Abstract
An otherwise healthy 19-year-old female patient had painless swelling in her left buccal mucosa. No precipitating factors were identified. Pathological analysis demonstrated the mass to be a Masson's hemangioma, a papillary proliferation of thin-walled capillaries intimately associated with thrombus. A very rare tumor occurring in oral cavity with only 80 cases being published in literature until date.
Keywords: Hemangioma, intravascular papillary endothelial hyperplasia, thrombus
Introduction
The term hemangioma commonly describes a large number of vasoformative tumors. Unfortunately, the nomenclature and the classification of these tumors are complex and not consistent over a period of time. The complexity and the inconsistency in its classification have resulted in usage of a large number of terms and classification systems, resulting in confusion in understanding the pathophysiology of these lesions and in comparing data from different periods.
What was referred to as a hemangioma 30 years ago may not necessarily be applicable today. The term hemangioma described many lesions that bore little relationship to each other, apart from their being involved with vessels. With this concept in mind, this article discusses a rare variant of hemangioma, i.e., Masson's Hemangioma occurring in the oral cavity.
Case Report
A 19-year-old female patient was referred to the Department of Oral and Maxillofacial Surgery by the Department of Oral Medicine for the diagnosis and management of a painless “swelling” in the left buccal mucosa. The intraoral swelling was noticed by the patient 1 year back. According to the patient, the swelling had recently enlarged interfering with her mastication. No changes of size or development of swelling during meal times were reported. The patient was in apparent good health and her medical history was non-contributory.
Clinical examination showed a 3 × 2 cm swelling in the left buccal mucosa, which was freely movable. Intra-orally, it was covered by a mucosa of normal texture and color. On digital palpation, the swelling was non-tender, non-fluctuant, and rubbery in consistency. The swelling had well-defined margins and was not fixed to the underlying as well as overlying structures. There was no sign of hypoesthesia or paresthesia of the area involved.
A computerized tomography (CT) scan with enhancement was performed to confirm the existence of a well-demarcated mass lying anterior to the masseter muscle [Figure 1]. The lesion was solid, without any relation to the mandible. The remainder of the head and neck scan did not reveal any other pathology or lymph node enlargement. Although it was believed that magnetic resonance imaging could give more precise and accurate information for the diagnosis and management of the lesion, the patient refused any further imaging study.
Figure 1.

CT scan showing a soft tissue mass lying anterior to masseter
Differential diagnosis
The structures of oral cavity can be affected by numerous pathological conditions that could be developmental, inflammatory, or neoplastic in origin. Lesions in the oral cavity may be present for a longer period of time before the patient seeks any medical intervention, which is usually as a result of interference with swallowing or speech.
Based on the clinical presentation of the swelling, it appeared that the mass originated from the underlying mesenchymal tissues as opposed to the overlying mucosa. Our differential diagnosis was broken down into the general categories of reactive lesions, benign neoplastic lesions, and infectious origin. Specifically, our differential diagnosis of this soft tissue mass of buccal mucosa included lesions of minor salivary gland origin (benign vs. malignant salivary gland tumor, mucocele), vascular origin (hemangioma), non-odontogenic soft-tissue infection, hematomas, an intramasseteric abscess, masseteric hypertrophy, benign neoplasms of smooth muscle origin (leiomyoma), and reactive and neoplastic neural lesions (traumatic neuroma, neurofibroma, neurilemoma).
Cystic lesions-like dermoid cysts were clearly excluded by the CT findings, because fluid in the cysts would not have demonstrated enhancement by the contrast material.
No history of trauma excluded the possibility of hematoma.
Traumatic neuroma was also considered. However, traumatic neuromas typically occur in the mental foramen region, tongue, and lower lip. One-third to one-fourth of these lesions are painful and are usually associated with trauma. The patient had no history of trauma. Benign neural neoplasms such as neurofibroma and neurilemoma may present as smooth-surfaced nodules similar in color to the adjacent normal mucosa. Approximately 25-45% of schwannomas or neurilemomas occur in the head and neck region, with tongue and buccal mucosa representing the most frequent intraoral lesions. Therefore, benign neural tumor was considered in one of the differential diagnosis.
Salivary gland tumors account for 1% of neoplastic lesions in the head and neck region.[1,2]
A salivary gland neoplasm could have been a possibility, because the lesion was in close proximity to both parotid gland and minor salivary glands of buccal mucosa. Although the parotid gland is by far the most common site for salivary gland neoplasms, accounting for 64-80% of all cases, CT scans of this patient failed to reveal any parotid gland enlargement. Approximately 11-15% of minor salivary gland tumors occur in buccal mucosa. These typically present as painless, slow-growing, firm, frequently mobile swellings.[3,4] Taking into account the size of the lesion in the present case, the possibility that this could represent either a high-grade mucoepidermoid carcinoma or adenoid cystic carcinoma of minor salivary gland origin was considered.
Infections and inflammatory lesions of perioral tissues may also present as a swelling in the buccal mucosa. Acute infections, such as Ludwig angina or cellulitis, which may derive from an odontogenic focus of infection, osteomyelitis, were not considered in the differential diagnosis because of the chronic nature of the condition.[5,6] In addition, fever, malaise, and pain would normally accompany the clinical presentation of an acute infection, and tenderness to palpation and fixed or fluctuant overlying skin would be apparent in the clinical examination. In addition, an intramasseteric abscess was unlikely, because there was no redness of skin or oral mucosa over the mass and the patient had no associated symptoms of fever or pain.
Masseteric hypertrophy is a benign condition characterized by an enlargement of the bilateral masseter muscle that appears as a homogenous enlargement on CT. In the present case, CT showed the lesion as a unilateral mass.
Mucoceles of the minor salivary glands are rarely >1.5 cm in diameter and are always superficial. Mucoceles found in deeper areas are usually larger. Mucoceles can cause a convex swelling, depending on the size and location, as well as difficulties in speaking or chewing.[7] Mucoceles can appear at any site of the oral mucosa containing salivary glands. The two types of mucoceles are more commonly found at different sites. Extravasation mucoceles appear frequently on the lower lip, whereas retention mucoceles appear at any other location of the oral cavity. The lower lip is the most frequent site for a mucocele, as it is the most probable place for a trauma, especially at the premolar level. A study of 312 patients showed 230 lesions on the lower lip (73.7%), with the tongue as the second most common location (15.4%).[8] These locations are followed by the buccal mucosa and palate and are rarely found in the retromolar region and posterior dorsal area of the tongue. Mucocele of buccal mucosa is a superficial lesion and, in the present case, the lump was deep in origin.
Hemangiomas frequently appear as reddish-blue lesions. Hemangiomas of the head and neck occur commonly in infancy and childhood, especially in girls. Hemangiomas in the masseter muscle are relatively rare, and approximately 90% of these lesions develop before the age of 30 years. However, this group of lesions was excluded from our differential diagnosis because the lesion did not blanch with pressure and needle aspiration was negative.
Lipomas are slow-growing, nearly always benign, adipose tumors that are most often found in the subcutaneous tissues.[9] These tumors may also be found in deeper tissues such as the intermuscular septa, the abdominal organs, the oral cavity, the internal auditory canal, the cerebellopontine angle, and the thorax.[10] Some lipomas are believed to have developed following blunt trauma. Lipomas usually present as non-painful, round, mobile masses, with a characteristic soft, doughy feel. The overlying skin appears normal. Lipomas can usually be correctly diagnosed by their clinical appearance alone. In the present case, the mass was mobile, non-tender, and rubbery in consistency, but non-slippery. Lipoma was also considered to be one of the differential diagnosis.
Management and diagnosis
Needle aspiration yielded neither blood nor any other fluid. An incisional biopsy was performed under local anesthesia, during which, profuse bleeding was noted. The patient did not have a history of bleeding disorders and was not taking anticoagulant or other medication that could interfere with coagulation. Histopathological examination of the specimen revealed cystic spaces with papillary projections, fibrocollagenous tissue, and skeletal muscles, which was not conclusive of any typical pathology. An excisional biopsy was performed under local anesthesia. After clinical and radiological diagnosis, the patient was planned under conscious sedation. Intra-oral incision or parallel to occlusal plane was given. Submucosally lesion was identified and dissected bluntly from rest of the tissue, particularly in the region of masseter muscle. Whole of the lesion was removed and, after achieving hemostasis, the wound was closed primarily. The excised tissue was submitted for histopathological evaluation [Figure 2]. The lesion appeared macroscopically as an enucleated soft tissue lesion without evidence of bony involvement. Histopathological examination revealed increased vascularity. Endothelial cells arranged in multiple papillary-like projections within the major lumen. Dilated vascular space lined by plump endothelial cells with multiple anastomosing channels were seen. Papillary projections were proliferating into the lumen of the major vessel and surrounded by muscles of the vessel wall. No increased mitotic activity was evident [Figures 3 and 4]. Since there was no dysplasia in the endothelial lining, the possibility of angiosarcoma histologically was also ruled out. Attempt of thrombus formation was evident in the lumen of many vessels.
Figure 2.
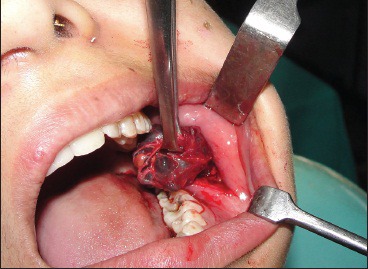
Complete surgical excision of the lesion
Figure 3.
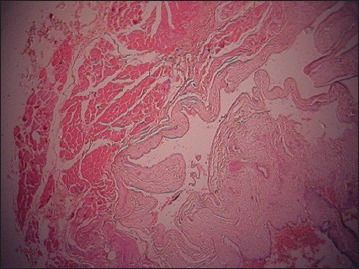
Multiple papillary projections within the major lumen (H and E, ×4)
Figure 4.

Attempt of thrombus formation into the lumen of blood vessel (H and E, ×10)
Immunohistochemical staining was performed using an avidin-biotin method. Immunoreactivity for factor VIII was seen positive in the papillary structure of the cystic lining [Figure 5].
Figure 5.
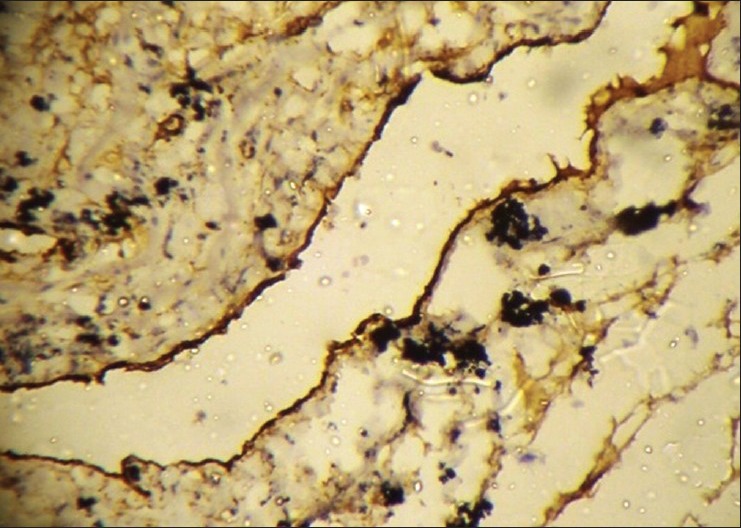
Positivity for factor VIII in the papillary projections. (Immunohistochemical staining, ×10)
The final diagnosis of Masson's hemangioma was made after extensively reviewing the slides and also after reviewing the archival literature. The patient was followed for several months and was found to be disease-free, without any evidence of local recurrence.
Discussion
Hemangiomas are benign non-reactive lesions, characterized by the presence of numerous blood vessels of varying caliber.[11] Hemangiomas are sometimes considered to represent hamartomas, exuberant growths of normal tissue at sites where the tissue is routinely present.[12] Hemangiomas may be localized or involve extensive regions of the body; the latter lesions are more appropriately termed angiomatosis. The head and neck region is a site of predilection for superficial hemangiomas, with a distinct female predilection.[12]
Based on histological appearance, hemangiomas have been sub-classified into several subtypes, including capillary, cavernous, and arteriovenous hemangiomas. This classification is based on the predominant type of vascular channels.[13]
First named “Hemangioendotheliome vegetant intravasculaire” by Masson in 1923, Masson's hemangioma is an exuberant endothelial proliferation that requires differential diagnosis from angiosarcoma. Masson described it to be a form of neoplasm and explained the pathogenesis as proliferation of endothelial cells into the vessel lumen, followed by obstruction, secondary degeneration, and necrosis. On the other hand, Henschen depicted the lesion as a reactive process rather than as a neoplasm. Kauffman and Stout remarked that, although endothelial proliferation that can be easily mistaken for a characteristic of sarcoma is present, the endothelial layer of the lesion is composed of normal endothelial cells, the endothelial proliferation is of benign papillae pattern, and the cells show no atypia. Today, it is considered to be a reactive vascular proliferation following traumatic vascular stasis.[14]
Microscopically, short, blunted papillary projections with a hyalinized core are associated with thrombotic or clot material and are covered by a single layer of plump endothelial cells that lack anaplasia, pleomorphism, or significantly elevated mitotic activity, unlike angiosarcomas.[14]
Histologically, Masson's hemangioma or intravascular papillary endothelial hyperplasia (IPEH) has a characteristic exuberant endothelial proliferation within the lumen of medium-sized veins. Hashimoto et al., described three forms of IPEH. The primary form arises in a dilated vascular space, the secondary or mixed form occurs within the preexisting vascular lesion, and the third or extravascular form appears within the hematomas. Pins et al., documented 314 cases, and the primary form was 56%, the secondary form originating within a preexisting vascular structure such as an aneurysm, hemangioma, arteriovenous malformation, or lymhpangioma was 40%, and the extravascular form was found in 4%.[15,16] In the present case, the patient did not have any history of trauma or preexisting vascular lesion, so it was considered as a primary form.
Although the most common sites of IPEH are the head, neck, fingers, and trunk, these tumors may occur in any blood vessel. However, the occurrence of IPEH in the oral cavity is extremely rare. A review in the accessible literature showed less than 80 cases of IPEH in the oral mucosa and lips.[17]
Although benign, this lesion is clinically important because it presents as a mass lesion that may be mistaken histologically for angiosarcoma. Moreover, it tends to recur if incompletely resected. Correct diagnosis of the lesion is essential to prevent overly aggressive treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Johns ME, Goldsmith MM. Incidence, diagnosis, and classification of salivary gland tumors. Part 1. Oncology (Williston Park) 1989;3:47–62. [PubMed] [Google Scholar]
- 2.Bentz BG, Hughes CA, Ludemann JP, Maddalozzo J. Masses of salivary gland region in children. Arch Otolaryngol Head Neck Surg. 2000;126:1435–9. doi: 10.1001/archotol.126.12.1435. [DOI] [PubMed] [Google Scholar]
- 3.Speight PM, Barret AW. Salivary gland tumors. Oral Dis. 2002;8:229–40. doi: 10.1034/j.1601-0825.2002.02870.x. [DOI] [PubMed] [Google Scholar]
- 4.Friedrich RE, Bleckmann V. Adenoid cystic carcinoma of salivary gland and lacrimal origin; localization, classification, clinical pathological correlation, treatment results and long term follow up control in 84 patients. Anticancer Res. 2003;23:931–40. [PubMed] [Google Scholar]
- 5.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofaical Pathology. Philadelphia: W.B. Saunders; 1995. [Google Scholar]
- 6.Regezi JA, Sciubba J. 2nd ed. Philadelphia: Saunders; 1993. Oral pathology, Clinical-pathologic Correlations. [Google Scholar]
- 7.Baurmash HD. Mucoceles and ranulas. J Oral Maxillofac Surg. 2003;61:369–78. doi: 10.1053/joms.2003.50074. [DOI] [PubMed] [Google Scholar]
- 8.de Camargo Moraes P, Bönecker M, Furuse C, Thomaz LA, Teixeira RG, de Araújo VC. Mucocele of the gland of Blandin-Nuhn: Histological and clinical findings. Clin Oral Investig. 2009;13:351–3. doi: 10.1007/s00784-009-0252-x. [DOI] [PubMed] [Google Scholar]
- 9.Anders KH, Ackerman AB. Neoplasms of the subcutaneous fat. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, et al., editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw-Hill; 1999. pp. 1292–300. [Google Scholar]
- 10.Koh HK, Bhawan J. Tumors of the skin. In: Moschella SL, Hurley HJ, editors. Dermatology. 3rd ed. Philadelphia: Saunders; 1992. pp. 1721–808. [Google Scholar]
- 11.Weiss SW, Goldblum JR. 4th ed. St. Louis: Mosby; 2001. Enzinger and Weiss's Soft Tissue Tumors. [Google Scholar]
- 12.Enzinger FM, Weiss S. St. Louis: Mosby; 1988. Soft Tissue Tumors. [Google Scholar]
- 13.Vilanova JC, Barceló J, Smirniotopoulos JG, Pérez-Andrés R, Villalón M, Miró J, et al. hemangioma from head to toe: MR imaging with pathologic correlation. Radiographics. 2004;24:367–85. doi: 10.1148/rg.242035079. [DOI] [PubMed] [Google Scholar]
- 14.Korkolis DP, Papaevangelou M, Koulaxouzidis G, Zirganos N, Psichogiou H, Vassilopoulos PP. Intravascular papillary endothelial hyperplasia (Masson's hemangioma) presenting as a soft-tissue sarcoma. Anticancer Res. 2005;25:1409–12. [PubMed] [Google Scholar]
- 15.Hashimoto H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia: A clinicopathologic study of 91 cases. Am J Dermatopathol. 1983;5:539–46. doi: 10.1097/00000372-198312000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Pins MR, Rosenthal DI, Springfield DS, Rosenberg AE. Florid extravascular papillary endothelial hyperplasia (Masson's pseudoangiosarcoma) presenting as a soft tissue sarcoma. Arch Pathol Lab Med. 1993;17:259–63. [PubMed] [Google Scholar]
- 17.Bologna-Molina R, Amezcua-Rosas G, Guardado-Luevanos I, Mendoza-Roaf PL, González-Montemayor T, Molina-Frechero N. Intravascular papillary endothelial hyperplasia (Masson's Tumor) of the mouth: A case report. Case Rep Dermatol. 2010;2:22–6. doi: 10.1159/000279656. [DOI] [PMC free article] [PubMed] [Google Scholar]


