Abstract
Background:
Firefighting is a unique job with contradictious demands that expose firefighters to many well documented causal factors of sleep debt, but no studies in Iran and only a few worldwide studies have investigated their sleep quality while sleep problems may lead to catastrophes especially in critical service workers. The aim of this study is to evaluate sleep quality and its related factors among a sample of professional Iranian firefighters.
Methods:
Using simple random sampling method in a cross-sectional study, 427 personnel of fire and rescue service were invited. They completed the Persian version of Pittsburgh Sleep Quality Index (PSQI) and a data collection sheet about their demographic and occupational features during an individual face to face interview in central office and firehouses throughout Tehran. Response rate was 88.7%.
Results:
The mean ± SD global PSQI score was 7.97 ± 3.77. Sleep latency was the component of PSQI with the greatest degree of abnormality. 69.9% of participants were poor sleepers. Interestingly, we found no significant differences between sleep quality of shift workers and non shift workers. Using multiple logistic regression analysis, only having another job, smoking and years of job experience were predictors of poor sleep.
Conclusions:
In comparison with adult population of Tehran, sleep quality deterioration is notably more common in Tehran firefighters which require health promotion interventions to prevent its serious adverse outcomes.
Keywords: Firefighters, pittsburgh sleep quality index, shift working, sleep quality
INTRODUCTION
Approximately 3100 professional firefighters from 4000 career personnel of Tehran fire and rescue service work in a 24/48 shift schedule. Previous researches have well documented the adverse effects of shift-working, specially very long shifts (>16 h), on sleep quality.[1,2,3] Firefighting is a job that exposes workers to job stress.[4,5] Nowadays we know that job stress can lead to a high prevalence of sleep problems;[6,7] insomnia may lead to depression and weakened job performance; which, in a cyclical manner, increases job stress.[8] In a study on Tehran firefighters, this job was classified as active,[9] but many worldwide studies classified firefighting as high strain according to Karasek model.[10,11]
There are a few reports on sleep quality of firefighters.[12,13] According to these studies, 59% of the US professional firefighters and more than 70% of Changhua firefighters in China had poor sleep quality. In contrast with nurses, sleep researches in other services such as fire protection is limited[14] especially in Iran.
In addition to personal life, the impact of decreased sleep quality on job performance is notable.[15] Undiagnosed and untreated sleep disorders can lead to catastrophes, especially in areas that require a rapid response time such as firefighting. The purpose of this study is to evaluate sleep quality and its related factors among professional firefighters of Tehran, the capital of Iran.
METHODS
This cross-sectional study was conducted in Tehran fire and rescue service. For a 95% confidence interval, a prevalence estimation of at least 60%[12,13] and 5% difference from the expected prevalence, the sample size was estimated approximately 370. We received the list of firefighters and selected 427 of them using simple random sampling. A trained researcher met them at firehouses and central office of the organization to explain the aim of research and answered their questions. He emphasized on the voluntary nature of study and asked them to sign written informed consent. For those who were not at work during the first visit, we scheduled another appointment. The research protocol was approved by the ethics committee of Tehran University of Medical Sciences.
During an individual face-to-face interview in a private room, the researcher asked each precipitant to complete a questionnaire which had two different parts. The first part contained some demographic and occupational data, as seen in Table 1, and the second part was the Persian version of Pittsburgh Sleep Quality Index (PSQI). The original English scale has been showed as a valuable instrument to measure the quality and patterns of sleep[16] and a recent study validated the Persian version.[17] The PSQI distinguishes between poor and good sleep by measuring seven items over the last month, as seen in Table 2. Scoring of the answers is based on a 0 to 3 scale for each item, where 3 reflects the negative extreme on the Likert Scale; therefore, the total score or global PSQI score could be within a range of 0 to 21. A global PSQI score >5 indicates a poor sleep quality.
Table 1.
Characteristics and some sleep habits of participants
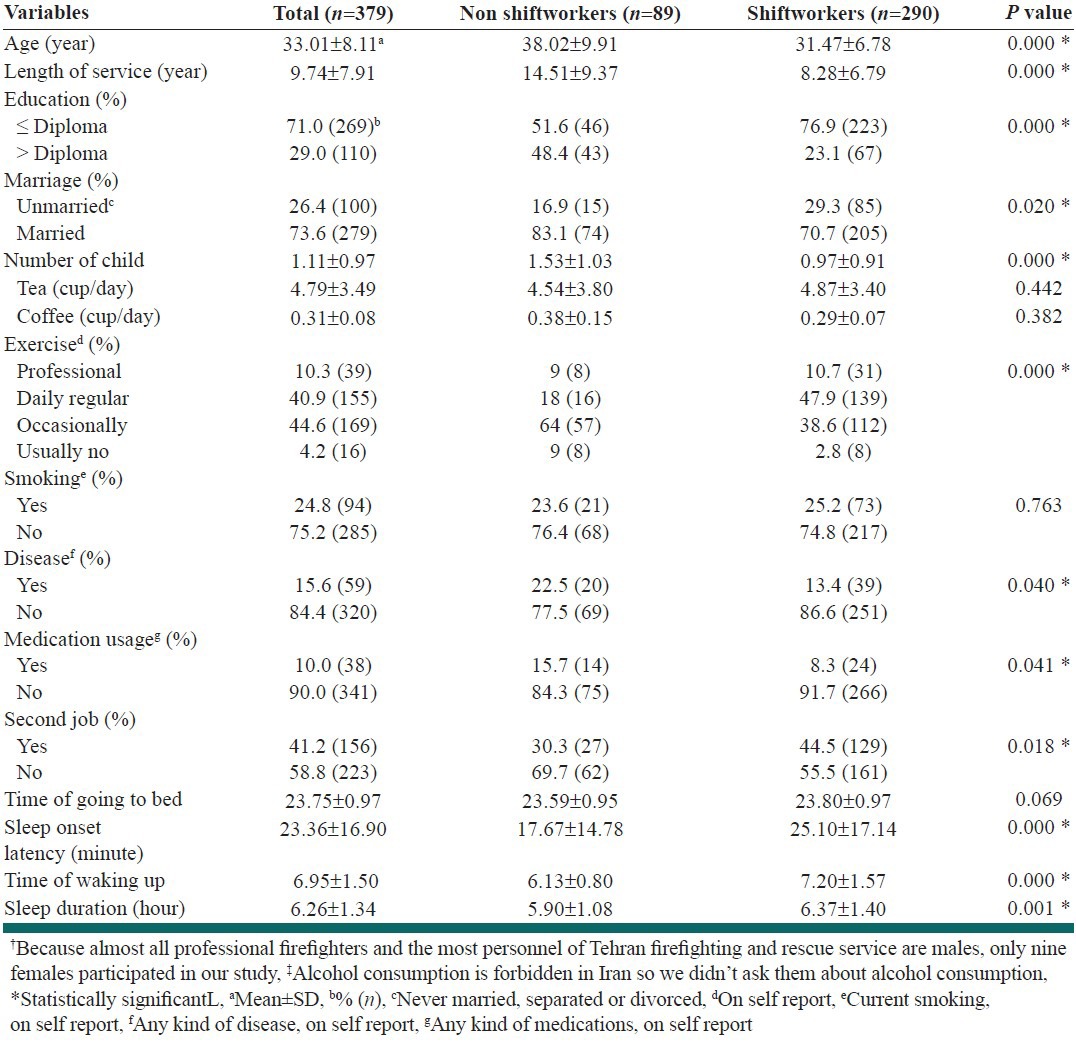
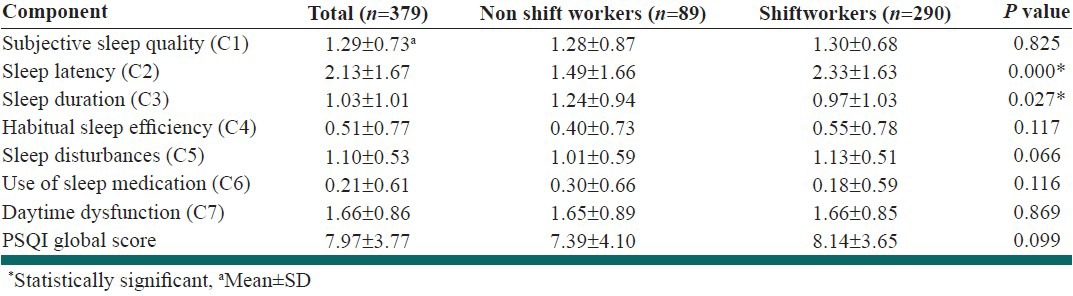
Table 2.
Components of Pittsburgh Sleep quality Index (PSQI) in participants with comparisons between shiftworkers and non shiftworkers
The data was analyzed using version 20 of the SPSS. Other than descriptive analysis, we used independent samples t-test, analysis of variance, Chi square and logistic regression to contrast clinical and demographic features of participants. The significance level was set at a level of P < 0.05.
RESULTS
330 of the 357 invited personnel of firehouses and 49 of the 70 personnel in central office participated in our study (Response Rate = 92.4% and 70.0% respectively). Total response rate was 88.7%. Table 1 demonstrates the characteristics and sleep habits of participants. Median (range) of mission's number in the selected firehouses was 33.50 (13 to 140) in the last month, where only 5.00 (2 to 19) of them were between 24 to 6 am while firehouses had attended to very more calls.
265 (69.9%) of participants were poor sleepers (global PSQI > 5). The prevalence of poor sleep quality among shift workers and non shift workers is shown in Figure 1. The difference between the two groups was not significant.
Figure 1.
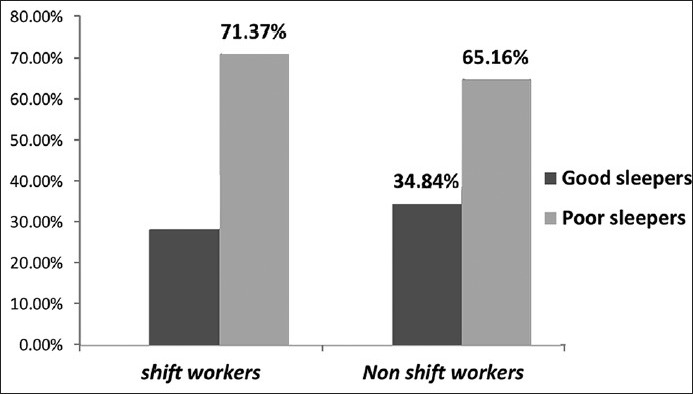
Prevalence of poor sleep quality among shiftworkers and non shiftworkers. The difference was not statistically significant
Components of Pittsburgh Sleep Quality Index (PSQI) among participants are shown in Table 2.
Mean ± SD of age in good sleepers (global PSQI ≤ 5) and poor sleepers was 32.66 ± 8.25 and 33.20 ± 8.04 years respectively; the difference was not significant (P = 0.54). Also we found no significant difference between good sleepers and poor sleepers in years of job experience as a firefighter (9.16 ± 7.93 vs. 10.06 ± 7.91, P = 0.29) and number of monthly fire and rescue missions (64.14 ± 52.00 vs. 66.17 ± 50.72, P = 0.74). Tea consumption (cup/day) was higher in poor sleepers (4.10 ± 2.67 vs. 5.16 ± 3.82, P = 0.00).
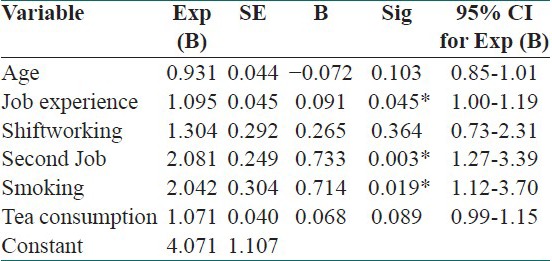
Chi-square tests found significant deteriorated sleep quality among smokers (OR = 1.94, CI 95%: 1.14-3.28, P = 0.01) and among those with another job (OR = 2.43, CI 95%: 1.54-3.82, P = 0.00). Interestingly, having another job was significantly associated with being a shift worker (OR = 1.84, CI 95%: 1.10-3.05, P = 0.01).
As can be seen in Table 3, after adjusting for some relevant variables using multiple logistic regression analysis, only having another job, smoking and years of job experience remained significant independent predictors of poor sleep.
Table 3.
Multiple logistic regression analysis for sleep quality adjusted for some personal and work-related variables
DISCUSSION
The prevalence of poor sleep in our study was 69.9% (CI 95%: 65-74). There were no other contemporary studies about sleep quality of Iranian firefighters available for comparison. The prevalence of poor sleep in the present study was slightly more than 59% prevalence in the US professional firefighters[12] but similar to “more than 70%” prevalence of poor sleep in Changhua firefighters,[13] both were done with similar research instrument. The mean ± SD global PSQI score was 7.97 ± 3.77, 6.02 ± 3.08 and 8.5 in Tehran, the US and Changhua firefighters respectively.
The high prevalence of poor sleep quality among Tehran firefighters was the most important finding of this survey. A study on adult population of Tehran (2008) with similar method and instrument showed that 37% (CI 95%: 35-39) of them were poor sleepers.[18] This notable sleep quality deterioration of Tehran firefighters could be attributed to multiple factors including their job.
There are many evidences that shift working can cause adverse sleep effects,[1,2,3] but we did not find any significant difference between sleep quality of shift workers and non shift workers in present study.
The different findings could be due to the following four reasons: First, although shift-working firefighters work in very long shifts, the number of night missions among selected firehouses was low; therefore their night sleep may be near normal during shifts. Second, up to 75% of non shift-workers have shift-work experiences for several years in their occupational history that may cause long-term permanent deterioration of sleep quality and some studies confirm this effect.[19,20] Third, the average years of job experience among non shift-workers are significantly greater than shift workers that can justify lower sleep quality of them as described below. Finally it seems that because of more flexibility in work schedule and having days off work following each shift among shift workers, they have more hours of night sleep and lesser work-related early morning rising in comparison with non shift workers, as seen in Table 1, that may reduce their sleep problems.[21,22]
Although the vast majority of studies have showed older age as an important risk factor of poor sleep quality,[19,23] our study suggested no significant age difference between good and poor sleepers. Many studies suggest that 50-55 years appear to be a critical point for sleep problems in male workers[24,25,26] but only 1.1% (4) of our participants were ≥55 that can explain difference between our results and those of others. However, a recently published article also showed a significant lower prevalence of sleep deprivation in firefighters ≥48 years of age.[12]
Interestingly, we found years of job experience as an independent predictor of poor sleep after adjustment for age. Other studies have showed a linear positive relationship between job experience as a firefighter and level of traumatic stress and depression. Experienced firefighters are more likely to be encountered to human disasters.[12,27]
In this study, smoker firefighters had a significant more poor sleep quality, as seen in Table 3, which is proved with results of similar researches in firefighters.[12,13]
Also we found a notable higher PSQI in firefighters with second job. Another study had suggested firefighters with other job had significant greater sleepiness.[28] Partially low monthly income may be a cause of this outcome although two days off work following each shift may be another cause in shift workers.
Some limitations of this study might be noted. First, the study design was cross-sectional with all of its limitations. Second, it was not possible to apply objective methods to this study. Third, many elder personnel, especially in central office, had no interest in the project which, similar to healthy worker effect, might be a source of underestimation.
In conclusion, a notable percent of Tehran fire and rescue service personnel were poor sleepers. Our results confirm the need for planning comprehensive programs to decrease the tendency of firefighters toward smoking and having another job. Countermeasures to ensure optimum sleep time, to raise monthly income and to manage sleep/stress of firefighters may be useful. Further follow-up studies are required to explore other probable causal factors.
ACKNOWLEDGMENT
We would like to thank all professional firefighters of Tehran fire and rescue service for their kind cooperation.
Footnotes
Source of Support: Grant funded by Tehran University of Medical Sciences, Tehran, Iran
Conflict of Interest: None declared
REFERENCES
- 1.Sallinen M, Kecklund G. Shift work, sleep, and sleepiness-differences between shift schedules and systems. Scand J Work Environ Health. 2010;36:121–33. doi: 10.5271/sjweh.2900. [DOI] [PubMed] [Google Scholar]
- 2.Caruso C, Rosa RR. Shift Workand Long Work Hours. In: Rom WN, editor. Environmental and Occupational Medicine. 4th ed. New York: Lippincott Williams and Wilkins; 2007. pp. 1360–4. [Google Scholar]
- 3.Lusa S, Hoakkoanen M, Lukkonen R, Vikari-Juntura E. Perceived physical work capacity, stress, sleep disturbance and occupational accidents among firefighters working during a strike. Work Stress. 2002;16:264–74. [Google Scholar]
- 4.Astorino TA, Roberson DW. Efficacy of acute caffeine ingestion for short-term high-intensity exercise performance: A systematic review. J Strength Cond Res. 2010;24:257–65. doi: 10.1519/JSC.0b013e3181c1f88a. [DOI] [PubMed] [Google Scholar]
- 5.Fullerton CS, Ursano RJ, Wang L. Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. Am J Psychiatry. 2004;161:1370–6. doi: 10.1176/appi.ajp.161.8.1370. [DOI] [PubMed] [Google Scholar]
- 6.Utsugi M, Saijo Y, Yoshioka E, Horikawa N, Sato T, Gong Y, et al. Relationships of occupational stress to insomnia and short sleep in Japanese workers. Sleep. 2005;28:728–35. doi: 10.1093/sleep/28.6.728. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, Lemoine P, Arnaud-Briant V, Dreyfus M. Prevalence and consequences of sleep disorders in a shift worker population. J Psychosom Res. 2002;53:577–83. doi: 10.1016/s0022-3999(02)00438-5. [DOI] [PubMed] [Google Scholar]
- 8.Reynolds CF. The implications of sleep disturbance epidemiology. JAMA. 1989;262:1514. [PubMed] [Google Scholar]
- 9.Yazdi SM, Sharifian SA. Job stress and its related factors in Tehran firefighters in year 2000. Tehran Univ Med J. 2001;59:72–8. [Google Scholar]
- 10.Sonnentag S, Frese M. John Wiley and Sons; 2003. Apr 15, [Last cited 2011 Oct 23]. Handbook of Psychology: Stress in Organizations [Internet] place unknown. Available from: http://www.onlinelibrary.wiley.com/doi/10.1002/0471264385.wei1218/full . [Google Scholar]
- 11.Merz MA, Bricout JC, Koch LC. Disability and job stress: Implications for vocational rehabilitation planning. Work. 2001;17:85–95. [PubMed] [Google Scholar]
- 12.Carey MG, Al-Zaiti SS, Dean GE, Sessanna L, Finnell DS. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J Occup Environ Med. 2011;53:928–33. doi: 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee Mh. Master's thesis. Changhua: Institute of Natural Healing Science; 2010. Associated factors affecting sleep quality and coping strategies for addressing insomnia in firefighters. [Google Scholar]
- 14.Doi Y. An epidemiologic review on occupational sleep research among Japanese workers. Ind Health. 2005;43:3–10. doi: 10.2486/indhealth.43.3. [DOI] [PubMed] [Google Scholar]
- 15.Walsleben JA, O’Malley EB, Rapoport DM. Sleep Disorders and Work. In: Rom WN, editor. Environmental and Occupational Medicine. 4th ed. New York: Lippincott Williams and Wilkins; 2007. pp. 1364–73. [Google Scholar]
- 16.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Shahidi J, Khodabakhshi R, Yahyazadeh S, Amini M, Nosrati H. Quality of sleep in cancer patients: Evidence from Persian translation of Pittsburg Sleep Quality Index. AJC. 2007;6:165–8. [Google Scholar]
- 18.Asghari A, Farhadi M, Kamrava SK, Ghalehbaghi B, Nojomi M. Subjective sleep quality in urban population. Arch Iran Med. 2012;15:95–8. [PubMed] [Google Scholar]
- 19.Marquie JC, Foret J. Sleep, age, and shiftwork experience. J Sleep Res. 1999;8:297–304. doi: 10.1046/j.1365-2869.1999.00170.x. [DOI] [PubMed] [Google Scholar]
- 20.Butat C, Barrit J, Brugère D, Cosset M, Touranchet A, Volkoff S. Troubles du sommeil en fonction de l’âge et des horaires de travail. Arch Mal Prof. 1993;54:209–15. [Google Scholar]
- 21.Akerstedt T. Shift work and disturbed sleep/wakefulness. Sleep Med Rev. 1998;2:117–28. doi: 10.1016/s1087-0792(98)90004-1. [DOI] [PubMed] [Google Scholar]
- 22.Kecklund G, Akerstedt T, Lowden A. Morning work: Effects of early rising on sleep and alertness. Sleep. 1997;20:215–23. doi: 10.1093/sleep/20.3.215. [DOI] [PubMed] [Google Scholar]
- 23.Foret J, Bensimon G, Benoit O, Vieux N. Quality of sleep as a function of age and shiftwork. In: Reinberg A, Vieux N, Andlauer P, editors. Night and Shiftwork. Oxford: Pergamon Press; 1981. pp. 149–54. [Google Scholar]
- 24.Nakata A, Haratani T, Kawakami N, Miki A, Kurabayashi L, Shimizu H. Sleep problems in white-collar male workers in an electric equipment manufacturing company in Japan. Ind Health. 2000;38:62–8. doi: 10.2486/indhealth.38.62. [DOI] [PubMed] [Google Scholar]
- 25.Jacquinet-Salord MC, Lang T, Fouriaud C, Nicoulet I, Bingham A. Sleeping tablet consumption, self reported quality of sleep, and working conditions. Group of Occupational Physicians of APSAT. J Epidemiol Community Health. 1993;47:64–8. doi: 10.1136/jech.47.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuppermann M, Lubeck DP, Mazonson PD, Patrick DL, Stewart AL, Buesching DP, et al. Sleep problems and their correlates in a working population. J Gen Intern Med. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- 27.Dees L. Ph.D. dissertation. Texas: Texas Woman's University; 2009. Perceived effects of sleepiness and sleep deprivation among firefighters and emergency medical services providers working a 24/48 shift schedule. [Google Scholar]
- 28.Kim KH, Kim JW, Kim SH. Influence of job stressors on psychosocial well-being, fatigue and sleep sufficiency among firefighters. Korean J Occup Environ Med. 2006;18:232–45. [Google Scholar]


