Abstract
Background:
Several conflicting findings have been published in the previous literature regarding the effects of impacted third molar surgery on the periodontal parameters of the adjacent second molar; some authors have shown improvement of periodontal health distal to the adjacent second molar, whilst others have demonstrated loss of attachment level (AL) and reduction of alveolar bone height. The purpose of this study was to evaluate the changes in periodontal health parameters distal to the adjacent second molar following extraction of an impacted third molar.
Materials and Methods:
Out of 50 patients participated in the study, 42 patients completed the study. The mean age of the sample was 20.9 (range, 18-25) years. All teeth were mesioangular impacted mandibular third molars categorized at C1 class based on the Pell and Gregory classification. All surgeries were performed by one surgeon and the same surgeon recorded the pre-operative and post-operative measurements of probing depth (PD) and AL on the distobuccal aspect of the second molars. Data analysis were carried out with the SPSS software (version 19), using the paired-samples t-test and one sample t-test.
Results:
Surgical extraction of impacted mandibular third molar resulted in a significant increase of PD on the distobuccal aspect of the second molars, whereas AL was decreased significantly after surgery (P < 0.05).
Conclusion:
Unlike plenty of researches that have shown improvement of periodontal parameters of the second molar after extraction of impacted third molar, our study showed a significant increase in PD at the distal aspect of the second molar. Further follow-up on clinical and radiological parameters are required for more profound understanding of the long-term effects of third molar extraction on the periodontal parameters of the adjacent second molar.
Keywords: Attachment level, probing depth, second molar, third molar surgery
INTRODUCTION
Mandibular third molars are found in 90% of the general population while 33% of them having at least one impacted third molar.[1] Mandibular third molar surgery is one of the most frequent surgical procedures carried out by oral surgeons. There are various reasons for M3 surgery such as caries and their outcomes, germination disorders, orthodontic problems, infection, trauma, and prevention or improvement of periodontal defects in the adjacent second molars.[2,3]
Surgical procedures for extraction of impacted third molars are associated with the significant morbidity including pain, swelling, trismus, and potential complications such as nerve injury and injury to adjacent teeth.[4] An important question to address is the risk of persistent or developing new periodontal defects on the distal aspect of the mandibular second molars following extraction of third molars.[5]
There is controversy about the incidence of periodontal defect at the distal aspect of the second molars after surgical extraction of the third molars. Some authors have shown improvement of periodontal health distal to the adjacent second molar, whilst others have demonstrated loss of AL and reduction of alveolar bone height.[6] Hence, the aim of our study was an evaluation of the periodontal parameters; PD, and AL, on the distobuccal aspect of the second molar after surgical extraction of the impacted third molar.
MATERIALS AND METHODS
To address the proposed specific aim, we used a prospective cohort study design. The sample was derived from the cohort of subjects enrolled in the clinical trial. To be included in the cohort, the subjects must be healthy young patients with a mesioangular impacted mandibular third molar that categorized at C1 class based on the Pell and Gregory classification [Figure 1].
Figure 1.
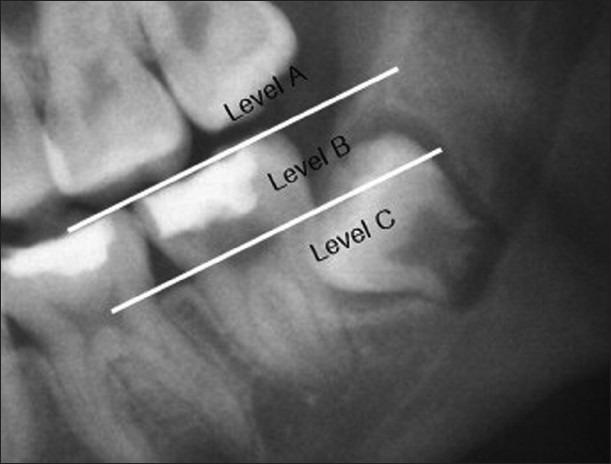
Class C mandible third molar impaction; the occlusal plane of the impacted tooth is apical to the cervical line of the adjacent tooth
The original cohort was composed of 50 subjects, with the mean age of 20.9 (range from 18 years to 25) years, of which 42 completed the study regular follow-up. All lower third molars were extracted by one surgeon under local anesthesia, generally with lidocaine in a 2% solution with epinephrine at 1:100,000. The surgeon raised a full-thickness triangular flap, which was protected by a Minnesota retractor. Lingual flap retraction with a Freer periosteal elevator was performed only when necessary.
Sterile moderate speed (30,000 rpm) handpieces and sterile saline solution were used for ostectomy and tooth sectioning when necessary. To close the wound, No. 3-0 Vicryle suture was used and after 7 days the suture was removed [Figure 2].
Figure 2.
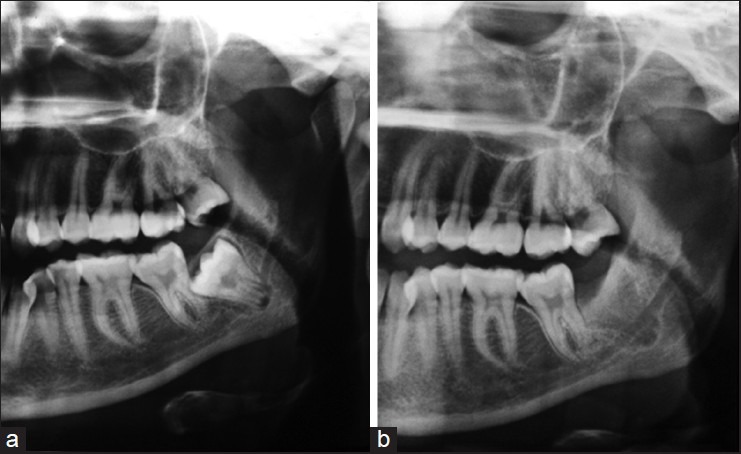
Pre-operative panoramic view of a class C impacted mandibular third molar (a), post-operative panoramic view of the same tooth (b)
Periodontal PD was measured on the distobuccal aspect of adjacent second molars with using a customized occlusal stent as a guide for the path of insertion of periodontal probe and Michigan O periodontal probe (Hu-Friedy, Chicago, IL) before surgery (PD1) and 6 months after surgery (PD2). AL also was measured from cementoenamel junction (CEJ) with using occlusal stent, before surgery (AL1) and 6 months after surgery (AL2) on the distobuccal aspect of the second molars.
One sample t-test was used to examine the mean difference of the PD1 between the sample and the known value of the normal PD.[7] This comparison showed that the mean of sample's PD1s was not statistically different from normal values. Indeed, samples before surgery were similar in term of this parameter to the right standard.
Data analyses were conducted by using SPSS software (version 19) and a probability level of 0.05 was used throughout. The results were analyzed statistically using one sample t-test and paired-sample t-test. The follow-up examination was performed by the same surgeon.
RESULTS
During the study interval, 50 patients enrolled in the study; 42 of them completed the study. Seven patients were excluded from analyses because they failed to complete regular follow-up. There were 42 third molar extraction sites available for evaluation.
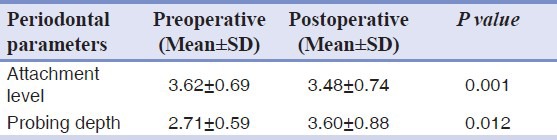
The pre-operative baseline PD (PD1) and 26 weeks post-operative (PD2) were measured; they ranged from a mean ± SD of 2.71 ± 0.59 mm to 3.60 ± 0.88 mm respectively.
The AL measurements ranged from a mean ± SD of 3.62 ± 0.69 mm pre-operative (AL1) to 3.48 ± 0.74 mm 26 weeks post-operative (AL2). For the periodontal PD measures, there was a statistically significant increase between the pre-operative baseline PDs (PD1) and 26 weeks post-operative (PD2) measurements. Furthermore, there were a statistically significant decrease between the pre-operative ALs (AL1) and 26 weeks post-operative (AL2) measures (P < 0.05) [Table 1].
Table 1.
Pre-operative and 26 weeks post-operative results and evaluation of them by the t-test
DISCUSSION
When managing impacted mandibular third molar in the adult population, the risk for developing or having persistent periodontal defects on the distal aspect of the mandibular second molar should be considered.
The results of this study showed that routine surgical management of full impacted mesioangular third molars resulted in statistically significant increased PD on the distal aspect of the mandibular second molars and the decrease in AL were also statistically significant 6 months after surgery.
Three important factors were found to influence periodontal status at the distal aspect of the second molar: patient's age, third molar impaction type and depth and pre-surgical periodontal defects.[8,9] Because of importance of above mentioned factors, two of the primary competency requirements for entrance to the study were the state and type of impaction. Only asymptomatic fully impacted mesioangular third molars were evaluated to avoid confounding factors related to exposure to the oral cavity and prior inflammatory/infectious processes.
Patient's age is another important risk factor commonly referenced in the literature.[8] For this reason, the sample analyzed in our study represented a group of young patients with the mean age of 20.9 (range from 18 to 25) years.
There are some study limitations. The study was unblinded, without randomization and control group. A small, specific sample group was selected (42 mandibular third molars from 50 patients) and given the statistically significant findings, by definition, the sample size was adequate. As in almost all longitudinal studies, the duration of follow-up was 6 months because there is a higher risk of patient dropout after 6 months.
In nearly all peer-reviewed studies, as in our study, only one specific PD site was noted but some reported the average measurements of two to three sites.[8,10,11]
Because the entire distal aspect of the second molar is at risk from the presence of pre-operative infrabony defects and iatrogenic injury during third molar surgery, it is more valuable that, the periodontal parameters be measured at three sites at the distal aspect of the second molar to provide a more detailed visualization of this area.
Previous studies showed that extraction of impacted mandibular third molar had no negative effects on the periodontal status of the adjacent second molar and in many patients it has resulted in improvement of the PD of second molars.[8] Other studies revealed the formation of periodontal defects at the distal aspect of second molars after surgical extraction of the mandibular third molars.[12] These studies did not classify the types of impaction, but our study concentrated on the mesioangular impacted third molars categorized in the C1 class based on the Pell and Gregory classification.
In this study, a period of at least 6 months following surgery had been elapsed prior to clinical examination for sufficient hard and soft-tissue healing to have occurred.[8] As localized periodontal lesions may remain symptomless until the periodontal attachment loss is very advanced, these may easily escape detection by the patient and an attending dentist.[13] This potentially creates a threat for the involved second molar. One study showed a greater reduction of deep intrabony defects persisting post-extraction in the 20-years-old age group versus the 30-years-old age group.[14] Another study found no correlation between age and increase PD at the distal aspect of the second molars after extraction of the third molars.[8]
In our study, all patients were in the same age group (18-25 years), so the influence of age on the periodontal parameters of the second molar after surgical extraction of the third molar was not shown.
Pre-operative condition of periodontal tissue at the distal aspect of the second molars may affect post-operative PD. The effect of different flap designs on post-operative periodontal pocket formation at the distal aspect of the second molar and other squeals has been reported.[15,16,17] We used sulcular incision with the releasing incision at the mesial aspect of second molars due to the necessity for wider access to the fully impacted third molars. Some other studies suggest reconstruction of bone defects after surgical removal of the impacted third molar.[18,19]
The current study may have a number of implications for health-care providers. First, the change of PD was evaluated in the target population after 6 months and second, the change of AL at the distal aspect of the second molar was evaluated after surgical removal of the third molar.
CONCLUSION
We concluded that the extraction of deeply impacted third molars causes increased PD at the distal aspect of the second molars, but AL decreased. Further studies using reconstructive procedures are recommended for preventing or resolving persistent periodontal defects on the distal aspect of the second molar after surgical removal of the impacted mandibular third molar.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rosa AL, Carneiro MG, Lavrador MA, Novaes AB., Jr Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:404–7. doi: 10.1067/moe.2002.122823. [DOI] [PubMed] [Google Scholar]
- 2.Nordenram A, Hultin M, Kjellman O, Ramström G. Indications for surgical removal of the mandibular third molar. Study of 2,630 cases. Swed Dent J. 1987;11:23–9. [PubMed] [Google Scholar]
- 3.Peterson LJ, Ellis E, III, Hupp JR, Tucker MR. St. Louis: Mosby; 1998. Contemporary Oral and Maxillofacial Surgery; pp. 215–25. [Google Scholar]
- 4.Bui CH, Seldin EB. Types, Frequencies, and Risk Factors for Complications After Third Molar Extraction. J Oral Maxillofac Surg. 2003;61:1379–89. doi: 10.1016/j.joms.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Richardson DT, Dodson TB. Risk of periodontal defects after third molar surgery: An exercise in evidence-based clinical decision-making. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:133–7. doi: 10.1016/j.tripleo.2005.02.063. [DOI] [PubMed] [Google Scholar]
- 6.Marmary Y, Brayer L, Tzukert A, Feller L. Alveolar bone repair following extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol. 1986;61:324–6. doi: 10.1016/0030-4220(86)90409-3. [DOI] [PubMed] [Google Scholar]
- 7.Wolf HF, Hassell TM. New York: Thieme; 2006. Color Atlas of Dental Hygiene: Periodontology; pp. 168–71. [Google Scholar]
- 8.Kan KW, Liu JK, Lo EC, Corbet EF, Leung WK. Residual periodontal defects distal to the mandibular second molar 6-36 months after impacted third molar extraction. J Clin Periodontol. 2002;29:1004–11. doi: 10.1034/j.1600-051x.2002.291105.x. [DOI] [PubMed] [Google Scholar]
- 9.White RP, Jr, Fisher EL, Phillips C, Tucker M, Moss KL, Offenbacher S. Visible third molars as risk indicator for increased periodontal probing depth. J Oral Maxillofac Surg. 2011;69:92–103. doi: 10.1016/j.joms.2010.07.076. [DOI] [PubMed] [Google Scholar]
- 10.Montero J, Mazzaglia G. Effect of removing an impacted mandibular third molar on the periodontal status of the mandibular second molar. J Oral Maxillofac Surg. 2011;69:2691–7. doi: 10.1016/j.joms.2011.06.205. [DOI] [PubMed] [Google Scholar]
- 11.Briguglio F, Zenobio EG, Isola G, Briguglio R, Briguglio E, Farronato D, et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: Clinical and statistical evaluations. Quintessence Int. 2011;42:445–53. [PubMed] [Google Scholar]
- 12.Gröndahl HG, Lekholm U. Influence of mandibular third molars on related supporting tissues. Int J Oral Surg. 1973;2:137–42. doi: 10.1016/s0300-9785(73)80030-4. [DOI] [PubMed] [Google Scholar]
- 13.Kugelberg CF, Ahlström U, Ericson S, Hugoson A, Kvint S. Periodontal healing after impacted lower third molar surgery in adolescents and adults. A prospective study. Int J Oral Maxillofac Surg. 1991;20:18–24. doi: 10.1016/s0901-5027(05)80689-7. [DOI] [PubMed] [Google Scholar]
- 14.White RP, Jr, Madianos PN, Offenbacher S, Phillips C, Blakey GH, Haug RH, et al. Microbial complexes detected in the second/third molar region in patients with asymptomatic third molars. J Oral Maxillofac Surg. 2002;60:1234–40. doi: 10.1053/joms.2002.35718. [DOI] [PubMed] [Google Scholar]
- 15.Jakse N, Bankaoglu V, Wimmer G, Eskici A, Pertl C. Primary wound healing after lower third molar surgery: Evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:7–12. doi: 10.1067/moe.2002.119519. [DOI] [PubMed] [Google Scholar]
- 16.Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–6. doi: 10.1016/j.tripleo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 17.Suarez-Cunqueiro MM, Gutwald R, Reichman J, Otero-Cepeda XL, Schmelzeisen R. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:403–8. doi: 10.1067/moe.2003.84. [DOI] [PubMed] [Google Scholar]
- 18.Dodson TB. Is there a role for reconstructive techniques to prevent periodontal defects after third molar surgery? Oral Maxillofac Surg Clin North Am. 2007;19:99–104. doi: 10.1016/j.coms.2006.11.004. vii. [DOI] [PubMed] [Google Scholar]
- 19.Sammartino G, Tia M, Gentile E, Marenzi G, Claudio PP. Platelet-rich plasma and resorbable membrane for prevention of periodontal defects after deeply impacted lower third molar extraction. J Oral Maxillofac Surg. 2009;67:2369–73. doi: 10.1016/j.joms.2009.04.093. [DOI] [PubMed] [Google Scholar]


