Abstract
This study aimed to evaluate the predictive performance of genetic risk models based on risk loci identified and/or confirmed in genome-wide association studies for type 2 diabetes mellitus. A systematic literature search was conducted in the PubMed/MEDLINE and EMBASE databases through April 13, 2012, and published data relevant to the prediction of type 2 diabetes based on genome-wide association marker–based risk models (GRMs) were included. Of the 1,234 potentially relevant articles, 21 articles representing 23 studies were eligible for inclusion. The median area under the receiver operating characteristic curve (AUC) among eligible studies was 0.60 (range, 0.55–0.68), which did not differ appreciably by study design, sample size, participants’ race/ethnicity, or the number of genetic markers included in the GRMs. In addition, the AUCs for type 2 diabetes did not improve appreciably with the addition of genetic markers into conventional risk factor–based models (median AUC, 0.79 (range, 0.63–0.91) vs. median AUC, 0.78 (range, 0.63–0.90), respectively). A limited number of included studies used reclassification measures and yielded inconsistent results. In conclusion, GRMs showed a low predictive performance for risk of type 2 diabetes, irrespective of study design, participants’ race/ethnicity, and the number of genetic markers included. Moreover, the addition of genome-wide association markers into conventional risk models produced little improvement in predictive performance.
Keywords: area under the curve, receiver operating characteristic curve, single nucleotide polymorphism, type 2 diabetes mellitus
The global prevalence and burden of type 2 diabetes mellitus (T2DM) have been rising at an alarming rate, creating one of the most important clinical and public health challenges worldwide (1, 2). According to the latest estimate by the International Diabetes Federation (3), the number of diabetes cases worldwide is approximately 366 million, or 8.3%, among adults aged 20–79 years in 2011, and it is projected to reach 552 million, or 9.9%, among adults aged 20–79 years by 2030 (3). T2DM constitutes about 90%–95% of diabetes cases (2). Given the availability of effective lifestyle modifications for preventing or delaying the onset of T2DM in individuals at high risk (4), it is particularly crucial to develop risk prediction tools for use in population-based screening and prevention programs.
Although the pathogenesis of T2DM is not completely understood, the epidemic is widely believed to result from multiple genetic and environmental risk factors and their complex interactions (5, 6). Advanced age, greater body mass index (weight (kg)/height (m)2), smoking, family history of diabetes, high blood pressure, unhealthy diet, and physical inactivity have been identified as important T2DM risk factors. During the past decade, several diabetes risk prediction models and diabetes risk scores incorporating these established risk factors, with and without biochemical markers, have been developed and validated (7, 8). Recently, the advent of genome-wide association (GWA) studies has presented an exciting opportunity to incorporate novel genetic variants into the risk prediction models for T2DM (9). So far, 59 loci associated with T2DM susceptibility (herein called GWA markers) have been identified and/or confirmed at the genome-wide significance level (P < 5 × 10−8) in GWA studies or meta-analyses of GWA studies (10). To translate emerging genomic knowledge into clinical applications, GWA marker–based genetic risk scores or genotype scores have been developed for the prediction of T2DM risk (7, 8, 11). Meanwhile, the “direct-to-consumer” genetic profiling for the prediction of T2DM risk has been offered by commercial companies (12). Studies based on simulated data have also demonstrated that combined information from multiple common genetic variants could improve the prediction of complex diseases (13, 14). However, empirical studies have not provided clear evidence to support the utility of incorporating genomic information into T2DM risk prediction (15–18).
The primary objective of this systematic review was to summarize the predictive performance of genome-wide association marker–based risk models (GRMs) for T2DM risk. The secondary objective was to evaluate whether adding GWA markers to conventional risk factor–based models (CRMs) improves the prediction of T2DM risk.
MATERIALS AND METHODS
Eligibility criteria
We adhered to guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (19) when undertaking this study. The C statistic or area under the receiver operating characteristic curve (AUC) (20–22), the most widely used metric in genetic prediction studies, was the main parameter of the population discriminative ability in this systematic review. The AUC allows comparison of the discriminative accuracy of diverse prediction models independent of the choice of cutoff value in different studies. When the sensitivity and specificity of a test are calculated for each possible cutoff value and plotted as receiver operating characteristic curves, the AUCs, which may vary from 0.5 (no discrimination) to 1 (perfect discrimination), measure the discriminative ability of the test. Recently, reclassification measures (20), including the net reclassification improvement (NRI) and integrated discrimination improvement (IDI), have been used as alternatives to the increase of the AUC for evaluating the incremental predictive performance of GWA markers. Thus, studies were eligible if they reported the AUC or these reclassification measures of GRMs for the prediction of T2DM risk. We did not use odds ratios or risk ratios because the magnitude of genetic associations or effect size does not closely correspond to predictive performance (23, 24).
Data sources and searches
Genetic association studies regarding T2DM prediction were searched in the PubMed/MEDLINE and EMBASE databases through April 13, 2012, by using a combination of free text and subheadings from MeSH and EMTREE terms. The following terms were used for the PubMed/MEDLINE search: (“diabetes mellitus, type 2/genetics”[MeSH] or type 2 diabetes[tiab]) and (“polymorphism, single nucleotide”[MeSH] or “genotype”[MeSH] or “alleles”[MeSH] or “genetic variation”[MeSH] or (“genetic risk score*”) or (“genetic score*”) or (“genotype score*”) or (“genetic variant*”) or genotype*[tiab] or allele*[tiab]) and (“ROC curve”[MeSH] or “area under curve”[MeSH] or “area under the curve” or “AUC” or “AUCs” or “AROC” or (“C statistic*”) or predict*[tiab] or discriminat*[tiab] or reclassification or net reclassification improvement or integrated discrimination improvement), not (review[pt] or editorial[pt]). Similar search terms were used for the EMBASE database. In addition, the references listed in relevant articles were screened. No restrictions on language, geographical location, or study design (e.g., cross-sectional, case-control, cohort study) were applied in the literature search process; however, conference abstracts without sufficient data were not included.
Study selection
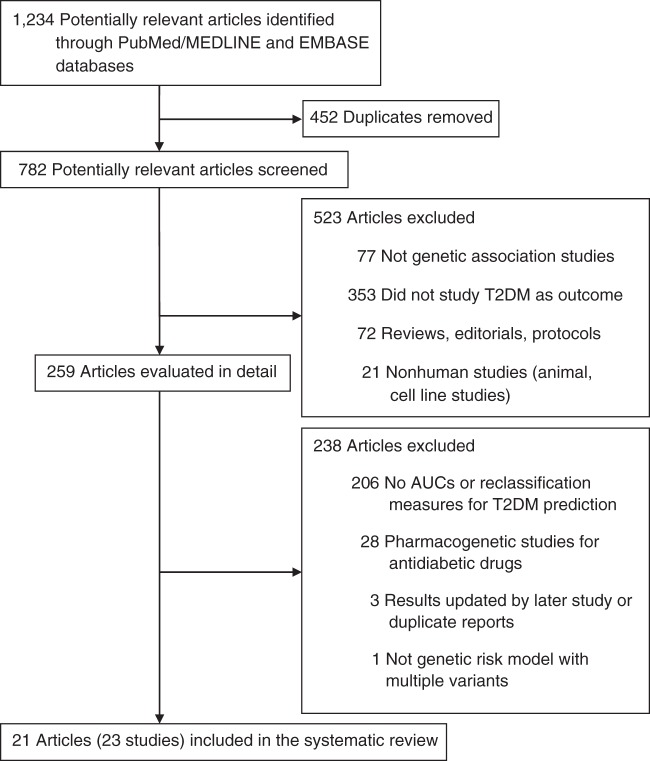
All of the indexed articles were evaluated independently by 2 reviewers (S.R. and Y.R.), and disagreements regarding eligibility were solved in consultation with a third reviewer (W.B.). The process of study selection is depicted in Figure 1. During the screening steps, we excluded review articles, editorials, and protocols, as well as the following study types: nonhuman studies (cell culture or animal studies); studies that did not assess genetic associations; studies with outcomes of obesity, prediabetes, metabolic syndrome, or other diseases but not T2DM; studies on quantitative traits for T2DM (e.g., glucose, insulin, hemoglobin A1c, lipid parameters, insulin sensitivity, β cell function); and studies on T2DM complications or concomitant diseases. In addition, pharmacogenetic or pharmacogenomic studies for antidiabetic drugs and genetic association studies that did not report the predictive performance of GWA markers for T2DM were also excluded. Three additional articles (16, 25, 26) were excluded because either their results (16, 25) were updated by the same group in more recent reports (15, 27), or the results (26) were previously reported in the same population (28). Another article was excluded because it did not report data separately for prediabetes and T2DM (29).
Figure 1.
Flow chart for study selection. AUC, area under the receiver operating characteristic curve; T2DM, type 2 diabetes mellitus.
Data extraction and quality assessment
Two reviewers (W.B. and S.R.) independently extracted data and evaluated study quality, and disagreements were solved by consensus. The following data were extracted from each published article: author's name, year of publication, characteristics of study subjects (e.g., age, sex, body mass index), sample size, genetic variants, AUC or reclassification measures, and consistency of genotype frequencies with Hardy-Weinberg equilibrium, if available. In studies that reported combined effects in prediction models incorporating both GWA markers and nongenetic risk factors, information about the nongenetic risk model was also extracted.
To assess study quality, we considered items in the Strengthening the Reporting of Genetic Risk Prediction Studies statement (30). We particularly evaluated the following items: study design (cross-sectional, case-control or prospective cohort), selection criteria and basic characteristics for participants in the study, genetic variants definition, measurement, coding, and risk model construction.
Data synthesis and analysis
AUCs for T2DM were the main measures in this systematic review because they were reported in almost all of the included studies. In addition, we reviewed the studies in which reclassification measures (i.e., NRI and/or IDI) were reported.
For studies that reported multiple AUCs for different genetic models, the model with the most comprehensive information was used. Statistical meta-analysis of the AUCs and their 95% confidence intervals was conducted to quantitatively summarize the findings in the included studies, and the detailed methods and results are shown in the Web Appendix and in Web Figures 1–4 available at http://aje.oxfordjournals.org/. Because of the various components included in the risk prediction models and the large heterogeneity of data, a descriptive summary (i.e., median) of AUCs and their ranges (minimum to maximum) were used in the main text. Stratification analyses were conducted according to study design (cross-sectional, case-control, and prospective cohort); sample size (i.e., number of T2DM cases); race/ethnicity (Caucasian, Asian, or other); the number of genetic variants included in the GRMs (<10, 10–19, or ≥20); and the average age at diagnosis of T2DM (<50 years or ≥50 years).
For our primary objective, cross-sectional, case-control, and cohort studies were all eligible for inclusion because there was no concern about the temporal causality between exposure (i.e., genotypes that were predetermined during gamete formation and conception) and outcome (i.e., T2DM). For the secondary objective, we restricted the analysis to cohort studies because of the possibility of reverse causality between conventional risk factors and T2DM (e.g., individuals with T2DM may change their lifestyles after diagnosis) that might arise in cross-sectional and case-control studies.
RESULTS
Study characteristics
We identified 1,234 potentially relevant articles from the PubMed/MEDLINE and EMBASE databases. After screening, we evaluated 259 articles in detail. Finally, 21 articles representing 23 studies (15, 27, 28, 31–49) published through April 13, 2012, were eligible for this systematic review (Figure 1). The studies by Lyssenko et al. (15) and Xu et al. (47) comprised 2 independent populations; therefore, they were treated as 2 studies in each of the articles. The study design, participants’ characteristics, and predictive performance for T2DM by using genetic risk models, conventional risk models, and combined models in the individual studies are shown in Tables 1 and 2. Of these eligible studies, 13 were conducted in Europe, 6 in Asia, 3 in the United States, and 1 in North Africa; 11 were prospective cohort studies, 9 were case-control studies, and 3 were cross-sectional studies. Most studies, but not all (33, 40, 41, 44), reported sufficient detail about selection criteria and basic characteristics for participants in the study population. All studies described the selection and measurement of genetic variants and the construction of GRMs. The number of genetic variants in the GRMs ranged from 3 to 40. The most common GWA markers included in the GRMs were solute carrier family 30 (zinc transporter), member 8 (SLC30A8) rs13266634; cyclin-dependent kinase inhibitor 2A/2B (CDKN2A/2B) rs10811661; transcription factor 7-like 2 (TCF7L2) rs7903146; hematopoietically expressed homeobox (HHEX) insulin-degrading enzyme (IDE) rs1111875; insulin-like growth factor 2 mRNA binding protein 2 (IGF2BP2) rs4402960; JAZF zinc finger 1 (JAZF1) rs864745; thyroid adenoma-associated (THADA) rs7578597; and ADAM metallopeptidase with thrombospondin type 1 motif, 9 (ADAMTS9) rs4607103. The most common components in the CRMs were age, sex, and body mass index. Additional components included blood pressure, waist circumference, family history of diabetes, and biochemical markers (e.g., fasting plasma glucose, triglycerides, high-density lipoprotein cholesterol). In addition, 3 studies included established diabetes risk scores as the CRMs, such as the Finnish Diabetes Risk Score (41), the German Diabetes Risk Score (37), the Cambridge Diabetes Risk Score (40), and the Framingham Offspring Diabetes Risk Score (40) (Web Table 1).
Table 1.
Study Design and Participant Characteristics for the Studies Included in the Systematic Review
| First Author, Year (Reference No.) | Study Location | Ethnic Origin | Study Design | No. of Participants |
Age, yearsa |
Male Sex, % |
BMIb |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | ||||
| Weedon, 2006 (31) | United Kingdom | Caucasian | Case-control | 2,409 | 3,668 | 48.7 | 31.8 | 58 | 50 | 31.4 | 27.2 |
| Cauchi, 2008 (43) | France | Caucasian | Case-control | 3,295 | 3,595 | 62 | 56 | 61.8 | 42.3 | 28.3 | 24.9 |
| Cauchi, 2008 (43) | France | Caucasian | Case-control | 937 | 1,000 | 66 | 50 | 61.7 | 42.8 | 31.1 | 24.1 |
| Lango, 2008 (32) | United Kingdom | Caucasian | Cohort | 2,309 | 2,598 | 55.7 | NA | 56 | 51 | 31.5 | 26.9 |
| Lyssenko, 2008 (15) | Sweden | Caucasian | Cohort | 2,063 | 13,998 | 45.5c | 64.9c | 24.3c | |||
| Lyssenko, 2008 (15) | Finland | Caucasian | Cohort | 138 | 2,632 | 44.9c | 45.5c | 25.6c | |||
| van Hoek, 2008 (28) | The Netherlands | Caucasian | Cohort | 601 | 5,221 | 68.2 | 69.0 | 44.3 | 40.4 | 28.0 | 26.0 |
| Vaxillaire, 2008 (33) | France | Caucasian | Cohort | 523 | 2,919 | NA | NA | NA | NA | NA | NA |
| Cornelis, 2009 (34) | United States | Caucasian | Cohort (men) | 1,197 | 1,338 | 55.7 | 55.4 | 100 | 100 | 27.8 | 25.1 |
| Cornelis, 2009 (34) | United States | Caucasian | Cohort (women) | 1,612 | 2,163 | 44.1 | 43.6 | 0 | 0 | 27.7 | 23.9 |
| Hu, 2009 (35) | China | Asian | Case-control | 1,849 | 1,785 | 61.2 | 57.4 | 52.5 | 41.2 | 24.0 | 23.6 |
| Lin, 2009 (36) | Switzerland | Caucasian | Cross-sectional | 356 | 5,004 | 60.7 | 52.8 | 67.4 | 46.0 | 30.4 | 25.5 |
| Miyake, 2009 (45) | Japan | Asian | Case-control | 2,316 | 2,370 | 61.3 | 67.5 | 58.2 | 45.9 | 23.6 | 23.3 |
| Schulze, 2009 (37) | Germany | Caucasian | Cohort | 579 | 1,962 | 54.6 | 49.4 | 58.7 | 36.9 | 30.4 | 25.9 |
| Sparsø, 2009 (38) | Denmark | Caucasian | Case-control | 4,093 | 5,302 | 60 | 47 | 59.3 | 46.3 | 30.6 | 25.6 |
| Fontaine-Bisson, 2010 (46) | Sweden | Caucasian | Cross-sectional | 1,327 | 1,424 | 53.6 | 53.1 | 58.4 | 50.2 | 29.5 | 25.8 |
| Qi, 2010 (39) | China | Asian | Case-control | 424 | 1,908 | 58.6 | 58.8 | 51.2 | 58.5 | 25.8 | 23.8 |
| Talmud, 2010 (40) | United Kingdom | Caucasian | Cohort | 302 | 5,233 | 49c | 67c | NA | NA | ||
| Wang, 2010 (41) | Finland | Caucasian | Cross-sectional | 518 | 6,714 | 45–74d | NA | NA | NA | NA | |
| Xu, 2010 (47) | China | Asian | Case-control | 1,825 | 2,200 | 63.3 | 59.3 | 43.9 | 38.4 | 26.3 | 24.3 |
| Xu, 2010 (47) | China | Asian | Cohort | 67 | 667 | 61.5 | 61.0 | 35.8 | 36.7 | 26.1 | 24.8 |
| de Miguel-Yanes, 2011 (27) | United States | Caucasian | Cohort | 446 | 3,025 | 46c | 46.5c | 26.0c | |||
| Hivert, 2011 (48) | United States | Mixed | Cohort | 2,843c | 50.6c | 33.2c | 34.0c | ||||
| Cauchi, 2012 (49) | Morocco | Arab | Case-control | 1,193 | 1,055 | 58 | 54 | 65.6 | 69.7 | 28.4 | 27.7 |
| Cauchi, 2012 (49) | Tunisia | Arab | Case-control | 1,446 | 942 | 61 | 61 | 54.2 | 55.7 | 27.6 | 24.4 |
| Janipalli, 2012 (42) | India | Asian | Case-control | 1,808 | 1,549 | 47.7 | NA | 55.8 | 53.2 | 25.7 | 19.4 |
Abbreviations: BMI, body mass index; NA, not available.
a Age indicates average age at diagnosis or testing.
b Calculated as weight (kg)/height (m)2.
c Values represent the entire cohort.
d Age range for the entire cohort.
Table 2.
AUCs for Genetic Risk Models, Conventional Risk Models, and Combined Models for Predicting Risk of Type 2 Diabetes in the Studies Included in the Systematic Review
| First Author, Year (Reference No.) | Study Location | Genetic Risk Modela |
Conventional Risk Modelb |
Combined Modelc |
P Valued | |||
|---|---|---|---|---|---|---|---|---|
| AUC | 95% CI | AUC | 95% CI | AUC | 95% CI | |||
| Weedon, 2006 (31) | United Kingdom | 0.58 | 0.57, 0.59 | NA | NA | NA | NA | NA |
| Cauchi, 2008 (43) | France | NA | NA | NA | NA | 0.86 | NA | NA |
| Lango, 2008 (32) | United Kingdom | 0.60 | 0.58, 0.62 | 0.78 | 0.77, 0.79 | 0.80 | 0.79, 0.81 | 2.9 × 10−12 |
| Lyssenko, 2008 (15) | Sweden | 0.62 | 0.61, 0.63 | 0.74 | 0.73, 0.75 | 0.75 | 0.74, 0.76 | 1.0 × 10−4 |
| Lyssenko, 2008 (15) | Finland | 0.68 | 0.63, 0.73 | 0.79 | 0.74, 0.84 | 0.80 | 0.76, 0.84 | NA |
| van Hoek, 2008 (28) | The Netherlands | 0.60 | 0.57, 0.63 | 0.66 | 0.63, 0.68 | 0.68 | 0.66, 0.71 | <0.0001 |
| Vaxillaire, 2008 (33) | France | 0.56 | 0.53, 0.59 | 0.82 | 0.82, 0.83 | 0.83 | 0.82, 0.83 | 0.26 |
| Cornelis, 2009 (34) | United States | 0.59 | 0.57, 0.60 | 0.78 | 0.77, 0.79 | 0.79 | 0.78, 0.80 | <0.001 |
| Hu, 2009 (35) | China | 0.62 | 0.60, 0.64 | 0.61 | 0.60, 0.63 | 0.67 | 0.65, 0.69 | 0.0002 |
| Lin, 2009 (36) | Switzerland | 0.57 | 0.54, 0.60 | 0.86 | 0.84, 0.88 | 0.87 | 0.85, 0.89 | 0.002 |
| Miyake, 2009 (45) | Japan | 0.63 | NA | 0.68 | NA | 0.72 | NA | NA |
| Schulze, 2009 (37) | Germany | 0.55 | 0.53, 0.58 | 0.90 | 0.89, 0.91 | 0.90 | 0.89, 0.91 | 0.6868 |
| Sparsø, 2009 (38) | Denmark | 0.60 | 0.59, 0.61 | 0.92 | 0.91, 0.93 | 0.93 | 0.92, 0.94 | NA |
| Fontaine-Bisson, 2010 (46) | Sweden | 0.59 | NA | NA | NA | NA | NA | NA |
| Qi, 2010 (39) | China | 0.62 | 0.59, 0.65 | 0.77 | 0.74, 0.80 | 0.79 | 0.76, 0.81 | 0.007 |
| Talmud, 2010 (40) | United Kingdom | 0.55 | 0.51, 0.59 | 0.78 | 0.75, 0.82 | 0.78 | 0.74, 0.81 | 0.10 |
| Wang, 2010 (41) | Finland | 0.55 | 0.53, 0.58 | 0.77 | 0.75, 0.79 | 0.77 | 0.75, 0.79 | NA |
| Xu, 2010 (47) | China | NA | NA | 0.71 | NA | 0.73 | NA | NA |
| Xu, 2010 (47) | China | NA | NA | 0.63 | NA | 0.66 | NA | NA |
| de Miguel-Yanes, 2011 (27) | United States | 0.63 | 0.61, 0.66 | 0.90 | 0.89, 0.92 | 0.91 | 0.89, 0.92 | 0.01 |
| Hivert, 2011 (48) | United States | NA | NA | 0.63 | NA | 0.63 | NA | 0.34 |
| Cauchi, 2012 (49) | Morocco and Tunisia | 0.60 | NA | 0.64 | NA | 0.67 | NA | 0.004 |
| Janipalli, 2012 (42) | India | 0.63 | 0.62, 0.65 | 0.96 | 0.95, 0.97 | 0.96 | 0.96, 0.97 | 0.001 |
Abbreviations: AUC, area under the curve; CI, confidence interval; GWA, genome-wide association; NA, not available; T2DM, type 2 diabetes mellitus.
a Risk prediction model based on genetic variants identified and/or confirmed in GWA studies of T2DM.
b Risk prediction model based on conventional risk factors of T2DM (e.g., age, sex, body mass index (weight (kg)/height (m)2), family history of diabetes).
c Risk prediction model based on both genetic variants identified or confirmed in GWA studies of T2DM and conventional risk factors of T2DM.
d P value for difference between the AUC for type 2 diabetes with a conventional risk factor–based model and with a combined model, indicating the incremental value when adding GWA markers into the conventional risk factor–based model.
Predictive performance of GRMs
The predictive performance of GRMs for T2DM was reported in 19 of the 23 eligible studies. In general, GRMs showed a relatively poor discrimination for T2DM in all studies (Table 2). The AUCs ranged from 0.55 to 0.68 with a median of 0.60.
In our subgroup analyses stratified by study design, sample size (i.e., number of T2DM cases) and race/ethnicity (Table 3), the median AUCs were as follows: for case-control studies, 0.62 (range, 0.58–0.63); for cohort studies, 0.60 (range, 0.55–0.68); for cross-sectional studies, 0.57 (range, 0.55–0.59); for studies with fewer than 1,000 T2DM cases, 0.57 (range, 0.55–0.68); for studies with 1,000–1,999 T2DM cases, 0.61 (range, 0.59–0.63); for studies with 2,000 or more T2DM cases, 0.60 (range, 0.58–0.63); for studies of Caucasians, 0.59 (range, 0.55–0.68); and for studies of Asians, 0.63 (range, 0.62–0.63).
Table 3.
Predictive Performance of GWA Marker–Based Genetic Risk Models for T2DM by Study Characteristics in the Included Studies
| Study Characteristic | No. of Studies | AUC |
|
|---|---|---|---|
| Median | Range | ||
| Study design | |||
| Case-control | 7 | 0.62 | 0.58–0.63 |
| Cohort | 9 | 0.60 | 0.55–0.68 |
| Cross-sectional | 3 | 0.57 | 0.55–0.59 |
| No. of T2DM cases | |||
| <1,000 | 9 | 0.57 | 0.55–0.68 |
| 1,000–1,999 | 4 | 0.61 | 0.59–0.63 |
| ≥2,000 | 6 | 0.60 | 0.58–0.63 |
| Race/ethnicity | |||
| Caucasian | 14 | 0.59 | 0.55–0.68 |
| Asian | 4 | 0.63 | 0.62–0.63 |
| Arab-African | 1 | 0.60 | |
| No. of variants | |||
| <10 | 2 | 0.57 | 0.56–0.58 |
| 10–19 | 13 | 0.60 | 0.55–0.68 |
| ≥20 | 4 | 0.59 | 0.55–0.63 |
| Average age at diagnosis of T2DM, years | |||
| <50 | 5 | 0.62 | 0.55–0.68 |
| ≥50 | 10 | 0.60 | 0.55–0.63 |
| Mixeda | 3 | 0.59 | 0.55–0.63 |
Abbreviations: AUC, area under the receiver operating characteristic curve; GWA, genome-wide association; T2DM, type 2 diabetes mellitus.
a Indicates studies that had multiple groups of participants with varying mean ages of below or above 50 years.
We also examined whether the AUCs for T2DM varied by the number of genetic variants included in the GRMs, because the Framingham Offspring Study showed that increasing the number of GWA markers in the GRMs from 18 in a previous report (16) to 40 in a recent report (27) improved the AUC for T2DM risk prediction, although the predictive performance of the updated model was still limited, and the magnitude of the change between the median AUCs was small (0.58 (range, 0.55–0.62) vs. 0.63 (range, 0.61–0.66)). In a subgroup study stratified by the number of genetic variants included in the GRMs, the median AUCs for T2DM were 0.57 (range, 0.56–0.58), 0.60 (range, 0.55–0.68), and 0.59 (range, 0.55–0.63) for GRMs including <10, 10–19, and ≥20 genetic variants, respectively.
In addition, a recent report suggested that the predictive performance of GRMs may vary by participant age (27). Therefore, we performed a subgroup analysis of cases by age (mean or median) at diagnosis or testing. We found a slightly higher AUC for studies with an average age of study participants younger than 50 years compared with those that included older study participants (with median AUCs of 0.62 (range, 0.55–0.68) and 0.60 (range, 0.55–0.63), respectively).
Predictive performance of GWA markers versus CRMs
To assess the incremental improvement in predictive performance of GWA markers beyond that of CRMs for T2DM risk, we included prospective cohort studies in which AUCs and 95% confidence intervals for CRMs with and without the addition of GRMs were reported. Among the 11 prospective cohort studies, the median AUCs were 0.78 (range, 0.63–0.90) for the CRMs and 0.79 (range, 0.63–0.91) for combined models that included both conventional risk factors and GWA markers.
In addition to reporting AUCs, several studies (15, 27, 36, 37, 40, 48) also reported reclassification measures as metrics for incremental predictive performance (Table 4). The categorical NRI is a cutoff point–dependent measure; however, the cutoff points were quite different among studies that reported NRI (15, 27, 40). Among studies that reported IDI (36, 37, 48), only 1 provided sufficient information on IDI and its 95% confidence interval (37). The results reported in the included studies were inconsistent; some studies found statistically significant improvement in NRI and/or IDI (15, 27, 36), whereas others did not (40, 48). However, even in studies that reported statistically significant improvement, the magnitude of NRI and/or IDI was modest (∼4.5% for NRI (15, 27) and 1.2% for relative IDI (36)) compared with results (NRI of ≤39% and IDI of ≤7.8%) from an empirical evaluation of the use of reclassification for assessment of improved prediction (50). This is consistent with the results of an ad hoc study showing that reclassification observed in the absence of an increase of AUC is unlikely to improve clinical utility (21).
Table 4.
Reclassification of GWA Study–Derived Genetic Risk Variants for T2DM Added to Conventional Risk Factor–Based Models in the Included Studies
| First Author, Year (Reference No.) | Study Location | Ethnic Origin | Study Type | No. of Variants | Conventional T2DM Risk Factors | Cutoff Points, %a | NRI |
IDI |
||
|---|---|---|---|---|---|---|---|---|---|---|
| % | P Value | % | P Value | |||||||
| Lyssenko, 2008 (15) | Sweden | Caucasian | Cohort | 11 | Age, sex, BMIb, FH, FPG, BP, TG | 10 and 20 | 4.5 | 2.5 × 10−5 | NA | 3.7 × 10−14 |
| Finland | Caucasian | Cohort | 11 | Age, sex, BMI, FH, FPG, BP, TG, HDL-C, waist circumference | 10 and 20 | 8.79 | 0.13 | NA | 0.001 | |
| Lin, 2009 (36) | Switzerland | Caucasian | Cross-sectional | 15 | Age, BMI, FH, WHR, TG/HDL-C | NA | NA | NA | 1.2 | 0.0003 |
| Schulze, 2009 (37) | Germany | Caucasian | Cohort | 20 | German Diabetes Risk Scorec, FPG, HbA1c, TG, HDL-C, GGT, ALT | NA | NA | NA | 0.34 | NA |
| Talmud, 2010 (40) | United Kingdom | Caucasian | Cohort | 20 | Cambridge Diabetes Risk Scored | 5, 10, and 15 | 4.6 | 0.17 | NA | NA |
| Talmud, 2010 (40) | United Kingdom | Caucasian | Cohort | 20 | Framingham Offspring Study T2DM Risk Scoree | 5, 10, and 15 | −3.2 | 0.35 | NA | NA |
| de Miguel-Yanes, 2011 (27) | United States | Caucasian | Cohort | 40 | Age, sex, BMI, FH, FPG, SBP, HDL-C, TG | 2 and 8 | 4.3 | 0.004 | NA | NA |
| Hivert, 2011 (48) | United States | Mixed | Cohort | 34 | Age, sex, ethnic background, treatment arm, and waist circumference | NA | NA | NA | −0.007 | 0.10 |
Abbreviations: ALT, alanine transaminase; BMI, body mass index; BP, blood pressure; FH, family history of diabetes; FPG, fasting plasma glucose; GGT, γ-glutamyltransferase; GWA, genome-wide association; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; IDI, integrated discrimination improvement; NA, not applicable or not available; NRI, net reclassification improvement; T2DM, type 2 diabetes mellitus; TG, triglycerides; WHR, waist-hip ratio.
a Predefined cutoff point for reclassification based on the likelihood of developing T2DM.
b Calculated as weight (kg)/height (m)2.
c The German Diabetes Risk Score includes age, waist circumference, height, history of hypertension, physical activity, smoking, and consumption of red meat, whole-grain bread, coffee, and alcohol.
d The Cambridge Diabetes Risk Score includes age, sex, drug treatment, FH, BMI, and smoking status.
e The Framingham Offspring Study Type 2 Diabetes Risk Score includes age, sex, parental history of T2DM, BMI, HDL-C, TG, and FPG.
DISCUSSION
In the current systematic review, we found that GRMs showed a relatively low predictive performance for T2DM risk irrespective of study design, participants’ race/ethnicity (i.e., Caucasian or Asian), and the number of genetic markers included, despite the fact that the associations of the included GWA markers with T2DM risk have been well established and replicated in previous studies (51–54). The risk prediction models for T2DM have been previously reviewed (7, 8, 11, 55); however, all of these reviews except Mihaescu et al. (11) focused mainly on the conventional risk factor–based models. Our results support the notion that known T2DM GWA markers add minimally to the predictive performance for T2DM beyond that of conventional risk factors (15, 16).
Genetic testing has been suggested for identifying individuals at risk of developing T2DM (25). Indeed, compared with nongenetic risk factors, genetic variants, such as single nucleotide polymorphisms (SNPs), have some unique features in that they are predetermined during gamete formation and conception, they do not change over time, and the temporal sequence of genotype-phenotype can be clearly established for outcome predictions (56). However, the predictive performance of genetic variants for T2DM may have been overestimated (57). Although an early study indicated an impressive 20-fold increased risk of T2DM by using the combination of 3 genetic variants among individuals who were obese and who had elevated fasting plasma glucose values (25), the discriminative accuracy for T2DM risk prediction did not significantly improve in a reexamination of the same study (23). In the present study, we found that the AUCs of GRMs for T2DM was relatively low, and CRMs, which incorporate age, BMI, and other factors, demonstrated appreciably higher AUCs than did GRMs. One may speculate that genetic profiling, theoretically, could be more useful for predicting T2DM risk among younger individuals who have not yet developed conventional risk factors. This hypothesis was tested recently among white and black adolescents (58) and young adults (59); both studies found that GRMs did not improve the predictive performance of T2DM compared with assessment of clinical risk factors.
The predictive performance of genetic markers for T2DM risk could be improved in future studies through several approaches. First, simulation studies suggest that the cumulative effect of a large number of common genetic variants could lead to an increased AUC for complex disease prediction (13, 14). According to mathematical modeling by Janssens et al. (60), to increase the AUC of genetic profiling to 0.80 or greater, 400 genetic variants with minor allele frequencies of 10% and odds ratios of the heterozygous genotypes for each variant greater than 1.25 are needed. Currently identified and/or confirmed GWA markers for T2DM are still limited, and the majority of them have a modest association with T2DM (odds ratios of heterozygous genotypes are less than 1.15 for most GWA markers); thus, it is not surprising that the AUC values for T2DM did not vary substantially according to the number of GWA markers (n ≤ 40) in this study. Although it has been found that known GWA markers explain only a limited proportion of the estimated genetic variation for T2DM, which suggests the existence of “missing” heritability (61), whether hundreds of common genetic variants for T2DM will be identified through GWA studies is unknown. Second, with the application of large-scale exon resequencing and next-generation sequencing technologies (62), rare variants for T2DM are likely to be uncovered (63). An empirical analysis suggested that the inclusion of rare variants might have appreciable effects on disease risk prediction (64). However, whether adding rare variants will improve the predictive performance for T2DM remains to be evaluated. Third, whether the incorporation of additional susceptibility loci discovered through novel liability methods (65) and obesity-predisposing SNPs (66) will improve the predictive performance for T2DM warrants further investigation.
It has been speculated that genetic profiling of GWA markers might motivate people who carry the risk variants to change their dietary and lifestyle habits that lead to T2DM (57); however, emerging evidence, although still limited, does not support this notion (67). A recent observational study showed that genome-wide profiling did not result in any measurable short-term changes in diet or exercise behavior (68), although long-term effects remain unknown. Moreover, a randomized trial also showed that diabetes genetic risk counseling with currently available variants does not significantly alter self-reported motivation or prevention program adherence for overweight individuals at risk for diabetes (67). Although it has been demonstrated that broad, population-based lifestyle interventions are effective at reducing the risk of T2DM in high-risk individuals (4), whether personalized interventions based on individual genetic backgrounds may increase the effectiveness warrants further evaluation (69, 70).
It should be noted that the ideal statistical measure of the incremental predictive performance of novel risk markers has been controversial. Most previous studies about the effect of GWA markers on T2DM risk prediction have focused on the AUC, which has been regarded as a standard measure of the effect of a new marker in risk prediction (71). However, the AUC is relatively insensitive to change if a few risk factors with strong associations with T2DM are already included in the model (20, 71). In addition, statistical issues regarding hypothesis testing of changes in AUCs have been documented (72–74). For example, under the null hypothesis, the DeLong test (75), the widely used nonparametric test for evaluating incremental AUCs in prediction models, has an exceptionally conservative test size and much lower power than the likelihood ratio and Wald tests (73). In addition, AUCs may also lack applicability to an individual patient in a clinical setting. As noted by Cook (76), a biomarker with an odds ratio of 3 may have little effect on the AUC, yet an increased level could shift an individual patient's risk from 8% to 24%, leading to different treatment recommendations. Recently, several new measures have been proposed as alternatives to discrimination measures, including reclassification measures (e.g., NRI and IDI) and decision-analytical measures (77). Among them, the classical NRI, also called categorical NRI, is highly dependent on the cutoff points of risk categories; thus, it is not appropriate for meta-analysis. IDI is category free and seems to be a promising complement to the AUC; however, a recent study showed that current methods for hypothesis testing with the IDI are invalid (78). Other novel measures, such as the continuous NRI (79) and the net benefit plotted by the “decision curves” (80), have not yet widely been used in practice. Thus, an empirical evaluation of the utility of these novel measures for assessing the incremental predictive performance of GWA markers in T2DM prediction is warranted.
Some limitations should be acknowledged. First, current GRMs are based on common SNPs, which represent only part of the genetic variation in the human genome (81). Whether the addition of rare SNPs and other genetic variants, such as copy number variations, which account for more than 12% of the assembled human genome sequence (82), will improve the predictive performance for risk of T2DM remains unanswered. It should be noted that a recent GWA study showed that common copy number variants that can be genotyped on existing platforms are unlikely to contribute substantially to the genetic basis of T2DM, and most of them are well tagged by SNPs (83). Second, most of the available studies were performed among Caucasians and Asians. Whether these results can be generalized to other ethnic groups warrants further investigation. Third, the role of gene-environment interactions in the prediction of T2DM was not addressed in this review because of limited available data. Both genetic and environmental factors (e.g., diet, lifestyle) and their complex interactions are implicated in the development of T2DM (5, 6), and available evidence suggests that individuals with higher genetic susceptibility of T2DM may benefit more from dietary and lifestyle changes. For instance, in the US Health Professionals Follow-up Study, the positive association between the Western dietary pattern and the risk of T2DM was more pronounced among men with a higher genetic risk score (≥12) than in those with a lower score (84). Moreover, the Diabetes Prevention Program suggested that lifestyle intervention might mitigate the elevated risk of T2DM conferred by variants of the TCF7L2 gene (85). However, a recent study showed that the inclusion of gene-environment interactions was unlikely to dramatically improve risk prediction for several types of complex diseases, including T2DM (86).
In summary, GRMs showed a relatively low predictive performance for T2DM risk regardless of study design, sample size, participants’ race/ethnicity (i.e., Caucasian, Asian), and the number of genetic markers included. Moreover, the addition of GWA markers to CRMs produced a minor improvement in predictive performance. Therefore, although the identification of GWA markers could help improve our understanding of the pathophysiology of T2DM, its clinical utility in improving the prediction of T2DM beyond that of conventional risk factors may be limited. Further investigation of the predictive performance of the genetic factors and their interactions with environmental factors is warranted.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Epidemiology Branch, Division of Epidemiology, Statistics, and Prevention Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Rockville, Maryland (Wei Bao, Katherine Bowers, Enrique F. Schisterman, Cuilin Zhang); Department of Nutrition and Food Hygiene, Hubei Key Laboratory of Food Nutrition and Safety, Ministry of Education Key Laboratory of Environment and Health, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China (Wei Bao, Shuang Rong, Ying Rong, Liegang Liu); Department of Nutrition, Harvard School of Public Health, Boston, Massachusetts (Frank B. Hu); and Department of Epidemiology, Harvard School of Public Health, Boston, Massachusetts (Frank B. Hu).
This study was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health (grant DK58845 to F.B.H.); and the China National High Technology Research and Development Program (863 program, grant 2009AA022704 to L.L.).
Conflict of interest: none declared.
REFERENCES
- 1.Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol. 2011;8(4):228–236. doi: 10.1038/nrendo.2011.183. [DOI] [PubMed] [Google Scholar]
- 2.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414(6865):782–787. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 3.Whiting DR, Guariguata L, Weil C, et al. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 4.Gillies CL, Abrams KR, Lambert PC, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334(7588):299. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365(9467):1333–1346. doi: 10.1016/S0140-6736(05)61032-X. [DOI] [PubMed] [Google Scholar]
- 6.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–1257. doi: 10.2337/dc11-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buijsse B, Simmons RK, Griffin SJ, et al. Risk assessment tools for identifying individuals at risk of developing type 2 diabetes. Epidemiol Rev. 2011;33(1):46–62. doi: 10.1093/epirev/mxq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noble D, Mathur R, Dent T, et al. Risk models and scores for type 2 diabetes: systematic review. BMJ. 2011;343:d7163. doi: 10.1136/bmj.d7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manolio TA. Genomewide association studies and assessment of the risk of disease. N Engl J Med. 2010;363(2):166–176. doi: 10.1056/NEJMra0905980. [DOI] [PubMed] [Google Scholar]
- 10.Hindorff LA, MacArthur J, Morales J, et al. Bethesda, MD: National Human Genome Research Institute, National Institutes of Health; 2012. A catalog of published genome-wide association studies http://www.genome.gov/gwastudies. Accessed November 25, 2012. [Google Scholar]
- 11.Mihaescu R, Meigs J, Sijbrands E, et al. Genetic risk profiling for prediction of type 2 diabetes. PLoS Curr. 2011;3:RRN1208. doi: 10.1371/currents.RRN1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonetta L. Getting up close and personal with your genome. Cell. 2008;133(5):753–756. doi: 10.1016/j.cell.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Janssens AC, Moonesinghe R, Yang Q, et al. The impact of genotype frequencies on the clinical validity of genomic profiling for predicting common chronic diseases. Genet Med. 2007;9(8):528–535. doi: 10.1097/gim.0b013e31812eece0. [DOI] [PubMed] [Google Scholar]
- 14.Yang Q, Khoury MJ, Botto L, et al. Improving the prediction of complex diseases by testing for multiple disease-susceptibility genes. Am J Hum Genet. 2003;72(3):636–649. doi: 10.1086/367923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyssenko V, Jonsson A, Almgren P, et al. Clinical risk factors, DNA variants, and the development of type 2 diabetes. N Engl J Med. 2008;359(21):2220–2232. doi: 10.1056/NEJMoa0801869. [DOI] [PubMed] [Google Scholar]
- 16.Meigs JB, Shrader P, Sullivan LM, et al. Genotype score in addition to common risk factors for prediction of type 2 diabetes. N Engl J Med. 2008;359(21):2208–2219. doi: 10.1056/NEJMoa0804742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janssens AC, Gwinn M, Bradley LA, et al. A critical appraisal of the scientific basis of commercial genomic profiles used to assess health risks and personalize health interventions. Am J Hum Genet. 2008;82(3):593–599. doi: 10.1016/j.ajhg.2007.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuehn BM. Inconsistent results, inaccurate claims plague direct-to-consumer gene tests. JAMA. 2010;304(12):1313–1315. doi: 10.1001/jama.2010.1328. [DOI] [PubMed] [Google Scholar]
- 19.Abbasi A, Peelen LM, Corpeleijn E, et al. Prediction models for risk of developing type 2 diabetes: systematic literature search and independent external validation study. BMJ. 2012;345:e5900. doi: 10.1136/bmj.e5900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–172. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 21.Mihaescu R, van Zitteren M, van Hoek M, et al. Improvement of risk prediction by genomic profiling: reclassification measures versus the area under the receiver operating characteristic curve. Am J Epidemiol. 2010;172(3):353–361. doi: 10.1093/aje/kwq122. [DOI] [PubMed] [Google Scholar]
- 22.Janssens AC, Khoury MJ. Assessment of improved prediction beyond traditional risk factors: When does a difference make a difference? [editorial] Circ Cardiovasc Genet. 2010;3(1):3–5. doi: 10.1161/CIRCGENETICS.110.938092. [DOI] [PubMed] [Google Scholar]
- 23.Janssens AC, Gwinn M, Khoury MJ, et al. Does genetic testing really improve the prediction of future type 2 diabetes? [letter] PLoS Med. 2006;3(2):e114. doi: 10.1371/journal.pmed.0030114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jakobsdottir J, Gorin MB, Conley YP, et al. Interpretation of genetic association studies: Markers with replicated highly significant odds ratios may be poor classifiers. PLoS Genet. 2009;5(2):e1000337. doi: 10.1371/journal.pgen.1000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyssenko V, Almgren P, Anevski D, et al. Genetic prediction of future type 2 diabetes. PLoS Med. 2005;2(12):e345. doi: 10.1371/journal.pmed.0020345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mihaescu R, van Hoek M, Sijbrands EJ, et al. Evaluation of risk prediction updates from commercial genome-wide scans. Genet Med. 2009;11(8):588–594. doi: 10.1097/GIM.0b013e3181b13a4f. [DOI] [PubMed] [Google Scholar]
- 27.de Miguel-Yanes JM, Shrader P, Pencina MJ, et al. Genetic risk reclassification for type 2 diabetes by age below or above 50 years using 40 type 2 diabetes risk single nucleotide polymorphisms. Diabetes Care. 2011;34(1):121–125. doi: 10.2337/dc10-1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Hoek M, Dehghan A, Witteman JC, et al. Predicting type 2 diabetes based on polymorphisms from genome-wide association studies: a population-based study. Diabetes. 2008;57(11):3122–3128. doi: 10.2337/db08-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruchat SM, Vohl MC, Weisnagel SJ, et al. Combining genetic markers and clinical risk factors improves the risk assessment of impaired glucose metabolism. Ann Med. 2010;42(3):196–206. doi: 10.3109/07853890903559716. [DOI] [PubMed] [Google Scholar]
- 30.Janssens AC, Ioannidis JP, van Duijn CM, et al. Strengthening the reporting of genetic risk prediction studies: the GRIPS statement. Ann Intern Med. 2011;154(6):421–425. doi: 10.7326/0003-4819-154-6-201103150-00008. [DOI] [PubMed] [Google Scholar]
- 31.Weedon MN, McCarthy MI, Hitman G, et al. Combining information from common type 2 diabetes risk polymorphisms improves disease prediction. PLoS Med. 2006;3(10):e374. doi: 10.1371/journal.pmed.0030374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lango H, Palmer CN, Morris AD, et al. Assessing the combined impact of 18 common genetic variants of modest effect sizes on type 2 diabetes risk. Diabetes. 2008;57(11):3129–3135. doi: 10.2337/db08-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vaxillaire M, Veslot J, Dina C, et al. Impact of common type 2 diabetes risk polymorphisms in the DESIR prospective study. Diabetes. 2008;57(1):244–254. doi: 10.2337/db07-0615. [DOI] [PubMed] [Google Scholar]
- 34.Cornelis MC, Qi L, Zhang C, et al. Joint effects of common genetic variants on the risk for type 2 diabetes in U.S. men and women of European ancestry. Ann Intern Med. 2009;150(8):541–550. doi: 10.7326/0003-4819-150-8-200904210-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu C, Zhang R, Wang C, et al. PPARG, KCNJ11, CDKAL1, CDKN2A-CDKN2B, IDE-KIF11-HHEX, IGF2BP2 and SLC30A8 are associated with type 2 diabetes in a Chinese population. PLoS One. 2009;4(10):e7643. doi: 10.1371/journal.pone.0007643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin X, Song K, Lim N, et al. Risk prediction of prevalent diabetes in a Swiss population using a weighted genetic score—the CoLaus Study. Diabetologia. 2009;52(4):600–608. doi: 10.1007/s00125-008-1254-y. [DOI] [PubMed] [Google Scholar]
- 37.Schulze MB, Weikert C, Pischon T, et al. Use of multiple metabolic and genetic markers to improve the prediction of type 2 diabetes: the EPIC-Potsdam Study. Diabetes Care. 2009;32(11):2116–2119. doi: 10.2337/dc09-0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sparso T, Grarup N, Andreasen C, et al. Combined analysis of 19 common validated type 2 diabetes susceptibility gene variants shows moderate discriminative value and no evidence of gene-gene interaction. Diabetologia. 2009;52(7):1308–1314. doi: 10.1007/s00125-009-1362-3. [DOI] [PubMed] [Google Scholar]
- 39.Qi Q, Li H, Wu Y, et al. Combined effects of 17 common genetic variants on type 2 diabetes risk in a Han Chinese population. Diabetologia. 2010;53(10):2163–2166. doi: 10.1007/s00125-010-1826-5. [DOI] [PubMed] [Google Scholar]
- 40.Talmud PJ, Hingorani AD, Cooper JA, et al. Utility of genetic and non-genetic risk factors in prediction of type 2 diabetes: Whitehall II prospective cohort study. BMJ. 2010;340:b4838. doi: 10.1136/bmj.b4838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang J, Stancakova A, Kuusisto J, et al. Identification of undiagnosed type 2 diabetic individuals by the Finnish Diabetes Risk Score and biochemical and genetic markers: a population-based study of 7232 Finnish men. J Clin Endocrinol Metab. 2010;95(8):3858–3862. doi: 10.1210/jc.2010-0012. [DOI] [PubMed] [Google Scholar]
- 42.Janipalli CS, Kumar MV, Vinay DG, et al. Analysis of 32 common susceptibility genetic variants and their combined effect in predicting risk of type 2 diabetes and related traits in Indians. Diabet Med. 2012;29(1):121–127. doi: 10.1111/j.1464-5491.2011.03438.x. [DOI] [PubMed] [Google Scholar]
- 43.Cauchi S, Meyre D, Durand E, et al. Post genome-wide association studies of novel genes associated with type 2 diabetes show gene-gene interaction and high predictive value. PLoS One. 2008;3(5):e2031. doi: 10.1371/journal.pone.0002031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marquezine GF, Pereira AC, Sousa AG, et al. TCF7L2 variant genotypes and type 2 diabetes risk in Brazil: significant association, but not a significant tool for risk stratification in the general population. BMC Med Genet. 2008;9:106. doi: 10.1186/1471-2350-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miyake K, Yang W, Hara K, et al. Construction of a prediction model for type 2 diabetes mellitus in the Japanese population based on 11 genes with strong evidence of the association. J Hum Genet. 2009;54(4):236–241. doi: 10.1038/jhg.2009.17. [DOI] [PubMed] [Google Scholar]
- 46.Fontaine-Bisson B, Renstrom F, Rolandsson O, et al. Evaluating the discriminative power of multi-trait genetic risk scores for type 2 diabetes in a northern Swedish population. Diabetologia. 2010;53(10):2155–2162. doi: 10.1007/s00125-010-1792-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu M, Bi Y, Xu Y, et al. Combined effects of 19 common variations on type 2 diabetes in Chinese: results from two community-based studies. PLoS One. 2010;5(11):e14022. doi: 10.1371/journal.pone.0014022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hivert MF, Jablonski KA, Perreault L, et al. Updated genetic score based on 34 confirmed type 2 diabetes loci is associated with diabetes incidence and regression to normoglycemia in the diabetes prevention program. Diabetes. 2011;60(4):1340–1348. doi: 10.2337/db10-1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cauchi S, Ezzidi I, El Achhab Y, et al. European genetic variants associated with type 2 diabetes in North African Arabs. Diabetes Metab. 2012;38(4):316–323. doi: 10.1016/j.diabet.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Tzoulaki I, Liberopoulos G, Ioannidis JP. Use of reclassification for assessment of improved prediction: an empirical evaluation. Int J Epidemiol. 2011;40(4):1094–1105. doi: 10.1093/ije/dyr013. [DOI] [PubMed] [Google Scholar]
- 51.Zeggini E, Scott LJ, Saxena R, et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet. 2008;40(5):638–645. doi: 10.1038/ng.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Voight BF, Scott LJ, Steinthorsdottir V, et al. Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nat Genet. 2010;42(7):579–589. doi: 10.1038/ng.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saxena R, Elbers CC, Guo Y, et al. Large-scale gene-centric meta-analysis across 39 studies identifies type 2 diabetes loci. Am J Hum Genet. 2012;90(3):410–425. doi: 10.1016/j.ajhg.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cho YS, Chen CH, Hu C, et al. Meta-analysis of genome-wide association studies identifies eight new loci for type 2 diabetes in East Asians. Nat Genet. 2011;44(1):67–72. doi: 10.1038/ng.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Collins GS, Mallett S, Omar O, et al. Developing risk prediction models for type 2 diabetes: a systematic review of methodology and reporting. BMC Med. 2011;9:103. doi: 10.1186/1741-7015-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu S, Song Y. Building genetic scores to predict risk of complex diseases in humans: Is it possible? [commentary] Diabetes. 2010;59(11):2729–2731. doi: 10.2337/db10-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Janssens AC, Gwinn M, Valdez R, et al. Predictive genetic testing for type 2 diabetes. BMJ. 2006;333(7567):509–510. doi: 10.1136/bmj.38953.598947.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vassy JL, Dasmahapatra P, Meigs JB, et al. Genotype prediction of adult type 2 diabetes from adolescence in a multiracial population. Pediatrics. 2012;130(5):e1235–e1242. doi: 10.1542/peds.2012-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vassy JL, Durant NH, Kabagambe EK, et al. A genotype risk score predicts type 2 diabetes from young adulthood: the CARDIA Study. Diabetologia. 2012;55(10):2604–2612. doi: 10.1007/s00125-012-2637-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Janssens AC, Aulchenko YS, Elefante S, et al. Predictive testing for complex diseases using multiple genes: Fact or fiction? Genet Med. 2006;8(7):395–400. doi: 10.1097/01.gim.0000229689.18263.f4. [DOI] [PubMed] [Google Scholar]
- 61.Manolio TA, Collins FS, Cox NJ, et al. Finding the missing heritability of complex diseases. Nature. 2009;461(7265):747–753. doi: 10.1038/nature08494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Evans JP, Berg JS. Next-generation DNA sequencing, regulation, and the limits of paternalism: the next challenge. JAMA. 2011;306(21):2376–2377. doi: 10.1001/jama.2011.1788. [DOI] [PubMed] [Google Scholar]
- 63.Bonnefond A, Clement N, Fawcett K, et al. Rare MTNR1B variants impairing melatonin receptor 1B function contribute to type 2 diabetes. Nat Genet. 2012;44(3):297–301. doi: 10.1038/ng.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu C, Walsh KM, Dewan AT, et al. Disease risk prediction with rare and common variants. BMC Proc. 2011;5(9 suppl):61S. doi: 10.1186/1753-6561-5-S9-S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stahl EA, Wegmann D, Trynka G, et al. Bayesian inference analyses of the polygenic architecture of rheumatoid arthritis. Nat Genet. 2012;44(5):483–489. doi: 10.1038/ng.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li S, Zhao JH, Luan J, et al. Genetic predisposition to obesity leads to increased risk of type 2 diabetes. Diabetologia. 2011;54(4):776–782. doi: 10.1007/s00125-011-2044-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grant RW, O'Brien KE, Waxler JL, et al. Personalized genetic risk counseling to motivate diabetes prevention: a randomized trial. Diabetes Care. 2013;36(1):13–19. doi: 10.2337/dc12-0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bloss CS, Schork NJ, Topol EJ. Effect of direct-to-consumer genomewide profiling to assess disease risk. N Engl J Med. 2011;364(6):524–534. doi: 10.1056/NEJMoa1011893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grant RW, Meigs JB, Florez JC, et al. Design of a randomized trial of diabetes genetic risk testing to motivate behavior change: the Genetic Counseling/Lifestyle Change (GC/LC) Study for Diabetes Prevention. Clin Trials. 2011;8(5):609–615. doi: 10.1177/1740774511414159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cho AH, Killeya-Jones LA, O'Daniel JM, et al. Effect of genetic testing for risk of type 2 diabetes mellitus on health behaviors and outcomes: study rationale, development and design. BMC Health Serv Res. 2012;12:16. doi: 10.1186/1472-6963-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hlatky MA, Greenland P, Arnett DK, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119(17):2408–2416. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Demler OV, Pencina MJ, D'Agostino RB., Sr Misuse of DeLong test to compare AUCs for nested models. Stat Med. 2012;31(23):2577–2587. doi: 10.1002/sim.5328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vickers AJ, Cronin AM, Begg CB. One statistical test is sufficient for assessing new predictive markers. BMC Med Res Methodol. 2011;11:13. doi: 10.1186/1471-2288-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seshan VE, Gonen M, Begg CB. Comparing ROC curves derived from regression models. Stat Med. 2013;32(9):1483–1493. doi: 10.1002/sim.5648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–845. [PubMed] [Google Scholar]
- 76.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115(7):928–935. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 77.Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–138. doi: 10.1097/EDE.0b013e3181c30fb2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kerr KF, McClelland RL, Brown ER, et al. Evaluating the incremental value of new biomarkers with integrated discrimination improvement. Am J Epidemiol. 2011;174(3):364–374. doi: 10.1093/aje/kwr086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pencina MJ, D'Agostino RB, Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30(1):11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–574. doi: 10.1177/0272989X06295361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Frazer KA, Murray SS, Schork NJ, et al. Human genetic variation and its contribution to complex traits. Nat Rev Genet. 2009;10(4):241–251. doi: 10.1038/nrg2554. [DOI] [PubMed] [Google Scholar]
- 82.Redon R, Ishikawa S, Fitch KR, et al. Global variation in copy number in the human genome. Nature. 2006;444(7118):444–454. doi: 10.1038/nature05329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Craddock N, Hurles ME, Cardin N, et al. Genome-wide association study of CNVs in 16,000 cases of eight common diseases and 3,000 shared controls. Nature. 2010;464(7289):713–720. doi: 10.1038/nature08979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Qi L, Cornelis MC, Zhang C, et al. Genetic predisposition, Western dietary pattern, and the risk of type 2 diabetes in men. Am J Clin Nutr. 2009;89(5):1453–1458. doi: 10.3945/ajcn.2008.27249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Florez JC, Jablonski KA, Bayley N, et al. TCF7L2 polymorphisms and progression to diabetes in the Diabetes Prevention Program. N Engl J Med. 2006;355(3):241–250. doi: 10.1056/NEJMoa062418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Aschard H, Chen J, Cornelis MC, et al. Inclusion of gene-gene and gene-environment interactions unlikely to dramatically improve risk prediction for complex diseases. Am J Hum Genet. 2012;90(6):962–972. doi: 10.1016/j.ajhg.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.