Abstract
Background:
Pain and dysfunction of the tempromandibular joint (TMJ) are major clinical problems, especially, in arthritis. The aim of this study was to compare the effect of intra-articular (IA) versus intra-peritoneal (IP) injection of betamethasone long acting on TMJ arthritis in rat.
Materials and Methods:
In this experimental study, an inflammation in the left TMJ of 29 rats was induced by injection of complete Freund's adjuvant. After 1 week, rats were divided into 5 groups: Group A: Rats of this group were not treated (n = 5); groups B, C: Rats were injected with a single dose of ½ mg/kg betamethasone L.A IA (n = 6); groups D, E: Rats received a single dose of ½ mg/kg betamethasone L.A IP (n = 6).
Rats in groups B and D after 1 week, and in groups C, E and A, at 4 weeks after drug injection were sacrificed. Severity of inflammation was scored from 1 to 11 according to synovial hyperplasia, vascularity, fibrin deposits, and synovial adhesion. Results were analyzed by using Kruskal-Wallis and Mann-Whitney (P < 0/05 was considered significant).
Results:
Significant differences were existed between groups B, D (P = 0/004) and groups C, E (P = 0/002). The least severity of Inflammation and also evidence of resorbtion in condylar head was seen in group C.
Conclusion:
The best therapeutic response was seen with IA injection of betamethasone L.A in comparison with IP injection.
Keywords: Betamethasone L.A, histological assessment, intra-articular, intra-peritoneal, tempromandibular joint
INTRODUCTION
Arthritis is one of the most common diseases, which involves tempromandibular joints (TMJs).[1] Pain and dysfunction of the TMJ are major clinical problems, especially in arthritis.[2] up to 75% of patients with the rheumatoid arthritis (RA) have TMJ involvement[3] symptoms often noted include pain, tenderness and limitation of mandibular movement. These symptoms are characterized by periods of exacerbation and remission.[4] pharmacologic therapy is one of the adjunective treatment in TMJ inflammation, which is used in combination with other methods.[5] intra-articular corticosteroid injection (IACI) is a very popular procedure, the main beneficial effect of IACI is pain relief.[6] IA injection of corticosteroid is used to reduce the persistent pain, but this method requires multiple injections that increase the risk of complications.[7] The use of IACI is controversial, they should be used only in patients with acute symptoms that don’t respond to conservative treatments.[8] The duration of response is different according to the type of steroids, dose, subtype of arthritis, and accuracy of injection.[6] Sub dermal injection of a dissoluble and long-effect corticosteroid has been suggested as an alternative for IA injection. Some of the considerable advantages of this method are imposing fewer traumas on joint structure and exact and clear place for the injection.[9] several studies indicated that IA injection of corticosteroids have beneficial effects on TMJ,[10,11,12,13] but there is limited research in field comparison between local and systemic effects of corticosteroids in TMJ. In this study, we aimed to investigate IA (local) versus intra-peritoneal (IP) (systemic) injection betamethasone L.A on TMJ arthritis in rat.
MATERIALS AND METHODS
This experimental animal study was approved according to the guidelines of the ethics committee of Isfahan University of medical sciences. Before beginning the study, a pilot study using four rats was performed to confirm the stages and existence of inflammation from histological aspect. In main study 29 male Wister rats, weighted 300-400 g was used. At first mixture of ketamin 10% (Ulfasan, Amsterdam, Netherlands) and acepromazine 1% (Ulfasan, Amsterdam, Netherlands) was injected intramuscular to create generalized anesthesia. After shaving the area over the left TMJ one volume 50 ml[14] of complete Freund's adjuvant (CFA) (Biojan, Mashhad, Iran) was injected into the joint. CFA is composed of dead and dried mycobacterium tuberculosis in oil[15] CFA is used to create artificial chronic inflammation; according to the other studies the inflammation that caused by CFA, conforms RA[16,17] the majority of inflammation was observed 1 week after CFA injection[18] rats were divided randomly into five groups, 1 week after CFA injection: Group A (control): Rats of this group were not treated (n = 5) groups B, C (n = 6 in each group): The rats were injected with a single dose of ½ mg/kg betamethasone L.A (Exir, Borujerd, Iran) IA into left TMJ and also saline was injected into the other Joint. Groups D, E (n = 6 in each group): Rats were received a single dose of ½ mg/kg betamethasone L.A (Exir, Borujerd, Iran) with using of IP injection method (for evaluation systemic effect).
Technique of IA injection
The joint felt 5-10 mm posterior to the lateral canthus of the eye while mandible was manipulated to provide movement of the condyle for a further positive identification of the Joint. The needle was inserted from a posterior superior direction until the mandibular condyle was felt. Needle was inserted inside the inferior joint cavity, and the drug injected slowly.[10]
Technique IP injection
Rats were held with their abdominal exposed in the left hand and the needle was inserted deeply into the abdominal cavity in the lower right quadrant. The needle angle was 15-20° and inserted approximately 5 mm.[10] Control rats were sacrificed at 4 week, after induction maximum inflammation. While groups B and D were sacrificed 1 week after betamethasone L.A injection and groups C, E were sacrificed 4 week after drug injection. The animals sacrificed with intramuscular injection trought an overdose of ketamine 10% (Ulfasan, Amsterdam, Netherlands). The head was separated and fixed for 48 h in formalins then processed to provide 4 μm thick section of the joint and sections were stained with H and E for histological examination. Samples were scored by a pathologist according to Muto et al.[19] and Suzuki et al.[20] methods. Synovial lining hyperplasia was graded from 0 to 2:
Grade 0: Indicated the presence of 1 to 3 layers of cells.
Grade 1: Indicated the presence of 4 to 6 layers of cells.
Grade 2: Showed 7 or more layers of cells.
Dilated vasculature was graded from 0 to 3
Grade 0: indicated that dilation was not present.
Grade 1: Indicated the presence of dilated blood vessels that involved less than 1/3rd of the synovial membrane length.
Grade 2: Involved 1/3rd to 2/3rd of the synovial membrane length.
Grade 3: Involved more than 2/3rd of the synovial membrane length.
Fibrin deposits and synovial adhesion were graded from 0 to 3 (similar to the dilated vasculature). The severity of inflammation was graded from 1 to 11 by adding the scores of the histological criteria then the data were collected and analyzed. Non-parametric analysis of Kruskal-Wallis was used to compare the groups with other. Mann-Whiteney test used to compare groups B, C and D, E with each other. P values less than 0/05 was considered to be significant.
RESULTS
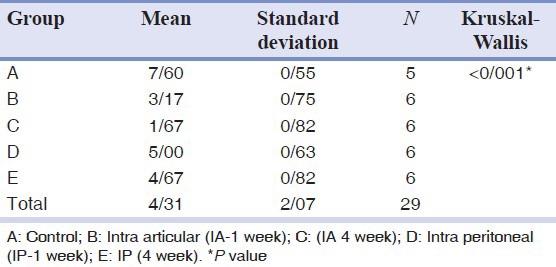
Mean values and standard deviations in 5 groups are shown in Table 1. According to Table 1 there were significant differences between 5 groups (P < 0/001).
Table 1.
Comparison the mean±standard deviations between the five groups
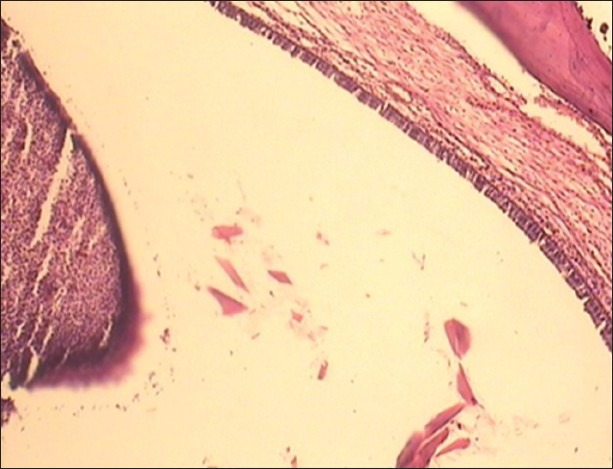
Inflammation is significantly lower in group C when compared with other groups. Also, evidence of resorption in condylar head was seen in group C [Figure 1].
Figure 1.
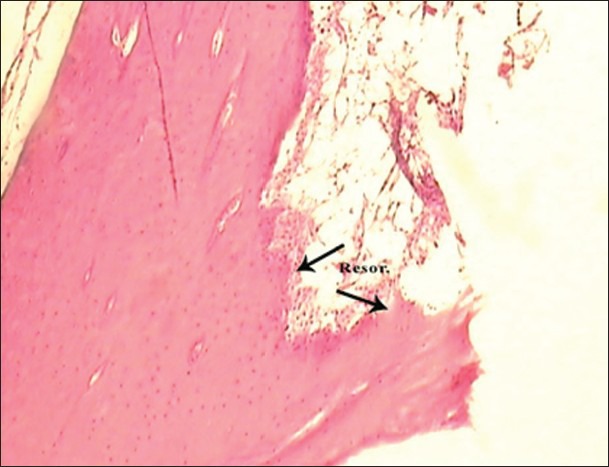
Photomicrograph of the group (C) 4 weeks after articular injection of betamethasone LA showing evidence for bone resorption of the condyle. Note active osteoclastic activity in the border of the condyle (H and E, ×100)
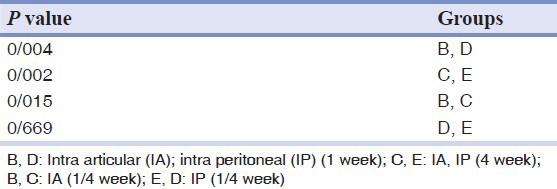
Mann-Whiteney test was used to find out which two groups have a significant statistical difference. All groups have significant statistical difference expect the groups D, E [Table 2].
Table 2.
Comparison groups based on P value
DISCUSSION
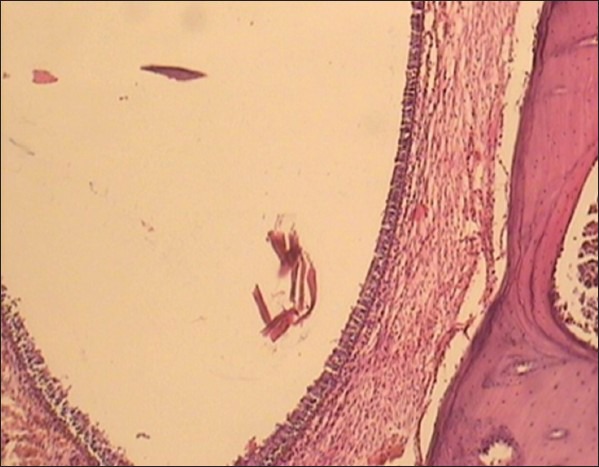
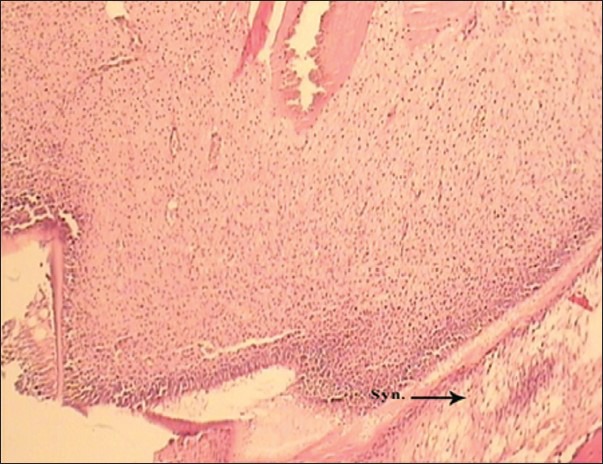
Animal models are necessary for assessment TMJ disorders,[21] rats were selected in this study because they have condylar translatory movements similar to human condyle[10] in this study administration of IA injection of betamethasone long acting showed a significant reduction in arthritis at 1 [Figures 2 and 3] and 4 weeks after drug injection compared with IP injection [Figures 4 and 5]. This might be due to local effects of betamethasone LA as an anti-inflammatory agent in chronic arthritis of the TMJ. Betamethasone L.A is a corticosteroied that is injected directly inside the joints for decrease pain and stiffness in arthritis rheumatoied. Therapeutic response started during several hours and continued about 1-4 weeks after IA and intra lesional injection.[22] Kopp et al.[23] reported that favorite anti-inflammatory effects is seen with joint injection because the drug efficacy is increased and the effect of injection is limited to the affected area. In the present study, the most anti-inflammatory response was observed at 4 weeks after IA injection of betamethasone L.A in histological aspect. Kopp et al. showed that IA injection of betamethasone (simple form) twice into the superior joint compartment of the TMJ with a 2-week interval between injections, reduced the symptoms and signs in patients who had pain and tenderness to palpation in TMJ.[12] Wennenberg et al. reported that betamethasone injections on TMJ arthritis showed a significant improvement in subjective symptoms, Clinical sign and bite forces at 1 or 2 years follow-up. Stability of therapeutic effects was observed even after at 8 years follow-up.[13] in the present study, although one injection was done, the condylar head showed resorption with osteoclastic activity at 4 weeks after drug injection. El-Hakim et al. reported evidences of bone resorption of the condylar head at 6 weeks after IA injection of dexamethasone[10] also bell showed that IA injection of steroids caused damage of TMJ in monkeys.[24] the results of this study was in agreement with El-Hakim et al. and the bell.[10,24] Toller could not report any radiographical evidences that a single IA injection of corticosteroids cause damage to TMJ, but he reported that multiple injections can cause damage to the TMJ[25] the differences between results of our study with Toller[25] Can be due to this fact that the base of assessment in Toller study was radiograophical evidence while the finding of this study and El-Hakim et al.[10] are based on histological findings during different times. The present study is the 1st research, which survey the local and systemic effect a single dose of betamethasone LA on TMJ structure while the other studies had used the multi injections of betamethasone (simple form). Our results are based on histological findings at different time periods that are considered more realistic while the results of other studies were based on the symptoms and clinical signs in patients.[12,13]
Figure 2.
Photomicrograph of the group (B) 1 week after articular injection of betamethasone LA showing mild hyperplasia of synovial cells (H and E, ×100)
Figure 3.
Photomicrograph of the group (D) 1 week after intra-peritoneal injection of betamethasone LA showing distinct hyperplasia of synovial cells (H and E, ×100)
Figure 4.
Photomicrograph of the group (C) 4 weeks after articular injection of betamethasone LA showing synovial cell adhesions (H and E, ×100)
Figure 5.
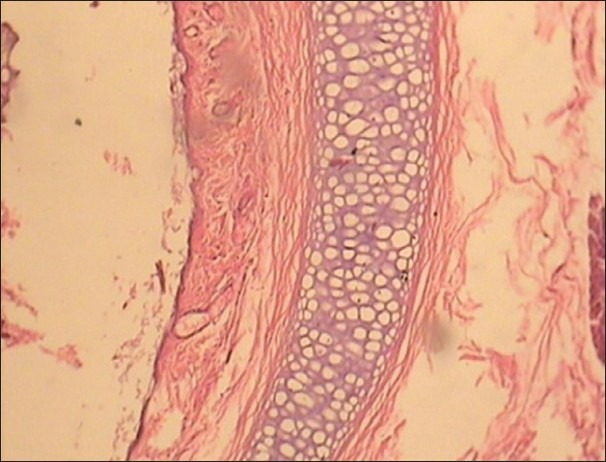
Photomicrograph of the group (E) 4 weeks after intra-peritoneal injection of betamethasone LA showing evidence of hyperplasia synovial cells (H and E, ×100)
Outstanding point in the study was condylar bone resorption 4 weeks after a single dose of IA betamethasone LA injection but El-Hakim et al.[10] observed this effect at 6 weeks with a single dose of IA dexamethasone injection.
CONCLUSION
The best therapeutic response was seen with IA injection of betamethasone L.A in comparison with IP injection.
IA injection of betamethasone L.A is recommended in treatment TMJ Arthritis. The resorption of condylar head may be due to side effect of the local injection of corticosteroids.
Footnotes
Source of Support: This report is based on a thesis which was submitted to the School of Dentistry, Isfahan University of Medical Sciences, Iran, in partial fulfillment of the requirements for the MSc degree in Post Graduate of Oral and Maxillofacial (#390551 proposal code). The study was approved by the Medical Ethics and Research Office at the Isfahan University of Medical Sciences and financially supported by this University
Conflict of Interest: None declared.
REFERENCES
- 1.Merjesjo C. Therapeutic and prognostic considerations in TMJ osteo arthrosis: A Literature review and a long term study in 11 subjects. J Craniomandib Pract. 1987;5:70. [PubMed] [Google Scholar]
- 2.Scutellari PN, Orzincolo C, Ceruti S. The temporo-mandibular joint in pathologic conditions: Rheumatoid arthritis and seronegative spondyloarthritis. Radiol Med. 1993;86:456–66. [PubMed] [Google Scholar]
- 3.Little JW, Falace DA, Miller CS, Rhodus NL. 8th ed. China: Elsevier Mosby; 2013. Dental Management of the Medically Compromised Patient; p. 323. [Google Scholar]
- 4.Greenberg M, Glick MA, Ship J. 11th ed. Hamilton: BC Decker; 2008. Burket's Oral Medicine; pp. 250–1. [Google Scholar]
- 5.Ertaş U, Tozoglu S, Sahin O, Seven B, Gundogdu C, Aktan B, et al. Evaluation of the anti-inflammatory effect of erythromycin on aseptic inflammation of temporomandibular joint in rabbit: A scintigraphic and histopathologic study. Dent Traumatol. 2005;21:213–7. doi: 10.1111/j.1600-9657.2005.00294.x. [DOI] [PubMed] [Google Scholar]
- 6.Habib GS, Saliba W, Nashashibi M. Local effects of intra-articular corticosteroids. Clin Rheumatol. 2010;29:347–56. doi: 10.1007/s10067-009-1357-y. [DOI] [PubMed] [Google Scholar]
- 7.Mountziaris PM, Kramer PR, Mikos AG. Emerging intra-articular drug delivery systems for the temporomandibular joint. Methods. 2009;47:134–40. doi: 10.1016/j.ymeth.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haddad IK. Temporomandibular joint osteoarthrosis. Histopathological study of the effects of intra-articular injection of triamcinolone acetonide. Saudi Med J. 2000;21:675–9. [PubMed] [Google Scholar]
- 9.Pertes RA, Gross Sh. Chicago, IL: Quintessence; 1995. Clinical management of temporomandibular disorders and orofacial pain; p. 69. (216-8). [Google Scholar]
- 10.El-Hakim IE, Abdel-Hamid IS, Bader A. Tempromandibular joint (TMJ) response to intra-articular dexamethasone injection following mechanical arthropathy: A histological study in rats. Int J Oral Maxillofac Surg. 2005;34:305–10. doi: 10.1016/j.ijom.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Peimani A. Evaluation of optimal dose on intra-articular injection of triamcinolone treatment of temmprondibular joint arthritis in rat. J Isfahan Dent Sch. 2009;4:192–8. [Google Scholar]
- 12.Kopp S, Wenneberg B, Haraldson T, Carlsson GE. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction. J Oral Maxillofac Surg. 1985;43:429–35. doi: 10.1016/s0278-2391(85)80050-1. [DOI] [PubMed] [Google Scholar]
- 13.Wenneberg B, Kopp S, Gröndahl HG. Long-term effect of intra-articular injections of a glucocorticosteroid into the TMJ: A clinical and radiographic 8-year follow-up. J Craniomandib Disord. 1991;5:11–8. [PubMed] [Google Scholar]
- 14.Kerins C, Carlson D, McIntosh J, Bellinger L. A role for cyclooxygenase II inhibitors in modulating temporomandibular joint inflammation from a meal pattern analysis perspective. J Oral Maxillofac Surg. 2004;62:989–95. doi: 10.1016/j.joms.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Fahim AT, Abd-el Fattah AA, Agha AM, Gad MZ. Effect of pumpkin-seed oil on the level of free radical scavengers induced during adjuvant-arthritis in rats. Pharmacol Res. 1995;31:73–9. doi: 10.1016/1043-6618(95)80051-4. [DOI] [PubMed] [Google Scholar]
- 16.McDougall JJ, Karimian SM, Ferrell WR. Alteration of substance P-mediated vasodilatation and sympathetic vasoconstriction in the rat knee joint by adjuvant-induced inflammation. Neurosci Lett. 1994;174:127–9. doi: 10.1016/0304-3940(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 17.McDougall JJ, Karimian SM, Ferrell WR. Prolonged alteration of vasoconstrictor and vasodilator responses in rat knee joints by adjuvant monoarthritis. Exp Physiol. 1995;80:349–57. doi: 10.1113/expphysiol.1995.sp003852. [DOI] [PubMed] [Google Scholar]
- 18.McDougall JJ. Abrogation of alpha-adrenergic vasoactivity in chronically inflamed rat knee joints. Am J Physiol Regul Integr Comp Physiol. 2001;281:R821–7. doi: 10.1152/ajpregu.2001.281.3.R821. [DOI] [PubMed] [Google Scholar]
- 19.Muto T, Kawakami J, Kanazawa M, Kaku T, Yajima T. Development and histologic characteristics of synovitis induced by trauma in the rat temporomandibular joint. Int J Oral Maxillofac Surg. 1998;27:470–5. doi: 10.1016/s0901-5027(98)80041-6. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki T, Segami N, Sato J, Nojima T. Accuracy of histologic grading of synovial inflammation in temporomandibular joints with internal derangement using Gynther's system. J Oral Maxillofac Surg. 2001;59:498–501. doi: 10.1053/joms.2001.22676. [DOI] [PubMed] [Google Scholar]
- 21.Almarza AJ, Hagandora CK, Henderson SE. Animal models of temporomandibular joint disorders: Implications for tissue engineering approaches. Ann Biomed Eng. 2011;39:2479–90. doi: 10.1007/s10439-011-0364-8. [DOI] [PubMed] [Google Scholar]
- 22.Abghon M. Tehran: Nooredanesh; 2003. Iranian generic drugs associated with the nursing care; pp. 101–3. [Google Scholar]
- 23.Kopp S, Akerman S, Nilner M. Short-term effects of intra-articular sodium hyaluronate, glucocorticoid, and saline injections on rheumatoid arthritis of the temporomandibular joint. J Craniomandib Disord. 1991;5:231–8. [PubMed] [Google Scholar]
- 24.Bell WE. 3rd ed. Chicago: Year Book Medical Publishers Inc; 1990. Temporomandibular Disorders, Classification, Diagnosis, Management; pp. 141–58. (231-72). 339-51. [Google Scholar]
- 25.Toller PA. Use and misuse of intra-articular corticosteroids in treatment of temporomandibular joint pain. Proc R Soc Med. 1977;70:461–3. [PMC free article] [PubMed] [Google Scholar]


