Abstract
Regulatory T (TR) cells consist of phenotypically and functionally distinct CD4+ and CD8+ T cell subsets engaged both in maintaining self-tolerance and in preventing anti–non-self effector responses (microbial, tumor, transplant, and so on) that may be harmful to the host. Here we propose that the proinflammatory function of virus-specific memory effector CCR7–CD8+ T cells, which are massively recruited in the liver, are inefficient (in terms of IFN-γ production) in patients with chronic hepatitis C virus (HCV) infection because of the concomitant presence of virus-specific CCR7–CD8+ TR cells producing considerable amounts of IL-10. These CD8+ TR cells are antigen specific, as they can be stimulated by HCV epitopes and suppress T cell responses that are in turn restored by the addition of neutralizing anti–IL-10. This study provides for the first time to our knowledge direct evidence of the existence of virus-specific CD8+ TR cells that infiltrate the livers of patients with chronic HCV infection, identifies IL-10 as a soluble inhibitory factor mediating suppression, and suggests that these cells play a pivotal role in controlling hepatic effector CD8+ T cell responses.
Introduction
Hepatitis C virus (HCV) is capable of persisting in the host to establish a lifelong liver disease in the majority of infected individuals (reviewed in ref. 1). The high propensity of HCV to establish persistent infection has been related to a severe dysfunction of HCV-specific CD8+ CTLs, which seems to be a critical factor in preventing resolution of infection and in favoring the onset of chronic liver immunopathology (1–11). In addition, further data indicated inefficient CTLs in both HCV-related and -unrelated chronic infections, suggesting that this phenotype is not restricted to HCV but is widely present in persistent viral infections (4, 12–17). However, the studies conducted thus far have not addressed the issues of why the expansion of HCV-specific CTL populations contrasts with their poor capacity to perform immediate effector functions or whether intrahepatic T cell populations have particular subsets involved in the establishment of chronic infection. Recently, a large body of evidence has indicated that different types of both CD4+ and CD8+ regulatory T (TR) cells, once activated, possibly in an antigen-specific manner, suppress excessive effector responses in an antigen-specific or a -nonspecific manner (18–24). This equilibrium may establish a status of long-lasting low-level inflammation critical to the survival of both the microbial agent and the host.
Here we report that patients with chronic HCV infection show a considerable enrichment of HCV-specific CTLs in the liver (in contrast to what is observed in the periphery) that express the tissue-homing phenotype of memory effector (ME) cells (CCR7–) (25), despite the fact that only a minority of these CTLs carry out prompt proinflammatory functions. Importantly, we demonstrate the concomitant presence in the liver of HCV-specific CTLs producing IL-10 that appear to have regulatory functions and thus have a major role in the establishment of the long-lasting low-level liver inflammation.
Methods
Study population.
We studied 48 patients with chronic HCV infection (Table 1) and 40 healthy donors (age range, 20–54 years; 28 HLA-A2+ and 12 HLA-A3+) as controls (for analyses of peripheral blood), according to the ethical guidelines of the 1975 Declaration of Helsinki and a priori approval by our Institutional Review Board. Serum HCV RNA levels and HCV genotypes were determined by Versant HCV RNA 3.0 (bDNA) and INNO-LiPA HCV II, respectively (Bayer Corporation, Tarrytown, New York, New York, USA). None of the patients were being treated with IFN-α with or without ribavirin at the time of this study. Of the 48 patients, 47 underwent percutaneous needle liver biopsy, part of which was processed for diagnostic and part, for immunological analyses. Histology was graded by the histological activity index (HAI): periportal necrosis, intralobular necrosis, or portal inflammation (values range from 0 to 10, 0 to 4, or 0 to 4, respectively; their sum provides “grading” or the “inflammatory index”), fibrosis (ranging from 0 to 4; this leads to “staging” or the “fibrosis index”), and total score (grading + staging) (26) (Table 1).
Table 1.
Clinical parameters of patients with chronic HCV infection
Cell preparations.
Lymphoprep cushions (Nycomed pharma, AS, Oslo, Norway) were used to isolate PBMCs from peripheral blood and liver-infiltrating lymphocytes (LILs) from liver biopsies, as previously described (3). CD8+ T cells were isolated from PBMCs or LILs by immunomagnetic separation with mouse anti-CD8–conjugated magnetic microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany). CCR7+ and CCR7– cells were purified from PBMCs by staining with purified mAb to CCR7 (3D12, rat IgG2a) (25) followed by phycoerythrin-conjugated (PE-conjugated) goat anti-rat IgG2a (Southern Biotechnology Associates, Birmingham, Alabama, USA) and then by mouse IgG1 anti-PE–conjugated magnetic microbeads (Miltenyi Biotec). FACS analysis demonstrated more than 99% CCR7+ cells in the positively purified population and less than 11% CCR7+ cells in the CCR7-depleted population. Immature DCs were derived from peripheral monocytes that had been purified by positive selection with mAb to CD14 coupled to magnetic beads (Miltenyi Biotec). Then, CD14+ cells were cultured for 5 days in RPMI 1640/5% FCS medium containing 2 mM glutamine, 1% nonessential amino acids, 1% sodium pyruvate, 50 μg/ml kanamycin (Gibco BRL), 50 ng/ml GM-CFS (Novartis Pharma, Basel, Switzerland), and 1,000 U/ml recombinant IL-4, kindly provided by Antonio Lanzavecchia (Institute for Research in Biomedicine, Bellinzona, Switzerland). DC maturation was induced by a 40-hour stimulation with CD40L-transfected J558L cells (at a DC/J558L ratio of 1:1), kindly provided by Peter Lane (University of Birmingham Medical School, Birmingham, UK), as previously described (27, 28).
Cytofluorimetric assays.
PBMCs or LILs were stained with a combination of tetramers and different mAb’s as previously described (3). The tetramers included PE- or PE-indodicarbocyanine–labeled (PE-Cy5–labeled) HLA-A2 tetramers in complexes with HCV nonstructural protein 31073–1081 (NS31073–1081) (CINGVCWTV), NS31406–1415 (KLVALGINAV), or NS41851–1859 (ILAGYGAGV) peptide, and PE-Cy5–labeled HLA-A3 tetramers in complexes with HCV core51–59 (KTSERSQPR), E2632–641 (RMYVGGVEHR), or NS31267–1275 (LGFGAYMSK) (Proimmune Limited, Oxford, UK). The mAb’s included tricolor (TC)- or PE-labeled anti-CD8 (Caltag Laboratories, Burlingame, California, USA), FITC-labeled anti-CD8 (Becton Dickinson, BD Pharmingen, San Diego, California, USA), and FITC-labeled anti-perforin (BD Pharmingen). Staining with mAb to CCR7 was performed prior to tetramer staining and was followed by the addition of labeled secondary antibodies. Cells were washed, acquired with a FACSCalibur flow cytometer (Becton Dickinson, San Jose, California, USA), and analyzed using CellQuest software (Becton Dickinson). Negative controls were obtained by staining cells with an irrelevant isotype-matched mAb.
Functional assays.
In functional experiments, PBMCs or LILs previously stained with tetramer and different mAb’s were left unstimulated or were stimulated for 6 hours at 37°C with peptide (10 μg/ml) plus mAb to CD28 (4 μg/ml) (BD Pharmingen); PMA (50 ng/ml) plus ionomycin (1 μg/ml) (Sigma-Aldrich, Milan, Italy); or peptide plus autologous irradiated PBMCs as APCs. At the second hour, 10 μg/ml brefeldin-A (Sigma-Aldrich) was added. Cells were washed, fixed, and permeabilized using Cytofix/Cytoperm solution (BD Pharmingen) at 4°C for 20 minutes, rewashed with Perm Wash Buffer (BD Pharmingen), and intracellularly stained with FITC-, PE- (BD Pharmingen), or PE-Cy5– (Jackson ImmunoResearch, West Grove, Pennsylvania, USA) labeled anti–IFN-γ or anti–IL-10 for 30 minutes at 4°C. Similar assays were performed by using short-term CD8+ lines derived from purified CCR7+CCR7– cells (after 7–10 days of stimulation with peptide plus mature DCs or 3 days of preculture with IL-2), PBMCs or LILs (after 7–10 days of stimulation with peptide plus anti-CD28 or 3 days of preculture with IL-2).
Suppressor assays.
In the antigen-nonspecific assays, PBMCs (responder cells) were cultured in 96-well round-bottomed plates for 6 days with or without 4 × 104 to 5 × 104 cells/well of highly purified CD8+ LILs as suppressor cells in the presence of both soluble anti-CD3 and anti-CD28 (BD Pharmingen) at a responder/suppressor ratio of 2/1. Because of the paucity of cells, we pooled LILs from two to three liver biopsies derived from different patients. In addition, supernatants from the cocultures described above were collected at the end of incubation and analyzed for IL-10 by ELISA (BD Immunocytometry Systems). In order to evaluate the antigen specificity of the suppressor cells, PBMCs were cocultured with autologous LILs (derived from single biopsies) in the presence or absence of both recombinant chimeric NS3/NS4 (IRIS Research Center, Chiron S.p.A., Siena, Italy) and HLA-A2–related HCV peptides. In some wells, neutralizing anti–IL-10 (JES3-9D7, IgG1), mAb to perforin (27-35; IgG2b) (10 μg/ml, BD Pharmingen), IL-2 (50–100 U/ml), or IgG1-IgG2b isotype controls were added at the beginning of the assay. Eighteen hours before cultures were harvested, 1 μCi [3H]thymidine (Amersham, Buckinghamshire, UK) was added and the cell radioactivity was determined as described (29).
Results
Low frequencies of peripheral (preferentially CCR7+) HCV-specific CTLs.
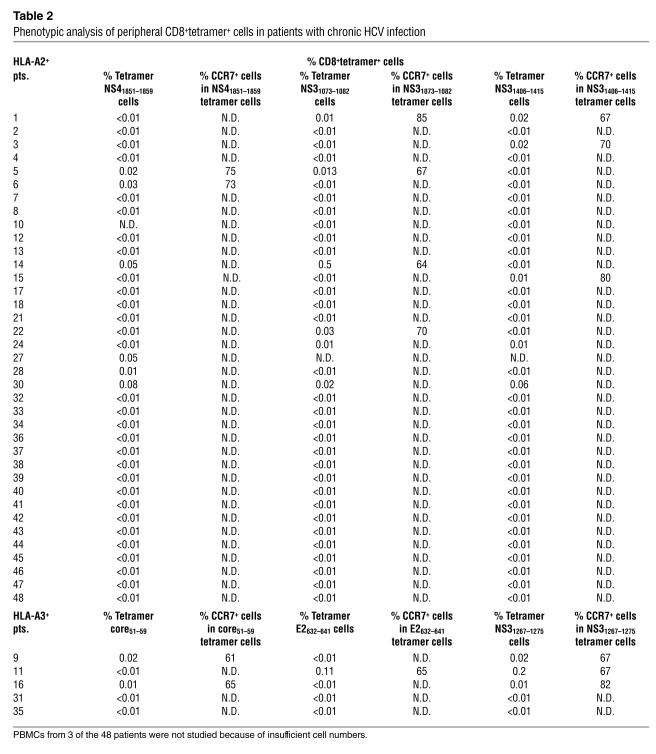
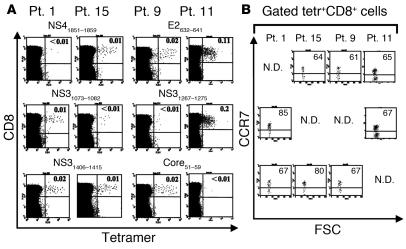
CD8+ class I HLA–peptide tetrameric complex+ (tetramer+) cells appeared at very low frequencies in the peripheral blood of patients chronically infected with HCV (Table 2 and Figure 1), and the majority of them expressed the central memory (CM) CCR7+ phenotype (25) (Table 2 and Figures 1 and 2A). The peripheral tetramer values were less than 0.01% (with a mean ± SD of 0.00347 ± 0.01612 for all the tetramer analyzed) in all healthy individuals studied; thus, 0.01% was considered the sensitivity level of the assay. Because of the very low percentages of peripheral tetramer+ cells, we were unable to document an effector function in any of the patients except for three showing a significant percentage of HCV-specific CTLs in the peripheral blood (Figure 3). Furthermore, they did not have significant antigen-specific effector function ex vivo, as detected by the production of IFN-γ or IL-10 in response to a few hours of contact with viral peptides (Figure 3). These cells were not intrinsically defective, as the majority of them produced IFN-γ promptly and efficiently in response to PMA and ionomycin (Figure 3). They proliferated abundantly and differentiated into effector cells in response to sustained antigen stimulation (Figure 4). This capability was a feature of CCR7+CD8+ T cellsCM, as only the positively selected CCR7+ but not the CCR7-depleted CD8+ T cellsME were capable of extensively differentiating upon sustained antigen/DC stimulation in vitro (Figure 4) (10, 25, 30–33). However, the finding that no correlation was shown between peripheral CTL frequencies (as well as the intrahepatic [see below]) and serum HCV RNA or alanine transaminase (ALT) levels suggests that CD8+ T cellsCM in vivo generate a massive expansion of the CD8+ T cellME population (homing to inflamed liver [see below]) that does not demonstrate an appropriate protective function.
Table 2.
Phenotypic analysis of peripheral CD8+tetramer+ cells in patients with chronic HCV infection
Figure 1.
Low frequencies of peripheral virus-specific CD8+ T cells expressing a dominant CM (CCR7+) phenotype. PBMCs from two representative HLA-A2+ patients (Pt. 1 and Pt. 15) and two HLA-A3+ patients (Pt. 9 and Pt. 11) were stained first with rat mAb to CCR7 and then with secondary FITC-conjugated goat anti-rat Ig, PE-Cy5–labeled anti-CD8, and the indicated PE-Cy5–labeled tetramers. (A) Dot plot analyses showing CD8+tetramer+ cell percentages. (B) Dot plots, corresponding to those reported in A, are gated on tetramer+CD8+ (Tetr+CD8+) cells, and show CCR7 staining. Results are expressed as percentage of cells, indicated in each quadrant. N.D., not determined; FSC, forward scatter.
Figure 2.
Correlations among immunological and clinical parameters. (A) Tetramer+ CD8+CCR7+ cells are significantly more numerous than their CCR7– counterparts in the peripheral (Periph.) blood of patients with chronic HCV infection. Each line represents a single patient. Only tetramer+ populations showing detectable CCR7+ cells have been considered. Statistical analysis was performed by Student’s t test for paired data. (B) Tetramer+CD8+ cells are significantly more numerous in the liver than in the peripheral blood of patients with chronic HCV infection. Each line joining a pair of circles between “Periphery” and “Liver” represents a single patient. Each “Periphery” circle represents the sum of peripheral virus-specific CD8+ T cell frequencies, which were detected by the single tetramers (Table 2). Each “Liver” circle represents the frequencies of virus-specific CD8+ LILs, as detected by the tetramer pool (Table 3). Statistical analysis was performed by Student’s t test for paired data; this included the values less than 0.01% that were arbitrarily considered 0%. (C) Frequencies of tetramer+CD8+ LILs producing IFN-γ are directly correlated with total HAI score. Statistical analysis was performed by the Spearman correlation test. (D) Frequencies of tetramer+CD8+ LILs producing IL-10 are inversely related to total HAI score. Statistical analysis was performed by the Spearman correlation test.
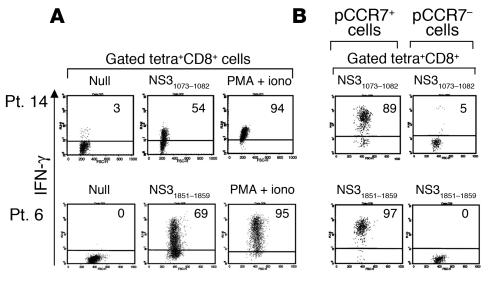
Figure 3.
Inefficient effector capacity of peripheral virus-specific CD8+ T cells ex vivo. Representative functional analyses of PBMCs from one HLA-A3+ patient (Pt. 11) and two HLA-A2+ patients (Pt. 6 and Pt. 14) selected for their elevated frequencies of peripheral virus-specific CD8+ T cells, as detected by the indicated tetramers. PBMCs from patients 11 and 6 were previously stained with rat mAb to CCR7, followed by staining with the secondary PE- or FITC-conjugated goat anti-rat Ig, TC-labeled anti-CD8, and the indicated PE-Cy5– or PE-labeled tetramers. Then, cells were stimulated with the relevant peptide and mAb to CD28 or with PMA and ionomycin (iono) and after 6 hours were stained intracellularly with FITC- or PE-labeled anti–IFN-γ. Gated tetramer+CD8+ cells show both single CCR7 staining in forward scatter analysis and double CCR7 and IFN-γ staining. PBMCs from patient 14 were stained with anti-CD8 and tetramers, then stimulated as described above and after 6 hours were stained intracellularly with FITC-labeled anti–IFN-γ or anti–IL-10. Gating analyses were performed at the CD8+ cell level.
Figure 4.
Peripheral virus-specific CCR7+ CTLs efficiently differentiate upon antigen-driven proliferation in vitro. (A) PBMCs from HLA-A2+ patients 14 and 6 (Pt. 14 and Pt. 6) (see Table 2) were stimulated with the indicated peptide plus anti-CD28 for 7 days. Then, cells were stained with the corresponding PE-Cy5– or PE-labeled HLA-A2.1+ tetramers and TC- or FITC-labeled mAb to CD8, restimulated or not with peptide and autologous APCs or PMA plus ionomycin for 6 hours, and stained intracellularly with FITC- or PE-Cy5–labeled mAb to IFN-γ. Dot plots are gated on tetramer+CD8+ cells. Results are expressed as percentage of cells. (B) Both peripheral CCR7+ (pCCR7+) and pCCR7– cells purified from PBMCs from both patients were cultured with the relevant peptides and autologous DCs for 7 days. Then, cells were double-stained with the corresponding PE-Cy5–labeled HLA-A2.1+ tetramers and TC- or FITC-labeled mAb to CD8, restimulated for a few hours with peptide and autologous Epstein-Barr virus B cells as APCs, and stained intracellularly with FITC- or PE-labeled mAb to IFN-γ. Dot plots are gated on tetramer+CD8+ cells. Results are expressed as percentage of cells.
Hepatic expansion of an inefficient effector CCR7– HCV-specific CTL population.
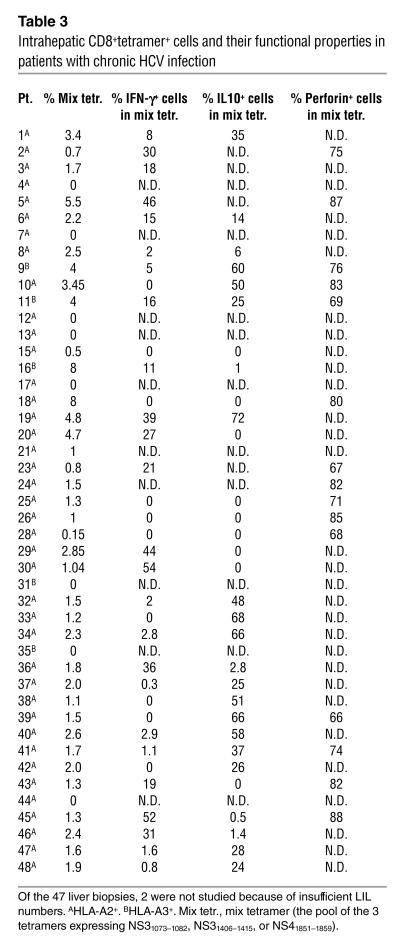
In order to validate the hypothesis of a selective compartmentalization of effector CTLs in infected livers, we compared LILs from patients chronically infected with HCV with those derived from peripheral blood. Because of the low number of LILs obtained from each biopsy (5 × 104 to 7 × 104 cells/biopsy), they were stained with the pool of either HLA-A2/HCV or HLA-A3/HCV tetramers plus mAb’s to CD8 and CCR7. The frequency of virus-specific CD8+ LILs, as detected by the tetramer pool, was significantly higher (with a mean of about 300-fold) than the corresponding sum of the peripheral cells, which were detected by the single tetramers (Table 3 and Figures 2B and 5). The peripheral tetramer+CD8+ cell percentages less than 0.01 (the sensitivity level of our assay) were arbitrarily considered 0% in the statistical analyses but do not appear in the plot because of the y-axis logarithmic scale. Moreover, in contrast to observation at the peripheral blood level, virtually all tetramer+ LILs had lost CCR7, thus acquiring the typical tissue-homing phenotype of ME cells (25) (Figure 5A). This phenotype was related to high expression of perforin, supporting the notion that the loss of CCR7 is a hallmark of ME cells (Table 3 and Figure 5A). Despite the acquisition of the ME phenotype, only a minority of CCR7– LILs acquired prompt IFN-γ production capacity after a few hours of contact with the pool of corresponding viral peptides (Table 3 and Figure 5B). Importantly, the frequency of tetramer+IFN-γ+CD8+ LILs was directly related to the total HAI score (Table 3 and Figure 2C), supporting the hypothesis of a major role of HCV-specific CTLs producing IFN-γ in establishing chronic liver immunopathology. Patients 10, 15, 18, 25, 26, 28, 33, 38, and 39 are presented as a single overlapping circle because they showed identical values for both HAI score (with a score of 2) and tetramer+CD8+IFN-γ+ cell percentage (0%) (see Tables 1 and 3). As expected, as with the peripheral CCR7– CTLs and in contrast to CCR7+ CTLs, LILs (being CCR7–) were unable to proliferate in response to sustained antigen stimulation (data not shown) (25, 30–32). Tetramer+ LILs, however, were capable of synthesizing large amounts of IFN-γ in response to 4–6 hours of antigen contact, after a brief preculture (48–72 hours) with IL-2 (50–100 U/ml) (Figure 6). These data suggest that CCR7– CTLs can terminate the effector cell program following exposure to IL-2, which is thought to be critical in driving full effector CTL differentiation (10, 11, 34).
Table 3.
Intrahepatic CD8+tetramer+ cells and their functional properties in patients with chronic HCV infection
Figure 5.
Concomitant hepatic expansions of virus-specific CCR7– CTL subsets with inappropriate proinflammatory functions or regulatory phenotypes. (A) Representative tetramer+CD8+ LILs from HLA-A2.1+ patient 2 (see Table 3) expressing the membrane phenotype (CCR7–) of effector cells and high perforin levels, but inappropriate IFN-γ production. In particular, LILs from patient 2 were subdivided in two parts. One part was stained intracellularly with TC-labeled mAb to CD8, the pool of PE-labeled HLA-A2.1+ tetramers expressing NS31073–1082, NS31406–1415, or NS41851–1859 (mix tetramer, Mix tetr.), and FITC-labeled anti-perforin. A second part, after being stained with primary rat mAb to CCR7, was stained with the secondary PE-conjugated goat anti-rat Ig and the pool of tetramers indicated above. Then, following stimulation or no stimulation with the corresponding peptides and APCs (autologous irradiated PBMCs) for 6 hours, cells were stained intracellularly with FITC-labeled mAb to IFN-γ. Dot plots are gated on tetramer+ cells. Results are expressed as percentage of cells. Similar results were obtained by studying the other patients tested (see Table 3) with the pool of tetramers indicated for each patient in Table 2. (B) Tetramer+CD8+ LILs isolated from each indicated patient producing poor IFN-γ but notable amounts of IL-10. LILs were stained with the mix tetramer (indicated for each patient in the Table 2), were left unstimulated or were stimulated with the corresponding peptides and autologous APCs for few hours, and were stained intracellularly with both FITC-labeled mAb to IFN-γ or to IL-10. IFN-γ or IL-10 was undetectable in unstimulated cultures in both experiments in A and B (data not shown).
Figure 6.
IL-2 drives virus-specific CCR7– cells to terminate the effector cell program. (A and B) Two independent experiments, in which LIL pools derived from two biopsies (for each experiment) of HLA-A2+ patients, were cultured with 50 U/ml IL-2 for 3 days. Then, cells were stained with TC-labeled mAb to CD8, and the pool of PE-labeled HLA-A2.1+ mix tetramer stimulated with the corresponding peptides and autologous PBMCs as APCs for 6 hours, and stained intracellularly with FITC-labeled mAb to IFN-γ. Dot plots are gated on tetramer+CD8+ cells. Results are expressed as percentage of cells. Null, no stimulus. (C) Fresh peripheral (p)CCR7+ and CCR7– cells purified from PBMCs of the patients presented in A were cultured with IL-2 as described above and stained with FITC-labeled mAb to CD8 and PE-Cy5–labeled HLA-A2.1+ tetramers expressing NS41851–1859. Then, cells were stimulated with autologous APCs and NS41851–1859 peptide for 6 hours and were stained intracellularly with PE-labeled mAb to IFN-γ. Dot plots are gated on tetramer+CD8+ cells. Results are expressed as percentage of cells.
Hepatic expansion of an IL-10–producing HCV-specific CCR7– CTL population.
At variance with peripheral CTLs, some of the CD8+tetramer+ LILsME were capable of producing IL-10 following peptide stimulation for 6 hours in vitro (Table 3 and Figure 4B). Notably, no double IFN-γ+IL-10+ cells were visualized within each tetramer+ population analyzed, suggesting that these cytokines were not synthesized by the same cells (data not shown). Importantly, tetramer+IL-10+CD8+ LIL frequencies were inversely related to the total HAI score (Figure 2D), in contrast to the tetramer+IFN-γ+ LIL frequencies that were directly related (Figure 2C). Patients 15, 18, 25, 26, and 28, showing identical HAI scores and tetramer+CD8+IL-10+ cell percentages, are presented as a single circle corresponding to an HAI score of 2 and tetramer percentage of 0; patients 20, 29, and 43 are presented as a circle corresponding to an HAI score of 7 and 0% CD8+tetramer+IL-10+ cells (see Table 3). Although we were unable to determine whether tetramer+perforin+CD8+ cells were confined within either IFN-γ+ or IL-10+ cell populations for the trivial reason of insufficient numbers of LILs, the finding that the majority of those analyzed expressed perforin suggests that they should be present in both tetramer+IFN-γ+ and tetramer+IL-10+ CD8+ LIL populations (Table 3), indicating that the latter control the proinflammatory rather than the potential cytotoxic function. The fact that no correlation was shown between the percentages of HCV-specific LILs producing either IFN-γ or IL-10 and either serum HCV RNA or ALT levels suggests that the intrahepatic HCV-specific CCR7– LILs are unable to clear the virus, possibly because of the IL-10–mediated suppression of the antiviral effect of IFN-γ.
Suppressor activity of intrahepatic IL-10–producing CD8+ T cells.
Because of the limitation of the tiny number of LILs we obtained (about 5 × 104 to 7 × 104 from each biopsy), we set up a simple and reproducible non–antigen-specific suppressor assay by pooling LILs obtained from two to three biopsies, with a yield of 1.5 × 105 cells. The rationale of this assay is that coculture of highly purified CD8+ LILs and PBMCs in the presence of mAb’s to CD3 and CD28 should simultaneously induce the proliferation of PBMCs as well as the prompt stimulation of the in vivo–differentiated CD8+ LILs with regulatory function (that should suppress PBMC proliferation) and the cytokines required for suppression. Importantly, in the majority of experiments, CD8+ LILs demonstrated a marked suppression function in terms of inhibition of PBMC proliferation, strongly supporting the idea of a major role played by CD8+ LILs as regulatory cells (Figure 7A). As expected, the same results were obtained by using either autologous or allogeneic PBMCs as responders in this non-antigen-suppression system. The addition of neutralizing anti–IL-10, but not of mAb to perforin or the corresponding isotypes used as a control, markedly abrogated suppression only by IL-10–producing CD8+ LILs (Figure 7, A and B). However, the finding that suppression was also exerted by some IL-10–CD8+ LILs suggests that further unknown suppression mechanisms are involved (Figure 7, A and B). Interestingly, the addition of IL-2 to the same cocultures abrogated the suppression function (Figure 7A). The finding that in independent experiments IL-2 selectively drove full effector cell differentiation (Figure 6) favors the possibility that this cytokine may overcome suppression via its effect in promoting differentiation of effector cells in PBMC populations, rather than blocking suppression by LILs. This hypothesis is corroborated by the evidence that IL-2 improved PBMC proliferation in control cultures to which CD8+ LILs had not been added (Figure 7A). Furthermore, control experiments showed that the addition of mAb to IL-10 to cultures containing only PBMCs did not exert any effect (Figure 7A), ruling out the possible presence of IL-10–producing regulatory cells in the periphery.
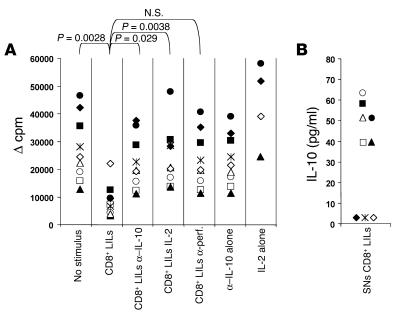
Figure 7.
Hepatic IL-10–producing CD8+ T cells perform a regulatory function. (A) Highly purified CD8+ LILs pooled from two to three biopsies were cocultured with PBMCs plus soluble mAb’s to CD3 and CD28 in the presence or absence of anti–IL-10 (α–IL-10), mAb to perforin (α-perf), or IL-2. Control cocultures were prepared in the presence of either IgG1 or IgG2b isotype, which did not produce any interference with suppressive function (data not shown). Control cultures in which PBMCs were stimulated with mAb’s to CD3 and CD28 in the presence of IL-2 or anti–IL-10 but in the absence of CD8+ LILs were also prepared. Each symbol represents an individual experiment performed with single LIL pool derived from two biopsies. In all experiments, 1 μC [3H]thymidine was added to the cultures after 6 days and the radioactivity incorporated by cells was determined after 18 hours. The cpm values were calculated after subtraction of background (Δ cpm). Statistical analysis was performed by Student’s t test for paired data. (B) The production of IL-10 was determined in the supernatant pool (not conditioned with mAb to IL-10) from cocultures indicated by symbols.
Antigen specificity of regulatory CD8+ LILs.
In an attempt to define the antigen specificity of the regulatory cells, we cocultured LILs derived from single biopsies with autologous PBMCs in the presence of both the relevant HLA-A2–related HCV peptides and a soluble form of a chimeric NS3/NS4. The rationale of this assay is that APC populations contained in PBMC populations can simultaneously present both soluble recombinant NS3/NS4 to their own (CD4+) T cells and HLA-A2-related HCV peptides to the in vivo–differentiated antigen-specific CD8+ regulatory cells, which in turn should inhibit the PBMC response to antigenic HCV stimuli if present in the autologous LIL population. In six independent experiments, performed with PBMCs for their capacity to proliferate in response to soluble NS3/NS4, LILs from HLA-A2+ patients were able to suppress autologous antigen-specific PBMC responses only upon antigen-specific activation with the pool of the HLA-A2–related peptides (NS31073–1081, NS31406–1415, and NS41851–1859) (Figure 8, A–F) but not when left unstimulated (Figure 8, A–F) or when stimulated with the pool of irrelevant HLA-A2–related HIV peptides (pol919–927, nef94–102, and env49–57) (Figure 8, E and F). These data clearly support the concept that the suppression function is antigen specific at least in the induction phase (18–20). Of note, the suppression was strongly overcome by the addition of neutralizing mAb to IL-10 (Figure 8, A–D).
Figure 8.
HCV antigens induce regulatory CD8+ T cells. (A–D) Four independent experiments showing that LILs derived from four HLA-A2+ patients suppress HCV-specific proliferation by autologous PBMCs only when stimulated with HCV peptides (HCVLILs) but not when left unstimulated (LILs). In particular, HLA-A2+ PBMCs were cocultured with autologous LILs in the presence or absence of both HLA-A2–related HCV peptides (NS31073–1081, NS31406–1415, and NS41851–1859) and soluble recombinant chimeric NS3/NS4. In some wells, anti–IL-10 Ab was added. (E and F) Two control experiments showing that LILs derived from two HLA-A2+ patients suppress HCV-specific proliferation by autologous PBMCs only when stimulated with HCV peptides (HCVLILs) but not when stimulated with irrelevant HLA-A2–related HIV peptides (pol919–927, nef94–102, and env49–57) (HIVLILs). After 6 days of coculture, 1 μCi [3H]thymidine was added to the cultures and the radioactivity incorporated by cells was determined after 18 hours. The cpm values of PBMCs (in the absence of LILs) in response to NS3/NS4 were calculated after subtraction of background and are indicated in parenthesis. The percent of suppression was calculated with the following formula: (PBMC-LIL coculture cpm / PBMC cpm) × 100.
Discussion
In this study, we have provided evidence that patients with chronic HCV infection show concomitant and considerable intrahepatic expansion of two independent subsets of virus-specific CCR7–CD8+ T cellME populations characterized by their capacity either to exert poor proinflammatory functions or to produce sizable amounts of IL-10. The finding that HCV-specific CCR7+CD8+ T cellsCM were confined only to the periphery and that they efficiently differentiated into effector cells in response to sustained antigen stimulation (in contrast to the CCR7– cellsME preferentially recruited in the liver) supports the model proposing different anatomical locations for these functionally distinct subsets (25, 35–37). Several lines of evidence indicate that T cellsCM express CCR7 and CD62L, allowing homing to peripheral lymphoid tissues where they can proliferate and rapidly differentiate into effector cells upon re-encountering microbial antigens. In contrast, T cellsME lose CCR7 and CD62L and can thus migrate into inflamed tissues (25, 35–37). The peripheral expansion of an HCV-specific CCR7+ CTLCM population in chronically infected patients is in contrast with previous findings in patients with acute HCV infection, who showed predominant expansion of an activated HCV-specific CCR7–CD8+ T cellME population in the peripheral blood (8, 10). It is tempting to hypothesize that the signal strength provided during T cell activation (31–33) may regulate different aspects of T cell differentiation in acute or chronic infections. In particular, in acute resolving HCV infection, the high viral load may push the majority of CM cells to differentiate into effector memory CTLs that disappear in parallel with the decrease in viremia, leaving a low level of central memory cells (8, 10). These CTLs can be maintained by homeostatic mechanisms in the absence of antigen (31–33). Instead, under conditions in which HCV successfully overcomes the effector T cell responses, persistent infection may maintain stable expansion of a peripheral HCV-specific CCR7+ CTLCM population with high proliferative potential; these cells would be instrumental in providing continuous waves of CCR7– CTLsME homing to the infected liver (31–33). However, CCR7– CTLsME (because of poor effector function) would be responsible for control but not resolution of the infection, a process resulting in chronic mild hepatitis. These data are consistent with recent studies in a murine model proposing that during persistent Leishmania major infection, CD4+CD25+ TR cells control the immune response to a degree that is sufficient to contain (but not to eradicate) the protozoa, thus allowing both the maintenance of memory T cells and the suppression of detrimental T cell effector responses (38).
In agreement with the view proposed in the previously described murine model study (38), the majority of intrahepatic HCV-specific CTLs were characterized by their inability to function as fully differentiated effectors, despite the acquisition of an effector tissue-homing membrane phenotype and expression of high levels of perforin (CCR7–perforinhighIFN-γlow). Despite their poor effector performance, these intrahepatic CTLs were directly related to the total HAI score, but not to ALT levels, suggesting that they are involved principally in determining the recruitment of inflammatory cells rather than hepatocyte lysis. This view is in accordance with the notion that serum ALT levels do not accurately reflect the degree of the hepatic inflammatory score (39). The significant intrahepatic expansion of these dysfunctional effector CTL populations may be sufficient only to provide long-lasting low-level tissue damages but not to eliminate the virus, a function proposed to be related more to the high production of antiviral cytokines than to the cytolytic effect of CTLs (40).
As to the mechanisms by which the effector responses are kept suppressed in individuals chronically infected with HCV, we propose that a key role is played by IL-10–producing CD8+ TR cells. Indeed, the finding that the frequency of IL-10–producing CCR7–CD8+ LILs was inversely correlated with the total HAI score, whereas that of IFN-γ–producing CCR7–CD8+ LILs was instead directly correlated with the total HAI score, suggests a major role for HCV-specific CTLs producing IL-10 in controlling the chronic liver immunopathology mediated by those producing IFN-γ. This interpretation is supported by experiments demonstrating a strong suppressor function of IL-10–producing CD8+ LILs that was significantly reduced by neutralizing anti–IL-10. This finding suggests that IL-10–secreting virus-specific CD8+ T cells detected in HCV-infected livers by tetramer staining are instrumental in mediating suppression via IL-10 secretion. In addition, our data clearly indicate that the regulatory CD8+ LILs are antigen specific in the induction phase of the response but that they exert suppression in a non–antigen-specific manner via IL-10 in the effector phase (18–21, 38, 41–45).
This phenotype (IL-10+CD8+ LILs) resembles that of IL-10–producing CD8+ TR cells generated by human plasmacytoid dendritic cells (DC2) (41). Because inflamed livers contain a significant proportion of DC2 (our study in progress), it is tempting to hypothesize that they might be involved in the generation of HCV-specific CD8+ TR cells in vivo. In contrast, although our IL-10–producing CD8+CCR7– LILs were also CD27–CD28–, a phenotype typical of terminally differentiated cells (9, 46) (data not shown), they are unlikely to belong to the CD8+CD28– T suppressor cell subset that inhibits DCs from inducing T cell activation via direct cell contact (47). However, the finding that some CD8+ LILs exerted a suppressive function irrespective of IL-10 suggests that other soluble factors play a role in suppression. Studies by the authors of this article are in progress in order to determine whether additional mechanisms, humoral factors, or regulatory cells (such as CD4+ type 1 TR cells suppressing via IL-10 production or CD4+CD25+ TR cells mediating suppression via cell contact [18–21, 38, 42–45]) may intervene in controlling excessive anti-HCV immune responses. On the other hand, although intrahepatic tetramer+ LILs expressed high perforin levels, it is unlikely they modulate liver immunopathology through cytotoxic functions proposed to be important mechanisms of immunological homeostasis (48–50). Indeed, only IL-10–producing but not perforin+tetramer+ cells significantly correlated with a low HAI score. The regulatory effect mediated by the cytotoxic potential of these CD8+ T cells is most probably involved in the selective killing of virus-infected lymphocytes rather than being a generalized immunosuppression in vivo (48, 51).
In conclusion, we report evidence that HCV-specific CD8+ TR cells producing IL-10 may have a role in controlling the magnitude of immune responses by sustaining both a long-lasting virus/host symbiosis and a constant pool of memory cells that are deemed essential to provide waves of effector cells on demand. HCV is usually incompletely suppressed by CTLs in acutely infected individuals (1–11) because of its capacity to generate escape mutants (52, 53) or to exert immunosuppressive effects via certain viral proteins (11, 54–56). In addition, it has been recently proposed that at the peak of response, effector CTL populations undergo programmed contraction even if infection persists, in order to prevent the possibility of high frequencies of nonprotective CTLs that may be detrimental for the host (10, 57). Our data suggest that in cases when the virus avoids effector CTL responses during the early phases of infection, HCV-specific CD8+ TR cells may intervene in an attempt to minimize chronic pathological responses by effector CTLs. Effector CTLs, on the other hand, would be sufficient both to contain the infection and to maintain a stable number of memory cells. This equilibrium may establish a status of long-lasting low-level inflammation instrumental for the survival of both the microbial agent and the host. Understanding the role of regulatory cells in antiviral immunity may provide an important platform for the design of innovative strategies to re-engineer antiviral immune responses in persisting infections.
Acknowledgments
This work was supported by “Cofin-MIUR” projects 2002–2003 to V. Barnaba and 2003 to M.U. Mondelli; “FIRB-MIUR” projects 2002 to V. Barnaba; “Ministero della Sanità-Istituto Superiore di Sanità” (Progetti AIDS 2001 to V. Barnaba and Progetto Strategico 2000 to M.U. Mondelli and V. Barnaba); “Ministero della Sanità-Ricerca finalizzata HCV” 1999 and 2000 to V. Barnaba; Progetto Finalizzato CNR “Biotecnologie” to V. Barnaba; European Community contract QLK2-CT-2001-01167 to V. Barnaba; “Associazione Italiana per la Ricerca sul Cancro” (AIRC) 2001–2003 to V. Barnaba; “Fondazione Italiana Sclerosi Multipla” (FISM) 2000–2002 to V. Barnaba. Support was also provided by an unrestricted grant from Schering-Plough Italy to M.U. Mondelli.
Footnotes
Daniele Accapezzato and Vittorio Francavilla contributed equally to this work.
Nonstandard abbreviations used: alanine transaminase (ALT); central memory (CM); class I HLA–peptide tetrameric complex (tetramer); hepatitis C virus (HCV); histological activity index (HAI); human plasmacytoid dendritic cells (DC2); indodicarbocyanine (Cy5); liver-infiltrating lymphocyte (LIL); memory effector (ME); nonstructural protein 3 (NS3); phycoerythrin (PE); regulatory T (TR); tricolor (TC).
Conflict of interest: The authors have declared that no conflict of interest exists.
References
- 1.Lauer GM, Walker BD. Hepatitis C virus infection. N. Engl. J. Med. 2001;345:41–52. doi: 10.1056/NEJM200107053450107. [DOI] [PubMed] [Google Scholar]
- 2.Cooper S, et al. Analysis of a successful immune response against hepatitis C virus. Immunity. 1999;10:439–449. doi: 10.1016/s1074-7613(00)80044-8. [DOI] [PubMed] [Google Scholar]
- 3.Prezzi C, et al. Virus-specific CD8+ T cells with type 1 or type 2 cytokine profile are related to different disease activity in chronic hepatitis C virus infection. Eur. J. Immunol. 2001;31:894–906. doi: 10.1002/1521-4141(200103)31:3<894::aid-immu894>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 4.He XS, et al. Quantitative analysis of hepatitis C virus-specific CD8+ T cells in peripheral blood and liver using peptide-MHC tetramers. Proc. Natl. Acad. Sci. U. S. A. 1999;96:5692–5697. doi: 10.1073/pnas.96.10.5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lechner F, et al. Analysis of successful immune responses in persons infected with hepatitis C virus. J. Exp. Med. 2000;191:1499–1512. doi: 10.1084/jem.191.9.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thimme R, et al. Determinants of viral clearance and persistence during acute hepatitis C virus infection. J. Exp. Med. 2001;194:1395–1406. doi: 10.1084/jem.194.10.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gruener NH, et al. Sustained dysfunction of antiviral CD8+ T lymphocytes after infection with hepatitis C virus. J. Virol. 2001;75:5550–5558. doi: 10.1128/JVI.75.12.5550-5558.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Urbani S, et al. Virus-specific CD8+ lymphocytes share the same effector-memory phenotype but exhibit functional differences in acute hepatitis B and C. J. Virol. 2002;76:12423–12434. doi: 10.1128/JVI.76.24.12423-12434.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scognamiglio P, et al. Presence of effector CD8+ T cells in hepatitis C virus-exposed healthy seronegative donors. J. Immunol. 1999;162:6681–6689. [PubMed] [Google Scholar]
- 10.Francavilla V, et al. Subversion of effector CD8+ T cell differentiation in acute hepatitis C virus infection: exploring the immunological mechanisms. Eur. J. Immunol. 2004;34:427–437. doi: 10.1002/eji.200324539. [DOI] [PubMed] [Google Scholar]
- 11.Accapezzato D, et al. Subversion of effector CD8+ T cell differentiation in acute hepatitis C virus infection: the role of the virus. Eur. J. Immunol. 2004;34:438–446. doi: 10.1002/eji.200324540. [DOI] [PubMed] [Google Scholar]
- 12.Moskophidis D, Lechner F, Pircher H, Zinkernagel RM. Virus persistence in acutely infected immunocompetent mice by exhaustion of antiviral cytotoxic effector T cells. Nature. 1993;362:758–761. doi: 10.1038/362758a0. [DOI] [PubMed] [Google Scholar]
- 13.Zajac AJ, et al. Viral immune evasion due to persistence of activated T cells without effector function. J. Exp. Med. 1998;188:2205–2213. doi: 10.1084/jem.188.12.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wedemeyer H, et al. Impaired effector function of hepatitis C virus-specific CD8+ T cells in chronic hepatitis C virus infection. J. Immunol. 2002;169:3447–3458. doi: 10.4049/jimmunol.169.6.3447. [DOI] [PubMed] [Google Scholar]
- 15.Champagne P, et al. Skewed maturation of memory HIV-specific CD8 T lymphocytes. Nature. 2001;410:106–111. doi: 10.1038/35065118. [DOI] [PubMed] [Google Scholar]
- 16.Appay V, et al. Memory CD8+ T cells vary in differentiation phenotype in different persistent virus infections. Nat. Med. 2002;8:379–385. doi: 10.1038/nm0402-379. [DOI] [PubMed] [Google Scholar]
- 17.Grabowska AM, et al. Direct ex vivo comparison of the breadth and specificity of the T cells in the liver and peripheral blood of patients with chronic HCV infection. Eur. J. Immunol. 2001;31:2388–2394. doi: 10.1002/1521-4141(200108)31:8<2388::aid-immu2388>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 18.Maloy KJ, Powrie F. Regulatory T cells in the control of immune pathology. Nat. Immunol. 2001;2:816–822. doi: 10.1038/ni0901-816. [DOI] [PubMed] [Google Scholar]
- 19.Sakaguchi S. Regulatory T cells: key controllers of immunologic self-tolerance. Cell. 2000;101:455–458. doi: 10.1016/s0092-8674(00)80856-9. [DOI] [PubMed] [Google Scholar]
- 20.Shevach EM. CD4+ CD25+ suppressor T cells: more questions than answers. Nat. Rev. Immunol. 2002;2:389–400. doi: 10.1038/nri821. [DOI] [PubMed] [Google Scholar]
- 21.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 22.Lider O, Reshef T, Beraud E, Ben-Nun A, Cohen IR. Anti-idiotypic network induced by T cell vaccination against experimental autoimmune encephalomyelitis. Science. 1988;239:181–183. doi: 10.1126/science.2447648. [DOI] [PubMed] [Google Scholar]
- 23.Gaur A, Ruberti G, Haspel R, Mayer JP, Fathman CG. Requirement for CD8+ cells in T cell receptor peptide-induced clonal unresponsiveness. Science. 1993;259:91–94. doi: 10.1126/science.8418501. [DOI] [PubMed] [Google Scholar]
- 24.Koh DR, et al. Less mortality but more relapses in experimental allergic encephalomyelitis in CD8–/– mice. Science. 1992;256:1210–1213. doi: 10.1126/science.256.5060.1210. [DOI] [PubMed] [Google Scholar]
- 25.Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 26.Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ. Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology. 1994;19:1513–1520. [PubMed] [Google Scholar]
- 27.Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J. Exp. Med. 1994;179:1109–1118. doi: 10.1084/jem.179.4.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Propato A, et al. Apoptotic cells overexpress vinculin and induce vinculin-specific cytotoxic T-cell cross-priming. Nat. Med. 2001;7:807–813. doi: 10.1038/89930. [DOI] [PubMed] [Google Scholar]
- 29.Barnaba V, et al. Recognition of hepatitis B virus envelope proteins by liver-infiltrating T lymphocytes in chronic HBV infection. J. Immunol. 1989;143:2650–2655. [PubMed] [Google Scholar]
- 30.Sprent J, Surh CD. T cell memory. Annu. Rev. Immunol. 2002;20:551–579. doi: 10.1146/annurev.immunol.20.100101.151926. [DOI] [PubMed] [Google Scholar]
- 31.Wherry EJ, et al. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nat. Immunol. 2003;4:225–234. doi: 10.1038/ni889. [DOI] [PubMed] [Google Scholar]
- 32.Gett AV, Sallusto F, Lanzavecchia A, Geginat J. T cell fitness determined by signal strength. Nat. Immunol. 2003;4:355–360. doi: 10.1038/ni908. [DOI] [PubMed] [Google Scholar]
- 33.van Stipdonk MJ, et al. Dynamic programming of CD8+ T lymphocyte responses. Nat. Immunol. 2003;4:361–365. doi: 10.1038/ni912. [DOI] [PubMed] [Google Scholar]
- 34.Manjunath N, et al. Effector differentiation is not prerequisite for generation of memory cytotoxic T lymphocytes. J. Clin. Invest. 2001;108:871–878. doi: 10.1172/JCI13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weninger W, Crowley MA, Manjunath N, von Andrian UH. Migratory properties of naive, effector, and memory CD8+ T cells. J. Exp. Med. 2001;194:953–966. doi: 10.1084/jem.194.7.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reinhardt RL, Khoruts A, Merica R, Zell T, Jenkins MK. Visualizing the generation of memory CD4 T cells in the whole body. Nature. 2001;410:101–105. doi: 10.1038/35065111. [DOI] [PubMed] [Google Scholar]
- 37.Masopust D, Vezys V, Marzo AL, Lefrancois L. Preferential localization of effector memory cells in nonlymphoid tissue. Science. 2001;291:2413–2417. doi: 10.1126/science.1058867. [DOI] [PubMed] [Google Scholar]
- 38.Belkaid Y, Piccirillo CA, Mendez S, Shevach EM, Sacks DL. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature. 2002;420:502–507. doi: 10.1038/nature01152. [DOI] [PubMed] [Google Scholar]
- 39.Pradat P, et al. Predictive value of ALT levels for histologic findings in chronic hepatitis C: a European collaborative study. Hepatology. 2002;36:973–977. doi: 10.1053/jhep.2002.35530. [DOI] [PubMed] [Google Scholar]
- 40.Guidotti LG, Chisari FV. To kill or to cure: options in host defense against viral infection. Curr. Opin. Immunol. 1996;8:478–483. doi: 10.1016/s0952-7915(96)80034-3. [DOI] [PubMed] [Google Scholar]
- 41.Gilliet M, Liu YJ. Generation of human CD8 T regulatory cells by CD40 ligand-activated plasmacytoid dendritic cells. J. Exp. Med. 2002;195:695–704. doi: 10.1084/jem.20011603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Groux H, et al. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 1997;389:737–742. doi: 10.1038/39614. [DOI] [PubMed] [Google Scholar]
- 43.McGuirk P, McCann C, Mills KH. Pathogen-specific T regulatory 1 cells induced in the respiratory tract by a bacterial molecule that stimulates interleukin 10 production by dendritic cells: a novel strategy for evasion of protective T helper type 1 responses by Bordetella pertussis. J. Exp. Med. 2002;195:221–231. doi: 10.1084/jem.20011288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sing A, et al. Yersinia V-antigen exploits toll-like receptor 2 and CD14 for interleukin 10-mediated immunosuppression. J. Exp. Med. 2002;196:1017–1024. doi: 10.1084/jem.20020908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pasare C, Medzhitov R. Toll pathway-dependent blockade of CD4+CD25+ T cell-mediated suppression by dendritic cells. Science. 2003;299:1033–1036. doi: 10.1126/science.1078231. [DOI] [PubMed] [Google Scholar]
- 46.Paroli M, et al. Long-lasting memory-resting and memory-effector CD4+ T cells in human X-linked agammaglobulinemia. Blood. 2002;99:2131–2137. doi: 10.1182/blood.v99.6.2131. [DOI] [PubMed] [Google Scholar]
- 47.Chang CC, et al. Tolerization of dendritic cells by TS cells: the crucial role of inhibitory receptors ILT3 and ILT4. Nat. Immunol. 2002;3:237–243. doi: 10.1038/ni760. [DOI] [PubMed] [Google Scholar]
- 48.Barnaba V, Franco A, Alberti A, Benvenuto R, Balsano F. Selective killing of hepatitis B envelope antigen-specific B cells by class I-restricted, exogenous antigen-specific T lymphocytes. Nature. 1990;345:258–260. doi: 10.1038/345258a0. [DOI] [PubMed] [Google Scholar]
- 49.Franco A, et al. Transferrin receptor mediates uptake and presentation of hepatitis B envelope antigen by T lymphocytes. J. Exp. Med. 1992;175:1195–1205. doi: 10.1084/jem.175.5.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trambas CM, Griffiths GM. Delivering the kiss of death. Nat. Immunol. 2003;4:399–403. doi: 10.1038/ni0503-399. [DOI] [PubMed] [Google Scholar]
- 51.Planz O, Seiler P, Hengartner H, Zinkernagel RM. Specific cytotoxic T cells eliminate B cells producing virus-neutralizing antibodies. Nature. 1996;382:726–729. doi: 10.1038/382726a0. [DOI] [PubMed] [Google Scholar]
- 52.Farci P, et al. The outcome of acute hepatitis C predicted by the evolution of the viral quasispecies. Science. 2000;288:339–344. doi: 10.1126/science.288.5464.339. [DOI] [PubMed] [Google Scholar]
- 53.Erickson AL, et al. The outcome of hepatitis C virus infection is predicted by escape mutations in epitopes targeted by cytotoxic T lymphocytes. Immunity. 2001;15:883–895. doi: 10.1016/s1074-7613(01)00245-x. [DOI] [PubMed] [Google Scholar]
- 54.Kittlesen DJ, Chianese-Bullick KA, Yao ZQ, Braciale TJ, Hahn YS. Interaction between complement receptor gC1qR and hepatitis C virus core protein inhibits T-lymphocyte proliferation. J. Clin. Invest. 2000;106:1239–1249. doi: 10.1172/JCI10323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yao ZQ, Nguyen DT, Hiotellis AI, Hahn YS. Hepatitis C virus core protein inhibits human T lymphocyte responses by a complement-dependent regulatory pathway. J. Immunol. 2001;167:5264–5272. doi: 10.4049/jimmunol.167.9.5264. [DOI] [PubMed] [Google Scholar]
- 56.Crotta S, et al. Inhibition of natural killer cells through engagement of CD81 by the major hepatitis C virus envelope protein. J. Exp. Med. 2002;195:35–42. doi: 10.1084/jem.20011124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Badovinac VP, Porter BB, Harty JT. Programmed contraction of CD8+ T cells after infection. Nat. Immunol. 2002;3:619–626. doi: 10.1038/ni804. [DOI] [PubMed] [Google Scholar]