Abstract
Background:
To assess the status of occupational hazards and their prevention among the practicing dentists in Chandigarh city, India.
Materials and Methods:
A closed-ended questionnaire was prepared to record demographic status, types of occupational hazards encountered, and status of measures used for their prevention. A total 113 out of 130 dentists completed the questionnaire and the response rate was 86.9%.
Frequency tables were prepared and coefficient of correlation was computed to check correlation between different variables. Statistical significance was set at P < 0.05.
Results:
The most common occupational hazard reported was injury from “sharps” (77%), out of which needle prick injury was the most frequent. Of the other occupational problems job related stress (43.3%), musculoskeletal problems (39.8%), and allergies (23.8%) from things used in dental clinics were most common. A reasonably high percentage of dentists were immunized against hepatitis-B virus (88.4%) and were following proper infection control measures and hospital waste disposal methods. Very few dentists were following the correct method of disposal of excess amalgam (11%) and measurement of radiation exposure (27.5%) within their clinic. Most of them (90.2%) were satisfied with their current working hours and job.
Conclusion:
Prevalence of occupational hazards among the studied group was high and certain preventive measures were not being followed properly. Therefore, there is a need to improve the knowledge of dentists regarding these hazards and their prevention.
Keywords: Chandigarh, dentists, India, musculoskeletal problems, needle prick injury, occupational hazards, questionnaire
INTRODUCTION
In carrying out their professional work, dentists are exposed to a number of occupational hazards. These cause the appearance of various ailments specific to the profession, which develop and intensify with years. In many cases they result in diseases and disease complexes, some of which are regarded as occupational illnesses.[1]
These hazards can be broadly categorized as: Physical, chemical, biological, mechanical and psychological. Physical and mechanical hazards include eye injuries occurring from projectiles, cuts from sharp instruments, or puncture wounds from needles or other sharps. Such injuries can result in the transmission of serious infectious diseases to the dental worker. Harmful radiation like Non-ionizing radiation (visible and UV light) and ionizing radiation (X-rays) can cause damage to various body cells. Noise and vibration from the hand-piece can lead to hearing problems. Musculoskeletal problems like wrist ache, lower backache, and neck ache can occur due to the need to work in specific working positions using a continuous repetitive motion. Chemical hazards can be Inorganic (mercury toxicity), organic (solvents, resins, gases), caustic (formaldehyde, hydrogen peroxide) and Latex glove allergy (contact dermatitis). Biological hazards can occur due to Allergens of biological origin, infections, dental material toxicity, and cross contamination. Lastly, psychological problems can arise due to stress/excess work load, lack of job satisfaction/insecurity, professional burnout, and medico-legal problems.[1]
Therefore, there is a need to educate and make the dentists aware of these hazards and the methods of their prevention. Before carrying out such an educational program we must have a baseline data of the prevalence and awareness among the study group regarding the topic. Majority of studies on occupational hazards among dentists are conducted in the developed world[2,3,4,5,6,7,8,9,10,11] however, the minimal data is available from the developing countries. Hence, this study was aimed at finding the status of occupational hazards among dentists working in private clinics in Chandigarh city. The other objective of the study was to know whether the dentists were adopting proper measures for their prevention.
MATERIALS AND METHODS
The present study was conducted among the dentists practicing in private clinics in Chandigarh city. The dentist population ratio of Chandigarh is 1:3000.[12] Since, the data on the total number of registered dental clinics were not available, it was decided to cover maximum number of dental clinics in the survey. In total 130 dentists were requested to fill up the questionnaire, out of which 113 returned the filled forms. The response rate was 86.9%. Collections of data were carried out over 2 months’ time period. Ethical clearance for the study was obtained by institutional ethical committee. Verbal as well as written informed consent was obtained from the study participants.
A 22 questions closed-ended questionnaire was prepared to assess the occurrence of occupational hazards and the necessary steps taken for their prevention. Subjects were questioned about their age, gender, qualification, years of practice, daily working hours, and average number of patients attended in a day. Further, questions assessed whether they have suffered from any of the various occupational hazards like injury from sharps and what precaution they had taken after the incident. Other hazards included were Burns, Hearing problems, musculoskeletal problems (back pain, cervical spondylitis, and carpel tunnel syndrome), allergies (allergy from dental materials like acrylic, latex etc.), and Stress and eye injuries.
The next part of questionnaire included questions on administration of hepatitis B vaccination and its booster dose, and the following of various cross infection control measures in the clinic. Next, questions were asked on use of amalgam in the clinic and its method of disposal, use of X-ray and measures available in the clinic for protection of staff from it. Lastly, subjects were asked questions related to their physical activity, job satisfaction, stress and its management through vacation, hobbies etc.
The questionnaire was pretested on 20 dental practitioners before the main survey. Some questions were modified according to the feedback received from the subjects. Data was analyzed using frequency tables to display the responses of the dental staff. SPSS software version-17 was used for analysis and level of significance was set at P < 0.05.
RESULTS
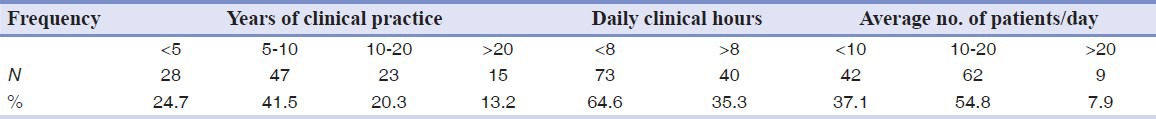
Total 113 dentists completed the questionnaire, out of which 68 were males and 45 females. Mean age of participants was 38.2 years (SD = 38.2, range – 24-70 years). 55 were graduates only whereas the rest 58 had carried out post-graduation as well. Table 1 depicts years of clinical practice, number of clinical hours in a day and average number of patients attended by the participants. Majority of participants were having a practice of 5-10 years (41.2%), were working less than 8 h in a day (64.6%) and were attending between 10 and 20 patients daily on an average (54.8%).
Table 1.
Distribution of participants according to years of clinical practice, number of clinical hours in a day and average number of patients attended daily
Out of the total 113 dentists, 88 (77%) responded positively when asked about history of injury from sharps. Figure 1 demonstrates the detail of when asked about the types of injury suffered by participants in clinics, maximum injury was reported from needle prick (49.5%), followed by an explorer or probe (42.4%) and 39.8% reported injury by files used for root canal treatment [Figure 1]. 59.9% of affected participants received post-exposure prophylaxis after the injury whereas the rest 40% did not undergo any such prophylactic treatment. Prevalence of other occupational hazards was also significantly high as 39.8% participants complained of one or more musculoskeletal problems and 23.8% reported allergies to one or more dental materials or gloves, however, it was the stress related to their job, which was affecting 43.3% of them. Hearing problem was affecting 7%, 9% had suffered burn injury and 4% reported eye injuries [Figure 2].
Figure 1.
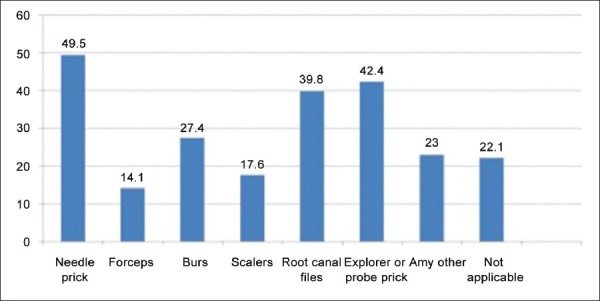
Distribution of participants according to types of injury from sharps
Figure 2.
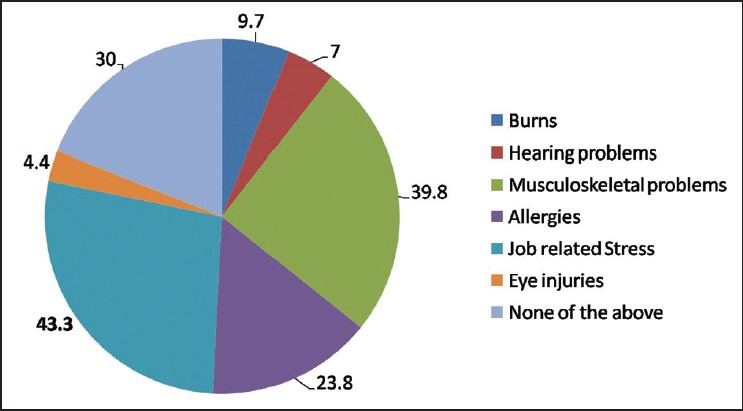
Prevalence of other occupational hazards
When questions were asked on hepatitis — B immunization, 88.4% had got the vaccination done and 70.7% also got the booster dose administered [Table 2]. Proper infection control measures that includes equipment for “personal protective equipment” and “post-exposure management” was present according to 73.4% participants in their clinics, a safe system for health-care waste management and disposal was adopted by 96.4% dentists but only 39.8% were sure whether they were following all the Occupational Safety and Health Administration regulations in their clinic [Table 3]. About 60 (53%) dentists were carrying out amalgam restorations in their clinic, among them, 66% were storing waste/excess amalgam in water and 21% were throwing them in the dustbin and only 11% were storing it in a radiographic fixer [Figure 3].
Table 2.
Measures taken for protection from hepatitis — B virus
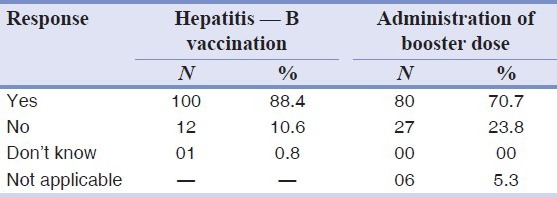
Table 3.
Measures for proper infection control in dental clinic
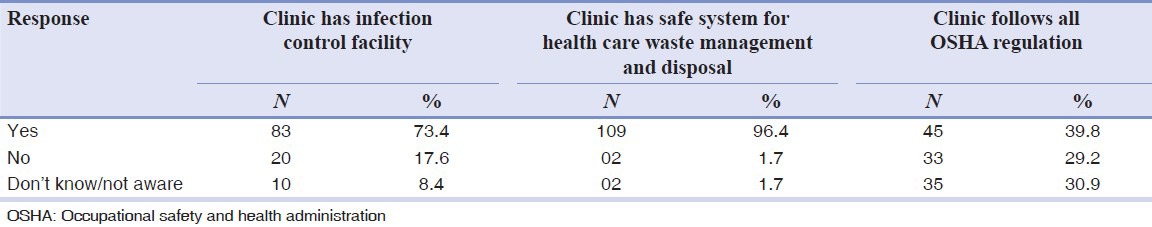
Figure 3.
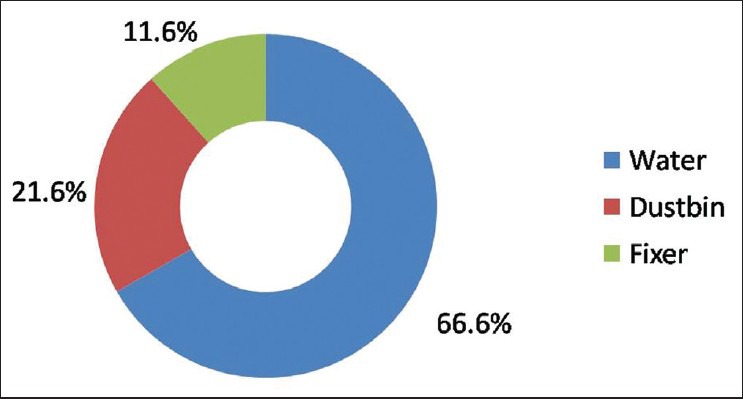
Methods of storage of excess amalgam in the clinic
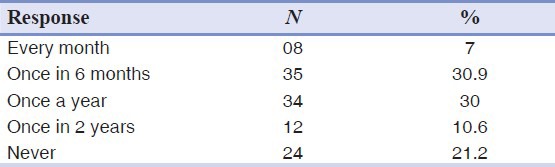
Most of the participant's dental clinics were having X-ray facility (80.5%), but majority of among them were not using any type of devices to measure radiation exposure (72.5%). However, 85.7% were using an appropriate protection barrier while taking the radiograph, as shown in Table 4. When asked how often do you take leave/holidays from your job, 30.9% were taking it once every 6 months followed by another 30% who had once in a year frequency [Table 5]. Regular participation in sports or any other physical activity was a life-style feature of 69.9% of the participants. Finally, when a question was put whether you are satisfied with your job and working hours, a staggering majority of 90.2% gave a positive response. No correlation was found between prevalence of occupational hazards with gender of participants, number of years of practice or with number of patients attended daily (P > 0.05).
Table 4.
Protection against X-ray radiation
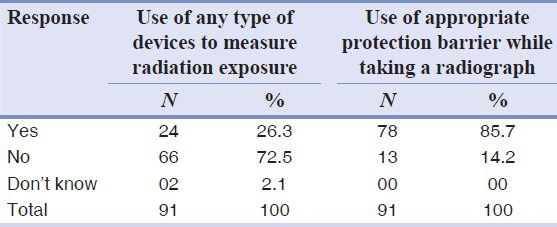
Table 5.
Frequency of taking leave/holidays from job
DISCUSSION
This questionnaire based survey was conducted on private dental practitioners in Chandigarh city, India to assess the status of occupational hazards and their prevention among them. Total 113 dentists completed the questionnaire; response rate was 86.9%, which can be considered satisfactory. Most common reason for not participating in the study (n = 17) was busy schedule of the dentists in their clinics. Mean age of participants was 38.2 years (range — 24-70 years). Gender division showed that there were 68 males and 45 females. Qualification of participants showed 55 graduates and 58 post-graduates, this clearly indicates that different categories of dentists were represented appropriately in this study.
Injury from “sharps” is a major concern for the profession as it is a source of transmission of various infectious agents like different types of hepatitis viruses and HIV. In our study 77% dentists gave a positive history of such injuries, which is higher compared to study done by 27.7% in Queensland, Australia,[2] 36% among the Nigerian dentists[3] and 50% among dentists in Thailand.[4] Most common cause of such injury was from the needle (49.5%), which is in agreement with other studies conducted in different countries.[2,3,4,5,6]
Stress due to job/business is present in all professions and dentistry is no exception to it as 43.3% of our study participants were a victim of this. These self-reported values are considerably less when compared to studies carried out by Leggat et al. in Thailand,[6] Kay and Lowe[7] and Myers and Myers[13] in England and Gijbels et al.[8] in Belgium, they reported prevalence of 96.1%, 86%, 60% and 54% respectively. The main reasons for stress among dentists are related to working hours, job satisfaction, staff/patient interactions and medico legal problems.
Musculoskeletal disorders (MSD) like lower backache, wrist ache, and neck, and shoulder pain are common hazards of our profession. A total of 39.8% participants complain one or more MSD in this study. Other studies reported prevalence of 59-87%.[4,9,14] MSD is one of the major factor for premature retirement among dentists along with stress and cardiovascular disease.[15] Around quarter (23.8%) of the dentists were suffering from allergies due to dental materials, gloves etc. This percentage is quite similar to as reported in the studies by Chowanadisai et al. (22%),[4] Leggat and Smith (29%)[10] and Gijbels et al. (22.5%).[8] Immunization against hepatitis — B virus was received by 88.4% of participants and 70% had even got the booster dose administered, these figures similar to reported in other parts of the world.[5] Protection from hepatitis – B virus is essential for the dentists as they are exposed to a variety of body fluids of patients. Majority of dentists were following proper infection control (73.4%) and hospital waste disposal management (96.4%) in the their clinics, other authors have also reported the same,[5,11] but these values are self-reported and so can have some degree of bias when responding to such questions as most dentists are aware that they have to follow the above procedures.
By far the most dangerous material used in dentistry is mercury in dental amalgam which poses a serious threat to dental as well as general population if not handled and disposed-off properly. In our study, 66% dentists who were carrying out amalgam restoration were storing excess amalgam in water; these figures are more than as reported by Leggat in Thailand.[6] Only 11% were storing excess amalgam in radiographic fixer, which is considered to be the proper method.[16]
Most of the participants (85.7%) were using an appropriate protection barrier while taking radiographs, but 72.5% were not using any devices to measure the amount of radiation exposure, this can be a cause of concern especially, considering that 38% of them were having conical positioning device in their X-ray machine. Overall, majority of them were satisfied with their job and working hours and were taking regular breaks from their routine. 70% of them were also involved in some kind of physical activity like sports; this percentage is comparable to a study done by Kay on UK dentists.[7]
As with any questionnaire study, the present study has limitations especially of false reporting as dentists are aware of what corrective measures are required to be taken for prevention of various occupational hazards which they must have studied in dental school. No physical inspection was carried out of the clinics by the investigators so such false reporting is possible. Although, pilot study was conducted to check feasibility of the study and to do necessary modifications of questions, validity, and reliability of questionnaire was not assessed statistically.
CONCLUSION
As the results of the present study demonstrates that there is a need to make dental practitioners of Chandigarh more aware about the prevention of different occupational hazards in dentistry. Areas, which require special attentions are radiation protection, proper storage of excess amalgam, post-exposure prophylaxis after “sharps” injury and stress management. This can be carried out by carrying various informative programs like continuing dental education programs, seminars, and workshops on prevention of occupational hazards in the region. Future research can include medical examination of the participants as well as physical examination to verify the answers provided by dentists.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Szymańska J. Occupational hazards of dentistry. Ann Agric Environ Med. 1999;6:13–9. [PubMed] [Google Scholar]
- 2.Leggat PA, Smith DR. Prevalence of percutaneous exposure incidents amongst dentists in Queensland. Aust Dent J. 2006;51:158–61. doi: 10.1111/j.1834-7819.2006.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 3.Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134–52. [PubMed] [Google Scholar]
- 4.Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U, Leggat PA. Occupational health problems of dentists in southern Thailand. Int Dent J. 2000;50:36–40. doi: 10.1111/j.1875-595x.2000.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 5.Yengopal V, Naidoo S, Chikte UM. Infection control among dentists in private practice in Durban. SADJ. 2001;56:580–4. [PubMed] [Google Scholar]
- 6.Leggat PA, Chowanadisai S, Kedjarune U, Kukiattrakoon B, Yapong B. Health of dentists in southern Thailand. Int Dent J. 2001;51:348–52. doi: 10.1002/j.1875-595x.2001.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 7.Kay EJ, Lowe JC. A survey of stress levels, self-perceived health and health-related behaviours of UK dental practitioners in 2005. Br Dent J. 2008;204:E19. doi: 10.1038/sj.bdj.2008.490. [DOI] [PubMed] [Google Scholar]
- 8.Gijbels F, Jacobs R, Princen K, Nackaerts O, Debruyne F. Potential occupational health problems for dentists in Flanders, Belgium. Clin Oral Investig. 2006;10:8–16. doi: 10.1007/s00784-005-0003-6. [DOI] [PubMed] [Google Scholar]
- 9.Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J. 2006;51:324–7. doi: 10.1111/j.1834-7819.2006.tb00451.x. [DOI] [PubMed] [Google Scholar]
- 10.Leggat PA, Smith DR. Prevalence of hand dermatoses related to latex exposure amongst dentists in Queensland, Australia. Int Dent J. 2006;56:154–8. doi: 10.1111/j.1875-595x.2006.tb00088.x. [DOI] [PubMed] [Google Scholar]
- 11.Leggat PA, Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U. Occupational hygiene practices of dentists in southern Thailand. Int Dent J. 2001;51:11–6. doi: 10.1002/j.1875-595x.2001.tb00811.x. [DOI] [PubMed] [Google Scholar]
- 12.Goyal A, Gauba K, Chawla HS, Kaur M, Kapur A. Epidemiology of dental caries in Chandigarh school children and trends over the last 25 years. J Indian Soc Pedod Prev Dent. 2007;25:115–8. doi: 10.4103/0970-4388.36559. [DOI] [PubMed] [Google Scholar]
- 13.Myers HL, Myers LB. ’It's difficult being a dentist’: Stress and health in the general dental practitioner. Br Dent J. 2004;197:89–93. doi: 10.1038/sj.bdj.4811476. [DOI] [PubMed] [Google Scholar]
- 14.Ayers KM, Thomson WM, Newton JT, Morgaine KC, Rich AM. Self-reported occupational health of general dental practitioners. Occup Med (Lond) 2009;59:142–8. doi: 10.1093/occmed/kqp004. [DOI] [PubMed] [Google Scholar]
- 15.Burke FJ, Main JR, Freeman R. The practice of dentistry: An assessment of reasons for premature retirement. Br Dent J. 1997;182:250–4. doi: 10.1038/sj.bdj.4809361. [DOI] [PubMed] [Google Scholar]
- 16.Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: A review. Ind Health. 2007;45:611–21. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]


