Abstract
Edentulous patients with maxillectomy defects present a significant challenge for prosthetic rehabilitation and the adaptive capabilities of the patient as retention is highly compromised. Hence, the option of using endosseous implants to increase obturator retention has been used. A patient of mucormycosis of the left maxilla was treated with surgical excision. After satisfactory healing, definitive implant supported magnet retained prosthesis was fabricated for the patient. Implants with magnetic units offer a practical method of improving the retention of obturators provided acceptable prosthetic protocols are followed for the rehabilitation.
Keywords: Edentulous maxillectomy, implants, magnets, mucormycosis, obturator
Introduction
The prosthetic rehabilitation for maxillectomy patients aims at separation of oral and nasal cavities to allow adequate deglutition and articulation, to restore the midfacial contour and to provide acceptable esthetic results. Lack of support, retention and stability are common problems associated with patients who have undergone maxillectomy.[1] The retention of an obturator depends on various factors such as: Direct and indirect retention provided by the remaining teeth, defect size, tissue undercuts available around the cavity and development of muscular control.[2] The presence of teeth facilitate prosthetic rehabilitation, however, fabrication of prosthesis for an edentulous patient with maxillectomy defect is challenging even to the most experienced clinician.[3,4]
This clinical case report describes the prosthodontic management of an edentulous patient who had undergone partial maxillectomy due to mucormycosis. Osseointegrated dental implants and magnet attachments were used to achieve a retentive and stable, large sized definitive obturator.
Case Report
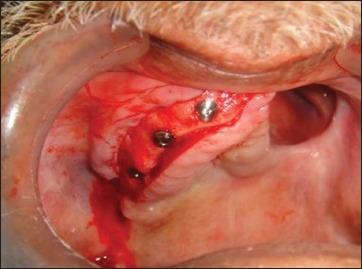
A 52-year-old ex-serviceman reported to the department of oral and maxillofacial surgery with chief complaints of foul breath and ulcer since 2 months. Medical history revealed that he was an uncontrolled Type II diabetic for the past 13 years. Histopathological investigations led to the diagnosis of mucormycosis of left maxilla. The lesion was excised; all periodontally compromised maxillary teeth were extracted. Partial maxillectomy was performed by the surgeons [Figures 1]. The patient was referred to Department of Prosthodontics for functional and aesthetic rehabilitation. Intraoral examination revealed a raw, 4 cm × 2 cm Aramany's Class I type of left maxillectomy defect. A surgical obturator was fabricated for the patient to aid in healing and function.
Figure 1.

Pre-operative view
The patient was recalled after 2 weeks for a review clinical examination. The defect was healed and covered with healthy mucosa. Mandibular movements were within the normal range; tongue function was normal and speech was inarticulate. The remaining mandibular teeth were supra erupted. For the interim prosthesis, irreversible hydrocolloid (Plastalgin, Septodont, France) impression was made and casts were prepared in Type III dental stone (Kalstone, Kalabhai, India). Functional border molding of the tissues was carried out and the defect area was impressioned using high fusing impression compound (Pinnacle, DPI, India) and light body silicone impression material (Aquasil, Dentsply, Germany). A hollow bulb obturator was fabricated using compression molding technique and inserted. The patient used the prosthesis for 03 months during, which multiple adjustments and relining with a resilient tissue conditioning material (GC Reline Soft, GC, Japan) were carried out.
Definitive prosthesis
The retention was a major concern, patient being edentulous. In the process of planning for an implant supported definitive prosthesis, radiographic evaluation revealed adequate height and width of the residual ridge with D3 type maxillary bone for implant placement. An implant supported definitive prosthesis was therefore planned, which would enhance the compromised retention for this case of “edentulous” maxillectomy defect. A diagnostic maxillary impression was made with an irreversible hydrocolloid using a stock metal tray. The impression was poured in Type III dental stone for designing of the definitive obturator and planning for placement of dental implants. Three two stage osseointegrated dental implants (MIS; Confident System) were placed in the residual right maxilla: (diameter: 3.75 mm, length: 11 mm) in the right maxillary first molar site; (diameter: 3.75 mm, length: 13 mm) in the right maxillary canine site and (diameter: 3.75 mm, length: 11 mm) in the right maxillary incisor region [Figure 2]. Post-operative orthopantomogram was carried out to check the implants placement after achieving clinical primary stability [Figure 3].
Figure 2.
Three implants placed in residual maxilla
Figure 3.

Post-operative OPG showing implants in position
The second stage surgery was performed after 08 months. After the implants were checked for clinical success they were exposed and gingival formers were placed. Abutments were milled and screwed; transfer copings were placed over the implants and an open tray impression was made with medium body silicone material (Aquasil, Dentsply Caulk, Germany). Impression was poured in Type III dental stone and master cast was fabricated. Magnetic keepers were placed over the abutments on the cast and wax patterns for the copings were fabricated. The modified copings were cast in nickel chrome alloy (Bellabond+, Bego, Germany). After polishing, copings were cemented to the superior surface of the abutment with resin cement (Variolink N, Ivoclar, Liechtenstein) [Figure 4]. In addition, surveying and designing procedures of master cast were carried out for the fabrication of metal denture base framework. Refractory cast was made by duplicating blocked out master cast. Wax up for the metal framework and routine investing and casting procedures were performed. The metal framework was finished, polished and tried in patient's mouth.
Figure 4.

Copings of magnetic keeper cemented over implants
A custom impression tray was fabricated on the metal framework using autopolymerizing resin and adjusted for proper extension in patient's mouth. Border molding was performed for the residual maxilla and the defect was recorded using the addition silicone soft putty (Aquasil, Denstply, Germany) and definitive impression was made using light body silicone impression material (Aquasil Ultra LV, Denstply Caulk, Germany). Conventional prosthodontic protocols of boxing and pouring the impression with American Dental Association Type III dental stone were followed to fabricate a definitive cast.
After adapting a layer of modeling wax (Cavex Outline, Netherlands), the definitive cast was flasked and processed in the customary manner to fabricate a hollow bulb using heat-activated methyl methacrylate (Lucitone 199; Dentsply). The processed record base was evaluated intraorally for extensions and occlusal rim was fabricated using modeling wax. Modeling wax was then used to fabricate occlusal rim. The wax rim was adjusted to provide adequate vertical dimension and lip support. Maxillomandibular jaw relations were recorded and transferred to an articulator (Hanau H2; Teledyne Technologies, Los Angeles) using a whipmix self-centered springbow type of facebow.
Denture teeth (Cosmo HXL, Dentsply, China) were arranged and evaluated intraorally for dentolabial relation and lip support and horizontal and vertical jaw relations were verified. Upon the patient's approval for phonetics and esthetics, waxing and festooning of the gingival and palatal portions of the obturator were completed, the processed base was reinvested and the prosthesis was processed into heat-activated methyl methacrylate. The completed prosthesis was fitted intraorally and remounted to equilibrate occlusion.
After necessary adjustments, each magnet (Cobalt-samarium, Ambica Co., India) was centered on the magnetic keeper coping with a thin (0.001 inch) cellophane separating sheet interposed to prevent acrylic resin from locking onto the abutment. A small amount of acrylic resin was added on the intaglio surface of the denture where magnets were to be secured. The denture was inserted intraorally and seated to pick up the magnets [Figure 5]. Pressure indicating paste was used to determine any undue pressure placed on the surrounding tissues.
Figure 5.
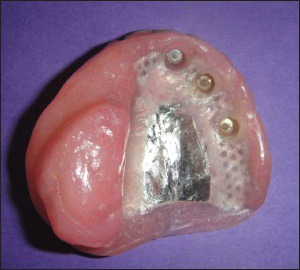
Finished prosthesis with magnets in place
The obturator prosthesis was inserted [Figure 6] and phonetics and esthetics was re-evaluated. Post-insertion instructions were given to the patient and follow-up was carried out every 03 weeks. The last follow-up of the patient was 6 months following the insertion of the new prosthesis. The patient had been using the new obturator prosthesis satisfactorily and no signs of failure associated with implants were detected. The peri-implant tissues and the defect area appeared healthy.
Figure 6.
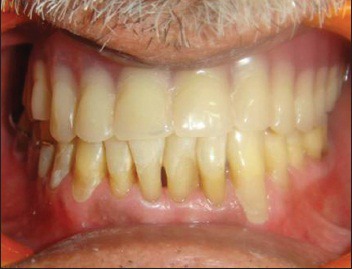
Prosthesis in situ
Discussion
Edentulous patients with maxillectomy defects present a significant challenge for prosthetic rehabilitation and the adaptive capabilities of the patient as retention is highly compromised. The only option for retaining prosthesis in such cases, besides implants, is optimum engagement of the available soft-tissue undercuts found within the defect space and the non-affected side. The ability to fully engage these undercuts is further limited by the path of insertion for the prosthesis and the restricted mouth opening.[4] Hence, the option of using endosseous implants to increase obturator retention has been introduced in the present case.[5] The overall survival rate for implants supporting maxillofacial prosthesis was reported to be as high as 96.1%.[6]
Although magnets may not result in adequate denture retention in every case, it is apparent that the nature of the magnetic force in controlling vertical displacement of the denture is likely to result in an improvement in retention.[7] Magnetic retention units in the form of cobalt samarium magnets can be embodied conveniently in the conventional obturators. The technique is simple to use, particularly when compared with other retention procedures, which can be both complicated and time consuming.[8] In this patient magnets were preferred over the conventional bar and clip design because of space constraints. Moreover, magnets avoid lateral stresses which are essential for long-term implant success.[9] Magnets have the disadvantages of low corrosion resistance and possible cytotoxic effects, which may limit their use in the oral cavity, but studies have revealed that no such-tissue damaging effects have been observed clinically for cobalt samarium magnets.[10]
Surgical reconstruction of the palate using a free tissue transfer may provide a stable permanent partition between oral and nasal cavities. However, it gives way to gravity, distorting palatal contours and preventing access into the defect for support and retention of the prosthesis. Surgically reconstructed defects may or may not improve the treatment outcome when compared with conventional prosthetic rehabilitation of the defect.[11,12] Zygomatic implants that provide remote anchorage have also been proposed in the rehabilitation of maxillary defects, but this option was eliminated because of the lack of available bone.[13]
Meticulous oral hygiene measures and regular follow-up needs to be instituted for a patient using implant supported obturator prosthesis. It is advised that the patient wears the prosthesis at night as sinus secretions and saliva cannot be managed without it.
Conclusion
Edentulous patients with maxillectomy defects present a challenging situation for the maxillofacial prosthodontist. Prosthetic rehabilitation is often difficult to achieve due to the absence of teeth, lack of favorable tissue undercuts and presence of non-keratinized nasal mucosa. Obturator prostheses should recreate a partition between the oral and nasal cavities to restore oral function and esthetics. Implants with magnetic units offer a practical method of improving the retention of obturators provided acceptable prosthetic protocols are followed for the rehabilitation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Beumer J, III, Curtis TA, Marunick MT. St. Louis: Ishiyaku Euro America, Inc; 1996. Maxillofacial Rehabilitation: prosthodontic and Surgical Considerations; p. 251. [Google Scholar]
- 2.Parr GR, Tharp GE, Rahn AO. Prosthodontic principles in the framework design of maxillary obturator prostheses. J Prosthet Dent. 1989;62:205–12. doi: 10.1016/0022-3913(89)90315-6. [DOI] [PubMed] [Google Scholar]
- 3.Keyf F. Obturator prostheses for hemimaxillectomy patients. J Oral Rehabil. 2001;28:821–9. doi: 10.1046/j.1365-2842.2001.00754.x. [DOI] [PubMed] [Google Scholar]
- 4.Roumanas ED, Nishimura RD, Davis BK, Beumer J., 3rd Clinical evaluation of implants retaining edentulous maxillary obturator prostheses. J Prosthet Dent. 1997;77:184–90. doi: 10.1016/s0022-3913(97)70233-6. [DOI] [PubMed] [Google Scholar]
- 5.Parel SM, Branemark PI, Jansson T. Osseointegration in maxillofacial prosthetics. Part I: Intraoral applications. J Prosthet Dent. 1986;55:490–4. doi: 10.1016/0022-3913(86)90184-8. [DOI] [PubMed] [Google Scholar]
- 6.Ueda M, Hibino Y, Niimi A. Usefulness of dental implants in maxillofacial reconstruction. J Long Term Eff Med Implants. 1999;9:349–66. [PubMed] [Google Scholar]
- 7.Smith GA, Laird WR, Grant AA. Magnetic retention units for overdentures. J Oral Rehabil. 1983;10:481–8. doi: 10.1111/j.1365-2842.1983.tb01471.x. [DOI] [PubMed] [Google Scholar]
- 8.Riley MA, Walmsley AD, Harris IR. Magnets in prosthetic dentistry. J Prosthet Dent. 2001;86:137–42. doi: 10.1067/mpr.2001.115533. [DOI] [PubMed] [Google Scholar]
- 9.Oh WS, Roumanas E. Dental implant-assisted prosthetic rehabilitation of a patient with a bilateral maxillectomy defect secondary to mucormycosis. J Prosthet Dent. 2006;96:88–95. doi: 10.1016/j.prosdent.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Gillings BR. Magnetic retention for complete and partial overdentures. Part I. J Prosthet Dent. 1981;45:484–91. doi: 10.1016/0022-3913(81)90032-9. [DOI] [PubMed] [Google Scholar]
- 11.Pigno MA. Conventional prosthetic rehabilitation after free flap reconstruction of a maxillectomy defect: A clinical report. J Prosthet Dent. 2001;86:578–81. doi: 10.1067/mpr.2001.119844. [DOI] [PubMed] [Google Scholar]
- 12.Genden EM, Okay D, Stepp MT, Rezaee RP, Mojica JS, Buchbinder D, et al. Comparison of functional and quality-of-life outcomes in patients with and without palatomaxillary reconstruction: A preliminary report. Arch Otolaryngol Head Neck Surg. 2003;129:775–80. doi: 10.1001/archotol.129.7.775. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt BL, Pogrel MA, Young CW, Sharma A. Reconstruction of extensive maxillary defects using zygomaticus implants. J Oral Maxillofac Surg. 2004;62:82–9. doi: 10.1016/j.joms.2004.06.027. [DOI] [PubMed] [Google Scholar]


