Abstract
Background:
Lumbar puncture (LP) is an essential procedure in the diagnosis and treatment of several critical situations. This procedure is routinely performed by palpating external landmarks to find the most appropriate inter-spinous space. In the current study, we compared surface landmark and ultrasound (US) guided LP in different aspects.
Materials and Methods:
This clinical trial study was conducted at the emergency department (ED) of a teaching hospital from March 2009 to March 2010. Eighty patients were allocated randomly in two equal groups. In first group, LP was performed by US-guided method and in the control group by palpation of external landmarks of spinal column. Pain score, number of attempts for successful dural penetration, numbers of traumatic LP, and procedure time were compared between two groups. The performance of US-guided LP was assessed with regard to body mass index (BMI) of patients too.
Results:
The mean of procedure time and pain scores were markedly higher in land mark group in comparison to US group (6.4 ± 1.2 and 7.4 ± 1.1 vs. 3.3 ± 1.2 and 4.4 ± 1.4 respectively). Number of attempts and number of traumatic LPs were significantly lower in US group too. In patients with different subgroups of BMI, US-guided LP showed better results and less complication when compared with surface landmark guided technique. All of these results were statistically significant.
Conclusion:
This study showed that US was able to find pertinent landmarks to facilitate the LP in patients admitted to ED and resulted in less pain and less time wasting. Moreover, patients who have high BMI may benefit more than others.
Keywords: Complication, emergency department, lumbar puncture, ultrasound
INTRODUCTION
Cerebrospinal puncture is an important procedure for diagnosis of some critical conditions such as subarachnoid hemorrhage and central nervous system infections. Also, therapeutic lumbar puncture (LP) is indicated in benign intracranial hypertension.[1,2]
LP is routinely carried out with the patient in the supine or lateral decubitus position using two techniques. Traditional technique uses Tuffier's line (an imaginary line connecting both iliac crests) to determine the level of the puncture site. This line crosses L4-L5 space. LP is usually performed in this space or 1 level over this, on the L3-L4 space.[3] Although this technique has high success rate it depends on personal expertise to find interspinous space. Inability to find the proper space is associated with repetitive painful attempts and high possibility of traumatized tap.[4]
An alternate method to surface landmark guided LP is ultrasound (US) guidance. For many years, US has been used to facilitate this procedure.[5] The use of US to find puncture site was first described 40 years ago in a medical journal in Russian language.[6]
In this technique vertebral column and surrounding structures can be shown. By placing US probe vertically and horizontally on spinous process of vertebras, subdural space would be seen as a dark space inside the spinal column. To find the most appropriate point for needle insertion, the examiner must be able to determine five structures by US: Spinous process, ligamentum flavum, dura, epidural, and subarachnoid spaces.[7,8]
Ten years later some anesthesiologists used US for better visualization of epidural and subarachnoid spaces for instillation of anesthetic drugs.[9] Also, in a series of studies, researchers showed that US could increase successful attempts and easiness of the procedure especially in obese patients.[10]
Interestingly, primary training of US-guided LP could improve expertise of physicians to identify pertinent landmarks to facilitate the procedure.[11,12] Although US-guided LP is not a new technique, the same studies in the field of emergency medicine are limited, especially in some residents with short training program of sonography.
The primary objective of this study was to compare the efficacy and feasibility of US-guided LP with traditional method in patients admitted to ED. We also assessed the performance of US-guided LP regarding to body mass index (BMI) of patients.
MATERIALS AND METHODS
Study design
This study was a prospective randomized clinical trial that was registered in Iranian Registry of Clinical Trials by code number of IRCT201008172337N4. It was carried out in the academic Emergency Department (ED) of Hazrat Rasoul Akram hospital, Tehran, Iran. The study was approved by the Local Ethics Committee.
Patients
We enrolled patients who admitted to our ED from March 2009 to March 2010 and were candidate for LP because of any medical problems [Diagram 1]. Exclusion criteria were age less than 18 or more than 60, mass in the brain, local infection at the puncture level, pregnant women, coagulopathy, previous spinal surgery, and those with unwillingness to participate in the study.
Diagram 1.
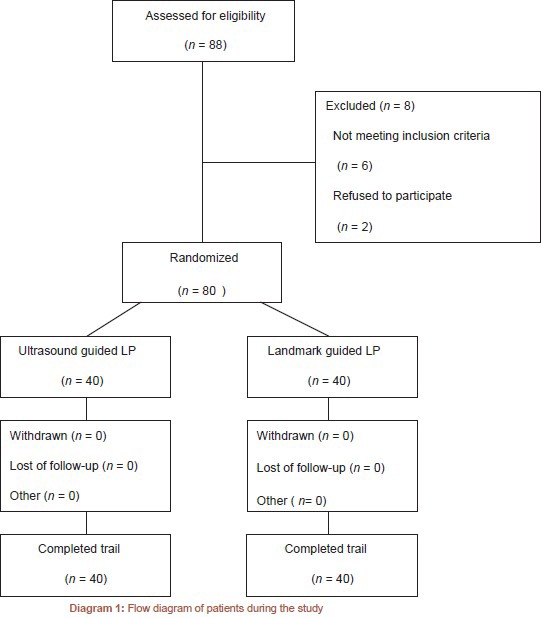
Flow diagram of patients during the study
Intervention
Patients were included to undergo LP using US guided or palpation of surface landmarks by simple randomization method. In the US group, insertion point determined at the L3-L4 inter-vertebral space by use of a 7.5-10 MHz linear probe. For deeper penetration in used. Sonographic landmarks were spinous processes, dura mater, ligamentum flavum, and epidural space [Figure 1].
Figure 1.
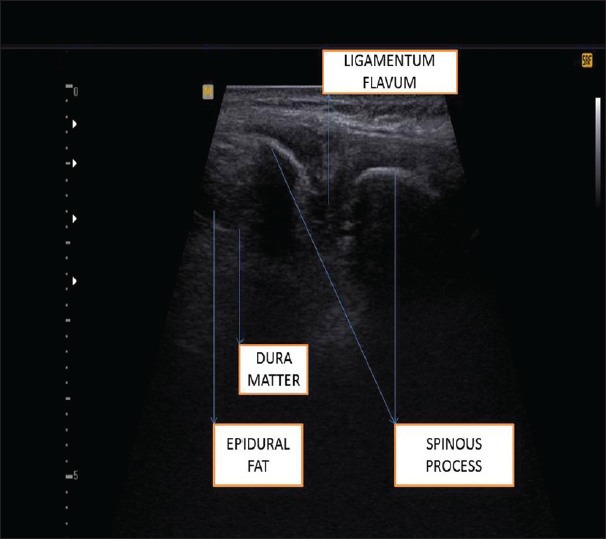
Ultrasound image of lumbar vertebra
In the control group, puncture level was determined by palpation of external landmarks, anterior superior iliac spines, and the spinous process of lumbar vertebrae L3, L4, and L5 which was performed by the study physicians. LPs were performed in a sterile manner with the patient in lateral decubitus fetal position.
Three PG-3 (post-graduate year) emergency medicine residents who underwent 2 h training on US to learn relevant spinal landmarks performed the procedures by supervision of a board-certified emergency medicine attending physician.
Before starting the study, all three residents performed some practice scans in healthy volunteers to ensure that they could capture the best possible image.
Measurements
Demographic characteristics, pain score using numerical rating scale from 0 to 10, number of attempts (needle insertion), procedure time (time to obtain the best scan possible until emersion of cerebrospinal fluid), and number of traumatic LP (needle-induced blood in the cerebrospinal fluid) were recorded by another observing emergency medicine resident. BMI was defined as the individual's body mass (in kilograms) divided by the square of his or her height (in meters). According to BMI, patients were categorized into three groups: Normal, less than 25; overweight, 25-29; obese, more than 29.
Sample size and statistic analysis
Sample size was estimated in 80 cases (40 cases in each group) by applying Altman's Nomogram. The procedure time was the variable that sample size was calculated based on it. The sample size was nearly similar to previous studies.[13,14,15] It was calculated considering the power of 80%, significance level of 0.05, and the standardized difference of 0.6. Informed consent was obtained from patients who were included in this study.
A statistical analysis was performed by means of the Mann–Whitney U-test, Student's t-test. Chi-squared test used when nominal data were compared between two groups. Data from BMI groups were compared using two-way analysis of variance and Bonferroni post hoc test. Two-way analysis of variance (ANOVA) for BMI and time of procedure, number of attempts, number of traumatic LP, and pain score were performed for each procedure subgroups. When the ANOVA was significant, a Bonferroni test was then used for multiple comparisons. All tests were two-tailed, and a P value of 0.05 was accepted as the limit of significance. Data analysis was performed using the Statistical Package for the Social Sciences (SPSS, Version 14, IBM, Chicago, Illinois, USA).
RESULTS
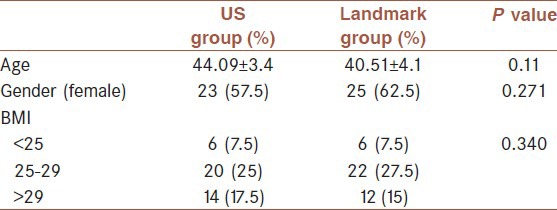
In this clinical trial, 80 eligible patients was allocated to two groups, each consisted of 40 cases. Among them, 48 patients (60%) were females. The patients’ mean of age was 42.3 ± 3.5 years old (44.09 ± 3.4 in US group and 40.51 ± 4.1 in landmark group). Patients categorized into three groups regarding BMI: 12 patients (15%) with BMI of less than 25, 42 patients (52.5%) with BMI of 25-29, and 26 patients (32.5%) with BMI more than 29. There was no statistically significant difference between two groups from the point of sex, mean of age, and BMI (P > 0.05). Details are showed in Table 1.
Table 1.
Characteristics of participants based on methods of lumbar puncture
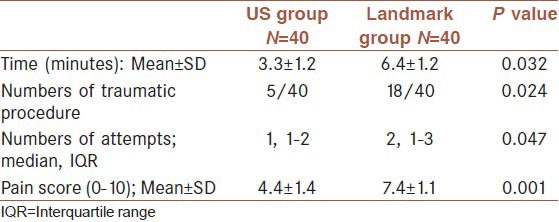
In all of the patients LP was performed successfully. Patients who underwent US-guided LP reported lower pain score (4.4 ± 1.4 vs. 7.4 ± 1.1, P = 0.001). Numbers of attempts and numbers of traumatic LP were less in US-guided group too (P = 0.047 and P = 0.024 respectively). US-guided LPs were performed faster and the mean of procedure times in the US group were 3.3 ± 1.2 min. In control group this time was 6.4 ± 1.2 min. (P = 0.032). Results are demonstrated in Table 2.
Table 2.
Comparison of different aspects of lumbar puncture regarding on ultrasound or traditional methods
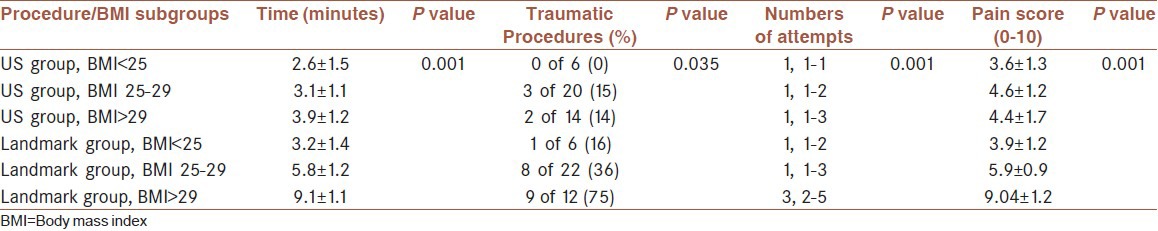
A two-way ANOVA model with interaction was used to evaluate the association of time, numbers of attempts, numbers of traumatic LP, and pain score with BMI subgroups and procedure group. Deviations differed between BMI subgroups [Table 3]. As shown, the durations of doing LP are markedly longer in patients with different BMI subgroups in traditional method (ANOVA, Bonferroni test, P = 0.000). Again participants with different BMI subgroups underwent less traumatic LP when US-guided method used (two-sided ANOVA, Bonferroni test, P = 0.035). Number of attempts and patient's pain scoring differed significantly in patients with different BMI subgroups and was significantly higher in traditional group (two-sided ANOVA, Bonferroni test, P = 0.001). Actually, US-guided LP improved all the factors assessed in our participants with different BMI subgroups and especially, BMI more than 29.
Table 3.
Two-way ANOVA model associations between procedure and body mass index subgroups, with time of procedure, number of attempts, procedure time, and pain score
DISCUSSION
LP is one of the important procedures in the EDs to obtain cerebrospinal fluid. The two different methods to find the insertion site are blind surface landmark guidance and US-guided techniques. Surface landmark guided LP has been shown to have high success rate in determining puncture site, but it may be difficult in some patients such as those with high BMI. Recently, US imaging of the spinal column has been proposed to facilitate identification of the pertinent landmarks for appropriate intervertebral space.[16,17]
Anesthesiologists have affirmed the use of US to find appropriate point of insertion for anesthetic catheters.[18,19] Coley et al.[20] showed that US can diagnose the cause of unsuccessful LP. Moreover, they concluded that US can help determine whether or not to try further. In this study all of the procedures in both groups were successfully carried out (zero failure rates). Indeed, there is no relation between selections of each method. But we found a marked reduction in time need for performing procedure in US group. Besides, number of attempts and pain score in US group was significantly lower than control group especially, in patients with BMI more than 29.
On 2004, Peterson et al.[21] concluded that use of US to guide LP had great benefit as a time-saving tool in ED. He showed that attending emergency physicians could easily perform US-guided LP when blind technique of needle insertion using surface landmark guidance was difficult or unsuccessful.
In the present study the number of traumatic LP in US group was significantly lower than control group (5 vs. 18). On 2007, a team of emergency physicians designed a study to compare the success rate and ease of performing LP in obese patients, with US-guided assistance or palpation of surface landmarks. They reported that using US could facilitate the procedure but there were no statistical differences in the number of attempts, patient comfort, traumatic LPs, or procedure time.[10] Because that was the only study that compared the rate of traumatic taps between two techniques, it seemed that further prospective randomized controlled studies should be planned to determine this probable benefit of US-guided LP.
In the current study, we found that patients with BMI more than 29 had significantly better outcome in terms of pain score, procedure time, number of attempts, and traumatic taps. Stiffler[15] compared the pain scores in patients with different BMI who underwent LP. He concluded that US-guided LP may be helpful in identifying pertinent landmarks in obese patients with BMI more than 30. These results have been reaffirmed in other studies.[11,14]
The current study evaluated the outcome of performing LP by PG-3 emergency medicine residents with two different methods. We recommend that future studies compare these methods in residents of other specialties such as neurology, internal medicine, pediatrics, and anesthesiology.
Notwithstanding the obvious benefits of US in determining proper insertion site in anesthetic blocks, there are few studies about the same profits for LP in EDs, so further studies in this area are needed.
CONCLUSION
The current study showed that US-guided LP has better results in comparison with surface landmark guided method. These benefits are more apparent in patients who had BMI more than 29.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mintegi S, Benito J, Astobiza E, Capapé S, Gomez B, Eguireun A. Well appearing young infants with fever without known source in the emergency department: Are lumbar punctures always necessary? Eur J Emerg Med. 2010;17:167–9. doi: 10.1097/MEJ.0b013e3283307af9. [DOI] [PubMed] [Google Scholar]
- 2.Delerme S, Castro S, Viallon A, Boutoille D, Bendahou M, Riou B, et al. Meningitis in elderly patients. Eur J Emerg Med. 2009;16:273–6. doi: 10.1097/MEJ.0b013e3283101866. [DOI] [PubMed] [Google Scholar]
- 3.Locks Gde F, Almeida MC, Pereira AA. Use of the ultrasound to determine the level of lumbar puncture in pregnant women. Rev Bras Anestesiol. 2010;60:13–9. doi: 10.1016/s0034-7094(10)70002-7. [DOI] [PubMed] [Google Scholar]
- 4.Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: Palpation versus ultrasound. Anesth Analg. 2008;106:538–40. doi: 10.1213/ane.0b013e31816069d9. table of contents. [DOI] [PubMed] [Google Scholar]
- 5.Ferre RM, Sweeney TW. Emergency physicians can easily obtain ultrasound images of anatomical landmarks relevant to lumbar puncture. Am J Emerg Med. 2007;25:291–6. doi: 10.1016/j.ajem.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Bogin IN, Stulin ID. Application of the method of 2-dimensional echospondylography for determining landmarks in lumbar punctures. Zh Nevropatol Psikhiatr Im S S Korsakova. 1971;71:1810–1. [PubMed] [Google Scholar]
- 7.Kil HK, Cho JE, Kim WO, Koo BN, Han SW, Kim JY. Prepuncture ultrasound-measured distance: An accurate reflection of epidural depth in infants and small children. Reg Anesth Pain Med. 2007;32:102–6. doi: 10.1016/j.rapm.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Kim SH, Lee KH, Yoon KB, Park WY, Yoon DM. Sonographic estimation of needle depth for cervical epidural blocks. Anesth Analg. 2008;106:1542–7. doi: 10.1213/ane.0b013e318168b6a8. table of contents. [DOI] [PubMed] [Google Scholar]
- 9.Grau T, Leipold RW, Conradi R, Martin E. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand. 2001;45:766–71. doi: 10.1034/j.1399-6576.2001.045006766.x. [DOI] [PubMed] [Google Scholar]
- 10.Nomura JT, Leech SJ, Shenbagamurthi S, Sierzenski PR, O’Connor RE, Bollinger M, et al. A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med. 2007;26:1341–8. doi: 10.7863/jum.2007.26.10.1341. [DOI] [PubMed] [Google Scholar]
- 11.Kawaguchi R, Yamauch M, Sugino S, Tsukigase N, Omote K, Namiki A. Two cases of epidural anesthesia using ultrasound imaging. Masui. 2007;56:702–5. [PubMed] [Google Scholar]
- 12.Carley SD. Towards evidence based emergency medicine: Best BETs from the manchester royal infirmary. Emerg Med J. 2007;24:492. doi: 10.1136/emj.2004.021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arzola C, Davies S, Rofaeel A, Carvalho JC. Ultrasound using the transverse approach to the lumbar spine provides reliable landmarks for labor epidurals. Anesth Analg. 2007;104:1188–92. doi: 10.1213/01.ane.0000250912.66057.41. tables of contents. [DOI] [PubMed] [Google Scholar]
- 14.Balki M, Lee Y, Halpern S, Carvalho JC. Ultrasound imaging of the lumbar spine in the transverse plane: The correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg. 2009;108:1876–81. doi: 10.1213/ane.0b013e3181a323f6. [DOI] [PubMed] [Google Scholar]
- 15.Stiffler KA, Jwayyed S, Wilber ST, Robinson A. The use of ultrasound to identify pertinent landmarks for lumbar puncture. Am J Emerg Med. 2007;25:331–4. doi: 10.1016/j.ajem.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Majd SA, Pourfarzam S, Ghasemi H, Yarmohammadi ME, Davati A, Jaberian M. Evaluation of pre lumbar puncture position on post lumbar puncture headache. J Res Med Sci. 2011;16:282–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Grau T, Leipold RW, Horter J, Conradi R, Martin E, Motsch J. The lumbar epidural space in pregnancy: Visualization by ultrasonography. Br J Anaesth. 2001;86:798–804. doi: 10.1093/bja/86.6.798. [DOI] [PubMed] [Google Scholar]
- 18.Furness G, Reilly MP, Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002;57:277–80. doi: 10.1046/j.1365-2044.2002.2403_4.x. [DOI] [PubMed] [Google Scholar]
- 19.Schlotterbeck H, Schaeffer R, Dow WA, Touret Y, Bailey S, Diemunsch P. Ultrasonographic control of the puncture level for lumbar neuraxial block in obstetric anaesthesia. Br J Anaesth. 2008;100:230–4. doi: 10.1093/bja/aem371. [DOI] [PubMed] [Google Scholar]
- 20.Coley BD, Shiels WE, 2nd, Hogan MJ. Diagnostic and interventional ultrasonography in neonatal and infant lumbar puncture. Pediatr Radiol. 2001;31:399–402. doi: 10.1007/s002470100453. [DOI] [PubMed] [Google Scholar]
- 21.Peterson MA, Abele J. Bedside ultrasound for difficult lumbar puncture. J Emerg Med. 2005;28:197–200. doi: 10.1016/j.jemermed.2004.09.008. [DOI] [PubMed] [Google Scholar]


