Abstract
Background/Aim:
Open access endoscopy (OAE) decreases the waiting time for patients and clinical burden to gastroenterologist; however, the appropriateness of referrals for endoscopy and thus the diagnostic yield of these endoscopies has become an important issue. The aim of this study was to determine the appropriateness of upper gastrointestinal (GI) endoscopy requests in an OAE system.
Patients and Methods:
A retrospective chart review of all consecutive patients who underwent an upper gastroscopy in the year 2008 was performed and was defined as appropriate or inappropriate according to the American Society for Gastrointestinal Endoscopy (ASGE) guidelines. Endoscopic findings were recorded and classified as positive or negative. Referrals were categorized as being from a gastroenterologist, internist, surgeon, primary care physicians or others, and on an inpatient or out-patient basis.
Results:
A total of 505 consecutive patients were included. The mean age was 45.3 (standard deviation 18.1), 259 (51%) of them were males. 31% of the referrals were thought to be inappropriate. Referrals from primary care physicians were inappropriate in 47% of patients while only 19.5% of gastroenterologists referrals were considered inappropriate. Nearly, 37.8% of the out-patient referrals were inappropriate compared to only 7.8% for inpatients. Abnormal findings were found in 78.5% and 78% of patients referred by gastroenterologists and surgeons respectively while in those referred by primary care physicians it was (49.7%). Inpatients referred for endoscopy had abnormal findings in (81.7%) while in out-patients it was (66.6%). The most common appropriate indications in order of frequency were “upper abdominal distress that persisted despite an appropriate trial of therapy” (78.9%), “persistent vomiting of unknown cause” (19.2%), upper GI bleeding or unexplained iron deficiency anemia (7.6%). The sensitivity and specificity of the ASGE guidelines in our study population was 70.3% and 35% respectively.
Conclusion:
A large proportion of patients referred for endoscopy through our open-access endoscopy unit are considered inappropriate, with significant differences among specialties. These results suggest that if proper education of practitioners was implemented, a better utilization would be expected.
Keywords: Appropriateness of gastroscopy, gastroscopy, open access endoscopy, Saudi Arabia
The increasing demand for gastrointestinal (GI) endoscopy has resulted in a rise in the overall costs and prolonged waiting lists for endoscopic procedures. One method to overcome this problem has been to adopt an open access endoscopy system that enables practitioners to refer their patients for endoscopic procedures without being seen by a gastroenterologist prior to the procedure. The impact of this system on the care of patients in routine clinical practice cannot be underestimated, it results in decreased subsequent GI consultations and the level of compliance with the endoscopists’ recommendations is high.[1] In order to optimize the use of finite resources in an open-access system, official guidelines for the appropriate use of esophagogastroduodenoscopies (EGDs) have been proposed by the American Society for Gastrointestinal Endoscopy (ASGE).[2,3] The validity of these expert-derived guidelines has never been tested in a randomized study, generating some uncertainty on their efficacy. However, following the introduction of these guidelines in clinical practice, some observational studies have generally shown a substantial rate of inappropriate EGD indications, which in turn has been associated with a lower diagnostic yield for relevant findings as compared to appropriate procedures.[4]
The aim of our study was to evaluate the diagnostic yield of EGDs in a Saudi tertiary care university hospital where open-access endoscopy is available to both primary care physician and other specialists.
PATIENTS AND METHODS
A retrospective chart review of all patients who had an EGD at King Khalid University Hospital (KKUH) in the year 2008 was performed. All patients who had EGDs were included, even those done on an emergency basis (e.g., GI bleeding). Patients who had an elective therapeutic endoscopy, repeated surveillance after esophageal varices band ligation or for Barrett's esophagus were excluded. Demographic data were sought and the main indication(s) for gastroscopy were recorded. The practice guidelines of the ASGE published in year 2000 were used to assess the appropriateness of each procedure. Referrals for procedure were classified into those “generally indicated” (appropriate) and those “generally not indicated” (inappropriate).[2] Endoscopic findings were recorded and classified as normal or abnormal. Relevant endoscopic findings included esophagitis, esophageal varices, Barretts esophagus, gastric or duodenal ulcers, erosive gastro-duodenitis, strictures, cancer, and signs of portal hypertension. Referrals were categorized as being from a gastroenterologist, internist, surgeon, primary care physicians or others, and as an inpatient or out-patient referral. All patients gave informed consent for endoscopy and the study was approved by our institution review board at KKUH with reference number of E-12-817.
RESULTS
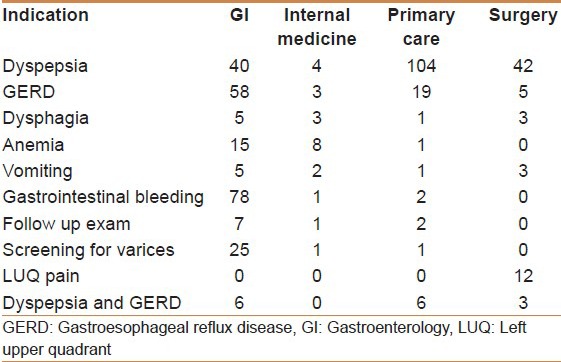
A cohort of 508 consecutive patients were included in the study. The mean age was 45.3 (standard deviation ± 18.1); 259 (51%) were males and 249 (49%) were females; 96.3% of them were Saudis. Gastroenterologists, primary care physicians, and surgeons were the referring physicians for 251 (49.4%), 147 (28.9%) and 73 (14.3%) patients respectively. Overall, 404 (78.8%) of all referrals were for out-patients, the remaining for hospitalized patients. The main indications for gastroscopy are shown in Table 1.
Table 1.
The main reason for endoscopy according to subspecialty
EGD indication was classified as appropriate according to the ASGE criteria in 349 (68.7%) patients and was inappropriate in the remaining 159 (31.3%).
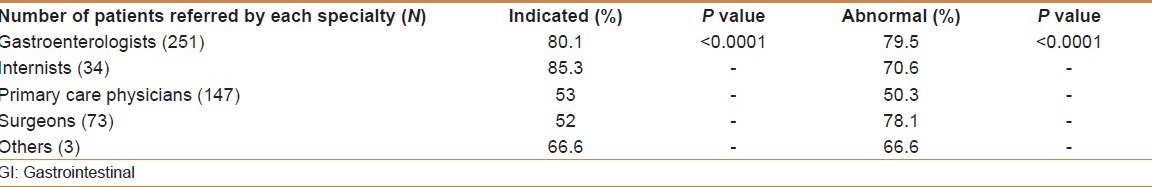
48% and 47% of referrals from surgeons and primary care physicians, respectively, were inappropriate, while only 19.5% (P < 0.00001) of referrals by gastroenterologists were inappropriate [Table 2]. The lowest rate of inappropriate referrals was from internists (14.7%). The mean sensitivity and specificity of the ASGE guidelines for the detection of relevant findings was 73.3% and 35%, respectively. Exclusion of patients with GI bleeding had no effect on the results, as shown in Table 2a.
Table 2.
Appropriateness and findings according to the referring physician and referral setting
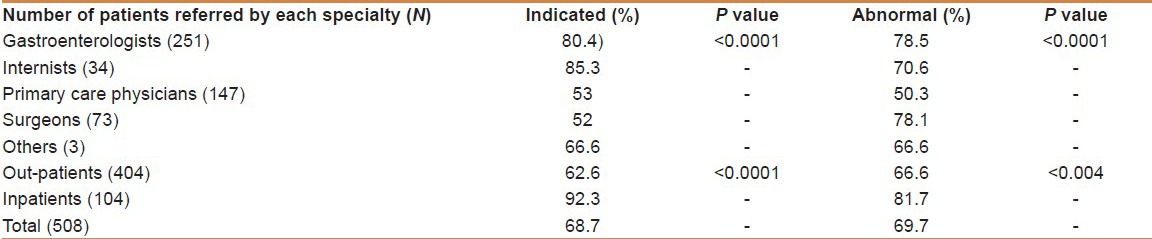
Table 2a.
Appropriateness and findings according to the referring physician and referral setting, excluding GI bleeding
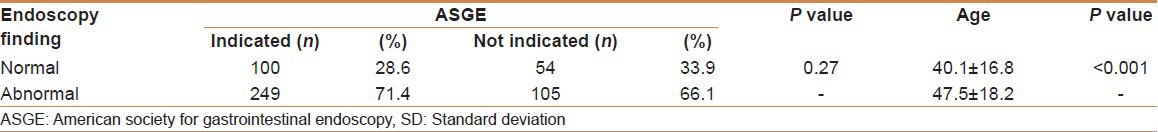
Patients older than 45 years of age were found to have more abnormal findings on endoscopy when compared to those below 45 years of age (P = 0.001). Abnormal biopsy results were found in 81 (47.9%) patients above 45 years of age. Endoscopic findings according to the ASGE guidelines and age are summarized in Table 3.
Table 3.
Findings of endoscopy according to ASGE guidelines and age
Nearly 37.4% of the out-patient referrals were inappropriate compared to only 7.4% for inpatients (P < 0.0001). Abnormal findings were found in 78.5% and 78% of patients referred by gastroenterologists and surgeons respectively while those referred by primary care physicians was 49.7% (P < 0.0001). Inpatients referred for endoscopy had abnormal findings in (81.7%) while only 66.6% of out-patients had abnormal findings on EGD. The most common appropriate indications in order of frequency were “upper abdominal distress that persisted despite an appropriate trial of therapy” (78.9%), “persistent vomiting of unknown cause” (19.2%), upper GI bleeding or unexplained iron deficiency anemia (7.6%). Overall, the most common inappropriate indication (48.3%) was “dyspepsia in patients aged below 45 years of age who had not tried an adequate course of medication.”
DISCUSSION
Upper endoscopy is a safe and accurate procedure and for this reason, most GI endoscopic centers, offer a service of open access upper endoscopy.[3,5,6] Consequently, a steady increase in the number of EGDs has been reported, resulting in a high-pressure demand with the risk of delaying the examinations for those patients with a potential serious disease. Therefore, evaluation of both the appropriateness and the diagnostic yield in relation to each clinical indication is critical to the assessment of the costs and benefits of procedures performed in an open-access setting. Several studies show a substantial rate of inappropriateness for the indication of upper endoscopy, widely ranging from 5% to 62%.[3,5,7,8,9,10,11,12]
Our results show that inappropriate use of EGD (31.3%) is higher than in the United Kingdom[11,13], United States[8,14], Italy[15], and also Asian populations[7], where inappropriate use of EGDs has been reported in 11% to 30% of patients referred for the procedure. Froehlich et al., from Switzerland reported a similar study with a rate of EGD inappropriateness as high as 40%.[3] However, caution is warranted in interpreting these data. Different guidelines are used in these studies as bench-marks, resulting in obvious differences in rates of appropriateness.
Although, the rate of inappropriate referrals by primary care physicians and surgeons were high in our study, the rate of inappropriate referrals by gastroenterologists was comparable to that found by Sánchez-del Río et al.,[16] where gastroenterologists referrals were inappropriate in only18.6%. In a prospective multicenter study, Hassan et al., found a huge variability of the inappropriateness of EGDs ranging from 2% to 60% (mean value was 22.9%).[17] They found the rate of inappropriate referrals from primary care physicians was more than 2-fold greater than that for specialists, confirming the results of a previous study.[10] Educational programs specifically dedicated to these primary care physicians were found to be critical to improve the overall effectiveness of an open-access system.[17]
The sensitivity and specificity of the ASGE guidelines in our study population was 70.3% and 35% respectively. In a large prospective multicenter study, Buri et al., found the ASGE guidelines for relevant findings to have a sensitivity of 88% and specificity of 27%, which is consistent with our findings.[15] Similar to other studies, the ASGE guidelines has a relatively high sensitivity for relevant findings, but it is hampered by a low specificity (ranges 25% to 30%).[9,15,18]
In a meta-analysis to assess the efficacy of the ASGE guidelines for appropriate gastroscopy referrals, eight cohort studies were included. For relevant findings, the adjusted sensitivity and specificity were 85% and 28% respectively.[9]
Despite the low specificity of ASGE guidelines for relevant findings in our study, abnormal findings were found in 78.5% and 78% of patients referred by gastroenterologists and surgeons. The frequency of positive findings in patients who underwent EGD for an indication judged inappropriate was strikingly high in the present and other studies.[5,7,19] The frequency of EGDs with positive findings that were performed for inappropriate indications ranges from 23% to 46%. Rossi et al., found that 3 (8%) of 38 cancers would have been missed if EGDs had not been performed, because the indication for these procedures was inappropriate by the recommendation of guidelines.[20] Age (above 45 years) was significantly associated with abnormal findings on endoscopy (P = 0.001) in our study, which is consistent with most of the previously reported studies.[3,19] Buri et al., showed that a simple rule based on age and alarm features may be as accurate as the more complex ASGE guidelines in predicting endoscopic outcomes in an unselected EGD population.[15]
In addition, although the probability of detecting a clinically relevant finding has been considered an important parameter for the appropriateness of endoscopy, a normal endoscopy in patients with dyspepsia greatly reduced the number of consultations and the prescription rates in one study.[21] Studies also have demonstrated a better quality of life and patient satisfaction, for patients with dyspepsia after the finding of a normal EGD.[22]
In conclusion, a large proportion of patients referred for endoscopy through our open-access endoscopy unit are considered inappropriate, with significant differences among specialties and a very low specificity. Independent predictive factors of abnormal findings were age over 45 years and referral by a gastroenterologist.
Footnotes
Source of Support: The authors extend their sincere appreciation to the Deanship of Scientific Research at King Saud University for its funding of this research through the Research Group Project number RGP-VPP-279
Conflict of Interest: None declared.
REFERENCES
- 1.Charles RJ, Cooper GS, Wong RC, Sivak MV, Jr, Chak A. Effectiveness of open-access endoscopy in routine primary-care practice. Gastrointest Endosc. 2003;57:183–6. doi: 10.1067/mge.2003.55. [DOI] [PubMed] [Google Scholar]
- 2.American Society for Gastrointestinal Endoscopy. Appropriate use of gastrointestinal endoscopy. Gastrointest Endosc. 2000;52:831–7. [PubMed] [Google Scholar]
- 3.Froehlich F, Burnand B, Pache I, Vader JP, Fried M, Schneider C, et al. Overuse of upper gastrointestinal endoscopy in a country with open-access endoscopy: A prospective study in primary care. Gastrointest Endosc. 1997;45:13–9. [PubMed] [Google Scholar]
- 4.Andriulli A, Annese V, Terruzzi V, Grossi E, Minoli G. “Appropriateness” or “prioritization” for GI endoscopic procedures? Gastrointest Endosc. 2006;63:1034–6. doi: 10.1016/j.gie.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 5.Gonvers JJ, Burnand B, Froehlich F, Pache I, Thorens J, Fried M, et al. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy unit. Endoscopy. 1996;28:661–6. doi: 10.1055/s-2007-1005573. [DOI] [PubMed] [Google Scholar]
- 6.Parente F, Bargiggia S, Bianchi Porro G. Prospective audit of gastroscopy under the ‘three-day rule’: A regional initiative in Italy to reduce waiting time for suspected malignancy. Aliment Pharmacol Ther. 2002;16:1011–4. doi: 10.1046/j.1365-2036.2002.01241.x. [DOI] [PubMed] [Google Scholar]
- 7.Chan YM, Goh KL. Appropriateness and diagnostic yield of EGD: A prospective study in a large Asian hospital. Gastrointest Endosc. 2004;59:517–24. doi: 10.1016/s0016-5107(04)00002-1. [DOI] [PubMed] [Google Scholar]
- 8.Mahajan RJ, Barthel JS, Marshall JB. Appropriateness of referrals for open-access endoscopy. How do physicians in different medical specialties do? Arch Intern Med. 1996;156:2065–9. [PubMed] [Google Scholar]
- 9.Di Giulio E, Hassan C, Marmo R, Zullo A, Annibale B. Appropriateness of the indication for upper endoscopy: A meta-analysis. Dig Liver Dis. 2010;42:122–6. doi: 10.1016/j.dld.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Zuccaro G, Jr, Provencher K. Does an open access system properly utilize endoscopic resources? Gastrointest Endosc. 1997;46:15–20. doi: 10.1016/s0016-5107(97)70203-7. [DOI] [PubMed] [Google Scholar]
- 11.Kahn KL, Kosecoff J, Chassin MR, Solomon DH, Brook RH. The use and misuse of upper gastrointestinal endoscopy. Ann Intern Med. 1988;109:664–70. doi: 10.7326/0003-4819-109-8-664. [DOI] [PubMed] [Google Scholar]
- 12.Manes G, Balzano A, Marone P, Lioniello M, Mosca S. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy system: A prospective observational study based on the Maastricht guidelines. Aliment Pharmacol Ther. 2002;16:105–10. doi: 10.1046/j.1365-2036.2002.01136.x. [DOI] [PubMed] [Google Scholar]
- 13.Brook RH, Park RE, Chassin MR, Solomon DH, Keesey J, Kosecoff J. Predicting the appropriate use of carotid endarterectomy, upper gastrointestinal endoscopy, and coronary angiography. N Engl J Med. 1990;323:1173–7. doi: 10.1056/NEJM199010253231705. [DOI] [PubMed] [Google Scholar]
- 14.Charles RJ, Chak A, Cooper GS, Wong RC, Sivak MV., Jr Use of open access in GI endoscopy at an academic medical center. Gastrointest Endosc. 1999;50:480–5. doi: 10.1016/s0016-5107(99)70069-6. [DOI] [PubMed] [Google Scholar]
- 15.Buri L, Hassan C, Bersani G, Anti M, Bianco MA, Cipolletta L, et al. Appropriateness guidelines and predictive rules to select patients for upper endoscopy: A nationwide multicenter study. Am J Gastroenterol. 2010;105:1327–37. doi: 10.1038/ajg.2009.675. [DOI] [PubMed] [Google Scholar]
- 16.Sánchez-del Río A, Quintero E, Alarcón O. Appropriateness of indications for upper gastrointestinal endoscopy in open-access endoscopy units. Gastroenterol Hepatol. 2004;27:119–24. doi: 10.1157/13058395. [DOI] [PubMed] [Google Scholar]
- 17.Hassan C, Bersani G, Buri L, Zullo A, Anti M, Bianco MA, et al. Appropriateness of upper-GI endoscopy: An Italian survey on behalf of the Italian society of digestive endoscopy. Gastrointest Endosc. 2007;65:767–74. doi: 10.1016/j.gie.2006.12.058. [DOI] [PubMed] [Google Scholar]
- 18.Bersani G, Rossi A, Suzzi A, Ricci G, De Fabritiis G, Alvisi V. Comparison between the two systems to evaluate the appropriateness of endoscopy of the upper digestive tract. Am J Gastroenterol. 2004;99:2128–35. doi: 10.1111/j.1572-0241.2004.40078.x. [DOI] [PubMed] [Google Scholar]
- 19.Trevisani L, Sartori S, Gilli G, Chiamenti CM, Gaudenzi P, Alvisi V, et al. Appropriateness of upper gastrointestinal endoscopy: A hospital-based study. Dig Dis Sci. 2001;46:2695–9. doi: 10.1023/a:1012775429096. [DOI] [PubMed] [Google Scholar]
- 20.Rossi A, Bersani G, Ricci G, Defabritiis G, Pollino V, Suzzi A, et al. ASGE guidelines for the appropriate use of upper endoscopy: Association with endoscopic findings. Gastrointest Endosc. 2002;56:714–9. doi: 10.1067/mge.2002.129222. [DOI] [PubMed] [Google Scholar]
- 21.Wiklund I, Glise H, Jerndal P, Carlsson J, Talley NJ. Does endoscopy have a positive impact on quality of life in dyspepsia? Gastrointest Endosc. 1998;47:449–54. doi: 10.1016/s0016-5107(98)70243-3. [DOI] [PubMed] [Google Scholar]
- 22.Rabeneck L, Wristers K, Souchek J, Ambriz E. Impact of upper endoscopy on satisfaction in patients with previously uninvestigated dyspepsia. Gastrointest Endosc. 2003;57:295–9. doi: 10.1067/mge.2003.122. [DOI] [PubMed] [Google Scholar]


