Abstract
Objectives
Ureteral reimplantation (UR) is the gold standard for the surgical treatment of vesicoureteral reflux (VUR) but few studies have documented its long-term results. We reviewed late cystography (LC) results following successful UR.
Methods
We performed a retrospective chart review of all children with primary VUR who underwent successful open UR (grade 0 VUR into the reimplanted ureter(s) on initial cystogram) at our institution from January 1990 – December 2002. We identified successful UR patients who underwent LC ≥ 1 year after UR and reviewed the results for the presence of recurrent VUR into the reimplanted ureter(s).
Results
794 patients underwent successful open UR for primary VUR, of whom 60 (7.6%) had a subsequent LC. Preoperative VUR grade was ≤II in 20 (34.5%), ≥III in 38 (65.5%). Median age at UR was 3.5 years (IQR: 1.3–6.2 years); 51 (85%) were female. UR was intravesical in 45 (75%) and bilateral in 19 (32%). LC was performed at a median of 38.7 months after UR (IQR: 19.6–66.1 months). Indication for LC was febrile UTI in 16 (27%), non-febrile UTI’s in 15 (25%), follow-up of contralateral VUR in 16 (27%) and other clinical indications in 13 (21%). The recurrence rate was 0%; of the 79 reimplanted ureters, 100% (95% CI: 95.4–100) had no VUR (grade 0).
Conclusions
Among children who underwent successful open UR for primary VUR, there was no VUR recurrence on extended follow-up. This suggests that the late durability of open anti-reflux surgery is excellent.
Keywords: Vesico-ureteral reflux, Surgical Procedures, Operative, Follow-up Studies, Urinary Tract Infections
INTRODUCTION
Open ureteral reimplantation (UR) remains the gold standard for surgical treatment of primary vesicoureteral reflux (VUR) and the technical success rates based on initial postoperative cystography are high. Indeed, UR is considered so reliable that some groups have suggested that the post-operative cystogram is unnecessary.[1, 2] Clinicians typically assume that, once VUR is corrected surgically, it does not recur. However, this assumption is not supported by strong evidence, as there are few data on the long-term durability of the anti-reflux effect of UR.[3, 4] Most long-term studies of outcomes after UR have used ultrasound to follow renal status, and it is clear that ultrasound is neither sensitive nor specific for VUR.[5] The question of UR durability is particularly relevant in light of recent concerns regarding long-term durability of endoscopic treatments for VUR, specifically with dextranomer/hyaluronic acid.[6] The purpose of this study was to assess the long-term durability of VUR resolution by reviewing the results of late cystography (LC) among children with a history of successful open UR for primary VUR.
MATERIALS AND METHODS
Patient Population
We performed a retrospective review of all patients with primary VUR (all grades) who underwent successful open UR at our institution between January 1990 and December 2002. Data were collected from electronic records and departmental and hospital paper charts after approval by the Institutional Review Board. We included all patients undergoing surgery for primary VUR. Intravesical and extravesical UR procedures were included as were procedures requiring ureteral tapering. We excluded all patients with secondary VUR (VUR associated with neurogenic bladder or spina bifida, posterior urethral valves, bladder exstrophy, renal transplant, prune belly syndrome, or ureterocele) as well as repeat procedures, laparoscopic or robotic procedures, and endoscopic procedures.
Patients with a successful UR met the following criteria: 1) a routine post-operative cystogram (radionuclide cystogram (RNC) or cyclic voiding cystourethrogram (VCUG)) performed within six months of UR, and 2) absence of VUR (grade 0) into the reimplanted ureter(s) on the postoperative cystogram. Among the group with successful reimplantation, we then identified patients who underwent at least one additional cystogram (RNC or VCUG) at least 12 months after successful UR; such cystograms were defined as a late cystogram (LC). Cystography was performed by the radiology department using standard imaging protocols. Cyclic studies were routinely performed in most cases. Filling was performed under gravity pressures (35–40 cm water) until voiding in non-toilet trained infants and children, and until sensation of fullness or urgency in toilet trained children. We reviewed and recorded these patients’ demographics, clinical presentation, preoperative VUR grade, procedure variables, additional surgical procedures, incidence of postoperative urinary tract infection (UTI), indication for LC, and LC results. Among patients with multiple preoperative cystograms, preoperative VUR was graded based on the final preoperative cystogram. VUR was graded using a five-point scale based on the International Reflux Study (IRS).[7] In cases where the final cystogram was an RNC (typically graded using a three-point scale) we converted these scores to the 5-point IRS scale using the following method: RNC grade 1 = IRS Grade I, RNC grade 2 = IRS grade 2 and RNC grade 3 = IRS grade 4. [8] In cases of bilateral VUR, the patient was categorized based on the higher grade side. Procedure variables included intravesical vs. extravesical approach, need for ureteral tailoring (tapered or excised), and reimplantation of single system vs. duplicated system (classified as duplicated if at least one duplicated system reimplanted).
To assess whether the group that underwent LC after successful UR differed from patients who did not undergo LC, we compared key parameters of these groups. We performed bivariate tests of association of patient/procedure characteristics between the LC and non-LC groups using Fisher’s exact test or Wilcoxon rank-sum test as appropriate based on data characteristics.
The primary outcome was the presence or absence of recurrent VUR into the reimplanted ureter(s) on LC. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC). All tests were two-sided and p-values of 0.05 or less were considered significant.
RESULTS
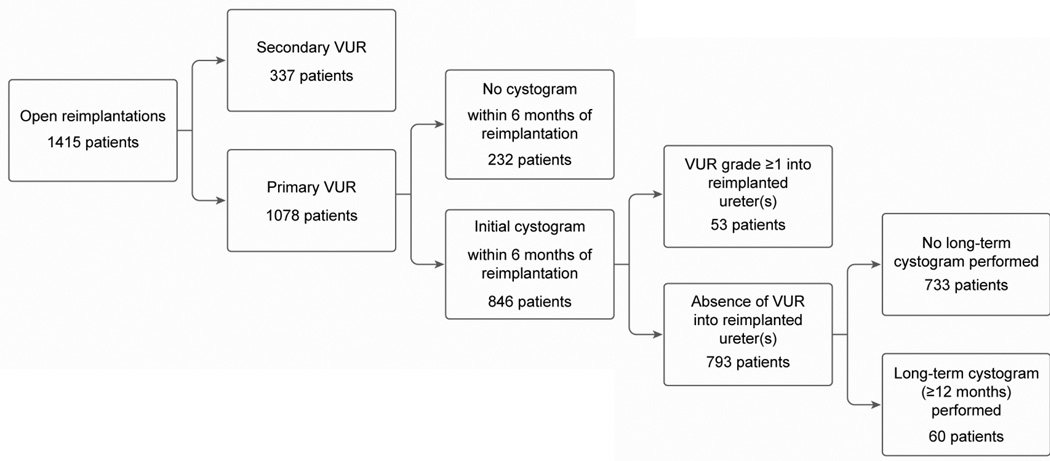
The selection process for identifying patients for inclusion in the study is shown in Figure 1. We identified 1415 patients who underwent open UR for VUR during the study period. 33-patients with secondary VUR were excluded. Of the remaining 1078 patients with primary reflux, 846 had an initial postoperative cystogram performed within six months of UR, and of these 793 (93.7%) had no VUR (grade 0) into the reimplanted ureter(s). Median follow-up was 2.9 years (range: 0–6.9 years). Many patients continued to be seen for many years after UR; 29.6% had follow-up > 5 years. 71.7% of the patients had more than 1 year of follow-up; 56.3% had more than 2 years; 49.1% had more than 3 years; 37.9% had more than 4 years.
Figure 1.
Patient selection
Of the 793 patients with a successful UR, 60 (7.6%) had a subsequent long-term cystogram performed at least 12 months after UR. A total of 79 ureters were reimplanted in these 60 patients. LC was performed at a median of 38.7 months (3.2 years) after UR. UTI (febrile or non-febrile) was the most common indication for LC (Table 2). Although patients with recurrent UTI were generally treated with behavioral modification and treatment of dysfunctional elimination symptoms, those with persistent, recurrent UTI’s were imaged with cystography. Late cystography results showed that the late recurrence rate of VUR was 0%. Of the 79 reimplanted ureters, 100% (95% CI: 95.4–100) had no VUR (grade 0) at a median of 38.7 months (IQR: 19.6–66.1 months). No patient required subsequent repeat UR for correction of recurrent VUR in a previously reimplanted ureter. Notably, eleven patients including nine girls were post-pubertal at the time of the final postoperative cystogram, suggesting that even with pubertal changes in anatomy UR maintains its durability.
Table 2.
Indications for long-term cystography
| Indication | N (%) |
|---|---|
| Febrile UTI | 16 (27%) |
| Recurrent non-febrile UTI | 15 (25%) |
| Follow-up of new, contralateral VUR on initial postoperative cystogram | 16 (27%) |
| Hydronephrosis | 5 (8%) |
| Voiding dysfunction/incontinence | 4 (7%) |
| Routine follow-up | 3 (5%) |
| Microhematuria | 1 (1%) |
Overall, the LC and non-LC patients were similar. There were no differences between LC and non-LC groups in race/ethnicity, initial presentation, preoperative VUR grade, laterality, surgical technique, duplex vs. single system, or need for ureteral tailoring (Table 1). As would be expected, follow-up was longer in the LC group than the non-LC group (median 65.7 v. 37.3 months, p<0.0001), and the LC group had higher rate of postoperative febrile UTI (35.0% vs. 4.5%, p<0.0001). Furthermore, non-LC patients were somewhat older (4.8 vs. 3.5 years, p=0.02), and had a larger percent of bilateral procedures (57.7% among non-LC vs. 31.7% among LC, p=.0002). The LC group tended to have more females, although the difference was not significant (85.0% vs. 73.7%, p=0.06).
Table 1.
Patient and Procedure Characteristics
| N (%) | |
|---|---|
| Patients undergoing LTC | 60 |
| Median age at surgery (years) | |
| 3.5 [1.3–6.2] | |
| Gender | |
| Male | 9 (15%) |
| Female | 51 (85%) |
| Race/Ethnicity | |
| White/Caucasian | 38 (90%) |
| Hispanic | 4 (10%) |
| Missing | 18 |
| Initial presentation | |
| UTI | 54 (90%) |
| Prenatal hydronephrosis | 4 (6%) |
| Sibling screen | 1 (2%) |
| Incidental diagnosis | 1 (2%) |
| Preoperative VUR grade (by patient) | |
| Grade ≤II | 20 (34.5%) |
| Grade ≥ III | 38 (65.5%) |
| Missing | 2 |
| Laterality | |
| Unilateral | 41 (68%) |
| Bilateral | 19 (32%) |
| Surgical technique | |
| Extravesical | 15 (25.1%) |
| Glenn-Anderson | 2 (3.3%) |
| Politano-Leadbetter | 17 (28.3%) |
| Cohen cross-trigonal | 26 (43.3%) |
| System reimplanted (by patient) | |
| Unilateral Single | 39 (65%) |
| Bilateral Single | 16 (27%) |
| Unilateral Duplex | 2 (3%) |
| Bilateral Duplex | 1 (2%) |
| One Duplex, One Single | 2 (3%) |
| Ureteral tapering (by ureter) | |
| No | 73 (92%) |
| Yes | 6 (8%) |
| Postoperative UTI | |
| No | 39 (65%) |
| Yes | 21 (35%) |
Several patients in the LC group had unusual or atypical clinical courses. One patient underwent cystogram at 9.4 months after successful UR due to incidental note of mild-moderate pelviectasis on routine renal ultrasound. Although this patient was noted to have recurrent grade IV VUR on the 9.4 month cystogram, they remained asymptomatic, no interventions were made, and the final follow-up LC performed at 74.1 months after UR showed no evidence of VUR. There were no other cases of transient recurrent VUR into the reimplanted ureter in this cohort.
Another patient underwent an apparently uncomplicated right single-system reimplantation with successful correction of VUR on initial cystogram. However, a subsequent screening ultrasound documented right upper pole hydronephrosis and it was determined that she had an unrecognized duplex system with a newly obstructed upper pole ureter. LC at 48 months after UR showed no recurrent VUR, but she subsequently required a right uretero-ureterostomy to correct the obstruction. Several patients underwent LC for persistent hydronephrosis, mild in all cases, and in all cases there was no recurrent VUR.
20 patients underwent LC because they had new contralateral VUR detected on initial postoperative cystogram after unilateral UR. This new contralateral VUR resolved on LC in 16 of these (80%). The remaining four patients with persistent new contralateral VUR on LC (all grade II) remained asymptomatic at a median of 66.8 months (IQR; 54.3–103.6 months) after reimplantation. Three additional patients whose initial postoperative cystogram was negative subsequently underwent LC for febrile UTI (2) or recurrent non-febrile UTI (1), and were incidentally found to have new, contralateral VUR on LC (grade II in two patients and grade IV in one patient). All three underwent reimplantation of the contralateral ureter at a median of 44.2 months after initial UR.
COMMENT
Despite recent advances in minimally invasive and endoscopic surgery, open UR remains a widely-utilized treatment for VUR in children.[9] Advances in anesthetic and analgesic management have made this an increasingly well-tolerated procedure that in some cases may be performed on an outpatient basis.[10, 11] Although the benefits of UR with respect to decreasing incidence of pyelonephritis are generally accepted, there are few data showing that the antireflux effect of UR (from which the reduction in UTI risk presumably arises) is itself durable in the long-term.[12] This question is of increased significance now that alternatives to open UR, such as endoscopic injection of dextranomer/hyaluronic acid (DHA) copolymer, are available, inviting comparisons of outcomes and effectiveness between techniques.[13]
The primary goal of this study was to document the long-term durability of UR results. This is a difficult outcome to assess because, for the most part, children whose VUR has resolved on the initial postoperative cystogram do not undergo subsequent cystography in the absence of clinical indications. Indeed, in our cohort most late cystograms were performed for specific clinical indications (most commonly UTI), and not simply for screening purposes. While it would be ideal for all patients to have late cystographic follow-up, this is simply not a realistic goal in the context of current pediatric urologic practice. Nonetheless, we found that even in this select cohort, who would seem to be at high risk for VUR recurrence based on clinical status, the anti-reflux effect of UR for primary VUR was durable. No patients had persistent recurrent VUR into a ureter that had been successfully reimplanted. The patient with reflux on the 9.4 month postoperative cystogram represents an atypical case. The apparent waxing and waning of reflux in some patients may be related to temporal changes in pelvic floor coordination and patient elimination habits.
There are very few studies describing the long-term anatomic durability of UR. Hegi and colleagues reported findings on routine VCUG one year after UR for VUR or primary obstructive megaureter.[14] Among patients with primary VUR, none had recurrent VUR. This sample differed from ours in that Hegi et al. performed 12-month cystography as part of a screening protocol, whereas most of our patients had cystography performed for clinical indications. Follow-up times in our study were considerably longer, as well. However, both studies support the hypothesis that the anti-reflux effect is durable beyond the first few months after surgery. Falkensammer et al. reported on 126 patients who had their initial postoperative VCUG twelve months after UR.[4] At 12 months, persistent VUR was detected in 6 patients (4.8%); since surgical success was not assessed with an early (<6 months) post-operative cystogram, this study could not differentiate between surgical failures and VUR recurrences. However, it seems likely that these patients simply reflect the widely-accepted ~5% failure rate of UR among patients with primary VUR.
Although open UR is highly effective and appears durable, endoscopic treatment for VUR has become increasingly popular over the past decade.[9] The late outcomes of endoscopic treatment, as with many relatively new products and procedures, are not well-documented. However, several recent studies have raised concerns about the durability of dextranomer/hyaluronic acid (DHA) injection for the treatment of primary VUR. The Swedish reflux study randomized children with VUR to endoscopic treatment with DHA, observation, or antimicrobial prophylaxis.[15] Among those patients who had resolution of VUR (either no VUR, or improved Grade I-II VUR) after 1 or 2 DHA injections, 20% (13/66) had recurrence of dilating VUR on cystography at 2 years. Similarly, Lee and colleagues performed a VCUG at 1 year in all patients who were initially cured of VUR by endoscopic injection.[6] Of these, 26% had recurrent VUR at 1 year; this meant that the overall 1-year success rate, accounting for both initial and late failures, was 46.1%. Early studies of DHA suggested that VUR might recur after successful endoscopic treatment. Lackgren et al. followed a large cohort of early DHA patients, and performed at late cystogram in a subset of these (2–5 years after treatment).[16] Of 45 ureters with no VUR on the initial post-treatment cystogram (3–12 months after injection), recurrent VUR of any grade developed in 6 (13%), and dilating reflux recurred in 2 (4%) on late cystography.[16] A study presented at the International Conference on Vesicoureteral Reflux in Children in Goteborg, Sweden in 2009 (but not yet published) found that recurrent VUR was diagnosed 21% of renal units between 6 months and 3 years after endoscopic treatment.[17]
Late VUR recurrence after endoscopic treatment is not limited to DHA. In a study of 42 patients who had successful endoscopic treatment with polytetrafluoroethylene, Yucel et al. observed recurrence of VUR in 27% or patients at a median of 2 years after treatment.[18] This suggests that the phenomenon of recurrence after successful endoscopic treatment may have less to do with the specific bulking agent used, and more to do with the mechanics of the implant with respect to changing anatomic relationships and tissue characteristics.
The current study, as well as most of those cited, focuses on anatomic correction of VUR as the primary clinical outcome. Clearly, however, other clinical outcomes are of equal or greater importance with respect the long-term health of the child, including recurrent UTI, renal scarring, and health-related quality of life. It has been pointed out that anatomic outcomes are not always the best indicator of “success” after treatment for VUR.[19] Nonetheless, it seems reasonable to expect that anti-reflux surgery should result in a predictably durable anatomic resolution of VUR, given the considerable time, expense, and morbidity that goes into any surgical procedure (whether open or endoscopic). The findings of the current study are therefore reassuring in that they document that the resolution of VUR that results from successful open UR is highly durable, even over a period of many years.
The results of this study should be interpreted in light of its limitations, including those inherent in the retrospective record review methodology. These data arise from a single-institution experience over a lengthy period of time. Therefore, the findings may not be generalizable to other settings, institutions, surgeons, or to contemporary practice. However, the cases in this series were performed by fourteen surgeons, and although medicine has changed since the 1990’s, we believe that the basic techniques for UR have not. Our sample in the study is highly selected, including only those patients whose VUR resolution was confirmed on a post-operative cystogram, and who had a subsequent LC. It is possible that this introduces bias if, in fact, patients who did not get initial cystography, or LC, differ systematically from those who did. However, we believe that patients who do not get initial or late cystograms after UR are, if anything, likely to be more healthy, and at lower risk for recurrence, than those who do undergo such imaging tests (since those in whom studies are obtained are more likely to have had clinical events (e.g. UTI) that would be indications for imaging). Despite this likely bias towards a higher risk for VUR recurrence in the LC group, no recurrence was noted. We compared the patients that did undergo LC with those who did not undergo LC, and found few differences in patient or procedure characteristics between groups. Therefore, it is reasonable to presume that the LC group is representative of all children undergoing UR at our institution. Nonetheless, we cannot be certain of this and it is possible that, had all patients undergone LC on a systematic basis, we would have observed a higher rate of VUR recurrence.
CONCLUSIONS
Among children who underwent successful open UR for primary VUR, there was no recurrence of VUR on extended follow-up. These findings suggest that the late durability of open anti-reflux surgery is excellent.
Acknowledgments
SUPPORT/FINANCIAL DISCLOSURES
Dr. Hubert is supported by grant number T32-HS19485 from the Agency for Healthcare Research and Quality (AHRQ)/American Recovery and Reinvestment Act (ARRA). Dr. Kokorowski is supported by grant number T32-DK60442 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Dr. Nelson is supported by grant number K23-DK088943 from the NIDDK.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Barrieras D, Lapointe S, Reddy PP, et al. Are postoperative studies justified after extravescial ureteral reimplantation? J Urol. 2000;164(3 Pt 2):1064–1066. doi: 10.1097/00005392-200009020-00035. [DOI] [PubMed] [Google Scholar]
- 2.Bomalski MD, Ritchey ML, Bloom DA. What imaging studies are necessary to determine outcome after ureteroneocystostomy? J Urol. 1997;158:1226–1228. doi: 10.1097/00005392-199709000-00144. [DOI] [PubMed] [Google Scholar]
- 3.Kennelly MJ, Bloom DA, Ritchey ML, et al. Outcome analysis of bilateral Cohen cross-trigonal ureteroneocystostomy. Urology. 1995;46(3):393–395. doi: 10.1016/S0090-4295(99)80226-X. [DOI] [PubMed] [Google Scholar]
- 4.Falkensammer ML, Gobet R, Stauffer UG, et al. To Cohen and Forget? Evaluation of Postoperative Imaging Studies after Transtrigonal Ureteric Reimplantation for Vesicoureteral Reflux in Children. Urol Int. 2007;81:218–221. doi: 10.1159/000144065. [DOI] [PubMed] [Google Scholar]
- 5.Blane CE, DiPietro MA, Zerin JM, et al. Renal ultrasonography is not a reliable screening examination for vesicoureteral reflux. J Urol. 1993;150:752–755. doi: 10.1016/s0022-5347(17)35605-7. [DOI] [PubMed] [Google Scholar]
- 6.Lee EK, Gatti JM, Demarco RT. Long-term followup of dextranomer/hyaluronic acid injection for vesicoureteral reflux: late failure warrants continued followup. J Urol. 2009;181(4):1869–1874. doi: 10.1016/j.juro.2008.12.005. discussion 1874-5. [DOI] [PubMed] [Google Scholar]
- 7.Medical versus surgical treatment of primary vesicoureteral reflux: report of the International Reflux Study Committee. Pediatrics. 1981;67:392–400. [PubMed] [Google Scholar]
- 8.Willi U, Treves S. Radionuclide voiding cystography. Urol Radiol. 1983;5(3):161–173. 175. doi: 10.1007/BF02926792. [DOI] [PubMed] [Google Scholar]
- 9.Routh JC, Nelson CP, Graham DA, et al. Variation in surgical management of vesicoureteral reflux: influence of hospital and patient factors. Pediatrics. 2010;125(3):e446–e451. doi: 10.1542/peds.2009-1237. [DOI] [PubMed] [Google Scholar]
- 10.Park JM, Houck CS, Sethna NF. Ketorolac suppresses postoperative bladder spasms after pediatric ureteral reimplantation. Anesth Analg. 2000;91(1):11–15. doi: 10.1097/00000539-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Wicher C, Hadley D, Ludlow D. 250 consecutive unilateral extravesical ureteral reimplantations in an outpatient setting. J Urol. 2010;184(1):311–314. doi: 10.1016/j.juro.2010.01.056. [DOI] [PubMed] [Google Scholar]
- 12.Weiss R, Tamminen-Möbius T, Koskimies O. Characteristics at entry of children with severe primary vesicoureteral reflux recruited for a multicenter, international therapeutic trial comparing medical and surgical management. The International Reflux Study in Children. J Urol. 1992;148(5 Pt 2):1644–1649. doi: 10.1016/s0022-5347(17)36993-8. [DOI] [PubMed] [Google Scholar]
- 13.Elmore JM, Kirsch AJ, Heiss EA. Incidence of urinary tract infections in children after successful ureteral reimplantation versus endoscopic dextranomer/hyaluronic acid implantation. J Urol. 2008;179(6):2364–2367. doi: 10.1016/j.juro.2008.01.149. discussion 2367-8. [DOI] [PubMed] [Google Scholar]
- 14.Hegi LP, Geffken BP, Hanimann B, et al. Is there a benefit from routine voiding cystourethrography after ureteroneocystostomy? Eur J Pediatr Surg. 2007;17:344–347. doi: 10.1055/s-2007-965421. [DOI] [PubMed] [Google Scholar]
- 15.Holmdahl G, Brandström P, Läckgren G. The Swedish reflux trial in children: II. Vesicoureteral reflux outcome. J Urol. 2010;184(1):280–285. doi: 10.1016/j.juro.2010.01.059. [DOI] [PubMed] [Google Scholar]
- 16.Läckgren G, Wahlin N, Sköldenberg E, et al. Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol. 2001;166(5):1887–1892. doi: 10.1016/s0022-5347(05)65713-8. [DOI] [PubMed] [Google Scholar]
- 17.Chertin B, Kocherov S, Chertin L. Endoscopic bulking materials for the treatment of vesicoureteral reflux: a review of our 20 years of experience and review of the literature. Adv Urol. 2011;2011:309626. doi: 10.1155/2011/309626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yücel S, Tarcan T, Simsek F. Durability of a single successful endoscopic polytetrafluoroethylene injection for primary vesicoureteral reflux: 14-year followup results. J Urol. 2007;178(1):265–268. doi: 10.1016/j.juro.2007.03.060. discussion 268. [DOI] [PubMed] [Google Scholar]
- 19.Kaye JD, Srinivasan AK, Delaney C. Clinical and radiographic results of endoscopic injection for vesicoureteral reflux: Defining measures of success. J Pediatr Urol. 2011 doi: 10.1016/j.jpurol.2011.02.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]