Abstract
Purpose:
Dental implants though a successful treatment modality there exists controversies regarding the relationship between the adequacy of the keratinized gingiva (KG) and peri-implant health. The presence of an adequate amount of peri-implant KG reduces gingival inflammation and hence soft-tissue augmentation should be frequently considered. Among the various periodontal plastic surgical procedures, the apically displaced flap increases the width of keratinized tissue with reduced patient morbidity. The current study aims at evaluating the esthetic improvement in KG around dental implants applying apically positioned flap (APF) technique.
Materials and Methods:
A total of 10 endosseous dental implants were placed in eight systemically healthy patients. APF surgery was performed at the implant site on the buccal aspect either at the time of implant placement (one stage surgical protocol) or during the implant recovery stage (two stage surgical protocols) for increasing the width of KG and reviewed until 12 weeks post-operatively. The width of KG was evaluated at baseline and at the end of 12 weeks after surgery. Paired t-test was performed to evaluate the changes in the width of KG at baseline and at 12 weeks post-operatively. In addition, soft-tissue esthetic outcome was assessed by using visual analog scale (VAS).
Results:
The mean width of KG at baseline was 1.47 mm and 12 weeks post-operatively was 5.42 mm. The gain in KG from baseline was 3.95 mm with the P value of 0.000, which was highly statistically significant. The assessment of esthetic outcome using VAS gave an average score of 7.1 indicating good esthetics.
Conclusion:
The technique of APF yielded a significant improvement in keratinized tissue, which is both functionally and esthetically acceptable.
Keywords: Dental esthetics, dental implants, flap, gingiva
Introduction
Dental implant has been a successful treatment modality in the management of edentulous patients. Success of osseointegrated implants is predominantly based upon patient selection, conservation of hard and soft-tissues along with following proper surgical techniques and prosthetic protocols. The presence of healthy peri-implant soft-tissue to provide an optimal seal between the oral environment and the implant with its associated super structure plays a crucial role in long-term success of dental implants.[1] The protective barriers for an osseointegrated implant are compromised due to the presence of parallel arrangement of gingival connective tissue fibers resulting in a weak peri-implant mucosal seal.
Controversies exist in the scientific literature regarding the relationship between the adequacy of the keratinized mucosa and the health of peri-implant tissues. Lang and Loe established that a minimum of 2 mm of keratinized gingiva (KG) is required to maintain gingival health regardless of the patient's oral hygiene.[2] However, according to de Trey and Bernimoulin, the width of attached gingiva is not the only determining factor for implant survival.[3] Factors like the patient's age, oral hygiene maintenance, esthetic considerations and patient's expectations, should also be taken into consideration.[4] Several experimental studies (Wennström et al., Mericske-Stern et al., Adell et al., Lekholm et al., Schou et al.) have suggested that there is no correlation between implant success rate and the presence of peri-implant keratinized soft-tissue as long as plaque control is maintained.[5,6,7,8,9] On the other hand, studies by Buser, Schroeder et al., and Kirsch and Ackermann have reported that keratinized mucosa around the abutments is an important requisite for peri-implant health,[10,11,12] presence of an adequate amount of KG around to the implant reduces gingival inflammation[13] and hyperplasia[14] and minimizes marginal peri-implant gingival tissues retraction.[7,14,15]
Though implant survival rate is not merely dependent on the width of keratinized tissues, in areas of esthetic concern and difficulties in plaque control the presence or augmentation of keratinized tissue around implants would be desirable for routine oral hygiene maintenance without causing discomfort.[16,17] Hence, soft-tissue augmentation should be considered to provide a keratinized mucous zone that is as wide as possible embracing the implant prosthesis. Soft-tissue management in areas of implant rehabilitation may be performed before the surgical phase or after the surgical phase and before the prosthetic phase or after the completion of the prosthetic phase.[18] Various periodontal plastic surgical procedures have been proposed for obtaining adequate amounts of keratinized tissue, which include free gingival auto grafts, lateral pedicle rotating flap, apically positioned flap (APF), coronally positioned flap, sub-epithelial connective tissue grafts and cellular dermal grafts.
The APF technique has shown to predictably increase the width of keratinized tissue around natural teeth.[19] The increasing height of attached gingiva occurs because of an apical alteration of the mucogingival junction, which includes apical displacement of the muscular insertions.[20] The advantages of APF technique are minimal post-operative bone loss, controlled post-operative position of the gingival margin and it does not require a second surgical site and hence better patient acceptance and comfort.[21] Disadvantages being that it cannot be advocated for a thin gingival biotype and occasionally formation of a white scar may occur. Though a few studies have shown the effectiveness of APF in improving KG around natural teeth,[22,23,24,25] except a case report by Park et al.,[26] no studies have been done so far to evaluate the gain of keratinized tissue around dental implants using APF; hence, the current study aims at evaluating the clinical improvement in KG and esthetic outcome by applying APF technique around dental implants.
Materials and Methods
The study enrolled 12 patients with partially edentulous dentition requiring the replacement of missing teeth either in the anterior or posterior region of maxilla and mandible who had reported to the Department of Periodontogy and Oral Implantology of SRM dental college, Chennai, India. Signed informed consent was obtained from the subjects before entering into the study and the study protocol was reviewed and approved by the institutional ethical committee. A total of 12 patients including 6 non - periodontitis and 6 with mild periodontitis were included in this study. Patients included had an age range of 24-47 years. Baseline evaluation of the full mouth plaque score, probing pocket depth, clinical attachment level, gingival biotype and the width of KG was recorded [Table 1]. Patients with moderate to severe periodontitis, pregnant women, lactating mothers, smokers and those with systemic diseases were excluded from the study. All patients had full mouth Scaling and Root surface debridement done and if any periodontal surgical procedures were to be performed was completed. Reevaluation of base line parameters was carried out after 8 weeks during which four patients who had poor oral hygiene maintenance and persisting active periodontal disease sites were excluded from the study [Table 1]. Finally, a total of 10 endosseous dental implants (self-threaded EZ - Hi tech life care implants, Israel) were placed in selected sites in 8 patients [Table 2]. APF surgery was performed at the implant site on the buccal aspect either at the time of implant placement (one stage surgical protocol) or during the implant recovery stage (two stage surgical protocols) for increasing the width of KG. A para-crestal incision was placed and a full thickness mucoperiosteal flap was raised 2 mm apical to the cemento enamel junction of the adjacent natural teeth followed by a split thickness flap. Two vertical releasing incisions were placed on either side on the buccal gingiva at the mesial and distal line angles of the adjacent teeth. The flap was positioned apically and was sutured around the healing cap. The vertical releasing incisions were sutured with simple interrupted sutures and a periosteal anchoring suture was placed at the base of the flap [Figures 1-5]. Periodontal dressing was placed if necessary and routine post-operative instructions and medications were given. Patients were followed at 1 week, 4 weeks and at 12 weeks post-operatively. The width of KG was evaluated at baseline and at the end of 12 weeks[27] after performing apically displaced flap surgery [Figures 6 and 7]. In addition, soft-tissue esthetic outcome was assessed by an independent examiner using visual analog scale (VAS) at 12 weeks following the surgery.
Table 1.
Baseline and 8 weeks re-evaluation values before implant placement
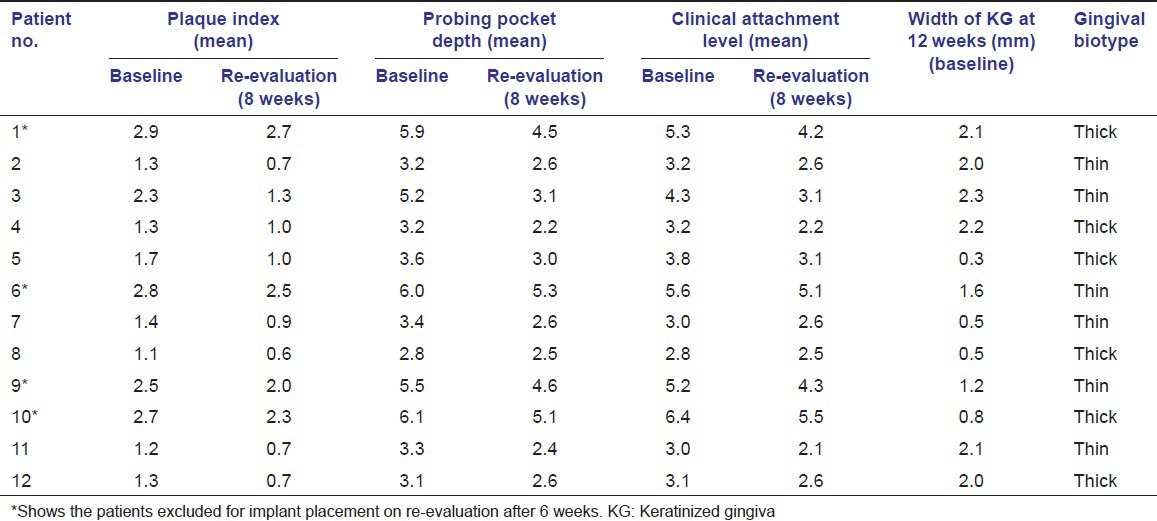
Table 2.
Implant sites, baseline and 12 week post.operative width of KG and VAS score
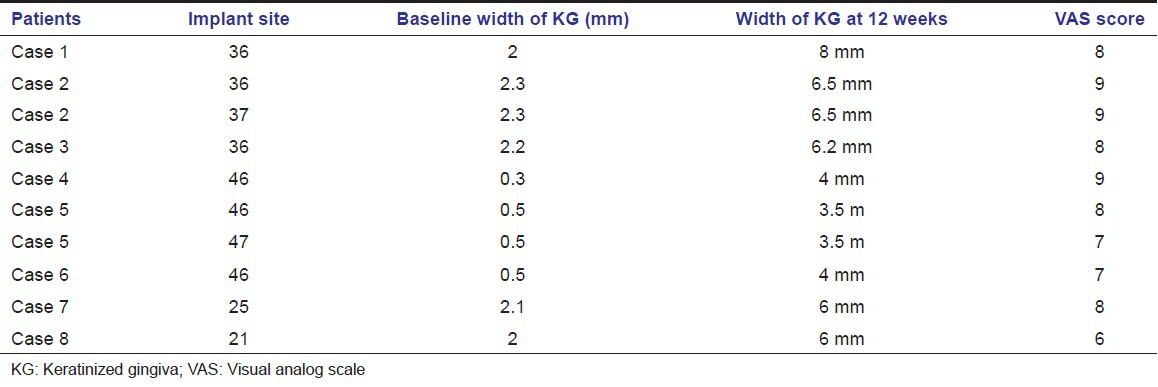
Figure 1.

Pre-operative edentulous site
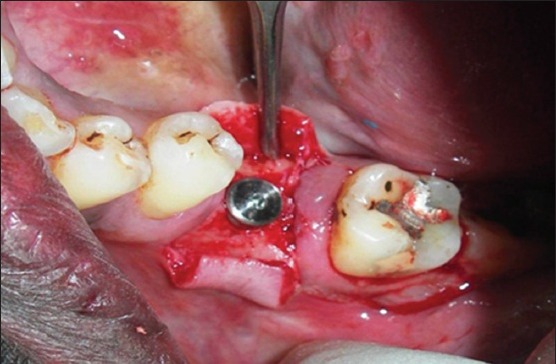
Figure 5.
Flap apically displaced and sutured
Figure 6.

12 weeks post-operative
Figure 7.

Implant with prosthesis
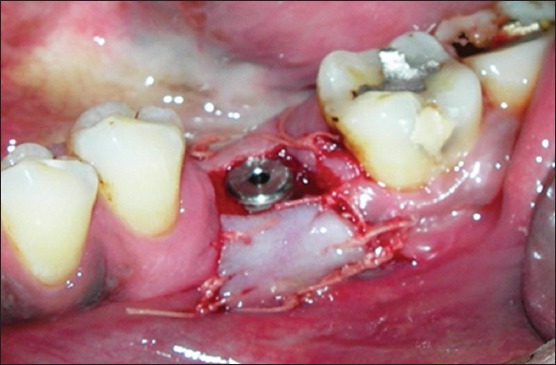
Figure 2.

Para crestal and papilla preservation incision given, flap reflection and implant osteotomy performed
Figure 3.
Implant placed
Figure 4.
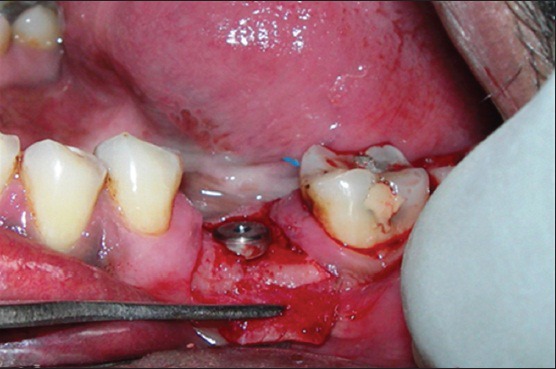
Split thickness flap raised with vertical releasing incisions
Statistical analysis
The statistical package for social sciences program SPSS v19.0 (SPSS Inc, Chicago, IL, USA) was used to perform Paired t-test to evaluate the changes in the width of KG at baseline and at 12 weeks post-operatively. A P < 0.05 was considered significant for the present study.
Results
Table 2 shows the baseline and 12 weeks post-operative width of KG and VAS score around 10 dental implants placed in eight patients.
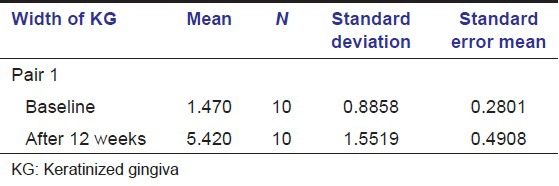
The mean width of KG at baseline was 1.47 mm and 5.42 mm at 12 weeks post-operatively as seen in Table 3.
Table 3.
Paired samples statistics
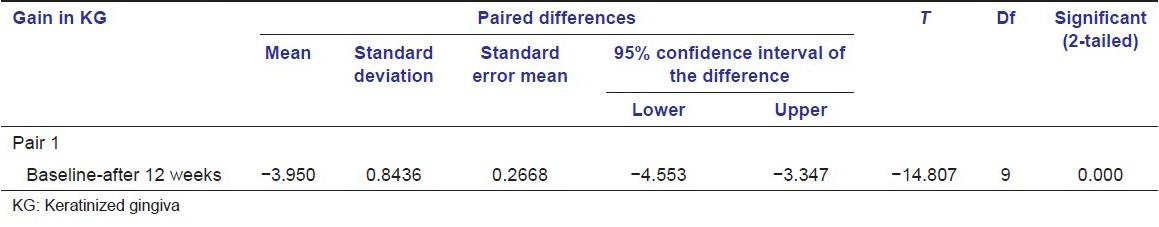
The gain in KG from baseline was 3.95 mm with the P value of 0.000, which was highly statistically significant as seen in Table 4a and b.
Table 4a.
Paired samples correlations
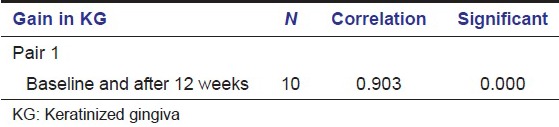
Table 4b.
Paired samples test
The assessment of esthetic outcome using VAS gave an average score of 7.1 indicating good esthetics.
Figures 8 and 9 show the diagrammatic representation of the changes in the width of KG at baseline and at 12 weeks post-operatively and the VAS score respectively.
Figure 8.
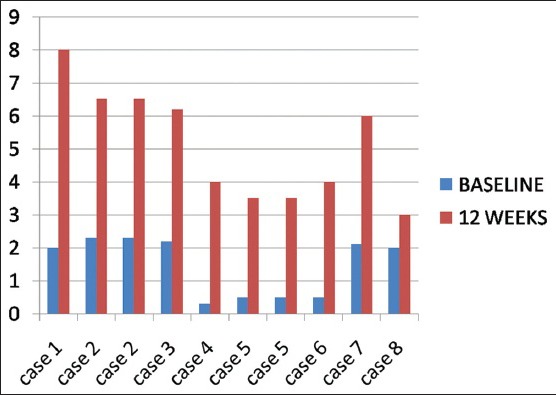
Diagrammatic representation of baseline and 12 weeks width of keratinized tissue
Figure 9.
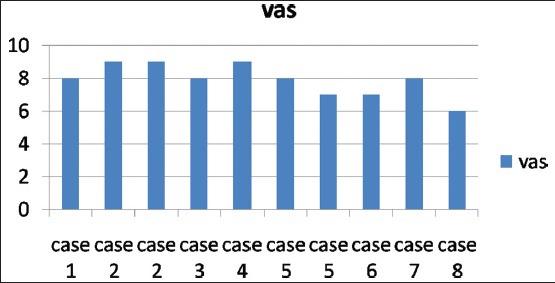
Visual analog scale scores
Discussion
The plaque accumulation around implants leads to marginal tissue inflammation, which may result in peri-implantitis.[28] Block and Kent had reported that the presence of keratinized tissue was significantly associated with good mucosal health and crestal bone loss of 2 mm or greater was seen in areas with lack of KG.[13] Warrer et al., in their animal experimental study in monkeys concluded that implants without keratinized mucosa resulted in more recession and attachment loss when compared with implants with adequate keratinized tissue.[13] Chung et al., suggested that plaque accumulation and gingival inflammation were higher around dental implants with keratinized mucosa <2 mm.[29] Recent studies by Bouri et al., Kim et al., Schrott et al., reported that increased width of keratinized mucosa around dental implants is associated with lesser soft-tissue recession and greater hard tissue stability resulting in an advantage for long-term maintenance of implants.[30,31,32]
The fact that mucosal thickness and the width of keratinized mucosa are of significance particularly in the esthetic zone, where narrow and thin gingival biotype may result in greater gingival recession, led to the introduction of many surgical procedures for soft-tissue augmentation around dental implants.[33,34] Numerous studies have shown that increase in the amount of KG can be obtained by several different types of procedures, either before, simultaneously or after implant placement.[35,36,37] Though subepithelial connective tissue graft is the gold standard for gingival augmentation, use of such soft-tissue grafts have the intrinsic drawback of second surgical site morbidity, increased surgical time and cost and additional patient discomfort due to prolonged healing time needed at the donor site, which can overcome by APF technique.
Park et al., 2010 reported two cases, where the pre-existing narrow band of keratinized mucosa was displaced bucco-apically by APF with a partial thickness flap and stabilized by using a pre-fabricated implant-retained stent clipped over provisional abutments.[26] In the present study, the technique of APF around implants showed statistically significant improvement with a mean gain of 3.95 mm in the width of KG at the end of 12 weeks (P < 0.000), the results of which correlate with case report by Park et al., who showed a gain in KG following APF and to the best of our knowledge this is the first study to assess the esthetic outcome of apically displaced flap around implants. The esthetic outcome evaluated by an independent examiner using VAS gave an average score of 7.1 indicating good esthetics.
Conclusion
The technique of APF resulted in significant improvement in keratinized tissue, which is both functionally and esthetically acceptable. Further longitudinal studies with a control group and adding clinical parameters such as plaque index, gingival index and evaluation of crestal bone loss should be done to assess long-term stability of the gain in KG and its influential role in maintaining peri-implant health.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cate AT. The gingival junction. In: Branemark PI, Zarb G, Albrektsson T, editors. Tissue-Integrated Prostheses. Chicago: Quintessence Publ. Co; 1986. pp. 145–53. [Google Scholar]
- 2.Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43:623–7. doi: 10.1902/jop.1972.43.10.623. [DOI] [PubMed] [Google Scholar]
- 3.de Trey E, Bernimoulin JP. Influence of free gingival grafts on the health of the marginal gingiva. J Clin Periodontol. 1980;7:381–93. doi: 10.1111/j.1600-051x.1980.tb02011.x. [DOI] [PubMed] [Google Scholar]
- 4.Hall WB. Present status of soft tissue grafting. J Periodontol. 1977;48:587–97. doi: 10.1902/jop.1977.48.9.587. [DOI] [PubMed] [Google Scholar]
- 5.Wennström JL, Bengazi F, Lekholm U. The influence of the masticatory mucosa on the peri-implant soft tissue condition. Clin Oral Implants Res. 1994;5:1–8. doi: 10.1034/j.1600-0501.1994.050101.x. [DOI] [PubMed] [Google Scholar]
- 6.Mericske-Stern R, Steinlin Schaffner T, Marti P, Geering AH. Peri-implant mucosal aspects of ITI implants supporting overdentures. A five-year longitudinal study. Clin Oral Implants Res. 1994;5:9–18. doi: 10.1034/j.1600-0501.1994.050102.x. [DOI] [PubMed] [Google Scholar]
- 7.Adell R, Lekholm U, Rockler B, Brånemark PI, Lindhe J, Eriksson B, et al. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg. 1986;15:39–52. doi: 10.1016/s0300-9785(86)80010-2. [DOI] [PubMed] [Google Scholar]
- 8.Lekholm U, Adell R, Lindhe J, Brånemark PI, Eriksson B, Rockler B, et al. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986;15:53–61. doi: 10.1016/s0300-9785(86)80011-4. [DOI] [PubMed] [Google Scholar]
- 9.Schou S, Holmstrup P, Hjørting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: A review of the literature. Clin Oral Implants Res. 1992;3:149–61. doi: 10.1034/j.1600-0501.1992.030401.x. [DOI] [PubMed] [Google Scholar]
- 10.Buser D. Mukogingival chirugrie. In: Schroeder HE, Sutter F, Krekeler G, editors. Orale Implantolgie Allegemeiene Grundlogen Und ITI-hohlzyl-indersystem. Stuttgart: Goerg Theime Verlag; 1988. pp. 285–97. [Google Scholar]
- 11.Schroeder A, van der Zypen E, Stich H, Sutter F. The reactions of bone, connective tissue, and epithelium to endosteal implants with titanium-sprayed surfaces. J Maxillofac Surg. 1981;9:15–25. doi: 10.1016/s0301-0503(81)80007-0. [DOI] [PubMed] [Google Scholar]
- 12.Kirsch A, Ackermann KL. The IMZ osteointegrated implant system. Dent Clin North Am. 1989;33:733–91. [PubMed] [Google Scholar]
- 13.Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995;6:131–8. doi: 10.1034/j.1600-0501.1995.060301.x. [DOI] [PubMed] [Google Scholar]
- 14.Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: The Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990;64:185–94. doi: 10.1016/0022-3913(90)90177-e. [DOI] [PubMed] [Google Scholar]
- 15.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 16.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 17.Block MS, Kent JN. Factors associated with soft- and hard-tissue compromise of endosseous implants. J Oral Maxillofac Surg. 1990;48:1153–60. doi: 10.1016/0278-2391(90)90531-6. [DOI] [PubMed] [Google Scholar]
- 18.Artzi Z, Tal H, Moses O, Kozlovsky A. Mucosal considerations for osseointegrated implants. J Prosthet Dent. 1993;70:427–32. doi: 10.1016/0022-3913(93)90079-4. [DOI] [PubMed] [Google Scholar]
- 19.Ainamo A, Bergenholtz A, Hugoson A, Ainamo J. Location of the mucogingival junction 18 years after apically repositioned flap surgery. J Clin Periodontol. 1992;19:49–52. doi: 10.1111/j.1600-051x.1992.tb01148.x. [DOI] [PubMed] [Google Scholar]
- 20.Carranza FA, Newman MG, Takei HH, Klokkevold PR. 10th ed. Rio de Janeiro: Guanabara Koogan; 2007. Periodontia Clínica; p. 1286. [Google Scholar]
- 21.Martins TM, Fernandes LA, Mestrener SR, Saito CT, de Oliveiranobrega FJ, Bosco AF. Apically positioned flap: Reestablishment of esthetics and integrity of the dentogingival unit. Perspect Oral Sci ABR. 2010;2:2175–5124. [Google Scholar]
- 22.Harris RJ. Clinical evaluation of 3 techniques to augment keratinized tissue without root coverage. J Periodontol. 2001;72:932–8. doi: 10.1902/jop.2001.72.7.932. [DOI] [PubMed] [Google Scholar]
- 23.McGuire MK, Nunn ME. Evaluation of the safety and efficacy of periodontal applications of a living tissue-engineered human fibroblast-derived dermal substitute. I. Comparison to the gingival autograft: A randomized controlled pilot study. J Periodontol. 2005;76:867–80. doi: 10.1902/jop.2005.76.6.867. [DOI] [PubMed] [Google Scholar]
- 24.McGuire MK, Scheyer ET, Nunn ME, Lavin PT. A pilot study to evaluate a tissue-engineered bilayered cell therapy as an alternative to tissue from the palate. J Periodontol. 2008;79:1847–56. doi: 10.1902/jop.2008.080017. [DOI] [PubMed] [Google Scholar]
- 25.Mohammadi M, Shokrgozar MA, Mofid R. Culture of human gingival fibroblasts on a biodegradable scaffold and evaluation of its effect on attached gingiva: A randomized, controlled pilot study. J Periodontol. 2007;78:1897–903. doi: 10.1902/jop.2007.070083. [DOI] [PubMed] [Google Scholar]
- 26.Park JC, Yang KB, Choi Y, Kim YT, Jung UW, Kim CS, et al. A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: A report of two cases. J Periodontal Implant Sci. 2010;40:194–200. doi: 10.5051/jpis.2010.40.4.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gordon HP, Sullivan HC, Atkins JH. Free autogenous gingival grafts. II. Supplemental findings – Histology of the graft site. Periodontics. 1968;6:130–3. [PubMed] [Google Scholar]
- 28.Cochran D. Implant therapy I. Ann Periodontol. 1996;1:707–91. doi: 10.1902/annals.1996.1.1.707. [DOI] [PubMed] [Google Scholar]
- 29.Chung DM, Oh TJ, Shotwell JL, Misch CE, Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77:1410–20. doi: 10.1902/jop.2006.050393. [DOI] [PubMed] [Google Scholar]
- 30.Bouri A, Jr, Bissada N, Al-Zahrani MS, Faddoul F, Nouneh I. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008;23:323–6. [PubMed] [Google Scholar]
- 31.Kim BS, Kim YK, Yun PY, Yi YJ, Lee HJ, Kim SG, et al. Evaluation of peri-implant tissue response according to the presence of keratinized mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e24–8. doi: 10.1016/j.tripleo.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 32.Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20:1170–7. doi: 10.1111/j.1600-0501.2009.01795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nemcovsky CE, Moses O. Rotated palatal flap. A surgical approach to increase keratinized tissue width in maxillary implant uncovering: Technique and clinical evaluation. Int J Periodontics Restorative Dent. 2002;22:607–12. [PubMed] [Google Scholar]
- 34.Simons AM, Darany DG, Giordano JR. The use of free gingival grafts in the treatment of peri-implant soft tissue complications: Clinical report. Implant Dent. 1993;2:27–30. doi: 10.1097/00008505-199304000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Phillips K, Kois JC. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998;42:57–70. [PubMed] [Google Scholar]
- 36.Misch CE, Al-Shammari KF, Wang HL. Creation of interimplant papillae through a split-finger technique. Implant Dent. 2004;13:20–7. doi: 10.1097/01.id.0000116368.76369.78. [DOI] [PubMed] [Google Scholar]
- 37.Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: An evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74:557–62. doi: 10.1902/jop.2003.74.4.557. [DOI] [PubMed] [Google Scholar]


