Abstract
Kidney stones are very common and unfortunately do not spare the pregnant population. Anatomical and pathophysiological changes occur in the pregnant female that alter the risk for development of nephrolithiasis. Acute renal colic during pregnancy is associated with significant potential risks to both mother and fetus. Diagnosis is often challenging because good imaging options without radiation use are limited. Management of diagnosed nephrolithiasis is unique in the pregnant population and requires multi-disciplinary care. Herein, we review the metabolic alterations during pregnancy that may promote kidney stone formation, the complications associated with acute renal colic in the pregnant state, and our proposed diagnostic and management algorithms when dealing with this clinical scenario.
Keywords: kidney stones, nephrolithiasis, pregnancy
Introduction
Kidney stones afflict 10% of the population during their lifetime and over the past two decades this statistic has risen, thought to be caused by diet, climate changes, and a concurrent rise in comorbidities like diabetes and obesity.1–5 This increase in stone events has been quite dramatic for women and incidence is now close to equal between sexes, while previously it was far more common in men.3,6 While this rise has not necessarily been observed in pregnant females, this population is still affected by kidney stones, which occur in 1 in 200–1,500 pregnancies.7–13
The top cause for nonobstetric hospital admission during pregnancy is acute urolithiasis.14,15 Anatomical and pathophysiological changes occur in the pregnant female to alter the urinary environment (Table 1). Elevated progesterone and mechanical compression cause urinary stasis. Increased glomerular filtration rate, calcium supplementation, and increased circulating Vitamin D levels lead to elevated urinary pH and hypercalciuria.16–27 Uric acid, sodium, and oxalate, all lithogenic factors, also all have increased urinary excretion during pregnancy.8,19,20 These changes promote calcium phosphate stone formation. Up to 75% of pregnant patients with kidney stones have calcium phosphate stones in contradistinction to the general population where calcium oxalate is the most common stone type.11,14,28–33
Table 1.
Changes in pregnancy affecting stone risk
| Stone promotion (mechanism) | Stone inhibition (mechanism) |
|---|---|
| Urinary stasis (mechanical compression, progesterone) | Hypercitraturia (increased GFR) |
| Lithogenic factors | |
| Hypercalciuria (increased GFR, increased vitamin D) | Increased excretion: magnesium, glycosaminoglycans, uromodulin, and nephrocalcin (increased GFR) |
| Elevated urine pH | |
| Increased excretion: uric acid, sodium, and oxalate (increased GFR) |
Abbreviation: GFR, glomerular filtration rate.
Renal colic has been associated with multiple potential risks to mother and fetus including preterm labor, preterm delivery, preterm premature rupture of membranes, recurrent pregnancy losses, and mild preeclampsia, but data are somewhat mixed.10,12,33–38 These potential complications make accurate diagnosis crucial.
Renal ultrasound is considered first-line because the gold standard for diagnosis in the non-pregnant state, computed tomography (CT), involves radiation use, which is avoided during pregnancy because of teratogenic risks and risk of childhood malignancy. Ultrasound has a poor sensitivity and one group only identified stones 60% of the time during pregnancy.39–41 Transvaginal ultrasound can be helpful to evaluate distal ureter and distinguish obstruction from physiological hydronephrosis of pregnancy which can occur in up to 90% of patients.23–25,42 When results are equivocal, half Fourier single shot turbo spin echo (HASTE) magnetic resonance urography (MRU) without contrast is safe, effective, comparable to CT accuracy, and now considered second-line during pregnancy when available.43–46 It visualizes the stone as a filling defect, evaluates secondary findings of obstruction, and also gives information about non-urologic organ systems. Low dose CT (fetal radiation dose 4 mGy versus 25 mGy) is highly sensitive and specific, increasing in popularity, but still is last-line given its use of radiation.47–49 Plain radiography, intravenous urogram, nuclear medicine scans, and magnetic resonance imaging with contrast can be done but all have limitations and risks associated with them during pregnancy.33,50–56 The need and importance for more accurate diagnosis is elucidated by White et al where they report a negative ureteroscopy rate of 14%.57 This means that 1 in 7 patients who went to the operating room for assumed nephrolithiasis did not have a stone.
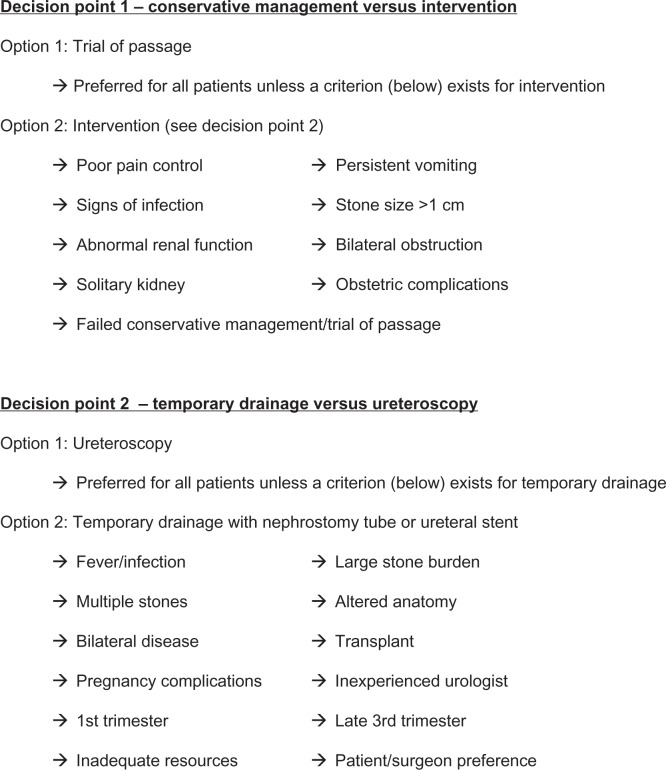
Once the diagnosis of a stone is made during pregnancy, multi-disciplinary decision-making is required given the potential complications that can occur as discussed above (Figure 1). Urology and obstetrics should be in active communication with the patient outlining a plan with close follow-up and monitoring.
Figure 1.
Algorithm for acute kidney stone event during pregnancy.
First choice, similar to the general population, is always conservative management and trial of passage with hydration and analgesia. Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually avoided during pregnancy and narcotics are generally required. Requirements for this pathway are a solitary stone less than 1 cm, absence of infection, adequate oral pain control, and ability to tolerate food and liquid. This will be successful 70%–80% of time and 50% of those without spontaneous passage during pregnancy will pass their stones after delivery.12,33,36,38,58–60 While some have found spontaneous passage rate to be higher during pregnancy, thought to be due to physiological ureteral dilation, others believe the rate to be biased because of higher subject numbers for trial of passage, given surgeon reluctance to operate.11 Additionally, the rate may be overestimated because of misdiagnosis and poor follow-up; a Mayo clinic series had 23% of patients misdiagnosed and only 48% passage rate.61 The patient should be followed closely with physical exam, blood work, and ultrasound.
Medical expulsive therapy can be used as an adjunct to trial of passage. Alpha blockers are Category B drugs; they have not been studied in humans but have been shown to be safe in animal studies and are often used during pregnancy. Gestational hypertension and preterm labor are often treated with calcium channel blockers and these are also thought to be safe.62
Similar to the general population, some patients are not candidates for trial of passage and some fail conservative management. If fever, infection, or obstetric complications are present then intervention is indicated. Renal insufficiency and anatomical considerations such as solitary kidney or bilateral obstruction also require intervention. More minor indications for further management are refractory pain, intractable nausea and vomiting, stone greater than 1 cm, or non-diagnostic imaging.63
If a procedure is needed, experienced anesthesiologists, neonatologists, radiologists, urologists, and obstetricians should be involved. Cardiopulmonary changes during pregnancy make a pregnant woman’s management more complex.17 Temporary drainage versus definitive treatment of the stone is the next decision point in the management algorithm. Only over the last decade has definitive management become an accepted option.17,64 Risks of surgery were previously thought to be too high and treatment too complex. However, over the last two decades endourology has expanded, and may be one of the most progressive fields within urology. Ureteroscopy is far more sophisticated with miniaturization, advanced visualization, improved deflection, and an immense armamentarium of instruments, baskets, and lasers available. Obstetrics care has also advanced and has improved monitoring technology. Shock wave lithotripsy and percutaneous nephrolithotomy are still contraindicated during pregnancy for a multitude of reasons.65–67
Multiple factors are considered when electing temporary drainage versus ureteroscopy. Infection is an absolute contraindication for ureteroscopy and urgent temporary drainage is required when fever is present. Experienced medical teams (surgeon, anesthesiologist, obstetrician, neonatologist), are required if stone treatment is elected. Adequate resources must be available as well (ie, laser, obstetric monitoring, etc).64 Other reasons to potentially choose temporary drainage include large stone burden, complex anatomy, bilateral stone disease, obstetric complications, presentation in the first trimester, or presentation near full term.64 Patient and surgeon preference are also important.
While once the preferred and only acceptable method of management, there are many disadvantages to temporary drainage. First and foremost, it is temporary and requires definitive management at a later date post-partum, often during a time that is hectic and focused on a new child. Additionally, multiple procedures may be required during pregnancy, as the physiological variations induce rapid encrustation and exchanges are required every 4–6 weeks.68–70 This is expensive and each exchange incurs a risk on the pregnancy. Temporary drainage is often not tolerated well. Tubes and stents dislodge, migrate, are uncomfortable, and become colonized with bacteria increasing risk for urinary infection; patients are often miserable. The advantages of temporary drainage are that it can be done very quickly, with minimal anesthesia and no radiation exposure. Stent versus nephrostomy tube is always the subject of a debate. With regards to infection, study has shown them to be equivalent in outcome.71 In general though, stent is preferred because it does not require an external tube which can be quite burdensome to the patient. Stents do cause lower urinary tract symptoms, whereas nephrostomy tubes do not. If a large stone burden is present, nephrostomy tubes can assist with future access for definitive treatment.17,72
Because of the above-mentioned disadvantages of temporary drainage, definitive treatment with ureteroscopy is often considered and is now accepted as a reasonable and sometimes ideal option (Table 2).17,64 Patient selection is critical and guided by the contraindications mentioned above. Ureteroscopy can be done under spinal or general anesthesia. Radiation is not required and good outcomes can be achieved using ultrasound alone.73 An experienced radiologist and/or technician can be involved in the operating room. In 2009 Semins et al performed a systematic review and meta-analysis of 14 reports of ureteroscopy during pregnancy in over 100 patients.74 Complication rates between the general female population and pregnancy were similar and ureteroscopy was deemed to be safe and effective in the properly selected patient. It is important to remember that these reports are by experienced endourologists with excellent available resources. Over the past 5 years, more groups have published case series reporting acceptable safety profiles and good efficacy for ureteroscopy during pregnancy.28,75–80 Johnson et al also stresses that a multi-disciplinary approach is critical as they did have 2 patients go into pre-term labor, 1 of which delivered early.79 Experience, patient selection, and available resources are vital to a good outcome.
Table 2.
Complication rates of ureteroscopy during pregnancy
| Literature | Patients (N) | Complications N (%) |
|---|---|---|
| Semins et al74 | 108 | 9 (8.3) – ureteral perforation (1), premature contractions (1), postoperative pain (2), UTI (5) |
| Meta-analysis | ||
| 14 studies | ||
| Travassos et al76 | 9 | 0 (0) |
| Rana et al77 | 19 | 0 (0) |
| Polat et al75 | 8 | 0 (0) |
| Ross et al28 | 21 | 0 (0) |
| Bozkurt et al78 | 41 | 15 (36) – ureteral injury (4), sepsis (1), UTI (4), pain (6) |
| Johnson et al79 | 46 | 2 (4) – preterm labor (1), preterm delivery (2) |
| Hoscan et al80 | 34 | 12 (35) – uterine contraction (1), UTI (3), other minor (8) |
Abbreviation: UTI, urinary tract infection.
In conclusion, urolithiasis during pregnancy is more complex than when it occurs in the general population and diagnosis can sometimes be quite challenging. Expectant management is first-line, but if not an option or if it fails, then both temporary drainage and definitive treatment are acceptable secondary management alternatives. Patient and surgeon preference, along with clinical variables and available resources, guide decision-making.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pearle MS, Calhoun EA, Curhan GC, Urologic Diseases of America Project Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848–857. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 2.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817–1823. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 3.Odvina CV, Pak CYC. Medical evaluation of stone disease. In: Stoller ML, Meng MV, editors. Urinary Stone Disease: A The Practical Guide to Medical and Surgical Management (Current Clinical Urology) Totowa, NJ: Humana Press Inc; 2007. pp. 259–268. [Google Scholar]
- 4.Asplin JR. Obesity and urolithiasis. Adv Chronic Kidney Dis. 2009;16:11–20. doi: 10.1053/j.ackd.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Scales CD, Jr, Smith AC, Hanley JM, Saigal CS, Urologic Diseases in America Project Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scales CD, Jr, Curtis LH, Norris RD, et al. Changing gender prevalence of stone disease. J Urol. 2007;177:979–982. doi: 10.1016/j.juro.2006.10.069. [DOI] [PubMed] [Google Scholar]
- 7.Dudley A, Riley J, Semins MJ. Nephrolithiasis and Pregnancy: Has the Incidence Been Rising? American Urological Association; 2013. p. 68. Abstract #. [DOI] [PubMed] [Google Scholar]
- 8.Maikranz P, Coe FL, Parks JH, Lindheimer MD. Nephrolithiasis and gestation. Bailleres Clin Obstet Gynaecol. 1987;1:909–919. doi: 10.1016/s0950-3552(87)80041-x. [DOI] [PubMed] [Google Scholar]
- 9.Maikranz P, Lindheimer MD, Coe F. Nephrolithiasis in pregnancy. Bailleres Clin Obstet Gynaecol. 1994;8:375–386. doi: 10.1016/s0950-3552(05)80326-8. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg E, Sergienko R, Abu-Ghanem S, et al. Nephrolithiasis during pregnancy: characteristics, complications, and pregnancy outcome. World J Urol. 2011;29:743–747. doi: 10.1007/s00345-011-0719-7. [DOI] [PubMed] [Google Scholar]
- 11.Meria P, Hadjadj H, Jungers P, et al. Stone Formation and Pregnancy: Pathophysiological Insights Gained From Morphoconstitutional Stone Analysis. J Urol. 2010;183:1412–1418. doi: 10.1016/j.juro.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Drago JR, Rohner TJ, Jr, Chez RA. Management of urinary calculi in pregnancy. Urology. 1982;20:578–581. doi: 10.1016/0090-4295(82)90302-8. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez PN, Klein AS. Management of urolithiasis during pregnancy. Surg Gynecol Obstet. 1988;166:103–106. [PubMed] [Google Scholar]
- 14.Horowitz E, Schmidt JD. Renal calculi in pregnancy. Clin Obstet Gynecol. 1985;28:324–338. [PubMed] [Google Scholar]
- 15.Strong DW, Murchison RJ, Lynch DF. The management of ureteral calculi during pregnancy. Surg Gynecol Obstet. 1978;146:604–608. [PubMed] [Google Scholar]
- 16.Resim S, Ekerbicer HC, Kiran G, et al. Are changes in urinary parameters during pregnancy clinically significant? Urol Res. 2006;34:244–248. doi: 10.1007/s00240-006-0051-7. [DOI] [PubMed] [Google Scholar]
- 17.Srirangam SJ, Hickerton B, Van Cleynenbreugel B. Management of urinary calculi in pregnancy: a review. J Endourol. 2008;22:867–875. doi: 10.1089/end.2008.0086. [DOI] [PubMed] [Google Scholar]
- 18.Ritchie LD, Fung EB, Halloran BP, et al. A longitudinal study of calcium homeostasis during human pregnancy and lactation and after resumption of menses. Am J Clin Nutr. 1998;67:693–701. doi: 10.1093/ajcn/67.4.693. [DOI] [PubMed] [Google Scholar]
- 19.Maikranz P, Holley JL, Parks JH, et al. Gestational hypercalciuria causes pathological urine calcium oxalate supersaturations. Kidney Int. 1989;36:108–113. doi: 10.1038/ki.1989.168. [DOI] [PubMed] [Google Scholar]
- 20.Smith C, Kristensen C, Davis M, et al. An evaluation of the physicochemical risk for renal stone disease during pregnancy. Clin Nephrol. 2001;55:205–211. [PubMed] [Google Scholar]
- 21.Conrad KP, Lindheimer MD. Renal and cardiovascular alterations. In: Lindheimer MD, Roberts JM, Cunningham FG, editors. Chesley’s Hypertensive Disorders in Pregnancy. 2nd ed. Stamford, CT: Appleton and Lange; 1999. pp. 263–326. [Google Scholar]
- 22.Gabert HA, Miller JM., Jr Renal disease in pregnancy. Obstet Gynecol Surv. 1985;40:449–461. doi: 10.1097/00006254-198507000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Peake SL, Roxburg HB, Langlois SL. Ultrasonic assessment of hydronephrosis of pregnancy. Radiology. 1983;146:167–170. doi: 10.1148/radiology.146.1.6849041. [DOI] [PubMed] [Google Scholar]
- 24.Marchant DJ. Effects of pregnancy and progestational agents on the urinary tract. Am J Obstet Gynecol. 1972;112:487–501. doi: 10.1016/0002-9378(72)90309-2. [DOI] [PubMed] [Google Scholar]
- 25.Gorton E, Whitfield H. Renal calculi in pregnancy. Br J Urol. 1997;80:4–9. [PubMed] [Google Scholar]
- 26.Buppasiri P, Lumbiganon P, Thinkhamrop J, et al. Calcium supplementation (other than for preventing or treating hypertension) for improving pregnancy and infant outcomes. Cochrane Database Syst Rev. 2011;10:CD007079. doi: 10.1002/14651858.CD007079.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Imdad A, Bhutta ZA. Effect of calcium supplementation during pregnancy on maternal, fetal and birth outcomes. Paediatr Perinat Epidemiol. 2012;(Suppl 1):138–152. doi: 10.1111/j.1365-3016.2012.01274.x. [DOI] [PubMed] [Google Scholar]
- 28.Ross AE, Handa S, Lingeman JE, et al. Kidney stones during pregnancy: an investigation into stone composition. Urol Res. 2008;36:99–102. doi: 10.1007/s00240-008-0138-4. [DOI] [PubMed] [Google Scholar]
- 29.Costa-Bauzá A, Ramis M, Montesinos V, et al. Type of renal calculi: variation with age and sex. World J Urol. 2007;25:415–421. doi: 10.1007/s00345-007-0177-4. [DOI] [PubMed] [Google Scholar]
- 30.Gault MH, Chafe L. Relationship of frequency, age, sex, stone weight and composition in 15,624 stones: comparison of resutls for 1980 to 1983 and 1995 to 1998. J Urol. 2000;164:302–307. [PubMed] [Google Scholar]
- 31.Parks JH, Worcester EM, Coe FL, et al. Clinical implications of abundant calcium phosphate in routinely analyzed kidney stones. Kidney Int. 2004;66:777–785. doi: 10.1111/j.1523-1755.2004.00803.x. [DOI] [PubMed] [Google Scholar]
- 32.Cass AS, Smith CS, Gleich P. Management of urinary calculi in pregnancy. Urology. 1986;28:370–372. doi: 10.1016/0090-4295(86)90063-4. [DOI] [PubMed] [Google Scholar]
- 33.Stothers L, Lee LM. Renal colic in pregnancy. J Urol. 1992;148:1383. doi: 10.1016/s0022-5347(17)36917-3. [DOI] [PubMed] [Google Scholar]
- 34.Banhidy F, Acs N, Puho EH, et al. Maternal kidney stones during pregnancy and adverse birth outcomes, particularly congenital abnormalities in the offspring. Arch Gynecol Obstet. 2007;275:481–487. doi: 10.1007/s00404-006-0277-1. [DOI] [PubMed] [Google Scholar]
- 35.Cormier CM, Canzoneri BJ, Lewis DF, et al. Urolithiasis in pregnancy: Current diagnosis, treatment, and pregnancy complications. Obstet Gynecol Surv. 2006;61:733–741. doi: 10.1097/01.ogx.0000243773.05916.7a. [DOI] [PubMed] [Google Scholar]
- 36.Lewis DF, Robichaux AG, Jaekle RK, et al. Urolithiasis in pregnancy. Diagnosis, management and pregnancy outcome. J Reprod Med. 2003;48:28–32. [PubMed] [Google Scholar]
- 37.Hendricks SK, Ross SO, Krieger JN. An algorithm or diagnosis and therapy of management and complications or urolithiasis during pregnancy. Surg Gynecol Obstet. 1991;172:49. [PubMed] [Google Scholar]
- 38.Swartz MA, Lydon-Rochelle MT, Simon D, et al. Admission for nephrolithiasis in pregnancy and risk of adverse birth outcomes. Obstet Gynecol. 2007;109:1099. doi: 10.1097/01.AOG.0000259941.90919.c0. [DOI] [PubMed] [Google Scholar]
- 39.Swanson SK, Hieilman RL, Eversman WG. Urinary tract stones in pregnancy. Surg Clin North Am. 1995;75:123. doi: 10.1016/s0039-6109(16)46539-4. [DOI] [PubMed] [Google Scholar]
- 40.Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics. 2007;27:1705. doi: 10.1148/rg.276075002. [DOI] [PubMed] [Google Scholar]
- 41.Butler EL, Cox SM, Eberts EG, et al. Symptomatic nephrolithiasis complicating pregnancy. Obstet Gynecol. 2000;96:753. doi: 10.1016/s0029-7844(00)01017-6. [DOI] [PubMed] [Google Scholar]
- 42.Laing FC, Benson CB, DiSalvo DN, et al. Distal ureteral calculi: Detection with vaginal US. Radiology. 1994;192:545. doi: 10.1148/radiology.192.2.8029429. [DOI] [PubMed] [Google Scholar]
- 43.Mullins JK, Semins MJ, Hyams ES, et al. Half Fourier Single Shot Turbo Spin Echo Magnetic Resonance Urography for the Evaluation of Suspected Renal Colic in Pregnancy. Urology. In press. [DOI] [PubMed]
- 44.Grenier N, Pariente JL, Trillaud H, et al. Dilatation of the collecting system during pregnancy: physiologic vs obstructive dilatation. Eur Radiol. 2000;10:271. doi: 10.1007/s003300050043. [DOI] [PubMed] [Google Scholar]
- 45.Regan F, Bohlman ME, Khazan R, et al. MR urography using HASTE imaging in the assessment of ureteric obstruction. AJR Am J Roentgenol. 1996;167:1115. doi: 10.2214/ajr.167.5.8911161. [DOI] [PubMed] [Google Scholar]
- 46.Regan F, Kuszyk B, Bohlman ME, et al. Acute ureteric calculus obstruction: unenhanced spiral CT versus HASTE MR urography and abdominal radiograph. Br J Radiol. 2005;78:506. doi: 10.1259/bjr/22314006. [DOI] [PubMed] [Google Scholar]
- 47.Hamm M, Knopfe E, Wartenberg S, et al. Low dose unenhanced helical computerized tomography for the evaluation of acute flank pain. J Urol. 2002;167:1687. [PubMed] [Google Scholar]
- 48.White WM, Zite NB, Gash J, et al. Low-dose computed tomography for the evaluation of flank pain in the pregnant population. J Endourol. 2007;21:1255. doi: 10.1089/end.2007.0017. [DOI] [PubMed] [Google Scholar]
- 49.McCollough CH, Schueler BA, Atwell TD, et al. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007;27:909. doi: 10.1148/rg.274065149. [DOI] [PubMed] [Google Scholar]
- 50.Spencer JA, Tomlinson AJ, Weston MJ, et al. Early report: Comparison of breath-hold MR excretory urography, Doppler ultrasound and isotope renography in evaluation of symptomatic hydronephrosis of pregnancy. Clin Radiol. 2000:55. doi: 10.1053/crad.2000.0443. [DOI] [PubMed] [Google Scholar]
- 51.Spencer JA, Chahal R, Kelly A, et al. Evaluation of painful hydronephrosis in pregnancy: Magnetic resonance urographic patterns in physiological dilatiation versus calculous obstruction. 2004. p. 171. [DOI] [PubMed]
- 52.Roy C, Saussine C, Le Bras Y, et al. Assessment of painful ureterohydronephrosis during pregnancy by MR urography. Eur Radiol. 1996:6. doi: 10.1007/BF00180604. [DOI] [PubMed] [Google Scholar]
- 53.Voight R, Stoll W, Arndt J. The value of radio-isotope investigations of the urinary tract for the diagnosis of urinary tract calculi during pregnancy. (Ger) Geburtshilfe Frauenheilkd. 1980;40:863. doi: 10.1055/s-2008-1037230. [DOI] [PubMed] [Google Scholar]
- 54.Biyani CS, Joyce AD. Urolithiasis in pregnancy: II: management. BJU Int. 2002;89:819. doi: 10.1046/j.1464-410x.2002.02773.x. [DOI] [PubMed] [Google Scholar]
- 55.Webb JA, Thomsen HS, Morcos SK, et al. The use of idoinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol. 2005;15:1234. doi: 10.1007/s00330-004-2583-y. [DOI] [PubMed] [Google Scholar]
- 56.Irving SO, Burgess NA. Managing severe loin pain in pregnancy. BJOG. 2002;109:1025. doi: 10.1111/j.1471-0528.2002.01340.x. [DOI] [PubMed] [Google Scholar]
- 57.White WM, Johnson EB, Zite NB, et al. Predictive value of current imaging modalities for the detection of urolithiasis during pregnancy: a multicenter, longitudinal study. J Urol. 2013;189:931. doi: 10.1016/j.juro.2012.09.076. [DOI] [PubMed] [Google Scholar]
- 58.Parulkar BG, Hopkins TB, Wollin MR, et al. Renal colic during pregnancy: A case for conservative treatment. J Urol. 1998:159. doi: 10.1016/s0022-5347(01)63918-1. [DOI] [PubMed] [Google Scholar]
- 59.Harris RE, Dunnihoo DR. The incidence of urinary calculi in pregnancy. Am J Obstet Gynecol. 1967;99:237. doi: 10.1016/0002-9378(67)90325-0. [DOI] [PubMed] [Google Scholar]
- 60.Evans HJ, Wollin TA. The management of urinary calculi in pregnancy. Curr Opin Urol. 2001;11:379. doi: 10.1097/00042307-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Burgess KL, Gettman MT, Rangel LJ, et al. Diagnosis of urolithiasis and rate of spontaneous passage during pregnancy. J Urol. 2011;186:2280. doi: 10.1016/j.juro.2011.07.103. [DOI] [PubMed] [Google Scholar]
- 62.Weber-Schoendorfer C, Hannemann D, Meister R, et al. The safety of calcium channel blockers during pregnancy: a prospective, multicenter, observational study. Reprod Toxicol. 2008;26:24. doi: 10.1016/j.reprotox.2008.05.065. [DOI] [PubMed] [Google Scholar]
- 63.Lee SJ, Rho SK, Lee CH, et al. Management of Urinary Calculi in Pregnant Women. JKMS. 1997:12. doi: 10.3346/jkms.1997.12.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Semins MJ, Matlaga BR. Management of stone disease in pregnancy. Curr Opin Urol. 2010;20:174. doi: 10.1097/MOU.0b013e3283353a4b. [DOI] [PubMed] [Google Scholar]
- 65.Chaussy EG, Fuchs GJ. Current state and future developments of noninvasive treatment of urinary stones with ESWL. J Urol. 1989;141:782. doi: 10.1016/s0022-5347(17)41010-x. [DOI] [PubMed] [Google Scholar]
- 66.Smith DR, Graham JB, Prystowsky JB, et al. The effects of ultrasound-guided sockwaves during early pregnancy in Sprague-Dawley rats. J Urol. 1992;147:231. doi: 10.1016/s0022-5347(17)37203-8. [DOI] [PubMed] [Google Scholar]
- 67.Asgari MA, Safarinejad MR, Hosseini SY, et al. Extracorporeal shock wave lithotripsy of renal calculi during early pregnancy. BJU Int. 1999:84. doi: 10.1046/j.1464-410x.1999.00275.x. [DOI] [PubMed] [Google Scholar]
- 68.Jarrard DJ, Gerber GS, Lyon ES. Management of acute ureteral obstruction in pregnancy utilizing ultrasound guided placement of ureteral stents. Urology. 1993;42:263. doi: 10.1016/0090-4295(93)90614-g. [DOI] [PubMed] [Google Scholar]
- 69.Kavoussi LR, Albala DM, Basler JW, et al. Percutaneous management of uroltihiasis during pregnancy. J Urol. 1992;148:1069. doi: 10.1016/s0022-5347(17)36820-9. [DOI] [PubMed] [Google Scholar]
- 70.Khoo L, Anson K, Patel U. Success and short-term complication rates of percutaneous nephrostomy during pregnancy. J Vasc Interv Radiol. 2004;15:1469. doi: 10.1097/01.RVI.0000140639.57131.6D. [DOI] [PubMed] [Google Scholar]
- 71.Pearle MS, Pierce HL, Miller GL, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol. 1998;160:1260. [PubMed] [Google Scholar]
- 72.vanSonnenberg E, Casola G, Talner LB, Wittich GR, Varney RR, D’Agostino HB. Symptomatic Renal Obstruction or Urosepsis During Pregnancy: Treatment by Sonographically Guided Perctaneous Nephrostomy. Am J Roentgenol. 1992;158:91–94. doi: 10.2214/ajr.158.1.1727366. [DOI] [PubMed] [Google Scholar]
- 73.Deters LA, Belanger G, Shah O, et al. Ultrasound guided ureteroscopy in pregnancy. Clin Nephrol. 2013;79:118–123. doi: 10.5414/CN107654. [DOI] [PubMed] [Google Scholar]
- 74.Semins MJ, Trock BJ, Matlaga BR. The Safety of Ureteroscopy During Pregnancy: A Systematic Review and Meta-Analysis. J Urol. 2009;181:139–143. doi: 10.1016/j.juro.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 75.Polat F, Yesil S, Kirac M, et al. Treatment outcomes of semirigid ureterorenoscopy and intracorporeal lithotripsy in pregnant women with obstructive ureteral calculi. Urol Res. 2011;39:487–490. doi: 10.1007/s00240-011-0376-8. [DOI] [PubMed] [Google Scholar]
- 76.Travassos M, Amselem I, Filho NS, et al. Ureteroscopy in Pregnany Women for Ureteral Stone. J Endourol. 2009;23:405–407. doi: 10.1089/end.2008.0181.23.3. [DOI] [PubMed] [Google Scholar]
- 77.Rana AM, Aquil S, Khawaja AM. Semirigid ureteroscopy and pneumatic litotripsy as definitive management of obstructive ureteral calculi during pregnancy. Urology. 2009;73:964–967. doi: 10.1016/j.urology.2008.12.054. [DOI] [PubMed] [Google Scholar]
- 78.Bozkurt Y, Soylemez H, Atar M, et al. Effectiveness and safety of ureteroscopy in pregnant women: a comparative study. Urolithiasis. 2013;41:37–42. doi: 10.1007/s00240-012-0523-x. [DOI] [PubMed] [Google Scholar]
- 79.Johnson EB, Krambeck AE, White WM, et al. Obstetric complications of ureteroscopy during pregnancy. J Urol. 2012;188:151–154. doi: 10.1016/j.juro.2012.02.2566. [DOI] [PubMed] [Google Scholar]
- 80.Hoşcan MB, Ekinci M, Tunçkıran A, Oksay T, Özorak A, Özkardeş H. Management of symptomatic ureteral calculi complicating pregnancy. Urology. 2012;80:1011–1014. doi: 10.1016/j.urology.2012.04.039. [DOI] [PubMed] [Google Scholar]