Abstract
Background
Multiple types of substance use are associated with HIV risk behaviors, but relatively little research has examined the association between marijuana use and risky sexual activities in treatment-seeking polysubstance abuse patients.
Objectives
This study evaluated the relationship between marijuana use and sexual behaviors in 239 patients with cocaine, opioid, or alcohol use disorders who were initiating outpatient substance use treatment.
Methods
Participants completed the HIV Risk Behavior Scale and were classified into one of three groups based on their marijuana use histories: never (n = 66), past but not current use (n = 124), or current use (n = 49).
Results
Compared to never marijuana users, current and former marijuana users had a greater likelihood of having more than 50 lifetime sexual partners [odds ratio (OR) and 95% confidence interval (CI) = 3.9 (1.0 – 15.7) and 5.2 (1.6 – 17.3), respectively]. Former marijuana users had increased risk of low frequency condom use with casual partners relative to never users [OR (95% CI) = 2.9 (1.1 – 7.6)]. Moreover, current marijuana users were more likely than never users to have had more than two recent sexual partners [OR (95% CI) = 8.1 (1.94 – 33.44)].
Conclusion
Treatment-seeking polysubstance abusers with current or past marijuana use histories may be at greater risk of HIV infection than their counterparts who do not use marijuana. These data underscore the importance of increasing awareness about the potential association between marijuana use and increased high risk sexual behavior among polysubstance abusing patients.
Keywords: marijuana, HIV risk behaviors, sexual behaviors
Marijuana is the most commonly used illicit drug in the United States. Up to 42% of adults report lifetime marijuana usage (1) and 7% indicate recent use (2). Marijuana is also considered a “gateway drug;” many individuals initiate marijuana use when young, go on to experiment with other drugs, and eventually develop substance use disorders (3). The majority of patients seeking substance abuse treatment have a current or past history of marijuana use (4–8).
Substance use is associated with HIV risk behaviors. Heroin is predominantly used intravenously, and needle sharing is a primary form of HIV risk (9–11). Further, cocaine use is associated with high numbers of sex partners (12–15).
The relationship between use of particular drugs and specific risk behaviors, however, is complex. For example, compared to non-crack users, crack users are more likely to have multiple partners and exchange sex for money/drugs, but they are not more likely to engage in unprotected sex (13). In fact, an unexpected positive association between crack and condom use is reported among homeless youth (16).
A large literature exists on associations of alcohol use and risky sexual activities (17–21). Drinking impairs decision making and leads to “alcohol myopia,” in which immediate pleasures are considered foremost while long-term consequences are minimized. This process may make it more likely that one engages in sexual activities or fails to use protection when drinking. Marijuana, similarly to alcohol, impairs judgment, and therefore, its use may also be associated with increases in risky behavior (22, 23).
The relation between sexual behaviors and marijuana use has been evaluated primarily in adolescents and young adults. Marijuana use is associated with global risky sexual behavior in high school (24) and college students (25). In 14–18 year-old adolescents on probation, greater marijuana use was inversely correlated with frequency of condom use (26). Adolescent detainees’ frequencies of marijuana use were related to unprotected sex (27), but no relationship between marijuana use and unprotected sex was found in primarily African American and Latino incarcerated male adolescents(28). Nevertheless, marijuana use before incarceration was associated with higher numbers of sexual partners in that sample (28).
Studies employing event-level analyses to examine how marijuana use may relate to sexual behaviors on a day-by-day basis have yielded inconsistent results. For example, using cannabis on particular days was not associated with risky sexual behaviors occurring on the same day in some samples of youth (29,30), but it was in others (27,31).
One explanation for the discrepant findings across studies may relate to use of other substances. Most studies evaluating marijuana use and risky sexual behaviors did not assess other drug use. Given that marijuana users often use other drugs (32–34), some of which may be independently related to sexual activities (13,14,35), other substance use may have impacted the findings.
In sum, the relationship between marijuana use and risky sexual behaviors is not well delineated, and most studies have been limited to young and non-treatment seeking marijuana users. Few studies have examined the association between marijuana use and risky sexual behavior in clinical samples of adults, and this was the purpose of the current investigation. We assessed this association in a general sample of polysubstance using patients initiating treatment so that results would be generalizable to the larger population of treatment-seeking substance users. Because marijuana is not used intravenously, we hypothesized that marijuana use would not be related to IV risk behaviors, but that it would be associated with sexual risk behaviors, even after controlling for other types of illicit drug use. Given its predominately IV use in treatment-seeking populations, we expected that opioid dependence would be related to IV drug use risk behaviors. We also anticipated that cocaine dependence would be related to sexual risk behaviors, consistent with prior studies (12–15), but that marijuana use may be independently associated with sexual risk behaviors.
Methods
Participants (N = 239) were initiating intensive outpatient substance use treatment at one of two community-based clinics from 2005–2009. The study in which participants were involved (36) was designed to evaluate the efficacy of a group-based contingency management approach in reducing cocaine, opioid and alcohol use. Thus, individuals with only a marijuana use disorder were not included, although many patients with cocaine, opioid or alcohol use disorders had a current or past history of marijuana use, as outlined below.
Patients were eligible for the study (36) if they were 18 years or older and met past-year Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) diagnosis of alcohol, cocaine, or opioid dependence (37). Participants could have one or more of these substance use disorders, along with other drug use problems (although diagnoses of other drug use disorders, including marijuana, were not assessed formally). Exclusion criteria were non-English speaking, and uncontrolled psychotic symptoms or suicidality. Being in recovery for pathological gambling was also an exclusion due to potential similarities between the experimental treatment and gambling (but see 38,39).
Procedures
Institutional Review Boards approved study procedures. After obtaining written informed consent, research assistants administered demographic questionnaires and modules adapted from the Structured Clinical Interview for DSM-IV for assessing cocaine, opioid, and alcohol use disorders (40).
Participants also completed the HIV Risk Behavior Scale (HRBS) (41), which has six questions on risky injection drug use and five on sexual behaviors. An example of a sexual risk behavior question was “How many people, including any regular partners, casual acquaintances and clients, have you had sex with?” Additional items related to frequencies of condom use with casual and regular partners, trading sex for drugs/money, and anal sex (see [41] for specific items). Responses are coded using a 6-point scale (0–5), with higher values indicating higher risk. Scores on each subscale are derived by summing the ordinal value of all responses. Thus, subscale scores range from 0–30 for intravenous drug risk and from 0–25 for sexual behaviors.
The psychometric properties of the HRBS are well defined, including internal reliabilities of 0.82 and 0.77 for lifetime and recent versions (42), and test-retest reliabilities of 0.90 (42) and 0.86 (41) for the respective versions. High agreement between substance abusers and their sexual partners is also observed (41). The structure of the scale is consistent with the component analysis, and confirms that it measures two types of HIV transmission (41,42).
Research assistants also administered the Addiction Severity Index (ASI) (43). It collected information regarding lifetime and current patterns of substance use, including marijuana. The Drug section of the ASI is reliable and valid in assessing substance use problems (44,45).
Data analyses
Patients were classified into one of three groups based upon marijuana use status: never users, past users, or current users. “Never” users were defined as those who reported no lifetime or past 30 day use of marijuana on the ASI. Past users were classified as those who reported lifetime use of marijuana but no use in the past 30 days, and current users were those who self reported use in the past 30 days. Chi-square and analysis of variance evaluated differences across these three marijuana use groups with respect to demographics and substance use characteristics.
The primary analysis used a single multivariate analysis of variance to assess the association between marijuana use and HIV risk behaviors. Lifetime and past 3-month HRBS drug and sexual behavior subscale scores were the dependent variables, entered simultaneously into the analyses. Independent variables were marijuana use status and demographic and baseline characteristics that differed significantly between the marijuana use groups: cocaine dependence, opioid dependence, age, and education. Age and education were entered as covariates and the remainder as fixed variables; all variables were entered simultaneously into the model. Analyses were also conducted with gender included as a fixed factor, but gender was not associated with risk behavior scores, ps > .30. Because gender did not differ by marijuana use status and was unrelated to risk behaviors, only results from the primary analysis described above are reported.
Subsequent analyses examined predictors of specific types of risk behaviors, when overall analyses were significant. Distributions of responses to HRBS items could not be normalized, and some likert response categories were very infrequently endorsed, so response options were dichotomized to lower versus higher risk, with the higher risk category including the riskiest response option(s) that were reported by at least 10% of the sample. For example, if “never” using condoms was reported by only three persons"never” and “rarely” using condoms were combined as the high-risk response. Logistic regressions investigated associations of marijuana use status with specific high-risk sexual behaviors. Presence or absence of the high-risk behavior was the dependent variable, and independent variables included marijuana use status, cocaine dependence, opioid dependence, age, and education. The first three were categorical and the later two continuous variables, with all entered simultaneously in the model. Odds ratios (OR) and 95% confidence intervals (CI) are presented for significant predictors of high-risk behaviors. Analyses were performed on SPSS for Windows (v 15), with 2-tailed alphas < 0.05 significant.
Results
Table 1 shows baseline characteristics of patients classified into groups based on self-reported marijuana use. Past and current marijuana users were younger than those reporting no marijuana use, and former users were less educated than never users. All participants had an alcohol, cocaine or opioid use disorder as a study inclusion criterion, but those who reported current or past marijuana use were more likely to be dependent on cocaine and opioids than their non-marijuana using counterparts. Rates of alcohol dependence in the full sample, however, were similar across marijuana use groups.
Table 1.
Demographic and baseline characteristics
| Variable | Never marijuana users |
Former marijuana users |
Current marijuana users |
Significance test value (df), p |
|---|---|---|---|---|
| n | 66 | 124 | 49 | |
| Clinic, % (n) | χ2 (2) = 3.58, .17 | |||
| A | 21.2 (14) | 25.8 (32) | 36.7 (18) | |
| B | 78.8 (52) | 74.2 (92) | 63.3 (31) | |
| Age | 43.3 ± 11.1a | 35.8 ± 10.8b | 34.7 ± 9.5b | F (2, 236) = 13.08, .000 |
| Male, % (n) | 51.5 (34) | 61.3 (76) | 53.1 (26) | χ2 (2) = 2.05, .36 |
| Married, % (n) | 13.6 (9) | 12.3 (15) | 12.2 (6) | χ2 (2) = 0.08, .96 |
| Years of education | 13.1 ± 2.4a | 12.2 ± 1.95b | 12.7 ± 1.7ab | F (2, 235) = 4.56, .01 |
| Income | $15,508 ± 23,956 | $12,318 ± 17,315 | $19,175 ± 23,310 | F (2, 234) = 1.08, .34 |
| Race/ethnicity, % (n) | χ2 (6) = 7.68, .26 | |||
| African American | 36.4 (24) | 25.8 (32) | 34.7 (17) | |
| European American | 51.5 (34) | 63.7 (79) | 44.9 (22) | |
| Hispanic American | 7.6 (5) | 8.1 (10) | 14.3 (7) | |
| Other | 4.5 (3) | 2.4 (3) | 6.1 (3) | |
| DSM-IV diagnoses, % (n) | ||||
| Alcohol dependence | 60.6 (40) | 54.0 (67) | 63.3 (31) | χ2 (2) = 1.53, .46 |
| Cocaine dependence | 50.0 (33)a | 68.5 (85)b | 73.5 (36)b | χ2 (2) = 8.66, .01 |
| Opioid dependence | 12.1 (8)a | 37.9 (47)b | 34.7 (17)b | χ2 (2) = 14.21, .001 |
| Past month marijuana use, days | 0.0 (0.0)a | 0.0 (0.0)a | 6.4 (7.4)b |
Kruskal Wallis (KW) χ 2 (2) = 234.10, .000 |
| Years regular marijuana use | 0.0 (0.0) | 8.6 (7.0) | 13.6 (9.1) | KW χ2 (2) = 150.43, .000 |
| Heterosexual, % (n) | 95.2 (60) | 88.5 (108) | 89.6 (43) | χ2 (2) = 2.26, .32 |
| Current legal problems,% (n) | 24.6 (16) | 25.8 (32) | 32.7 (16) | χ2 (2) = 1.07, .59 |
Values are means and standard deviations unless noted. Income was log transformed prior to analyses. Groups with different superscripts differ from one another in post-hoc tests.
In the multivariate analyses of variance predicting lifetime and past 3 month HRBS subscale scores, marijuana use status, opioid dependence, cocaine dependence, and age were all associated with subscale scores, F (6,452) = 2.34, p = .02, F (4,225) = 13.95, p < .001, F (4,225) = 3.10, p = .02, and F (4,225) = 3.64, p < .01, respectively. As expected, opioid dependence was the only variable associated with HRBS lifetime and past 3 month drug risk subscale scores, F (1,228) = 46.36 and 22.87, ps < .001; means (SE) of non-opioid dependent and opioid dependent patients, respectively, on the IV drug use subscale were 0.9 (0.5) and 6.9 (0.8) for the lifetime version and 0.1 (0.2) and 1.5 (0.3) for the past 3-month version. Cocaine dependence was associated with higher lifetime and past 3 month sexual subscale scores, F (1,228) = 8.20 and 7.02, ps < .01; means (SE) on the sexual subscale for non-cocaine dependent and cocaine dependent patients were 9.2 (0.5) and 10.8 (0.4) for lifetime and 2.9 (0.4) and 4.3 (0.3) for past 3-month versions, respectively. Age was positively related to lifetime, but not recent, sexual subscale scores, F (1,228) = 9.78, p < .01.
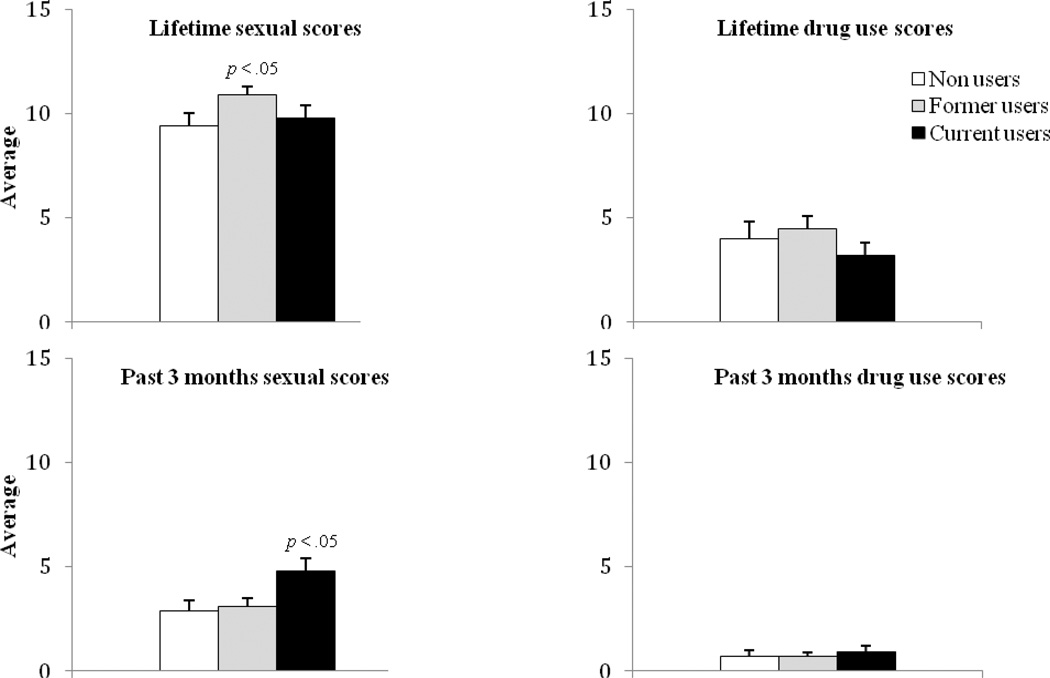
Marijuana use status was related to HRBS sexual risk behavior subscale scores, both over the lifetime and the past 3 months, F (2,228) = 2.97 and 4.03, ps < .05, respectively, even when other variables were included in these analyses. HRBS subscale scores, derived from the single multivariate analysis, are shown in Figure 1, based on marijuana status. Post-hoc tests revealed that former users scored significantly higher than never users on the lifetime HRBS sexual risk scale, and current users scored higher than never users on the past 3 months sexual subscale (ps < .05).
Figure 1.
Average subscale scores obtained in the lifetime and past 3- month of the HIV Risk Behavior Scales. Graphs on the top depict lifetime sexual and injection drug use subscale scores, and graphs on the bottom depict past 3 months sexual and injection drug use subscale scores. Never marijuana users are shown in open bars, former marijuana users in lightly shaded bars, and current users in black bars. Error bars depict standard errors. The “p < .05” refers to results from multivariate analyses of variance evaluating omnibus differences between the three marijuana using groups.
Logistic regression evaluated independent correlates of having more than 50 sexual partners over the lifetime. The model was significant, χ2(6) = 28.33, p < .001, correctly predicting 85.7% of the cases. Age was positively associated with greater likelihood of more than 50 sexual partners, β (SE) = 0.05 (0.02), Wald = 5.40, p < .02, OR (95% CI) = 1.05 (1.01–1.10). Opioid dependence was inversely related to having large numbers of lifetime sexual partners, β (SE) = −1.36 (0.58), Wald = 5.49, p < .02, OR (95% CI) = 0.26 (0.08–0.80). Current marijuana users had a greater likelihood of more than 50 lifetime sexual partners relative to never marijuana users, β (SE) = 1.37 (0.70), Wald = 3.76, p < .05, OR (95% CI) = 3.94 (1.00–15.74). Former marijuana users were more likely than never users to have had ≥50 partners, β (SE) = 1.67 (0.61), Wald = 7.59, p < .01, OR (95% CI) = 5.20 (1.62–17.30).
Marijuana use was also related to high numbers of recent sexual partners. A logistic regression predicting having more than 2 sexual partners in the past 3 months was significant, χ2(6) = 19.41, p < .01, predicting 87.7% of cases correctly. Over this timeframe, the only variable associated with greater than 2 sexual partners was marijuana status. Current marijuana users were more likely than never users to have had more than 2 recent sexual partners, β (SE) = 2.09 (0.73), Wald = 8.24, p < .01, OR (95% CI) = 8.05 (1.94–33.44).
Marijuana use status was also associated with low frequency of condom use (“rarely” or “never”) with casual sexual partners over lifetime. The overall model was significant, χ2 (6) = 17.70, p < .01, and correctly predicted 83.1% of cases. Age was significantly associated with low frequency of condom use with casual partners, β (SE) = 0.07 (0.02), Wald = 12.57, p < .001, OR (95% CI) = 1.07 (1.03–1.12). Former marijuana users were more likely to “rarely” or “never” use condoms with casual partners than never users, β (SE) = 1.05 (0.50), Wald = 4.48, p < .03, OR (95% CI) = 2.87 (1.08–7.61).
Marijuana use status was not a significant predictor of frequency of condom use with regular sexual partners over the lifetime or past 3 months, ps > .05. Marijuana use status was also not related to paid or anal sexual activities in either timeframe, ps > .05 (data not shown).
Discussion
Consistent with prior studies (9,11–14), opioid dependence was related to greater IV drug use risk behaviors, and cocaine dependence was associated with increased sexual risk behaviors. Even after controlling for these other drug use diagnoses, this study found consistent associations between marijuana use and increased risky sexual activities. Associations between marijuana use and risky sexual activities were noted both over the lifetime and the past 3 months, and they remained significant even after controlling for a range of variables including other illicit drug use. Polysubstance marijuana users in this study had a larger number of sexual partners, despite their younger age, and greater frequency of unprotected sex with casual partners than their non-marijuana using counterparts. These results are consistent with previous studies in student samples (24,25) and adolescents involved with the criminal justice system (26–28), indicating that marijuana use is associated with risky sexual activities.
Previous research examining the associations between marijuana use and risky sexual activities focused primarily on young samples, and it generally has not assessed or controlled for other illicit drug use or its impact on sexual risk behaviors. Consistent with epidemiological studies (32,34), marijuana users in this clinical sample were more likely to use and be dependent on cocaine and opioids than never users. Even after controlling statistically for other illicit drug use, associations between marijuana use and increased risky sexual activities remained significant.
Potential mechanisms behind the increased risks associated with marijuana use include situational and/or pharmacological effects of marijuana, which could decrease self-control and increase sexual-risk behaviors. For example, marijuana users may suffer a deficit in information processing (46), and they report sensory alteration and feelings of relaxation (47) that may impact willingness to engage in sexual activities when smoking marijuana. The group differences may also relate to differences in lifestyles or personality, such as greater impulsivity or risk-taking tendencies among polydrug marijuana users compared to their non-marijuana using counterparts.
The present findings, however, should be interpreted with caution given limitations of the study design. This was a cross-sectional study, and it did not analyze the association between marijuana use and sexual behavior in a longitudinal manner. Therefore, it could only assess global associations. Although we controlled for variables that differed between groups, findings could have been influenced by other variables that were not assessed. Participants were treatment-seeking polysubstance abusing patients in the Northeast, who appeared similar to patients seeking outpatient treatment generally (48,49). However, whether results generalize to other polysubstance abusing populations, samples using only marijuana, or substance abusers in other areas of the country remain to be determined. Future studies should focus on whether the increase in high-risk sexual behavior observed in this study was related to the direct effects of marijuana use or indicative of general characteristics of this sample. Additionally, marijuana dependence was not diagnosed in this study, and urine samples were not tested for marijuana. Marijuana classifications were by self-report, and some patients may have denied recent or lifetime use and been misclassified. Nevertheless, there were no legal or treatment consequences for reports of marijuana use, and items used to classify marijuana use status appear to have high face validity (see Methods). Furthermore, the group of current marijuana users was smaller than the other groups. Although power was sufficient to detect some significant associations, it may not have been high enough to detect other relationships that may be important.
Despite limitations, this is one of the first studies to examine explicitly the associations of marijuana use with HIV risk behaviors in adult polysubstance abusing patients seeking treatment. The clinical significance of these findings is that treatment-seeking polydrug abusing patients with current or past marijuana use histories may be at greater risk of HIV infection than their non-marijuana using counterparts, especially in terms of having multiple sexual partners. These findings go against the common belief that marijuana use may be relatively low risk (2,50). The data suggest that marijuana use among treatment-seeking adults with cocaine, opioid, and alcohol use disorders is an indicator of even greater risk. Efficacious HIV prevention campaigns, especially those targeting sexual risk behaviors, should be aimed at increasing awareness that marijuana use is associated with greater risky sexual behavior, even among those with an already high level of sexual risk behavior.
References
- 1.Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, de Girolamo G, Gureje O, Huang Y, Karam A, Kostyuchenko S, Lepine JP, Mora ME, Neumark Y, Ormel JH, Pinto-Meza A, Posada-Villa J, Stein DJ, Takeshima T, Wells JE. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS Med. 2008;5(7):e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 3.Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PF, Nelson EC, Statham DJ, Martin NG. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289(4):427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 4.Bjork JM, Grant SJ, Hommer DW. Cross-sectional volumetric analysis of brain atrophy in alcohol dependence: Effects of drinking history and comorbid substance use disorder. Am J Psychiatry. 2003;160(11):2038–2045. doi: 10.1176/appi.ajp.160.11.2038. [DOI] [PubMed] [Google Scholar]
- 5.Buster MA, Rook L, van Brussel GA, van Ree J, van den Brink W. Chasing the dragon, related to the impaired lung function among heroin users. Drug Alcohol Depend. 2002;68(2):221–228. doi: 10.1016/s0376-8716(02)00193-x. [DOI] [PubMed] [Google Scholar]
- 6.Higgins ST, Sigmon SC, Wong CJ, Heil SH, Badger GJ, Donham R, Dantona RL, Anthony S. Community reinforcement therapy for cocaine-dependent outpatients. Arch of Gen Psychiatry. 2003;60(10):1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- 7.Higgins ST, Heil SH, Dantona R, Donham R, Matthews M, Badger GJ. Effects of varying the monetary value of voucher-based incentives on abstinence achieved during and following treatment among cocaine-dependent outpatients. Addiction. 2007;102(2):271–281. doi: 10.1111/j.1360-0443.2006.01664.x. [DOI] [PubMed] [Google Scholar]
- 8.Lindsay JA, Stotts AL, Green CE, Herin DV, Schmitz JM. Cocaine dependence and concurrent marijuana use: A comparison of clinical characteristics. Am Journal Drug Alcohol Abuse. 2009;35(3):193–198. doi: 10.1080/00952990902933860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker A, Kochan N, Dixon J, Wodak A. Drug use and HIV risk-taking behaviour among injecting drug users not currently in treatment in Sydney, Australia. Drug Alcohol Depend. 1994;34(2):155–160. doi: 10.1016/0376-8716(94)90136-8. [DOI] [PubMed] [Google Scholar]
- 10.Chaisson RE, Baccheltti P, Osmond D, Brodie B, Sande MA, Moss AR. Cocaine use and HIV infection in intravenous drug users in San Francisco. JAMA. 1989;261(4):561–565. [PubMed] [Google Scholar]
- 11.Darke S, Hall W, Carless J. Drug use, injecting practices and sexual behaviour of opioid users in Sydney, Australia. Br J Addic. 1990;85(12):1603–1609. doi: 10.1111/j.1360-0443.1990.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 12.Flom PL, Friedman SR, Kottiri BJ, Neaigus A, Curtis R, Des Jarlais DC, Sandoval M, Zenilman JM. Stigmatized drug use, sexual partner concurrency, and other sex risk network and behavior characteristics of 18- to 24-year-old youth in a high-risk neighborhood. Sex Transm Dis. 2001;28(10):598–607. doi: 10.1097/00007435-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Hudgins R, McCusker J, Stoddard A. Cocaine use and risky injection and sexual behaviors. Drug Alcohol Depend. 1995;37(1):7–14. doi: 10.1016/0376-8716(94)01060-x. [DOI] [PubMed] [Google Scholar]
- 14.Rolfs RT, Goldberg M, Sharrar RG. Risk factors for syphilis: Cocaine use and prostitution. Am J Public Health. 1990;80(7):853–857. doi: 10.2105/ajph.80.7.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tyndall MW, Patrick D, Spittal P, Li K, O'Shaughnessy MV, Schechter MT. Risky sexual behaviours among injection drugs users with high HIV prevalence: implications for STD control. Sex Transm Infect. 2002;78(Suppl 1):170–175. doi: 10.1136/sti.78.suppl_1.i170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey SL, Camlin CS, Ennet ST. Substance use and risky sexual behavior among homeless and runaway youth. J Adolesc Health. 1998;23(6):378–388. doi: 10.1016/s1054-139x(98)00033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of Alcohol, Expectancies, and Partner Type on Condom Use in College Males: Event-Level Analyses. J Sex Res. 2005;42(3):259–266. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- 18.Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scott-Sheldon LJ, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS Behav. 2010;14(4):845–853. doi: 10.1007/s10461-008-9426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vanable PA, McKirnan DJ, Buchbinder SP, Bartholow BN, Douglas, Judson FN, MacQueen KM. Alcohol use and high-risk sexual behavior among men who have sex with men: The effects of consumption level and partner type. Health Psycho. 2004;23(5):525–532. doi: 10.1037/0278-6133.23.5.525. [DOI] [PubMed] [Google Scholar]
- 21.Shillington AM, Cottler LB, Compton WM, Spitznagel EL. Is there a relationship between 'heavy drinking' and HIV high risk sexual behaviors among general population subjects? Int J Addict. 1995;30(11):1453–1478. doi: 10.3109/10826089509055842. [DOI] [PubMed] [Google Scholar]
- 22.Adlaf EM, Smart RG. Risk-taking and drug-use behaviour: An examination. Drug Alcohol Depend. 1983;11(3–4):287–296. doi: 10.1016/0376-8716(83)90020-0. [DOI] [PubMed] [Google Scholar]
- 23.Lane SD, Cherek DR, Tcheremissine OV, Lieving LM, Pietras CJ. Acute Marijuana Effects on Human Risk Taking. Neuropsychopharmacology. 2005;30(4):800–809. doi: 10.1038/sj.npp.1300620. [DOI] [PubMed] [Google Scholar]
- 24.Poulin C, Graham L. The association between substance use, unplanned sexual intercourse and other sexual behaviours among adolescent students. Addiction. 2001;96(4):607–621. doi: 10.1046/j.1360-0443.2001.9646079.x. [DOI] [PubMed] [Google Scholar]
- 25.Bon SR, Hitner JB, Lawandales JP. Normative perceptions in relation to substance use and HIV-risky sexual behaviors of college students. J Psychol. 2001;135(2):165–178. doi: 10.1080/00223980109603688. [DOI] [PubMed] [Google Scholar]
- 26.Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Dev Psychol. 2012;48(5):1429–1442. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- 27.Kingree JB, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. J Adolesc Health. 2000;27(3):179–185. doi: 10.1016/s1054-139x(00)00101-4. [DOI] [PubMed] [Google Scholar]
- 28.Valera P, Epperson M, Daniels J, Ramaswamy M, Freudenberg N. Substance use and HIV-risk behaviors among young men involved in the criminal justice system. Am J Drug Alcohol Abuse. 2009;35(1):43–47. doi: 10.1080/00952990802342923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hensel DJ, Stupiansky NW, Orr DP, Fortenberry JD. Event-level marijuana use, alcohol use, andcondom use among adolescent women. Sex Transm Dis. 2011;38(3):239–243. doi: 10.1097/OLQ.0b013e3181f422ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS Behav. 2006;10(5):599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- 31.Anderson BJ, Stein MD. A behavioral decision model testing the association of marijuana use and sexual risk in young adult women. AIDS Behav. 2011;15(4):875–884. doi: 10.1007/s10461-010-9694-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Degenhardt L, Hall W, Lynskey M. The relationship between cannabis use and other substance use in the general population. Drug Alcohol Depend. 2001;64(3):319–327. doi: 10.1016/s0376-8716(01)00130-2. [DOI] [PubMed] [Google Scholar]
- 33.Grant BF, Pickering R. The relationship between cannabis use and DSM-IV cannabis abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1998;10(3):255–264. doi: 10.1016/s0899-3289(99)00006-1. [DOI] [PubMed] [Google Scholar]
- 34.von Sydow K, Lieb R, Pfister H, Höfler M, Sonntag H, Wittchen H. The natural course of cannabis use, abuse and dependence over four years: A longitudinal community study of adolescents and young adults. Drug Alcohol Depend. 2001;64(3):347–361. doi: 10.1016/s0376-8716(01)00137-5. [DOI] [PubMed] [Google Scholar]
- 35.Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168(2):93–97. [PMC free article] [PubMed] [Google Scholar]
- 36.Petry NM, Weinstock J, Alessi SM. A randomized trial of contingency management delivered in the context of group counseling. J Consult Clin Psychol. 2011;79(5):686–696. doi: 10.1037/a0024813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. text rev. Washington, DC: Author; 2000. [Google Scholar]
- 38.Petry NM, Alessi SM. Prize-based contingency management is efficacious in cocaine-abusing patients with and without recent gambling participation. J Subst Abuse Treat. 2010;39(3):282–288. doi: 10.1016/j.jsat.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petry NM, Kolodner KB, Li R, Pierce JM, Roll JR, Stitzer ML, Halminton JA. Prize-based contingency management does not increase gambling. Drug Alcohol Depend. 2006;83(3):269–273. doi: 10.1016/j.drugalcdep.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 40.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. Washington, DC: American Psychiatric Press, Inc.; 1996. [Google Scholar]
- 41.Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5(2):181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Petry NM. Reliability of drug users’ self-reported HIV risk behaviors using a brief, 11-item scale. Subst Use Misuse. 2001;36(12):1731–1747. doi: 10.1081/ja-100107576. [DOI] [PubMed] [Google Scholar]
- 43.McLellan AT, Luborsky L, Cacciola J, Griffith JE, Evans F, Barr HL, O'Brien CP. New data from the Addiction Severity Index Reliability and validity in three centers. The J Nerv Ment Dis. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Bovasso GB, Alterman AI, Cacciola JS, Cook TG. Predictive validity of the Addiction Severity Index’s composite scores in the assessment of 2-year outcomes in a methadone maintenance population. Psychol Addict Behav. 2001;15(3):171–176. [PubMed] [Google Scholar]
- 45.Leonhard C, Mulvey K, Gastfriend D, Shwartz M. The addiction severity index: a field study of internal consistency and validity. J Subst Abuse Treat. 2000;18(2):129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 46.Kelleher LM, Stough C, Sergejew AA, Rolfe T. The effects of cannabis on information-processing speed. Addict Behav. 2004;29(6):1213–1219. doi: 10.1016/j.addbeh.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 47.Green B, Kavanagh D, Young R. Being stoned: A review of self-reported cannabis effects. Drug Alcohol Rev. 2003;22(4):453–460. doi: 10.1080/09595230310001613976. [DOI] [PubMed] [Google Scholar]
- 48.Ross J, Teesson M, Darke S, Lynskey M, Ali R, Ritter A, Cooke R. The characteristics of heroin users entering treatment: Findings from the Australian treatment outcome study (ATOS) Drug Alcohol Rev. 2005;24(5):411–408. doi: 10.1080/09595230500286039. [DOI] [PubMed] [Google Scholar]
- 49.bSubstance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment Episode Data Set (TEDS): 1996–2006. National Admissions to Substance Abuse Treatment Services, DASIS Series: S-43, DHHS Publication No. (SMA) 08-4347. Rockville, MD: 2008. [Google Scholar]
- 50.Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J Stud Alcohol Drugs. 2009;70(2):279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]