Abstract
Background:
Physicians have long recognized the association between diabetes mellitus and several pathologic conditions of the hand. The most commonly recognized maladies are limited joint mobility (LJM), Dupuytren's disease (DD), trigger finger (TF), and carpal tunnel syndrome (CTS). Incidence of these hand disorders has increased in the setting of diabetes. Collectively, these are described as diabetic hand syndrome.
Aim:
The aims were to find out the prevalence of hand disorders in diabetic patients, and to study the relation of these hand disorders with microvascular complications.
Subjects and Methods:
This is an observational cross-sectional case-control study done over a period of 1 year Patients of type 2 DM, of age < 65 years, who visited Gandhi Memorial Hospital, Lucknow were enrolled and were described as cases. Age- and sex-matched nondiabetic individuals were taken in the control group. The data were analyzed using software SPSS. SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc. Means and standard deviations were computed; the Student t-test and Chi-square (χ2) test were used as appropriate.
Results:
A total of 400 subjects were studied, 200 each in the case and control groups. Of total 200 diabetic patients, 30% (60/200) patients had neuropathy, 37.5% (75/200) had nephropathy, and 44.5% (89/200) patients had retinopathy. In the study population, 67% patients were having one or more hand disorders, in which LJM was found in 40.5% (81/200) patients, DD was found in 19% (38/200) patients, TF in 16.5% (33/200), and CTS in 14% (28/200) patients.
Conclusions:
This study shows a high prevalence of hand disorders in diabetic patients and also correlates with the duration of type 2 DM, LJM being the most common hand disorder and more common in patients who have microvascular complications.
Keywords: Carpal tunnel syndrome, Dupuytren's disease, Limited joint mobility, Trigger finger
Introduction
Diabetes mellitus has large number of complications; some of them are well known such as nephropathy, and retinopathy, and neuropathy. Diabetic foot has always been a point of worry for treating physicians but complications like diabetic hand syndrome might not have gained enough recognition. Diabetes is complicated by musculoskeletal problems of upper extremity and particularly the hand, collectively referred as “the diabetic hand.” The entity includes not only more specific diabetic-related conditions like limited joint mobility (LJM) but also conditions related to the nondiabetic hand, such as trigger finger, Dupuytren's contracture, and peripheral nerve compression lesions.[1] LJM is also known as diabetic cheiroarthropathy/diabetic stiff hand syndrome and it has been found in 8-50% of all patients with type 1 diabetes and is also seen in type 2 diabetic patients. Rosenbloom, et al. have described an association between microvascular complications and cheiroarthropathy in patients with type 1 DM.[2] LJM is also known as diabetic cheiroarthropathy or stiff hand syndrome [Figure 1]. Limited joint mobility is a painless and nondisabling complication of diabetes caused by thickening and stiffness of peri-articular connective tissue. It involves mainly the small joints of the hand and is often neglected until hand deformity is severe enough to interfere with daily life.
Figure 1.

Diabetic cheiroarthropathy or stiff hand syndrome
Patients with LJM typically have limited extension of the metacarpophalangeal, proximal, and distal interphalangeal joints, generally beginning in the ulnar digits and spreading radially. The preacher's sign involves the patient holding the hands opposed to one another vertically with elbows flexed and wrists extended. A positive sign is indicated by an inability of the patient to completely approximate the palmar surface of the digits [Figure 2]. The table top sign is a similar test in which the patient places the palms flat on a hard surface with the digits spread. Normally, the entire palmar surface of the digits should contact the table. If the test is positive, the digits and palm will not lay flat. Positive screening tests warrant careful passive examination of each joint to assess limited extension. Both these tests can be positive with other clinical conditions, such as Dupuytren's contracture or previous trauma, so a careful history and physical examination to rule out these conditions is needed.
Figure 2.

The preacher's sign involves the patient holding the hands opposed to one another vertically with elbows flexed and wrists extended. A positive sign is indicated by an inability of the patient to completely approximate the palmar surface of the digits
Limited joint mobility has been recognized as the most common and earliest long-term complication of type I DM and it also occurs in type 2 DM. There is documented evidence on the relationship between LJM and microvascular complications, whereas the age, DM duration, and glycemic control play inconclusive roles. There is also a 3-fold increased risk of microvascular complications. This could provide clues to earlier diagnosis of long-term complications in this group of patients.[3]
Since only few studies have been reported from India that compared rheumatic manifestations in a cohort of diabetic patients with control group, one such effort was made by Sarkar, et al.[4] The characteristics of diabetic foot disease are well documented in India; henceforth it would be appropriate to evaluate the problem of diabetic hand syndrome in this environment, and an attempt to characterize the relevance of these disorders with microvascular complications of type 2 DM.
Subjects and Methods
Study design
This was a cross-sectional case-control study conducted over a period of 1 year.
Study population
Patients of type 2 DM and nondiabetic patients who attend the outdoors or have admitted in the Department of Medicine at KG Medical University, Lucknow, India, were enrolled.
Inclusion criteria
Patients of type 2 DM, age less than 65 years and, age and sex matched nondiabetics who consented to participate in the study were selected for the study provided they did not have any obvious previous hand pathology.
Exclusion criteria
Patients who had hand diseases due to rheumatoid arthritis, osteoarthritis, infective arthritis, traumatic arthritis, gouty arthritis, end-stage renal disease, and thyroid disorders were excluded.
Procedure
All subjects were undergone through a thorough clinical examination. The demographic parameters [age, gender and body mass index (BMI)] were noted of each subject. In diabetic patients, fasting plasma glucose and 2-h postprandial glucose was evaluated. The presence of proteinuria was determined with Albustix® test on at least two clinic visits. The prayer sign and flattening sign were also used for qualitative assessment of limited joint mobility.
The prayer sign is described as the inability to fully flatten the two palms when opposed and clasped together. The flattening sign is described as the inability to fully flatten the palm on a flat surface. Trigger finger (Flexor tenosynovitis) patients complain of a catching sensation or locking phenomenon that may be associated with pain in the affected fingers. Examination shows a palpable nodule, usually in the area overlying the metacarpophalangeal joint, and thickening along the affected flexor tendon sheath on the palmar aspect of the finger and hand. Also, the locking phenomenon may be reproduced with either active or passive finger flexion. Phalen's and Tinel's signs were looked for diagnoses of carpel tunnel syndrome (CTS). Tinel's sign, tapping over the median nerve on the volar aspect of the wrist produces paresthesias distally in the hand was considered positive for diagnoses of CTS. In Phalen's test, patients were asked to flex both wrists so that the dorsa of both hands are touching and to hold that position for 30-60 s. A positive Phalen's test consisted of paresthesias being reproduced in the hand with this maneuver. Patients were also examined for possible motor weakness caused by median nerve compression. This is done by assessing thenar muscle strength and examining the hand for the presence of thenar muscle atrophy. This study was approved by ethical committee of our institute.
Statistical analysis
The data of this study were analyzed using descriptive and inferential statistics on statistical package for the social sciences software, release 17.0 for Windows (SPSS version 17.0., Chicago: SPSS Inc). Means and standard deviations were computed; Student t-test and Chi-square (χ2) test were used as appropriate. A significant difference was implied when the P value is < 0.05.
Results
The study encompassed a total of 400 subjects, 200 in each case and control group. The mean (SD) age of DM patients was 51.8 (11.5) years with a range of 19-65 years, while that of the control was mean (SD) 53.1 (12.5) years with a range of 19-65 years. The case group comprised 98 males and 102 females while the control group had 101 males and 99 females. There was no significant difference between the ages, genders, heights, weights, and BMI of patients and controls. In the case group, among microvascular complication retinopathy was the most common, was present in 44.5% (89/200), 37.5% (75/200) patients had nephropathy, and 30% (60/200) patients had neuropathy.
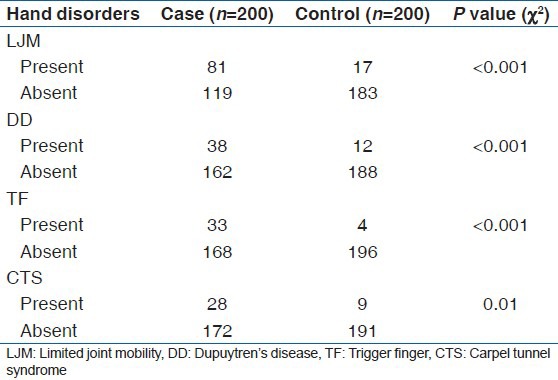
Cases had mean (SD) fasting blood glucose (FBG) and 2-h postprandial (PP) blood glucose level of 126 (28) mg/dl with a range of 104-142 mg/dl and 164 (23) mg/dl with a range of 145-198 mg/dl, respectively. In the study population, 67% (134/200) patients were having one or more hand disorders, and it was found in 19 (38/200) patients of the control group. Limited joint mobility (LJM) with a prevalence rate of 40.5% (81/200) was the most common hand disorder present in the case group. Comparison of the prevalence of various hand disorders in the case and control groups is shown in Table 1.
Table 1.
The distribution of various hand disorders in the case and control groups
In subgroup analysis, cases with LJM had mean (SD) FBG and PP level of 148 (29) mg/dl and 196 (32) mg/dl, respectively which was more than the total mean. The number of patients who had higher HbA1c level (> 7) was more in patients with LJM and DD while such a difference was not seen in patients having TF and CTS [Table 2]. In subgroup analysis, cases of LJM had most commonly retinopathy in 70.3% (57/81) than nephropathy in 58.0% (47/81) and then had neuropathy in 50.5% (41/81), shown in Table 2.
Table 2.
The distribution of various hand disorders in relation to HbA1c and microvascular complications in the case group
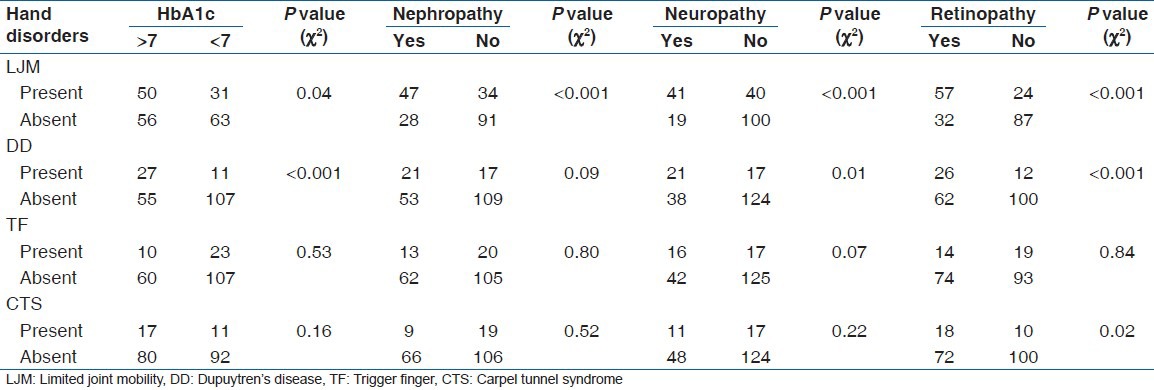
The subgroup of cases with DD also had retinopathy 68.4% (26/38) as most common microvascular complication followed by neuropathy and nephropathy in 55.3% (21/38).
Out of 33 TF patients, 48.5% (16/33) were having neuropathy, while out of 167 non-TF patients only 25.2% (42/167) patients were having neuropathy (P = 0.01). Out of 33 TF patients, 39.4% (13/33) were having nephropathy while out of 167 non-TF patients, 37.1% (62/167) were having nephropathy (P = 0.81). Out of 33 TF patients, 42.4% (14/33) had retinopathy while out of 167 non-TF patients, 44.5% (74/167) (44.5%) had retinopathy (P = 0.84).
Out of 28 CTS patients, 39.3 (11/28) (39.3%) were having neuropathy while out of 172 patients without CTS, 27.9% (48/172) were having neuropathy (P = 0.22). Out of 28 CTS patients, 32.1% (9/28) were having nephropathy while out of 172 patients without CTS, 38.2% (66/172) were having nephropathy (P = 0.52). Out of 28 CTS patients, 64.3% (18/28) were having retinopathy while out of 172 patients without CTS, 41.9% (72/172) were having retinopathy (P = 0.02).
On the basis of duration of diabetes since they diagnosed to have diabetes, cases were categorized into two groups; < 10 years were 70.5% (141/200) and > 10 years were 29.5% (59/200). Except for CTS; LJM (P < 0.001), DD (P < 0.001), and TF (P = 0.01) were more commonly observed in patients who were having diabetes for > 10 years than who had it for < 10 years.
It is clear from above data that all microvascular complications (nephropathy, neuropathy, and retinopathy) were found to be significantly higher in the patients having LJM and DD [Figure 3]. While TF and CTS was found to be significantly associated with retinopathy and neuropathy, respectively, it was also observed that HbA1c of patients with LJM and DD was significantly higher than those without LJM and DD.
Figure 3.
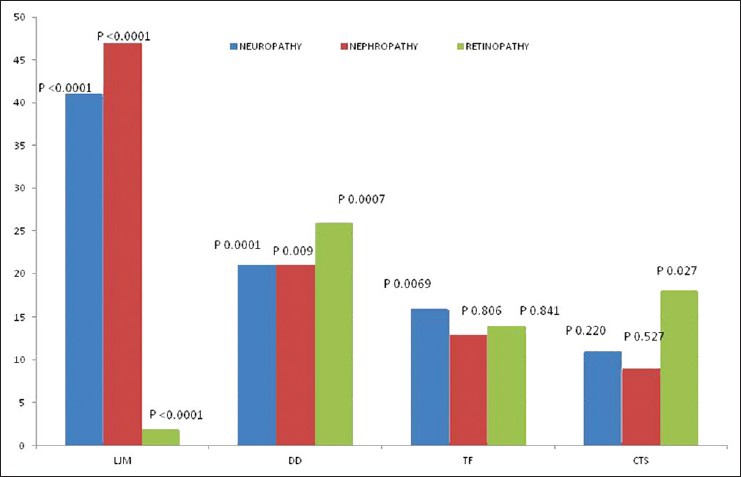
Relative percentage of hand disorder with respect to microvascular complication
Discussion
This study found that the hand disorders were present in two third of the patients of type 2 DM, LJM being the most common hand disorder followed by DD then TF and CTS. Similarly, the prevalence of hand disorder is reported in the Mota, et al. study where the prevalence was 50%.[5] LJM was common in diabetic patients with prevalence of 40.5% compared to controls with a prevalence of 19%. LJM is a common complication of DM, occurring in 8-58% of patients; most studies suggest that the prevalence is about 30-40%.[2,6,7,8] Moreover, we also found that the prevalence of hand disorder increases with duration of diabetes. In patients with LJM, retinopathy was the most common microvascular complication seen followed by nephropathy and neuropathy. LJM is associated with a 3-4 fold risk for retinopathy, nephropathy, and neuropathy.[9,10,11]
There was no significant relationship between gender and hand disorders in patients of type 2 DM. Moreover, we found that the prevalence of hand disorder increases with duration of diabetes. This condition is associated with and predictive of other diabetic complications. This syndrome is characterized by thick, tight, waxy skin reminiscent of scleroderma. A limited joint range of motion (inability to fully flex or extend the fingers) and sclerosis of tendon sheaths is also seen. The underlying cause is thought to be multifactorial.[12] Increased glycosylation of collagen in the skin and periarticular tissue, decreased collagen degradation, diabetic microangiopathy, and possibly diabetic neuropathy are thought to be some of the contributing factors. Flexion contractures of the fingers may develop at advanced stages. One indication of the presence of this condition is known as the “prayer sign.”[13] This is the patients’ inability to press their palms together completely without a gap remaining between opposed palms and fingers. The specific treatment of diabetic cheiroarthropathy (other than optimizing glycemic control) is unknown. Obvious findings of cheiroarthropathy like the “prayer sign” may not be seen in all cases as a rule. Subclinical limited joint mobility can be measured using a finger goniometer and in this study a highly significant association was demonstrated between restriction of flexion of small joints of hands and duration and severity of T2DM. This is a path-breaking finding based on which further studies can be planned to demonstrate the association of restriction of flexion of small joints of hands and microvascular complications in T2DM. If an association between these disorders is discovered then finger flexion may be used as a marker for microvascular complications.
Flexor tenosynovitis (or trigger finger) is another frequent diabetic complication of the hands. Patients complain of a catching sensation or locking phenomenon that may be associated with pain in the affected fingers. Examination shows a palpable nodule, usually in the area overlying the metacarpophalangeal joint, and thickening along the affected flexor tendon sheath on the palmar aspect of the finger and hand. Also, the locking phenomenon may be reproduced with either active or passive finger flexion.[14,15] This complication is thought to have the same pathogenesis as diabetic cheiroarthropathy, and its prevalence is similarly related to the duration of diabetes.[16]
Dupuytren's contracture results from a thickening, shortening, and fibrosis of the palmar fascia. Nodule formation along the fascia is seen. Flexion contractures of the fingers may result, usually at the fourth finger, but sometimes involving any of the second through fifth digits.[17,18] Dupuytren's contracture has been reported in 16-42% of diabetic patients. Its pathogenesis is thought to be the same as that for cheiroarthropathy. Physical therapy may be beneficial for early or mild cases. Varied success has been reported with local corticosteroid injections. Surgical intervention may be needed for severe cases.[18]
Carpal tunnel syndrome (CTS) is seen in up to 20% of diabetic patients.[19] Its specific relationship to diabetes is thought to be median nerve entrapment caused by the diabetes-induced connective tissue changes mentioned above. The prevalence of CTS in diabetic patients generally increases with duration of diabetes.[20] CTS is usually diagnosed based on patients’ history and clinical findings. Classically, patients complain of burning, paresthesias, or sensory loss in the median nerve distribution (the first three fingers as well as the radial half of the fourth finger). They may also complain of pain in the same area, often with radiation proximally into the forearm and arm. The pain may awaken patients from sleep and is aggravated by activities involving wrist flexion or extension, such as holding a newspaper or book, typing, driving, or using a knife and fork.[19,20,21] Awareness on the part of the clinicians is necessary in order to intercede in CTS before the development of thenar muscle atrophy. Diabetic patients also have paresthesias that may be attributed to underlying peripheral neuropathy, and these two entities must be differentiated. Conservative treatment is tried initially for early or mild cases, using volar wrist splints (particularly at night) with or without nonsteroidal anti-inflammatory drugs. Ergonomic adjustment of computer workstations should be made when appropriate. Local corticosteroid injection of the carpal tunnel may be tried as well. Patients with severe or refractory cases, as well as those with thenar atrophy or progressive neurological changes on serial EMG/NCV testing, should be sent for definitive therapy with surgical release of the transverse carpal ligament by a hand surgeon.[14]
The study is limited by the following facts; the number of subjects was small in both case and control groups; the diagnoses of various hand disorders was considered only on clinical examination; radioimaging of hand joints was not taken into account which might have strengthen our findings. Electromyogram/nerve conduction velocity (EMG/NCV) testing was not done which could confirm the diagnosis of CTS in uncertain cases and could also help to localize the site of nerve entrapment.
Still we would like to conclude that the examination of peri-articular regions of the hands and its joints should be included in the evaluation of patients with DM because the hand disorders are common in patients of type 2 DM. LJM is the most common hand disorder present in type 2 DM. Most of the hand disorders seem to be associated with the duration of DM and are associated with microvascular complication thus probably related to the long-term glycemic control of the diabetes appear in younger age in diabetic patients in comparison to their counterparts in the general population.
Acknowledgment
We thank patients and their relatives for cooperation and support without which this undertaking could not have been possible.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Ikem RT, Kolawole BA, Olasode O. A descriptive study of foot complications in diabetic patients with symptomatic peripheral neuropathy. Afr J Neurol Sci. 2005;24:7–12. [Google Scholar]
- 2.Rosenbloom AL, Silverstein JM, Lezotte DC, Richardson K, Mc Callum M. Limited joint mobility in childhood diabetes indicates increased risk for microvascular disease. N Engl J Med. 1981;305:191–4. doi: 10.1056/NEJM198107233050403. [DOI] [PubMed] [Google Scholar]
- 3.Lekholm C, Sundkvist G, Lundborg G, Dahlin L. The diabetic hand-complication of diabetes. Lakapudninger. 2001;98:306–12. [PubMed] [Google Scholar]
- 4.Sarkar RN, Banerjee S, Basu AK, Bandyopadhyay R. Rheumatological manifestations of diabetes mellitus. J Indian Rheumatol Assoc. 2003;11:25–9. [Google Scholar]
- 5.Mota M, Panus C, Mota E, Sfredel V, Patrascu A, Vanghelie L, et al. Hand abnormalities of the patients with diabetes mellitus. Rom J Intern Med 2000. 2001;38-39:89–95. [PubMed] [Google Scholar]
- 6.Seibold JR. Digital sclerosis in children with insulin-dependent diabetes mellitus. Arthritis Rheum. 1982;25:1357–61. doi: 10.1002/art.1780251112. [DOI] [PubMed] [Google Scholar]
- 7.Larkin JG, Frier BM. Limited joint mobility and Dupuytren's contracture in diabetic, hypertensive, and normal populations. Br Med J (Clin Res Ed) 1986;292:1494. doi: 10.1136/bmj.292.6534.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kapoor A, Sibbitt WL., Jr Contractures in diabetes mellitus: The syndrome of limited joint mobility. Semin Arthritis Rheum. 1989;18:168–80. doi: 10.1016/0049-0172(89)90059-0. [DOI] [PubMed] [Google Scholar]
- 9.Rosenbloom AL, Silverstein JH, Lezotte DC, Riley WJ, Maclaren NK. Limited joint mobility in diabetes mellitus of childhood: Natural history and relationship to growth impairment. J Pediatr. 1982;101:874–8. doi: 10.1016/s0022-3476(82)80351-x. [DOI] [PubMed] [Google Scholar]
- 10.Garg SK, Chase HP, Marshall G, Jackson WE, Holmes D, Hoops S, et al. Limited joint mobility in subjects with insulin dependent diabetes mellitus: Relationship with eye and kidney complications. Arch Dis Child. 1992;67:96–9. doi: 10.1136/adc.67.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Starkman HS, Gleason RE, Rand LI, Miller DE, Soeldner JS. Limited joint mobility (LJM) of the hand in patients with diabetes mellitus: Relation to chronic complications. Ann Rheum Dis. 1986;45:130–5. doi: 10.1136/ard.45.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lundbaek K. Stiff hands in long-term diabetes. Acta Med Scand. 1957;158:447–51. doi: 10.1111/j.0954-6820.1957.tb15511.x. [DOI] [PubMed] [Google Scholar]
- 13.Lawson PM, Maneschi F, Kohner EM. The relationship of hand abnormalities to diabetes and diabetic retinopathy. Diabetes Care. 1983;6:140–3. doi: 10.2337/diacare.6.2.140. [DOI] [PubMed] [Google Scholar]
- 14.Blyth MJ, Ross DJ. Diabetes and trigger finger. J Hand Surg. 1996;21B:244–5. doi: 10.1016/s0266-7681(96)80106-9. [DOI] [PubMed] [Google Scholar]
- 15.Griggs SM, Weiss AP, Lane LB, Schwenker C, Akelman E, Sachar K. Treatment of trigger finger in patients with diabetes mellitus. J Hand Surg. 1995;20A:787–9. doi: 10.1016/S0363-5023(05)80432-0. [DOI] [PubMed] [Google Scholar]
- 16.Jennings AM, Milner PC, Ward JD. Hand abnormalities are associated with the complications of diabetes in type 2 diabetes. Diabet Med. 1989;6:43–7. doi: 10.1111/j.1464-5491.1989.tb01137.x. [DOI] [PubMed] [Google Scholar]
- 17.Noble J, Heathcote JG, Cohen H. Diabetes mellitus in the aetiology of Dupuytren's disease. J Bone Joint Surg. 1984;66B:322–5. doi: 10.1302/0301-620X.66B3.6725338. [DOI] [PubMed] [Google Scholar]
- 18.Loos B, Puschkin V, Horch RE. 50 years experience with Dupuytren's contracture in the Erlangen University hospital: A retrospective analysis of 2919 operated hands from 1956 to 2006. BMC Musculoskelet Disord. 2007;8:60. doi: 10.1186/1471-2474-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chammas M, Bousquet P, Renard E, Poirier JL, Jaffiol C, Allieu Y. Dupuytren's disease, carpal tunnel syndrome, trigger finger, and diabetes mellitus. J Hand Surg. 1995;20A:109–14. doi: 10.1016/S0363-5023(05)80068-1. [DOI] [PubMed] [Google Scholar]
- 20.Comi G, Lozza L, Galardi G, Ghilardi MF, Medaglini S, Canal N. Presence of carpal tunnel syndrome in diabetics: Effect of age, sex, diabetes duration and polyneuropathy. Acta Diabetol Lat. 1985;22:259–62. doi: 10.1007/BF02590778. [DOI] [PubMed] [Google Scholar]
- 21.Singh R, Gamble G, Cundy T. Lifetime risk of symptomatic carpal tunnel syndrome in type 1 diabetes. Diabet Med. 2005;22:625–30. doi: 10.1111/j.1464-5491.2005.01487.x. [DOI] [PubMed] [Google Scholar]


