, Fang W, Zhang W, Ni Z, Qian J. Treatment of nephrotic idiopathic membranous nephropathy with monthly i.v. pulse cyclophosphamide and oral steroids: a single centre's retrospective study. Nephrology (Carlton) 2011;16:440–445. doi: 10.1111/j.1440-1797.2010.01427.x. [DOI] [PubMed] [Google Scholar]
- 22.Menon S, Valentini RP. Membranous nephropathy in children: clinical presentation and therapeutic approach. Pediatr Nephrol. 2010;25:1419–1428. doi: 10.1007/s00467-009-1324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cucer F, Miron I, Müller R, Iliescu Halitchi C, Mihaila D. Treatment with Cyclophosphamide for steroid-resistant nephrotic syndrome in children. Maedica (Buchar) 2010;5:167–170. [PMC free article] [PubMed] [Google Scholar]
- 24.Van Husen M, Kemper MJ. New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol. 2011;26:881–892. doi: 10.1007/s00467-010-1717-5. [DOI] [PubMed] [Google Scholar]
- 25.Shenoy M, Plant ND, Lewis MA, Bradbury MG, Lennon R, Webb NJ. Intravenous methylprednisolone in idiopathic childhood nephrotic syndrome. Pediatr Nephrol. 2010;25:899–903. doi: 10.1007/s00467-009-1417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitra N, Abbas M, Nematollah A. Correlation between prognosis and response to treatment in children with FSGS. Acta Med Iran. 2009;47:93–96. [Google Scholar]
- 27.Sümegi V, Haszon I, Bereczki C, Papp F, Túri S. Long-term follow-up after cyclophosphamide and cyclosporine-A therapy in steroid-dependent and -resistant nephrotic syndrome. Pediatr Nephrol. 2008;23:1085–1092. doi: 10.1007/s00467-008-0771-8. [DOI] [PubMed] [Google Scholar]
- 28.Kawasaki Y. The pathogenesis and treatment of pediatric Henoch-Schönlein purpura nephritis. Clin Exp Nephrol. 2011;15:648–657. doi: 10.1007/s10157-011-0478-1. [DOI] [PubMed] [Google Scholar]
- 29.Edström Halling S, Söderberg MP, Berg UB. Treatment of severe Henoch-Schönlein and immunoglobulin A nephritis: a single center experience. Pediatr Nephrol. 2009;24:91–97. doi: 10.1007/s00467-008-0990-z. [DOI] [PubMed] [Google Scholar]
- 30.Oshima S, Kawamura O. Long-term follow-up of patients with IgA nephropathy treated with prednisolone and cyclophosphamide therapy. Clin Exp Nephrol. 2008;12:264–269. doi: 10.1007/s10157-008-0045-6. [DOI] [PubMed] [Google Scholar]
- 31.Gulati S, Sharma AP, Sharma RK, Gupta A, Gupta RK. Do current recommendations for kidney biopsy in nephrotic syndrome need modifications? Pediatr Nephrol. 2002;17:404–408. doi: 10.1007/s00467-002-0840-3. [DOI] [PubMed] [Google Scholar]
- 32.Yagi K, Yanagida H, Sugimoto K, Kuwajima H, Tabata N, Morita K, Okada M, Takemura T. Clinicopathologic features, outcome, and therapeutic interventions in four children with isolated C3 mesangial proliferative glomerulonephritis. Pediatr Nephrol. 2005;20:1273–1278. doi: 10.1007/s00467-005-1919-4. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi Y, Tateno S, Hiki Y, Shigematsu H. IgA nephropathy: prognostic significance of proteinuria and histological alterations. Nephron. 1983;34:146–153. doi: 10.1159/000183000. [DOI] [PubMed] [Google Scholar]
- 34.McQuarrie EP, Shakerdi L, Jardine AG, Fox JG, Mackinnon B. Fractional excretions of albumin and IgG are the best predictors of progression in primary glomerulonephritis. Nephrol Dial Transplant. 2011;26:1563–1569. doi: 10.1093/ndt/gfq605. [DOI] [PubMed] [Google Scholar]
- 35.Shou I, Tashiro K, Kurusu A, Kaneko S, Hayashi T, Fukui M, Shirato I, Kubota K, Tomino Y. Serum levels of soluble Fas and disease activity in patients with IgA nephropathy. Nephron. 1999;81:387–392. doi: 10.1159/000045321. [DOI] [PubMed] [Google Scholar]
- 36.Sano H, Asano K, Minatoguchi S, Hiraoka J, Fujisawa K, Nishigaki K, Yasuda N, Kumada H, Takemura M, Ohashi H, et al. Plasma soluble fas and soluble fas ligand in chronic glomerulonephritis. Nephron. 1998;80:153–161. doi: 10.1159/000045159. [DOI] [PubMed] [Google Scholar]
- 37.Kacprzyk F. Serum level and urinary excretion of soluble Fas (sFas) in patients with primary glomerulopathies. Pol Arch Med Wewn. 2002;108:843–847. [PubMed] [Google Scholar]
- 38.Polanco N, Gutiérrez E, Covarsí A, Ariza F, Carreño A, Vigil A, Baltar J, Fernández-Fresnedo G, Martín C, Pons S, et al. Spontaneous remission of nephrotic syndrome in idiopathic membranous nephropathy. J Am Soc Nephrol. 2010;21:697–704. doi: 10.1681/ASN.2009080861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berthoux F, Mohey H, Laurent B, Mariat C, Afiani A, Thibaudin L. Predicting the risk for dialysis or death in IgA nephropathy. J Am Soc Nephrol. 2011;22:752–761. doi: 10.1681/ASN.2010040355. [DOI] [PMC free article] [PubMed] [Google Scholar]